respiratory system
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
126 Terms
what are the main functions of the respiratory system ?
internal and external respiration
removal of inhaled foreign particles
warming and humidification of air
pH balance
production of sound
external respiration
gas exchange between alveolar air and blood
internal respiration
gas exchange between blood and tissues
cellular respiration
oxidising food to co2 and water
what are the accessory muscles of inspiration ?
sternocleidomastoid and scalenus
what are the muscles of active respiration ?
internal intercostals and abdominals
what are the major muscles of inspiration ?
external intercostals and diaphragm
positive co-operativity
binding of each O2 to a given subunit increases the O2-binding affinity of the other subunits
what divides the upper and lower respiratory system ?
below larynx = lower
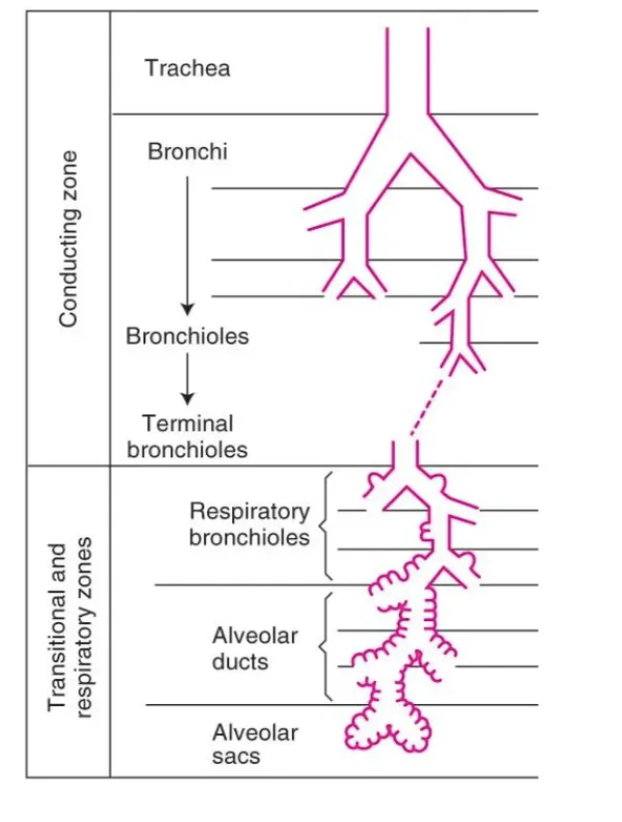
where does the conducting zone end ?
terminal bronchioles
role of upper respiratory tract
filters and humidifies air
the pharynx is further divided into
naso, oro and laryngopharynx
role of sinuses
reduce skull weight
modify and amplify sound
cushioning effect
the lungs are located in
the thorax
the right lung has how many lobes ?
3 - left only 2
role of lower respiratory tract
allows airflow in and out of lungs
how many cm from larynx does the trachea bifurcate into L+R bronchi ?
10cm
conducting zone
nasal cavity to terminal bronchioles
warms and moistens air
why is the conducting zone referred to as anatomical dead space ?
no gas exchange (150ml)
respiratory zone
respiratory bronchioles to alveoli
site of gas exchange
how type I and II alveoli (pneumocytes) differ ?
type I - thin, delicate, flat
type II - produce surfactant
what % of alveolar surface is composed of type I pneumocytes ?
90 - 95
microorganisms and dust are removed from respiratory surfaces by
alveolar macrophages
apnoea
temporary cessation of breathing
asphyxia
tissue starvation due to lack of oxygen in air
cyanosis
blueness of skin from insufficient o2 in blood
dyspnoea
difficult of laboured breathing
hyperpnoea
increased pulmonary ventilation that matches increased metabolic demand
when not breathing pressure in lungs =
atmospheric
what happens to vol and pressure during inspiration ?
increased vol so decreased pressure
what happens to vol and pressure during exhalation ?
decreased vol. increased pressure
the lungs move due to…
contraction / relaxation of diaphragm and intercostal muscles
the lungs are connected to skeletal muscles of the thoracic wall via the
pleura
the visceral pleura lines
lungs
the parietal pleura lines
inner surface of thoracic cavity and rib cage
pressure in the pleural cavity compared to the lungs or atmosphere is
always negative
the diaphragm is innervated by
phrenic nerve
air flows in what direction ?
down pressure gradient
why is exhalation described as a passive process ?
