Endocrine Labs ACS
1/178
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
179 Terms
Which hormones are studied under Anterior Pituitary studies?
Growth Hormone (GH)
Prolactin (PRL)
Follicle Stimulating Hormone (FSH) & Luteinizing Hormone (LH);
Thyroid Stimulating Hormone (TSH);
Adrenocorticotropic Hormone (ACTH).
FLAT PEG
What is the name of the hormones studied under Posterior Pituitary studies?
Antidiuretic Hormone (ADH) and Oxytocin (NOT measured)
What is the alternate name for Antidiuretic Hormone (ADH)?
Vasopressin.
What triggers the release of Antidiuretic Hormone (ADH)?
High plasma osmolality; Low blood volume or blood pressure.
Is Oxytocin typically measured in lab studies?
No.
What type of feedback mechanism controls Oxytocin release?
Positive feedback mechanism.
What are the target tissues for Oxytocin?
Uterus; Breast.
How do sufficient circulating levels of T3 and T4 utilize negative feedback?
Signals pituitary to decrease production of TSH; Signals hypothalamus to decrease production of TRH.
How does the endocrine system respond if T3 and T4 levels drop?
Signals release of additional TRH and TSH.
What are the primary functions of the thyroid gland?
Moderate growth; metabolism; and energy balance.
What causes primary HYPOthyroidism regarding T4/T3 production?
The thyroid gland under functions and is not producing enough T4 (and T3); resulting in low blood levels of T4 (and T3).
What is the resulting TSH level in primary HYPOthyroidism?
High blood levels of TSH; as signals are sent to the hypothalamus and pituitary to send more stimulating hormone.
What causes primary HYPERthyroidism regarding T4/T3 production?
The thyroid gland over functions; producing too much T4 (and T3); resulting in high blood levels of T4 (and T3).
What is the resulting TSH level in primary HYPERthyroidism?
Low blood levels of TSH; as signals are sent to the hypothalamus and pituitary to send less stimulating hormone.
Which thyroid test is the most sensitive first-line screening test?
TSH.
What is the general protocol if TSH is found to be in the normal range?
No further testing is required.
Under what circumstances are TSH and Free T4 (FT4) often ordered simultaneously?
When there is a high suspicion for thyroid disease.
When should Free T4 (FT4) be ordered if TSH results are available?
Order FT4 NEXT if TSH outside of reference range.
Why is Total T4 less reliable than Free T4 (FT4)?
Total T4 is affected by changes in thyroid-binding globulin concentrations (a transport protein).
Why is Free T4 (FT4) considered a better test than Total T4?
FT4 is a better reflection of how much thyroid hormone is available.
Why are FT3 levels generally not needed if T4 levels are adequate?
T4 converts to T3; therefore (generally speaking) FT3 levels correlate well with T4 levels.
When should T3 be ordered in addition to T4?
Order T3 as well if TSH is LOW.
Why is it necessary to check T3 and T4 when TSH is low?
TSH can be suppressed by either high FT4 and/or high T3; therefore; check both.
What is the most common cause of thyroid disease in relation to labs?
AntiThyroid Antibodies.
Which antibody is associated with Hashimoto Thyroiditis (HYPOthyroidism)?
Thyroid Peroxidase Antibodies (TPO Ab).
In what percentage of patients with Hashimoto's are TPO Ab present?
Approximately 90%.
Which thyroid condition is associated with Graves Disease?
HYPERThyroidism.
What percentage of patients with Grave’s Disease typically have associated antibodies?
Approximately 85%.
Besides TPO Ab; what are other AntiThyroid Antibodies?
Thyroglobulin Abs; TSH Receptor Abs.
What is the normal lab value range for TSH?
0.5 – 6 mcU/mL.
What is the normal lab value range for FT4?
0.8 – 2.8 ng/dL.
What components typically make up a complete Thyroid Panel?
TSH and FT4; plus FT3 or Total T3.
List three symptoms consistent with HYPOthyroidism.
Fatigue; cold sensitivity; weight gain; hair loss or dryness; brittle nails; dry skin; constipation; changes in menstruation.
List three symptoms consistent with HYPERthyroidism.
Weight loss; palpitations; dizziness; sweating; irritability; restlessness; heat intolerance; excessive hunger; insomnia; diarrhea; hair loss; tremor; changes in menstruation.
List three signs consistent with thyroid disease.
Thyroid goiter; enlargement; or nodules; tachycardia or bradycardia; hyper- or hyporeflexia; exophthalmos; elevated BP; hair; skin; and nail changes.
What is the primary function of Prolactin (PRL)?
Stimulate lactation.
What type of feedback mechanism controls Prolactin (PRL) production?
More complicated feedback mechanism.
Where is Prolactin production regulated?
By the hypothalamus.
