biology mass transport
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
What is a single circulatory system?
Fish have them
heart -> gills --> body --> heart
What is a double circulatory system?
Mammals have them
heart --> body --> heart--> lungs --> heart
One circuit goes to the lungs to pick up oxygen (pulmonary circulation)
The other circuit carries the oxygen and nutrients around the body (systematic circulation)
What are the features of a double closed circulatory system?
Blood is confined to vessel and passes twice though the heart twice of each complete circuit
When blood passes through the lungs - pressure is reduced
blood is returned to the heart to boost its pressure before being circulated to the rest of the tissues
As a result, substances are delivered to the rest of the body quickly - maintains a high temperature and metabolism
What is an open circulatory system?
E.g. molluscs, invertebrates
Blood not in vessels
Trachea delivers 02 directly from environment to tissues
Body cavity filled with haemocoel (fluid)
What is a closed circulatory system?
E.g. vertebrates, a few invertebrates
Blood remains in vessels
Blood pumps at higher pressure and delivered faster
Waste removed more quickly
Tissues bathed in tissue fluid
Where is the heart?
Between the two lungs
Enclosed by pericardium
Pericardial fluid is secreted between them to aid movement
Pericardium protects the heart over expansion
What is the heart made of?
The walls of the heart are made of cardiac muscle (myocardium)
Only found in the heart
Never tires but can't tolerate lack of 02
What does the heart look like?
Contains two halves - two ventricles and two atriums split by a septum
What are the pressure changes like in the heart?
Atrium has a lower max pressure as only pumps blood into the ventricle - ventricle pumps to the whole body
closure of the valves is a passive process - it depends on the relative pressures on either side of the valve
How do the valves respond to pressure changes?
The atrioventricular valves close when the pressure in the ventricles is higher than in the atrium
They open when the pressure is higher in the atrium than the ventricle
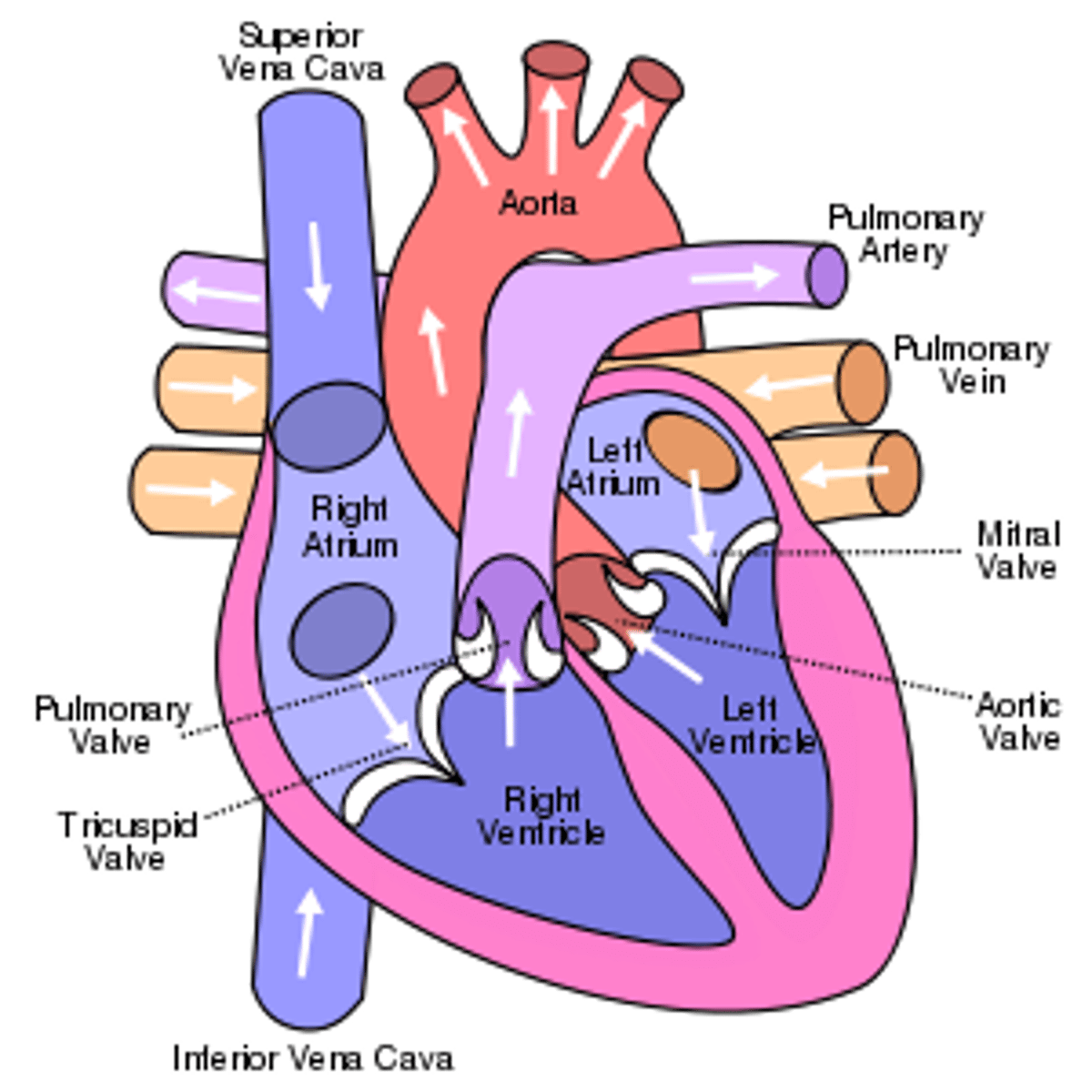
What is the pathway of blood on the right side?
