Med-Surge Objecttve 5 Lecture 1 Fluid and Electrolyte Balance in Nursing Care
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
Hydration
Essential for life and bodily functions.
Fluid Functions
Transport nutrients and waste in the body.
Sweat Glands
Excrete 600 ml/day of fluid.
Bowels
Eliminate 100-200 ml/day of fluid.
Kidneys
Main regulator, excretes 1-2 liters/day.
Lungs
Release 300 ml/day of fluid.
Fluid Regulators
Brain regulates thirst and fluid intake.
Homeostasis
Equilibrium in body's internal environment.
Adaptive Mechanisms
Responses promoting healthy survival and balance.
Total Body Water
60% of adult body weight is water.
Age and Water Content
Varies by age, gender, and body mass.
Intracellular Fluid
Accounts for 2/3 of body fluid.
Extracellular Fluid
Makes up 1/3 of body fluid.
Transcellular Fluid
Fluid within epithelial spaces.
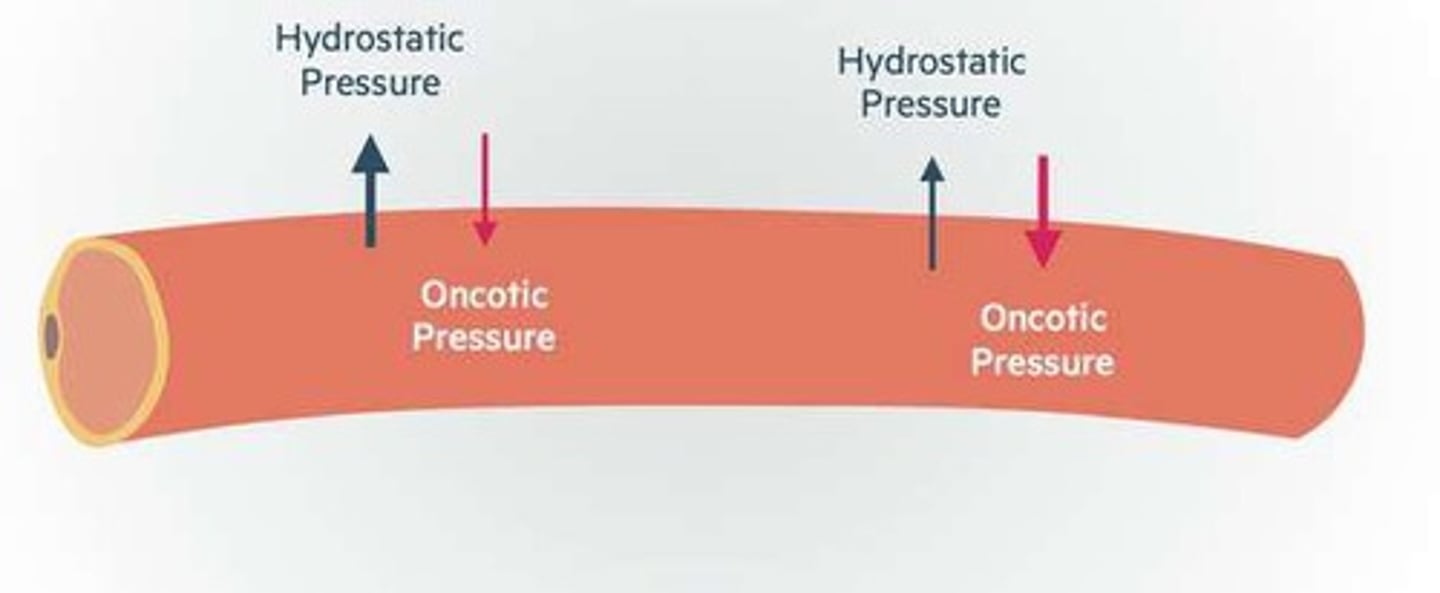
Intravascular Fluid
Fluid within blood vessels.
Interstitial Fluid
Fluid between cells, 2/3 of ECF.
Diffusion
Passive movement of solutes from high to low concentration.