lungs naturally want to recoil inwards
how does forced expiration differ from passive ?
contraction of accessory muscles further reduces volume of thoracic cavity
abdominal and internal intercostals
why do lungs have a tendency to recoil ?
elastic fibres - stretched during inspiration
surface tension
effect of surface tension
promotes alveolar collapse
causes irregular lung recoil
makes inspiration more difficult
surfactant
minimises surface tension
secreted by type II alveolar epithelial cells
increases lung compliance
NRDS
neonatal respiratory distress syndrome
developmental insufficiency of pulmonary surfactant and structural immaturity in lungs
what forces keep alveoli open ?
surfactant and alveolar interdependence
what forces promote alveolar collapse ?
surface tension and elastic recoil
alveolar interdependence
tendency of surrounding alveoli to pull open collapsing alveolus, resisting collapse
what proportion of respiratory work is required to overcome elastic recoil?
70% of total work
what is meant by respiratory work ?
energy and mechanical effort required to breathe
includes work to overcome elastic and airway resistance
what proportion of respiratory work is required to overcome airway resistance ?
30%
where is airway resistance greatest ?
medium sized bronchi
how does bronchoconstriction affect airway resistance?
decreases airway radius and increases resistance
airflow rate (F) =
pressure gradient / airway resistance
what is the atmospheric pressure at sea level ?
760mmHg
which part of the nervous system causes bronchodilation?
SNS sympathetic
which part of the nervous system causes bronchoconstriction ?
PNS parasympathetic
where does gas exchange occur in the lungs ?
between alveolar sacs and pulmonary capillaries
what air the main components of air ?
nitrogen, oxygen, co2
what % of air is nitrogen
78
how does emphysema affect gas exchange ?
decreases alveolar surface area, reducing gas exchange
what conditions increase respiratory membrane thickness?
pulmonary oedema
fibrosis
pneumonia
what percentage of oxygen in blood is physically dissolved ?
3%
how is the majority of oxygen transported in the blood ?
bound to haemoglobin
what determines haemoglobin saturation with oxygen?
partial pressure of oxygen (PO₂)
PO₂ is a measure of
dissolved oxygen in blood
how many oxygen molecules can one haemoglobin bind ?
4
what are the two components of haemoglobin ?
globin (4 polypeptide chains) and 4 iron-containing haem groups
avg. haematocrit (% of RBCs)
45%
myoglobin
oxygen-binding protein in muscle
stores O₂ and binds only one molecule
what does the oxygen dissociation curve show ?
relationship between PO₂ and haemoglobin saturation
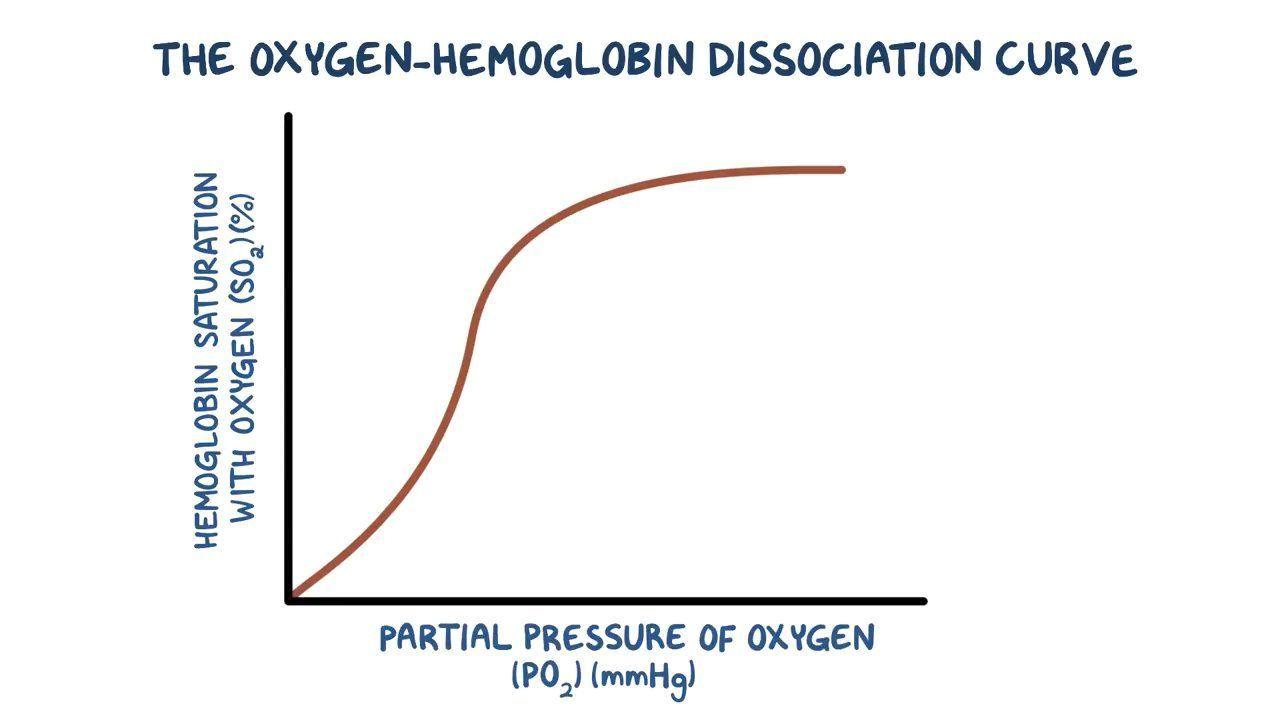
what is positive co-operativity in haemoglobin binding ?
