Immunology and Transplant Rejection: Key Concepts and Mechanisms
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
What did Peter Medawar's experiments prove?
Genetically identical (syngeneic) grafts are tolerated; genetically different (allogeneic) grafts are rejected.
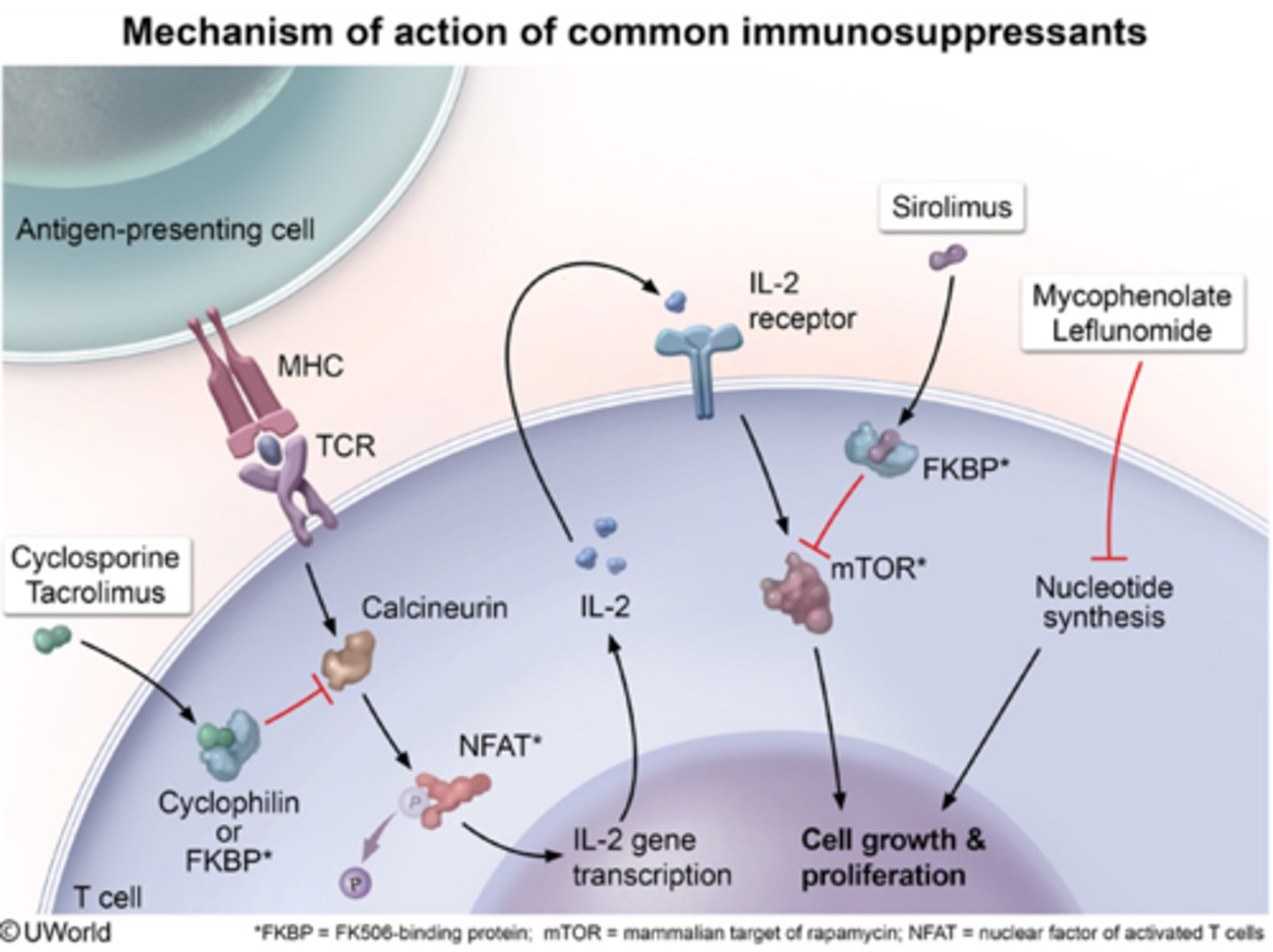
What immune mechanism drives graft rejection?
T-cell recognition of non-self MHC molecules.T cells identify the donor's MHC proteins as foreign "antigens" and mount a cellular attack.
What is 'First-set' vs. 'Second-set' rejection?
First-set: Primary T-cell-mediated rejection (~10 days). Second-set: Accelerated rejection (3-4 days) due to immunological memory.
What causes Hyperacute Rejection?
Pre-existing antibodies against donor antigens can cause immediate tissue damage.(in minutes to hours )
What defines Chronic Transplant Rejection?
Long-term, low-grade immune injury leading to progressive graft failure, often characterised by fibrosis and vascular narrowing over months or years.
Why can rejection occur even with 'Perfect' MHC matching?
Minor histocompatibility antigens can still differ between individuals and can activate a T-cell response..
What is Immunosurveillance?
The immune system's constant patrolling to detect and eliminate transformed (cancerous) cells before they can form a clinically detectable tumour.
Which immune cells are most important in tumour control?
Cytotoxic T cells (CD8+) and Natural Killer (NK) cells. T cells recognise specific tumour antigens, while NK cells target cells with "missing-self" (downregulated MHC).
What are Tumour-Infiltrating Lymphocytes (TILs)?
Immune cells found within the tumour microenvironment. A high density of TILs is generally a positive "biomarker" associated with an improved patient prognosis.
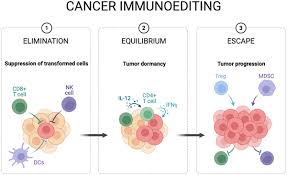
What is 'Immune Editing' and its three phases?
The process where immune pressure shapes tumour evolution: Elimination, Equilibrium, Escape.
What do RAG knockout mice demonstrate about cancer?
They develop spontaneous tumours, showing that adaptive immunity prevents cancer formation.
How do pathogens and tumours evade Cytotoxic T cells?
By down-regulating MHC Class I expression.
How does Mycobacterium tuberculosis (TB) survive inside Macrophages?
By inhibiting phagosome-lysosome fusion.. This prevents the bacteria from being exposed to the acidic, digestive enzymes meant to kill them.
What is the 'Granuloma' in TB pathology?
A structured wall of immune cells that contains the infection but prevents complete clearance.

What is the role of NuoG and KatG in TB evasion?
NuoG inhibits host cell apoptosis, and KatG detoxifies reactive oxygen species.
What triggers the initial Innate response to infection?
Recognition of PAMPs by host PRRs, triggering inflammatory cytokine production.