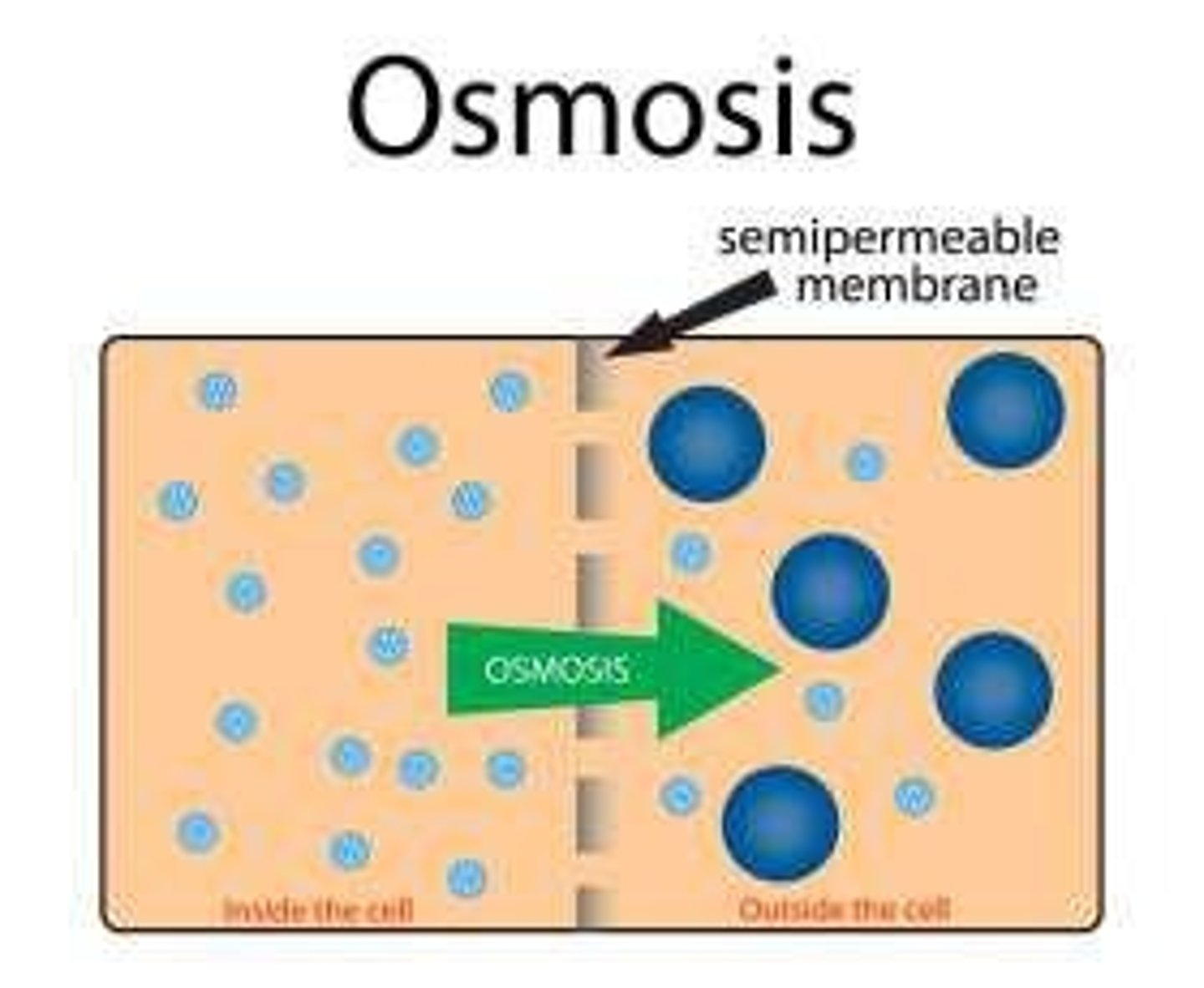
Osmosis
Passive movement of fluid from high to low concentration.
Active Transport
Energy-dependent movement against concentration gradient.
Electrolyte Movement
Regulates fluid balance and cell function.
Fluid Movement
Constant motion, influenced by sodium levels.
Infusion Therapy
Used to manage fluid and electrolyte imbalances.
Water Functions
Transporting nutrients, electrolytes, and oxygen to cells.
Hypovolemia
Fluid volume deficit, leading to dehydration.
Hypervolemia
Fluid volume excess, causing swelling.
Third Spacing
Fluid volume displaced from vascular compartments.
Gastro-hypovolemia
Fluid deficit due to gastrointestinal loss.
Kidney Failure
Fluid excess due to impaired kidney function.
Allergic Reaction
Third spacing caused by severe allergic response.
IV Fluid Therapy
Treatment for excessive fluid loss or deficit.
Lasix
Diuretic medication causing fluid volume reduction.
Fluid Imbalances Causes
Reduced intake, poor diet, excessive substances.
Extracellular Fluid Volume Deficit
Insufficient volume in vascular compartments.
Signs of Hypovolemia
Thirst, acute weight loss, oliguria, and confusion.
Oliguria
Low urine output indicating fluid deficit.
Blood Pressure Changes
Decreased BP with rapid, weak pulse.
