Bipolar Disorder
1/48
Earn XP
Description and Tags
Exam 1 - sem 3
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
Bipolar Epidemiology
Affects approximately 4.4% of U.S. adults with 89% of those cases being severe
Incidence equal between men and women
Average age of onset – age 25, and following 1st manic episode the disorder tends to be recurrent.
More frequent in higher socioeconomic class
6th leading cause of disability in the middle-age group in the U. S.
Bipolar spectrum
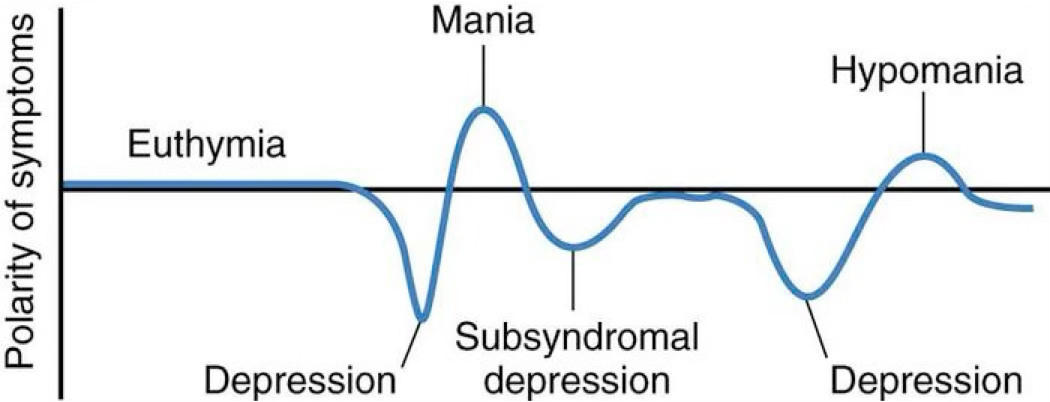
Bipolar disorder
Characterized by mood swings from profound depression to extreme euphoria
Intervening periods of normalcy
Delusions or hallucinations may be present
Mania
An alteration in mood that is expressed by feelings of elation, inflated self-esteem, grandiosity, hyperactivity, agitation, and accelerated thinking and speaking
Manic episode
Mood is elevated, expansive, or irritable
Marked impairment in occupational or social functions
Motor activity is excessive and frenzied
Psychotic feature may be present
Client may need to be hospitalized for safety of themselves and others
Patients may like this phase as they have increase energy and feels like they “take in the world”
Patient may refuse medications that will “bring them down”
Moving a lot → not eating → burning a lot of calories → not sleeping → losing weight
Hypomania
A mild form of mania
Symptoms are excessive hyperactivity, but not sever enough to cause marked impairment in social or occupational functioning or to require hospitalization
May come across as more irritable
May become mania if untreated
Types of Bipolar Disorder
Bipolar I
Bipolar II
Cyclothymic Disorder
Substance/Medication-Induced Bipolar Disorder
Bipolar Disorder due to another medical condition
Bipolar I and II
Diagnostic picture the same as for MDD expect the client must have a history of one or more manic/hypomanic episodes
Bipolar I Disorder
Client who is currently experiencing a manic episode or has a history of more than one manic episodes
May have also experienced episodes of depression
Psychotic or catatonic feature may also be noted
Bipolar II disorder
Recurrent bouts of major depression with episodic occurrence of hypomania
Cyclothymic Disorder
Chronic mood disturbance of at least 2 years duration, involving numerous periods of elevated mood that do not meet the criteria for a hypomanic episode and numerous periods of depressed mood of insufficient severity to meet criteria for Major Depressive Disorder (chronic low-level depression)
Substance and Medication-Induced Bipolar Disorder
The disturbance of mood is a direct result of physiological effects of a substance (ingestion of or withdrawal from a drug of abuse or a medication)
The mood disturbance may involve elevated, expansive, or irritable mood with inflated self-esteem, decreased need for sleep, and distractibility
Mood disturbances are associated with intoxication from substances such as alcohol, amphetamines, cocaine, hallucinogens, inhalants, opioids, phencyclidine, sedatives, hypnotics, and anxiolytics
A number of prescribed medications have been known to evoke mood symptoms
Predisposing factors of bipolar
Strong genetic vulnerability
Research suggests that bipolar disorder strongly reflects an underlying genetic vulnerability
Twin studies have indicated a concordance rate for bipolar disorder among monozygotic (identical) twins at 60 to 80 percent compared to 10 to 20 percent in dizogotic (fraternal) twins
Show that if one parent has a mood disorder, the risk that a child will have a mood disorder is between 10 and 25 percent
If both parents have the disorder, the risk is two to three times as great
Nursing Diagnoses for bipolar
Risk for Injury
Risk for Violence: To self or others
Imbalanced Nutrition: Less Than Body Requirements
Disturbed Sleep Pattern
Impaired Social Interaction
Nursing Interventions for bipolar
SAFETY FIRST! Remove hazardous objects
Reduce environmental stimuli
Limit group activities until appropriate
Observe client’s behavior and assess for behaviors that are a safety risk; manic patients can be impulsive
Maintain calm attitude
Be prepared to administer PRN medications
Offer high protein, high calorie finger foods for pacing client
Record I & O’s, lab values, weight
Set limits on manipulative behaviors – communicate these limits to all staff
Do not argue, bargain or try to reason with the client. Be direct
Follow through with consequences
Provide positive reinforcement for good behaviors
Protect the client’s privacy as much as you can (they like to walk around naked)
The nurse is prioritizing nursing diagnosis in the plan of care for a patient experiencing a manic episode. Number the diagnoses in order of the appropriate priority:
Disturbed sleep pattern AEB sleeping only 4-5 hours a night
Risk for injury r/t manic hyperactivity
Impaired social interaction AEB manipulation of others
Imbalanced nutrition AEB wt loss and poor skin turger
PUT IN ORDER
2, 4, 1, 3
Education for bipolar
Medication teaching
Importance of compliance
Educate the FAMILY about illness to help them understand
Give community resources
*They may be frustrated when they are doing everything right, but you aren’t getting better
What about kids with bipolar?