body
vena cava
deoxygenated blood
atrium
tricuspid valve
right ventricle
pulmonary valve
pulmonary artery
lungs
pulmonary vein
What is the pathway of blood on the left side?
pulmonary vein
oxygenated blood
atrium
bicuspid valve
left ventricle
semi-lunar valve
aorta
body
What are the roles of the chambers in the heart?
Atrium - receives blood from veins
Ventricle - pumps blood into arteries
What do valves do?
Valves prevent backflow
When pressure in the ventricles exceeds that in the atrium in the bicuspid/tricuspid valves hut
This makes the first noise we hear with a stethoscope
tendinous chords attached to papillary muscles prevent valves turning inside out
Semi-lunar valves prevent backflow in the pulmonary artery and aorta
Closure of these makes the second noise of the heart beat (hence lub-dub)
How is oxygen linked to the cycle?
The heart requires a lot of oxygen and nutrients
Some oxygenated blood leaving the left ventricle goes directly to the heart through the coronary arteries
These branch many times to supply oxygen and nutrients throughout the cardiac muscle
When these get blocked a heart attack is likely and by-pass surgery required
What is systole?
Contraction of the heart
What happens in the atrial systole?
Atria contract, ventricles are relaxed
Blood moves from the atria into the ventricles along pressure gradient - AV valve open
Semi-lunar valves closed - to prevent backflow of blood into the ventricles (pressure lower in ventricles than arteries)
What happens in the ventricular systole?
Ventricle contracts, atria are relaxed
Blood is forced into arteries along pressure gradient - semi-lunar valves open
Bicuspid and tricuspid (AV) valves closed to prevent backflow of blood (pressure lower in atria than the ventricles)
What is diastole?
Relaxation of the heart
What happens during diastole?
Ventricles relax and atria are still relaxed
Atria fills with blood from the veins
Semi-lunar valves closed to prevent backflow of blood from the arteries (as pressure in the ventricles is lower)
What is cardiac output?
Stroke volume x heart rate
What is the need for a transport system?
Size
Metabolic activity
Surface area to volume ratio
Why does size affect the need for a transport system?
Larger organisms have body cells too far away from their surface to allow efficient exchange
A transport system allows for all body cells to be extremely close to a supply of nutrients for metabolic processes and to get rid of waste
Why does metabolic activity affect the need for a transport system?
Very active animals and those that maintain their body temperature (endotherms) require a good supply of glucose and oxygen for respiration (for muscle contraction and heat production) and to get rid of waste products like carbon dioxide
Why does surface area to volume ratio affect the need for a transport system?
The larger the organism the smaller the surface area to volume ratio
This means for each gram of body tissue in a larger organism, there is a smaller surface area for exchange compared to a smaller organism
What does an artery look like?
Lumen
Endothelium
Elastic fibres
Smooth muscle
Collagen fibres
How is the structure of an artery related to its function?
Narrow lumen to maintain high blood pressure
Thick layer of elastic tissue to allow artery to expand and recoil to maintain blood pressure
Thick layer of smooth muscle to allow blood vessel to constrict and dilate to maintain blood pressure
Thick layer of collagen and elastic fibres in outer wall to withstand the high pressure of the blood
Inner endothelial layer is folded - so that it can stretch when there is an increase in pressure
What does a vein look like?