binding of the first O₂ makes it easier for the next O₂ to bind
why is oxygen released from haemoglobin at tissues ?
PO2 decreases (CO2, acidity and temp increase)
reduce Hb affinity for O2
does arterial PO₂ equal alveolar PO₂ in health ?
yes
what are the 3 main ways CO₂ is transported in the blood?
Physically dissolved in plasma (10%)
Bound to haemoglobin as carbaminohaemoglobin (30%)
As bicarbonate ions (most CO₂)
what determines the amount of CO₂ dissolved in plasma ?
the PCO2
how does CO₂ bind to haemoglobin ?
binds to globin portion, forming carbaminohaemoglobin (HbCO₂)
how is most CO₂ transported in the blood ?
as bicarbonate ions (HCO₃⁻) after reacting with water to form carbonic acid, then dissociating
which enzyme accelerates the conversion of CO₂ and water into carbonic acid ?
carbonic anhydrase - found in RBCs
why is bicarbonate an efficient CO₂ transport form ?
more soluble than CO₂ and can easily diffuse out of RBCs into plasma
what is the result of carbon manoxide binding to Hb ?
prevents O2 binding
what is hypercapnia ?
elevated CO₂ in the blood, usually due to hypoventilation
what condition does hypercapnia cause ?
respiratory acidosis lowers blood pH due to excess H⁺
hypocapnia
low CO₂ in the blood, usually due to hyperventilation
what condition does hypocapnia cause ?
respiratory alkalosis - increased blood pH due to reduced H⁺ production.
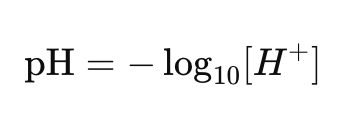
what is the normal plasma pH range ?
7.35 - 7.45
what pH values are incompatible with life ?
below 6.8 above 7.8
how is pH related to hydrogen ion conc. ?
a pH change of 1 = 10 fold change in conc. of hydrogen ions
what is a volatile acid ?
acids excreted via lungs eg. carbonic acid
short chain fatty acids
what are metabolic (non-volatile) acids ?
produced from sources other than CO2
not excreted by lungs
result of incomplete metabolism of carbs. fats, proteins
examples of metabolic acids
lactic acid
ketones
fatty acids
amino acids
what leads to gain of H+ in body
metabolic processes (produce CO2)
loss of bicarbonate (in diarrhoea and urine)
what leads to a loss of H+ in the body ?
vomiting or excretion via urine
what indicates a respiratory acid-base disturbance ?
abnormal PCO2
what indicates a metabolic acid-base disturbance ?
abnormal HCO3- (bicarbonate)
what defines acidosis ?
blood pH below 7.35
what defines alkalosis ?
blood pH above 7.45
what are the three mechanisms for maintaining pH balance?
Buffer systems (first line)
Respiratory compensation
Renal compensation
what is the major extracellular buffer ?
bicarbonate
how does the respiratory system compensate in metabolic acidosis ?
increases ventilation to remove CO2 and lower H+
how do the kidneys compensate for respiratory acidosis ?
excrete H⁺ and reabsorb/regenerate bicarbonate