The biggest comorbidities are ADHD and conduct disorders, making it hard to diagnose
Because stimulants can exacerbate mania, it is suggested that medication for ADHD be initiated ONLY after bipolar symptoms have been controlled with a mood stabilizing agent
Bipolar disorder treatments
Individual Psychotherapy
Group Therapy
Family Therapy
Cognitive Therapy
ECT
Pharmacology
Mood Stabilizers
lithium (Lithobid)
Anti-epileptics/Anti-convulsants
carbamazepine (Tegretol)
lamotrigine (Lamictal)
valproate (Depakote)
Atypical Antipsychotics
olanzapine (Zyprexa)
quetiapine (Seroquel)
risperidone (Risperdal)
aripiprazole (Abilify)
haloperidol (Haldol)
Mood stabilizing drugs are used for what to treat bipolar?
Stabilizing the client’s mood
Preventing or minimizing the high and lows of character
Lithium
7-14 days to take effect
Need to get pregnancy test prior to start (manic episodes tend to start at 25 which is also prime child bearing age)
Check kidney/thyroid function
My be used with atypical antipsychotics (risperidone, olanzapine, aripiprazole)
Decreases agitation and restlessness until mood stabilizer kicks in
Lithium side effects and nursing interventions
GI DISTRESS – Give med with food or milk, advise client GI symptoms usually transient
FINE HAND TREMORS – Administer beta blocker such as Inderal. Educate client to report increase as could be signs of lithium toxicity
Mild tremors are normal, horse tremors are when we start to get concerned
POLYURIA, MILD THIRST –encourage adequate fluid intake
WEIGHT GAIN – Educate about the importance of living a healthy lifestyle
RENAL TOXICITY – Monitor I&O, assess and monitor BUN, creatinine, kidney function
GOITER & HYPOTHYROIDISM – Baseline T3, T4 and TSH levels and then annually. Educate about signs of hypothyroidism (cold, dry skin, decreased HR, weight gain. Administer levothyroxine (Synthroid)
CARDIAC — arrhythmias, hypotension, electrolyte imbalances-maintain adequate fluid and sodium intake
Therapeutic Lithium levels
0.6-1.2 mEq/L
Early indication of lithium toxicity
Less than 1.5 mEq/L
D, N, V, and polyuria
Muscle weakness, FINE hand tremors
Slurred speech
Hold the med and contact provider
Advanced indication of lithium toxicity
1.5-2.0 mEq/L
Mental confusion, poor coordination
COURSE tremors
Ongoing GI distress
Hold the med, contact provider
Excretion mat need to be promoted
Severe indication of lithium toxicity
2.0-2.5 mEq/L
Extreme polyuria of dilute urine
Tinnitus, seizure, blurred vision
Severe hypotension, respiratory complications
Administer an emetic or gastric lavage
Urea, mannitol, or aminophylline
to increase rate of excretion
Extreme indication of lithium toxicity
Greater than 2.5 mEq/L
Coma or death
May attempt hemodialysis
Administration of Lithium
Monitor plasma lithium levels Q 2-3 days until stable, then every 1 – 3 months
Lithium blood levels should be obtained in the morning, usually 12 from hours last dose
Administered 2 – 3 times a day due to short half life
Lithium contraindications
Pregnancy
Breastfeeding
Use cautiously in renal dysfunction, heart disease, sodium depletion, and dehydration
Lithium patient education
Take as ordered: double up on dose if dose missed - take within the day
BLOOD levels as ordered
Increased risk of toxicity in elderly
Do not use if pregnant
7-14 days to take effect
Take with food to decrease GI distress
Maintain fluid and sodium intake
NSAIDS: Increase renal reabsorption of lithium = toxicity: ASA is better choice
Diuretics: May cause toxicity (sodium decrease=lithium increase=toxic)
Signs and symptoms of toxicity
Adverse effects of carbamazepine (Tegretol)
Blood dyscrasias (leukopenia, anemia, thrombocytopenia)
Teratogenesis (congenital malformations in fetus)
Hypo-osmolarity/hyponatremia (watch in CHF)
Stevens-Johnson syndrome (rash)
all over body rash that is lethal if not treated
Also many drug/drug interactions with Tegretol
Adverse effects lamotrigine (Lamictal)
Stevens-Johnson syndrome (Begins with flu-like symptoms followed by a painful red or purplish rash that spreads and blisters. Top layer dies and sheds)
Double/Blurred vision
Dizziness
Headache
Nausea/Vomiting
Start low and go slow!