What primarily controls Prolactin release?
Inhibition rather than stimulation.
What substance inhibits Prolactin release?
Dopamine.
What stimulates Prolactin production?
Thyrotropin Releasing Hormone (TRH); Prolactin releasing factors.
List three physiologic causes of high Prolactin (HYPERProlactinemia).
Pregnancy; Breastfeeding; Stress; Physical activity; Breast stimulation.
What is a common pathologic cause of Prolactin OVER-production (HYPERProlactinemia)?
Prolactin-secreting pituitary tumor (i;e; pituitary microadenoma).
List two types of medications that can cause hyperprolactinemia as a side effect.
Multiple psychotropics (e;g; antidepressants: SSRI; SNRI; antipsychotics: haloperidol; olanzapine…); sedatives; opiates; verapamil.
List two non-pituitary diseases that can cause hyperprolactinemia.
Other endocrine diseases (i;e; hypothyroidism; adrenal insufficiency); Non-endocrine diseases (i;e; chronic kidney disease; liver failure).
What is a rare cause of Prolactin underproduction?
Panhypopituitarism.
What is the typical normal range for Prolactin in a premenopausal female?
3.3 – 27 ug/L.
What is the typical normal range for Prolactin in a menopausal female?
2.7 – 19.6 ug/L.
What is the typical normal range for Prolactin in a male?
2.6 – 13.1 ug/L.
What special requirement should be followed when collecting Prolactin labs?
Collect as fasting lab in a.m.
List three symptoms that would prompt ordering a Prolactin level.
Amenorrhea with a negative pregnancy test; galactorrhea; hypogonadism; male and female infertility; erectile dysfunction; loss of libido.
What type of feedback mechanism controls Growth Hormone (GH) release?
Negative feedback mechanism.
What are the primary functions of Growth Hormone (GH)?
Accelerates growth of muscle; bone; and cartilage; Antagonizes the action of insulin on peripheral tissues; thereby decreasing glucose uptake and increasing glucose production.
How is Growth Hormone (GH) production regulated by the hypothalamus?
Production is regulated by the hypothalamus.
What is the GH Inhibitory Hormone that regulates GH production; and which hormone is more influential on production?
Somatostatin (aka; Growth Hormone Inhibitory Hormone); it is more influential on production.
What stimulates Growth Hormone production?
Growth Hormone Releasing Hormone (GHRH).
What condition results from GH OVER-production in children?
Giantism.
What condition results from GH OVER-production in adults?
Acromegaly.
What is the usual cause of GH over-production?
Usually from a pituitary tumor (i;e; pituitary macroadenoma).
What condition results from GH UNDER-production in children?
Dwarfism (small stature with normal body proportions).
What are potential causes of GH underproduction in children?
Hypothalamic or pituitary damage or hormone deficiencies.
What are potential causes of GH underproduction in adults?
Pituitary adenoma or irradiation.
What is a good initial screening test for Growth Hormone abnormalities?
Insulin-like Growth Factor-1 (IGF-1).
If Insulin-like Growth Factor-1 (IGF-1) is high; what provocative test is typically performed next?
GH Suppression test (Glucose Tolerance test).
If Insulin-like Growth Factor-1 (IGF-1) is low; what provocative test is typically performed next?
GH Stimulation test (Insulin Tolerance test).
When are GH levels actually checked in relation to provocative testing?
GH is checked after the GH stimulation test or GH suppression test.
What special requirement applies to GH stimulation and suppression tests?
They must be completed after fasting.
Utilize age specific ranges
A 45-year-old male notices an insidious need for larger shoe and ring sizes; along with slightly coarsened facial features. Which hormonal excess is suggested by bony overgrowth of the mandible and widening of the hands and feet?
EXCESS GH (Acromegaly).
List three symptoms of deficient GH in adults.
Less muscle mass; fatigue; increased body fat (esp; around waist); anxiety/depression; loss of libido; heat and cold intolerance.
What is the primary function of FSH in women?
Stimulate ovaries to make follicles (i;e; eggs) which produce Estrogen.
What is the primary function of LH in women?
Stimulates ovulation.
What is the primary function of FSH in men?
Promotes sperm production.
What is the primary function of LH in men?
Stimulates Testosterone production.
What stimulates the secretion of FSH and LH from the pituitary?
Gonadotropin Releasing Hormone (GnRH).
How do rising sex hormone levels (Estrogen; Progesterone; Testosterone) inhibit FSH and LH release?
By inhibiting the continued release of FSH and LH from the pituitary (and GnRH from the hypothalamus).
Why do FSH and LH lab values vary significantly in women?
Values differ based on prepubertal; premenopausal; menopausal; timing with menstrual cycle; pregnancy.
How do FSH and LH lab values vary in men?
