HA PRELIMS WEEK 2
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
52 Terms
GENERAL STATUS SURVEY
- is the first part of the physical examination and begins the moment the nurse meets the client.
- It provides an overall impression of the client’s whole being.
- Observations to make:
o Physical development and body build
o Gender and sexual development
o Apparent age compared to reported age
o Skin condition and color
o Dress and hygiene
o Posture and gait
o Level of consciousness
o Behaviors, body movements, and affect
o Facial expression
o Speech
o Vital Signs
VITAL SIGNS
- (Pulse, Respirations, Blood Pressure, Temperature, and Pain) are the body’s indicators of health.
TEMPERATURE
- Normal Core Body Temperature: 36.5°C – 37.7°C (96.0°F – 99.9°F)
- Methods & Normal Ranges:
METHOD / ROUTE | NORMAL RANGE | PROCEDURE | INDICATIONS |
Oral | 35.9°C – 37.5°C (96.6°F – 99.5°F) | Place thermometer under the tongue to the right or left of the frenulum, deep in the posterior sublingual pocket. | • Sublingual area rich in blood vessels ❌ Not for patients with seizures ❌ Not for unconscious patients |
Tympanic (Ear) | 36.7°C – 38.3°C (98.0°F – 100.9°F) | Place probe gently at the opening of the ear canal for 2–3 seconds. | • Measures temperature near the eardrum • Close to hypothalamus (core control center) • Good for toddlers |
Axillary (Armpit) | 35.4°C – 37.0°C (95.6°F – 98.5°F) | Place thermometer in the axilla with arm held snugly against the body. | • Measures body heat released ✔ Infants ✔ Cooperative adults ✔ Sleeping patients • Usually 0.5°C (1°F) lower than oral |
Temporal (Forehead) | 36.3°C – 37.9°C (97.4°F – 100.3°F) | Scan thermometer across the forehead/temporal artery. | ✔ Sleeping patients ✔ Large group screening • Approximately 0.4°C (0.8°F) higher than oral |
Rectal | 36.3°C – 37.9°C (97.4°F – 100.3°F) | Insert thermometer gently into the rectum; never force. | • Closest to core temperature • Use only if other routes are not practical ❌ Hemorrhoids ❌ Low platelet count patients ❌ Neutropenic patients |
ORAL
TYMPANIC
AXILLARY
TEMPORAL
RECRAL
ROUTE FOR GETTING TEMPERATURE
ORAL
35.9°C – 37.5°C (96.6°F – 99.5°F) | Place thermometer under the tongue to the right or left of the frenulum, deep in the posterior sublingual pocket. | • Sublingual area rich in blood vessels ❌ Not for patients with seizures ❌ Not for unconscious patients |
TYMPANIC
36.7°C – 38.3°C (98.0°F – 100.9°F) | Place probe gently at the opening of the ear canal for 2–3 seconds. | • Measures temperature near the eardrum • Close to hypothalamus (core control center) • Good for toddlers |
AXILLARY
35.4°C – 37.0°C (95.6°F – 98.5°F) | Place thermometer in the axilla with arm held snugly against the body. | • Measures body heat released ✔ Infants ✔ Cooperative adults ✔ Sleeping patients • Usually 0.5°C (1°F) lower than oral |
TEMPORAL
36.3°C – 37.9°C (97.4°F – 100.3°F) | Scan thermometer across the forehead/temporal artery. | ✔ Sleeping patients ✔ Large group screening • Approximately 0.4°C (0.8°F) higher than oral |
RECTAL
36.3°C – 37.9°C (97.4°F – 100.3°F) | Insert thermometer gently into the rectum; never force. | • Closest to core temperature • Use only if other routes are not practical ❌ Hemorrhoids ❌ Low platelet count patients ❌ Neutropenic patients |
PULSE
- Definition: A shock wave produced when the heart contracts and pumps blood out of the ventricles into the aorta.
- How to Palpate: Use the pads of your two middle fingers and lightly palpate the radial artery on the lateral aspect of the client’s wrist.
- Normal Rate: 60–100 beats/min (Adults).
- What to Assess: Rate, Rhythm, Amplitude (0 to 3+ scale), and Elasticity.
GRADE | DESCRIPTION | CLINICAL SIGNIFICANCE |
0 (Absent) | Unable to palpate pulse | Cardiac arrest, shock, clot |
1+ (Weak / Diminished) | Easy to obliterate with light pressure | Weak heart, hypovolemia, dehydration |
2+ (Normal) | Obliterates with moderate pressure | Normal finding |
3+ (Bounding) | Unable to obliterate or requires firm pressure | Sepsis, fever, wide pulse pressure, anxiety, pregnancy |
RESPIRATIONS
- Normal Rate: 12–20 breaths/min.
o bpm – breaths/min
o cpm – cycles/min
- How to Measure: Observe the client’s chest rise and fall with each breath. Count for 30 seconds and multiply by 2.
o Tip: Monitor without alerting the client (e.g., keep fingers on the pulse site while counting respirations) to prevent the client from altering their breathing pattern.