Skin Turgor
Poor skin elasticity indicating dehydration.
Rehydration Therapy
8-10 glasses of water daily for hydration.
Monitoring Interventions
Track weight, intake, output, and vital signs.
Client Education
Inform about treatment reasons and engage participation.
Hypervolemia Causes
Excessive intake or abnormal fluid retention.
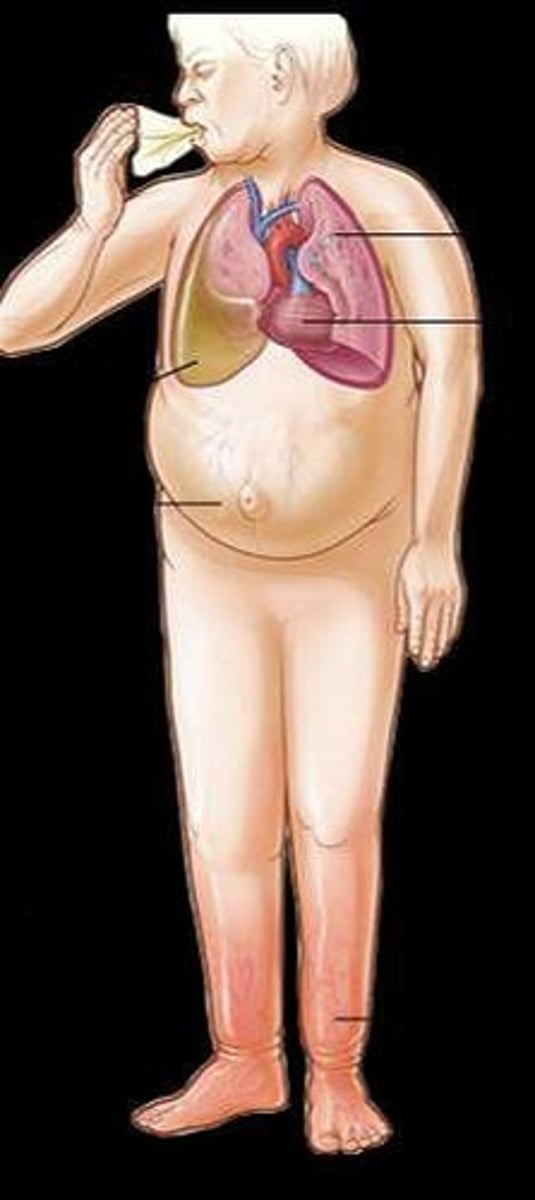
Pulmonary Edema
Fluid accumulation in lung air sacs.

Signs of Hypervolemia
Elevated BP, increased breathing effort, crackles.
Physical Assessments
Monitor for signs of improvement or worsening.
Fluid Volume Excess (FVE)
Condition with excess fluid in body tissues.
Signs of FVE
Weight gain and prominent jugular veins.
Diuretics
Medications known as 'water pills' for fluid removal.
IV Therapy
Intravenous delivery of medications and fluids.
Provider Interventions
Medications for breathing, BP, and swelling management.
Increased Monitoring
Frequent assessments to ensure client stability.
Fluid Restriction
Limiting fluid intake to manage FVE.
Dietary Restriction
Reducing salt intake to prevent fluid retention.
Third Spacing
Fluid trapped in body areas, not contributing to equilibrium.
Common Sites of Third Spacing
Fluid accumulation in abdomen, causing ascites.
Pitting Edema
Swelling that leaves an indentation when pressed.
Non-Pitting Edema
Swelling that does not leave an indentation.
Albumin
Concentrated protein that draws fluid into vascular space.
Fluid Volume Deficit (FVD)
Condition with insufficient fluid in the body.
Signs of Third Spacing
Weight gain, decreased BP, increased HR.
Client Education
Informing clients about treatment reasons and participation.
Daily Weights
Regular monitoring to track fluid retention changes.
Safety Interventions
Using side rails for clients at risk of dizziness.
Fluid Imbalance Consequences
Can lead to low BP and organ damage.
Diffusion
Movement of molecules from high to low concentration.
Fluid Shifts in Dehydration
Fluid moves from blood vessels into interstitial spaces.
Assessment of Crackles
Indicates potential fluid volume excess in lungs.
Monitoring Intake and Output
Tracking fluid consumption and excretion for stability.
Physical Assessments
Evaluating signs of improvement or worsening condition.
Implementing PHCP Orders
Following provider's directives for patient care.
Documenting Changes
Recording patient progress or lack thereof.
Oxygen and Ventilation
Supportive measures for clients with FVE.