Values differ based on prepubertal vs; post-pubertal.
List three contexts where FSH and LH are typically ordered.
Within the context of a work-up for infertility; amenorrhea (or oligomenorrhea); hypogonadism.
What other labs are often ordered alongside FSH and LH in an endocrine work-up?
Androgens (i;e; testosterone; DHEAS); Prolactin; TSH.
What type of feedback mechanism controls Antidiuretic Hormone (ADH) aka vasopressin?
Negative feedback mechanism.
What is the primary function of Antidiuretic Hormone (ADH)?
Regulates water balance in the body and sodium levels in the blood.
What is the pathological result of EXCESS ADH?
Syndrome of Inappropriate ADH (SIADH).
How does SIADH lead to hyponatremia?
Ongoing release of ADH without a stimulus causes kidneys to retain water; which leads to increased water in blood and dilutional HYPONatremia.
What is the difference between Diabetes Insipidus (DI) and Nephrogenic DI?
DI is deficient production of ADH; Nephrogenic DI is when kidneys become desensitized to ADH so do not respond appropriately.
What Urine Sodium (Na+) and Serum Sodium (Na+) pattern indicates SIADH?
HIGH Urine (Na+) (overlyconcentrated urine) and LOW Serum (Na+); indicating inappropriate conservation of water.
What Urine Sodium (Na+) and Serum Sodium (Na+) pattern indicates Diabetes Insipidus (DI)?
LOW Urine (Na+) and HIGH Serum (Na+); indicating releasing more water into the urine.
What Urine Osmolality and Serum Osmolality pattern indicates SIADH?
HIGH Urine osmolality and LOW Serum osmolality.
What Urine Osmolality and Serum Osmolality pattern indicates Diabetes Insipidus (DI)?
LOW Urine osmolality and HIGH Serum osmolality.
In the presence of which electrolyte abnormality should ADH labs be ordered?
Hyponatremia.. BUT NOT ALL HYPONATREMIA IS SIADH
A patient presents with confusion; lethargy; muscle weakness; and anorexia in the setting of hyponatremia. This presentation is consistent with which condition?
ADH excess (SIADH).
What is the potential outcome if severe ADH excess (SIADH) is left untreated?
Seizures; coma; CNS damage; and death.
List three classic symptoms of ADH deficiency (Diabetes Insipidus).
Polyuria; polydipsia; dehydration; fatigue.
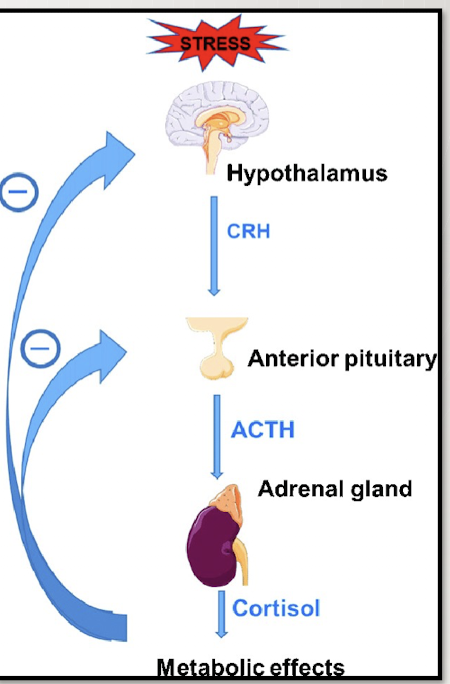
What type of feedback mechanism controls Adrenocorticotropic Hormone (ACTH)?
Negative feedback mechanism.
List two primary functions of ACTH.
Stimulates the production of Cortisol from the ADRENAL GLAND; Controls blood pressure and glucose levels under stressful conditions.
What hormone does the hypothalamus release to stimulate ACTH production?
Corticotropin-Releasing Hormone (CRH).
What triggers the release of CRH from the hypothalamus?
Emotional and physical stress (e;g; infection; trauma; exercise).
How do elevated Cortisol levels regulate ACTH and CRH production?
Elevated Cortisol levels then create a negative feedback to the hypothalamus and pituitary to decrease CRH and ACTH production.
What is the difference between Cushing Syndrome and Cushing Disease regarding Cortisol production?
Cushing Syndrome is EXCESS Cortisol production caused by the Adrenal gland (i;e; adrenal tumor); Cushing Disease is EXCESS Cortisol production caused by too much ACTH (i;e; pituitary microadenoma secreting ACTH).
What is the primary cause of Addison Disease?
Autoimmune disease that prevents adequate production of Cortisol (and Aldosterone).
What is the primary cause of Secondary Adrenal Insufficiency?
Decreased ACTH production (i;e; pituitary damage; long-term use of steroid therapy suppressing CRH and therefore ACTH).