BLOOD PRESSURE
- Definition: The pressure exerted on the walls of the arteries.
- Apparatus Used: Sphygmomanometer (aneroid, mercury, or electronic) and Stethoscope.
- Normal Values:
o Systolic: < 120 mmHg
o Diastolic: < 80 mmHg
SPHYGMOMANOMETER
Apparatus Used in Getting Blood Pressure
PREPARATION FOR GETTING BLOOD PRESSURE
- To get an accurate reading, you must eliminate factors that cause temporary BP spikes.
- The Environment: Room should be quiet and comfortable (not too hot/cold).
- The Client:
o Must rest for 5–10 minutes before the test.
o NO: Recent exercise, smoking (nicotine), alcohol, or a full bladder.
o NO: Talking during the measurement (by you or the client).
o Legs: Uncrossed and feet flat on the floor.
CUFF SELECTION
- Using the wrong size causes errors.
- The Rule: The rubber bladder inside the cuff should wrap around 80% of the arm.
o Too Small/Tight: = False HIGH reading.
o Too Large/Loose: = False LOW reading.
POSITIONING
PLACEMENT
ESTIMATION
MEASUREMENT
LISTENING
Steps for BP Measurement
POSITIONING
Posture: Client sits with back supported, legs uncrossed.
Arm: Upper arm exposed (remove tight clothing), supported at. HEART LEVEL, palm facing up
PLACEMENT
Apply Cuff: Wrap cuff snugly about 1 inch (2.5 cm) above the bend of the elbow (antecubital area).
Align: Ensure ARTERY MARKER on the cuff aligns with the BRACHIAL ARTERY
ESTIMATION (PALPATORY METHOD)
Purpose: Ensures you pump high enough and do not miss the systolic (top) number.
Palpate radial or brachial pulse.
Inflate cuff until pulse disappears
Note the number and ADD 30 mmHg → TARGET INFLATION PRESSURE.
MEASUREMENT (AUSCULTATORY METHOD)
Place stethoscope lightly over the brachial artery.
Inflate cuff to the target number from Step C.
Deflate SLOWLY at 2 mmHg per second.
LISTENING (KOROTKOFF SOUNDS)
SYSTOLIC (Top Number): First clear tapping sound (Phase I).
DIASTOLIC (Bottom Number): Sound disappears completely (Phase V).
Deflate fully and remove cuff.
PULSE PRESSURE
- Computation: Systolic BP minus Diastolic BP (Example: 120 − 80 = 40 mmHg)
- Normal Range: 30–50 mmHg
OXYGEN SATURATION
- Normal Values: 95 – 100%
- Measurement: Can be measured using a mobile monitoring system (e.g., “DINAMAP”) or Pulse Oximeter which often includes an oxygenation saturation detector.
PAIN
- is a universal experience but is unique to every individual.
- It is considered the “Fifth Vital Sign” and should be assessed with the same vigilance as temperature, pulse, respiration, and blood pressure.
o Primary Definition (Margo McCaffery): “_____ is whatever the experiencing person says it is, existing whenever he or she says it does.”
o Technical Definition: An unpleasant sensory and emotional experience associated with actual or potential tissue damage.
TRANSDUCTION
TRANSMISSION
PERCEPTION
MODULATION
4 process of pain detection (Nociception)
TRANSDUCTION
The conversion of a noxious (painful) mechanical, thermal, or chemical stimulus into an electrical signal (action potential) by nociceptors (nerve endings).
TRANSMISSION
The pain signal travels from the peripheral nerves to the spinal cord and then to the brain.
PERCEPTION
The brain recognizes, defines, and responds to pain — this is when the person becomes aware of the pain.
MODULATION
The body’s natural attempt to inhibit or alter pain impulses, such as through the release of endorphins.