Adverse effects of valproic acid (Depakote)
GI → Give with food
Hepatotoxicity(liver function tests Q 2 months)
Pancreatitis
Thrombocytopenia (monitor platelet counts)
Teratogenesis/PCOS - consider alternative for females of child bearing years (toxic to fetus)
Decreases effectiveness of oral contraceptives: this is for all antiepileptics
CONTRAINDICATED in clients who have bone marrow suppression, bleeding disorders, liver disorders
Weight gain
Patient education of valproic acid (Depakote)
Baseline and routine monitoring of AST/ALT and LDH
Monitor for signs and symptoms of Steven Johnson Syndrome
Monitor Depakote level and ammonia levels regularly during treatment
Brain stimulation therapies
Electroconvulsive therapy (ECT)
Transcranial magnetic stimulation (TMS)
Vagus nerve stimulation (VNS)
What is electroconvulsive therapy?
ECT uses electrical current to induce brief seizure activity while the client is under anesthesia
Electroconvulsive Therapy (ECT)
Mechanism of action – biochemical – electrical stimulation results in significant increases in the circulatory levels of several neurotransmitters, such as serotonin, norepinephrine, dopamine, and possibly glutamate and gamma aminobutyric (GABA)
ECT indications
Major depressive disorder
Not responsive to medication
Risks of other treatments outweigh risks of ECT
Client is suicidal/homicidal
Client is depressed with psychotic features
Schizophrenia
Catatonic clients
Schizoaffective disorder
Acute manic episodes
Bipolar disorder with rapid cycling
Clients unresponsive to treatment with lithium and antipsychotic medications
ECT contraindications
There are no absolute contraindications, however must assess the client for conditions that could place the client at higher risk for adverse effects:
Cardiovascular disorders: recent MI’s, HTN, heart failure, arrhythmias. ECT increases stress on the heart during treatment
Cerebrovascular disorders: hx of stroke, brain tumor, subdural hematoma. ECT increases intracranial pressure during treatment
How ECT works
Typical course of treatment: 2-3 times a week for 6-12 weeks
Can be performed either inpatient or outpatient
Need to obtain informed consent
Pre—ECT workup: chest x-ray, labwork, EKG, spinal x-ray, EEG
Discontinue any benzodiazepine use as they can interfere with seizure process
ECT is not a permanent cure and may need follow up maintenance treatments
Usually on a muscle relaxer as well
ECT medication management for treatment
30 minutes prior to procedure: IM injection of atropine sulfate or glycopyrrolate administered to decrease secretions
At time of procedure: anesthesiologist administers a short-acting anesthetic (propofol) via IV bolus
A muscle relaxant (succinylcholine) is also administered to paralyze the client’s muscles during seizure activity to decrease risk for injury. This med also paralyzes the respiratory muscles so the client requires assistance with breathing and oxygenation
There might be memory loss from the day ECT happened
IV has to be hep-locked
ECT nursing mangment
Monitor VS and mental status prior and after ECT procedure
Assess the client’s and family’s understanding and knowledge of the procedure and provide teaching as necessary
Client will have a hep-lock/IV that will be used for treatments..need to assess and document
Clients are expected to become alert 15 minutes following ECT
ECT complications
Memory loss and confusion
Occurs immediately following the procedure and can persist for several hours.
Can have retrograde amnesia: loss of memory of events leading up to the procedure
Can persist for several weeks
ECT nursing actions
Provide frequent orientation
Provide a safe environment
Assist client with hygiene as needed
Monitor for reactions to anesthesia
Monitor VS and cardiac rhythms
Transcranial Magnetic Stimulation (TMS)
Currently approved for the treatment of Major Depressive Disorder
An electrical magnetic coil is placed on the scalp. Pulsed high-intensity current (MRI strength) passes through the coil, creating powerful magnetic fields that change the way brain cells function
Treatments last for 20-40 min a session and must be 5 days a week for appx 5-6 weeks
Limited insurance coverage, but improving. It is very expensive and results are inconclusive for treatment of depression
Unlike ECT, no seizure activity occurs
Minimal side effects v. ECT
Less invasive than ECT
Happens outpatient
TMS contraindications
Clients with cochlear implants, brain stimulators, medication pumps, pacemakers because the metal in the devices can interfere with treatment