Lumen
Endothelium
Elastic fibres
Smooth muscle
Collagen fibres
How is the structure of a vein related to its function?
Wider lumen to reduce resistance and allow the blood to flow easier
Thinner layer of elastic tissue as veins do not need to expand and recoil to maintain blood pressure
Thinner layer of smooth muscle as veins do not need to constrict and dilate to maintain blood pressure
Thinner layer of collagen and elastic fibres in outer wall as the blood is under very low pressure
Presence of valves to prevent backflow of blood
What does a capillary look like?
Red blood cell
Endothelium
Lumen
How is the structure of a capillary related to its function?
Very narrow lumen (7um) so red blood cells are squeezed through reducing the rate of flow and providing materials to move between the blood and tissue fluid
Capillary wall consists of single layer of flattened endothelial cells providing a short diffusion pathway
Gaps between the endothelial cells allow materials to enter and leave the blood (leaky)
What are the roles of arterioles?
Connect arteries to capillaries
Smooth muscle in their wall allows them to constrict and dilate - vasoconstriction and vasodilation
Vasoconstriction will reduce blood flow to the tissue e.g. reduced blood flow to the skin on a cold day to regulate temperature
Vasodilation will increase blood flow to the tissue e.g. increased blood flow to the muscles during exercise
What are the roles of the venules?
Connect capillaries to veins
Similar to veins they have walls consisting of a thin later of muscle, elastic and collagen
Wider lumen than arterioles to reduce resistance to blood flow
What are the factors aiding venous return?
venous blood pressure alone is too low to promote adequate blood return and is aided:
-respiratory pump - pressure changes created during breathing, sucks blood towards the heart by squeezing local veins -muscular pump contraction of skeletal muscles move the blood toward the heart
valves prevent backflow during venous return
What is the biconcave shape on the red blood cell for?
maximises surface area for gas exchange and allows the cells to be flexible enabling them to squeeze through narrow capillaries
What does the lack of nucleus do?
mature red blood cells don't have a nucleus, allowing more space for haemoglobin and increasing their oxygen-carrying capacity
What does the haemoglobin do?
this protein binds to oxygen in the lungs and releases it in the tissues
it makes up 95% of the dry mass of a red blood cell
what does the flexible membrane do?
it allows the cells to deform and pass through narrow blood vessels
what do the lack of organelles?
just like mitochondria and ribosomes there are no organelles
maximises space for haemoglobin
what's the tertiary structure of haemoglobin?
each polypeptide folded into a precise shape - important for its ability to carry oxygen
What's the quaternary structure of haemoglobin?
four polypeptide chains are linked to form an almost spherical molecule
each polypeptide has a haem group which contains a fe2+ ion, each ion can bind to a single oxygen molecule
4 oxygen per haemoglobin
What is loading/associating?
The process by which haemoglobin binds with oxygen is called loading or associating
in humans this takes place in the lungs
What is unloading/dissociating?
The process by which haemoglobin releases oxygen
In humans it takes place in the tissues
What is a high affinity?
Haemoglobin with this can take up oxygen more easily but release it less easily
What is a low affinity?
Haemoglobin with this can take up oxygen less easily but release it more easily
What's the affinity of haemoglobin for oxygen in a gas exchange surface?
high oxygen concentration
low carbon dioxide concentration
high affinity of haemoglobin for oxygen
results in oxygen being associated
What's the affinity of haemoglobin for oxygen in respiring tissues?
low oxygen concentration
high carbon dioxide concentration
low affinity of haemoglobin for oxygen
results in oxygen being dissociated
What is the partial pressure of o2?
a measure of oxygen concentration
high in the lungs
lower in body tissues such as the muscles
What does it mean that haemoglobins affinity for oxygen depend on the po2?
oxygen associates with haemoglobin to form oxyhaemoglobin where there's a high po2
oxygen dissociates from haemoglobin where there's a lower po2
What's the oxygen dissociation curve?