ACUTE PAIN
CHRONIC PAIN
CANCER PAIN
Types of Pain By Duration/Etiology
ACUTE PAIN
Short-term, usually less than 6 months | Recent injury or surgery | Associated with “fight-or-flight” response → increased HR and BP; client often appears anxious or restless |
CHRONIC PAIN OR NONMALIGNANT PAIN
Persistent, lasts more than 6 months | Arthritis, fibromyalgia, back pain | Body adapts to pain; vital signs often normal; client may appear depressed or withdrawn rather than anxious |
CANCER PAIN
May be acute or chronic | Compression of peripheral nerves or meninges due to tumor growth, surgery, chemotherapy, or radiation | Often progressive and may require aggressive pain management |
CUTANEOUS PAIN
VISCERAL PAIN
DEEP SOMATIC PAIN
RADIATING PAIN
REFERRED PAIN
PHANTOM PAIN
TYPES OF PAIN BY LOCATION/SOURCE
CUTANEOUS PAIN
Skin or subcutaneous tissue | Sharp, burning pain (e.g., paper cut, burn) |
VISCERAL PAIN
Abdominal cavity, thorax, cranium | Often vague, dull, or cramping (e.g., menstrual cramps, appendicitis) |
DEEP SOMATIC PAIN
Ligaments, tendons, bones, blood vessels, nerves | Achy and tender (e.g., ankle sprain, fracture) |
RADIATING PAIN
Originates at a source and extends to other tissues | Pain is felt at the source and along the path |
REFERRED PAIN
Perceived away from the actual pain source | (e.g., left arm pain in myocardial infarction, shoulder pain from gallbladder disease) |
PHANTOM PAIN
Nerves of a missing, amputated, or paralyzed body part | Pain is perceived despite absence of the body part |
NEUROPATHIC PAIN
BOCICEPTIVE PAIN
TYPES OF PAIN BY CAUSE
NEUROPATHIC PAIN
Abnormal processing of pain messages due to damage to the nerves | Diabetic neuropathy, shingles | Burning, shooting, electric-shock-like |
NOCICEPTIVE PAIN
Normal response to damage to somatic or visceral tissue | Tissue injury, inflammation | Aching, throbbing, sharp |
7 DIMENSIONS OF PAIN
DIMENSION | DESCRIPTION | EXAMPLES |
Physical | The patient’s physiologic perception of pain | Bodily sensation of pain |
Sensory | The quality of the pain | Severity, location, quality |
Behavioral | Verbal and nonverbal behaviors related to pain | Grimacing, guarding, crying |
Sociocultural | Influence of social context and cultural background on pain expression | Cultural norms, family influence |
Cognitive | Beliefs, attitudes, and memories regarding pain | Pain expectations, past experiences |
Affective | Feelings and emotions resulting from pain | Anxiety, fear, depression |
Spiritual | Meaning or purpose attributed to the pain | “Is this punishment from God?” |
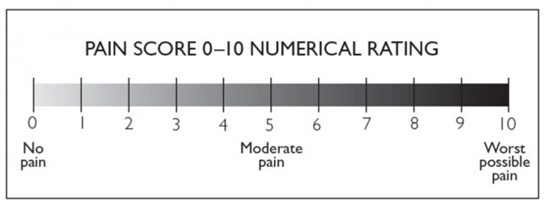
NUMERIC RATING SCALE (NRS)
- 0 (No Pain) to 10 (Worst Possible Pain). Best for cognitively intact adults.
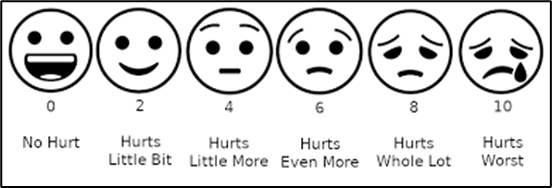
WONG-BAKER FACES SCALE
- Faces ranging from smiling (0) to crying (10). Best for children and clients with cognitive barriers.
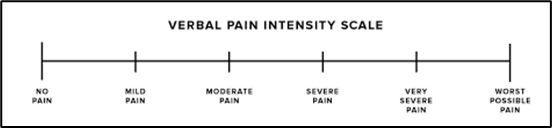
VERBAL DESCRIPTION SCALE
- Uses words (Mild, Moderate, Severe)
FLACC SCALE
- Face, Legs, Activity, Cry, Consolability
- Observational tool used for infants and non-verbal clients.
ITEM | 0 | 1 | 2 |
FACE | No particular expression or smile. | Occasional grimace, frown, withdrawn, or disinterested. | Frequent to constant frown, clenched jaw, quivering chin. |
LEGS | Normal position or relaxed. | Uneasy, restless, tense. | Kicking or legs drawn up. |
ACTIVITY | Lying quietly, normal position, moves easily. | Squirming, shifting back and forth, or tense. | Arched, rigid, or jerking. |
CRY | No cry. | Moans, whimpers, or occasional complaint. | Crying steadily, screams or sobs, frequent complaints. |
CONSOLABILITY | Content, relaxed. | Reassured by occasional touching, hugging, or being talked to, distractible. | Difficult to console or comfort. |
PATIENT BARRIERS
PROVIDER BARRIERS
BARRIERS TO PAIN ASSESSMENT
PATIENT BARRIERS
- Fear of addiction to pain medication.
- Belief that pain is a normal part of aging.
- Desire to be a “good” patient (not complaining).
PROVIDER BARRIERS
- Failure to believe the client’s report (Subjectivity).
- Focusing only on vital signs.
- Time constraints.
- Personal bias regarding drug-seeking behavior.
STOIC CULTURES
- May value self-control and hide pain; may not report pain unless asked directly.