when haemoglobin is exposed to different partial pressures of oxygen, it does not bind in a linear fashion
the relationship between partial pressure of oxygen and percentage saturation is like a filament lamp
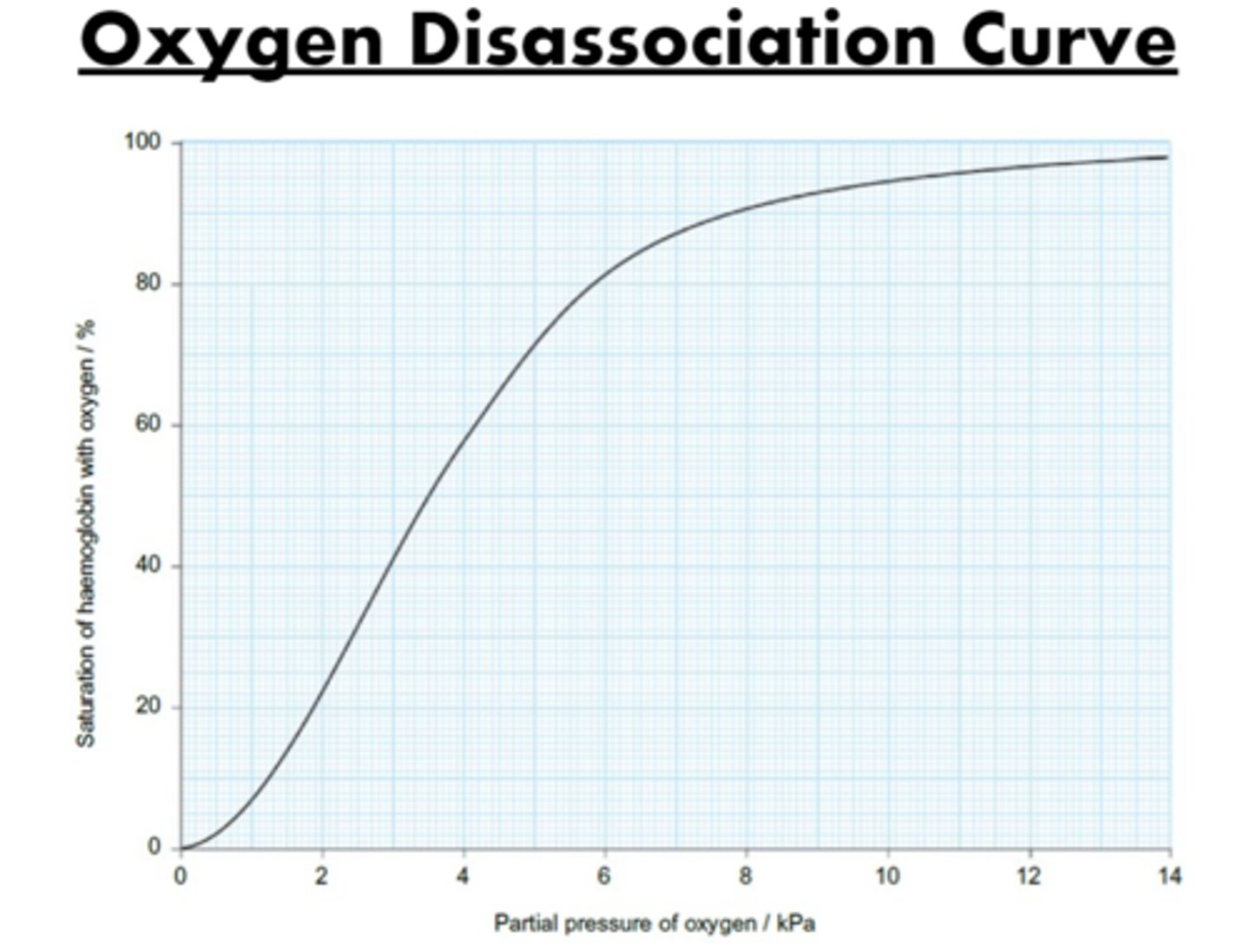
Why is the curve s shaped?
At lower pressures, there isn't a great deal of change in the saturation of the Hb
A small change in the po2 can result in a large change in the percentage saturation of the blood
At higher partial pressures there isn't a great deal of change in the saturation of the Hb
What are the molecules like, making it s shaped?
First molecule of 02 combines with an Hb and slightly distorts it, the joining of the first is usually quite slow
After the Hb has changed shape a little, it becomes easier and easier for the second and third 02 to join (positive cooperativity)
It flattens off at the top because joining the fourth 02 is more difficult due to probability
How does it have to do with the shape of haemoglobin?
It's a protein molecule with a specific shape - held together by those bonds in the tertiary structure
After oxygen binds it causes a slight shape change in haemoglobin as it distorts some of the bonds in the tertiary structure, allowing the second and third oxygen to bind easily - positive co-operativity
The 4th oxygen struggles to bind as a matter of probability (most binding sites are occupied now so it's less likely oxygen will collide with a binding site)
What does the capillary look like?
arteriole
lymphatic system
venule
body cells
capillary
blood flow through
What is the capillary bed?
Made up of a network of many branching capillaries, ensuring every body cell is extremely close to the blood for exchange of materials
What is the plasma?
Contains dissolved oxygen and nutrients, is forced through the capillary wall at the arteriole end of the capillary bed
What is the fluid formed called?
Tissue fluid
It bathes the cells so they can receive the nutrients required
What happens to the cells?
cells, platelets and large plasma proteins remain in the blood as they are too large to pass through the capillary wall
What happens at the venule end of the capillary bed?
Most of the tissue fluid is returned to the blood and contains the waste products from the cells
What happens to some of the tissue fluid?
It's removed by the lymphatic system and is eventually returned to the blood via a vein near the heart
What is tissue fluid?
A watery liquid that contains glucose, amino acids, salts and oxygen, supplying them all to the tissues
Tissue fluid formation aids the movement of nutrients from the capillaries to the tissues
Tissue fluid does not contain plasma proteins or any blood cells - these are too large to leave the capillary
What's the pressure like at the arteriole end?
Water and small molecules leave plasma due to high blood pressure or hydrostatic pressure
What's the pressure like at the venule end?
The hydrostatic pressure is lower than the osmotic effect of the plasma proteins in the capillary
The majority of the fluid is drawn back into the capillaries by osmosis
What is hydrostatic pressure?
The pressure created by a fluid pushing against the sides of its container/vessel
What is osmotic/oncotic pressure?
The pressure created by the osmotic effects f dissolved substances in a liquid (lowering of water potential)
What happens at the arteriole end of the capillary?
The blood entering the capillary is under higher hydrostatic pressure than the surrounding tissue fluid (5.2kPa compared to 1.3kPa)
Oncotic pressure created by solutes dissolved in both the blood and the tissue fluid (-2.9kPa compared to -1.2kPa)
The hydrostatic pressure has a greater effect and net movement is out of the capillary
Plasma and dissolved nutrients are forced out of the capillary
What is the hydrostatic pressure forcing small molecules out of the arteriole end opposed by?
hydrostatic pressure of tissue fluid outside of capillaries, preventing outward movement of liquids
Lower water potential of blood (due to plasma proteins), pulling water back into capillaries
BUT Hp is large enough inside that it overcomes these and has enough pressure to force small molecules out of capillaries, leaving cells and proteins behind (ultrafiltration)
What happens at the venule end of the capillary?
At the venule end of the capillary, the hydrostatic pressure of the blood is much lower and there is now less of a difference between the hydrostatic pressure of the blood and tissue fluid (1.8kPacompared to 1.3kPa)
Oncotic pressure now has a greater effect and net movement is into the capillary from the tissues
Tissue fluid returns to the capillary with dissolved waste from the cells, such as carbon dioxide, in it
What is the osmotic pressure pulling the fluid back in at the venule end opposed by?
Hydrostatic pressure of the fluid inside of the capillaries, preventing inward movement of liquids
BUT the hydrostatic pressure is GREATLY reduced by the time we reach the venule end
Therefore the osmotic pressure is greater and fluid can return to the venule
What is lymph formation?
Not all tissue fluid is reabsorbed back into the capillary network. However excess fluid does need to be moved away.
This fluid enters small, blind ended, lymphatic vessels.
The lymph vessels form a network throughout the body and drain back into the bloodstream via 2 ducts that join veins close to the heart.
What is oedema?
accumulation of excess tissue fluid
a failure to return excess interstitial fluid is oedema
edema is the swelling of ankles and feet
What does the lymph system contain?
jugular trunk
right lymphatic duet
brachiocephalic vein
bronchomediastinal trunk
intercostal trunk
internal jugular vein
thoracic duet
subclavian trunk
thoracic duct
intestinal trunk
lumbar trunk
lymphatic vessels
What are the main locations for the lymphatic system?
The main locations for fluid return to blood - right lymphatic duct and thoracic duct on left subclavian vein
This is because blood pressure is lowest here
What is lymph movement like?
Action of skeletal muscles
Respiratory movements
Smooth muscle in larger lymphatic vessels
Valves in lymphatic vessels