Comprehensive Biomaterials and Implant Fixation Strategies | Quizlet
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
What is biocompatibility?
The ability of a biomaterial to perform with an appropriate host response in a specific application without eliciting undesirable effects.
What are osteoblasts?
Bone forming cells.
What are osteoclasts?
Bone removing cells.
What does Wolff's law state?
When there's insufficient loading of the bone, bone resorption occurs, indicating loading-related remodeling.
What is stress shielding?
When a prosthesis takes over too much loading, leading to insufficient loading on the bone and subsequent bone resorption.
What is osteopenia?
A reduction in bone density as a consequence of the removal of normal stress from the bone.
What is proximal interface stress?
Low Young's modulus is better for reducing stress shielding but increases proximal interface stress, leading to potential loosening and fatigue failure.
What is small particle disease?
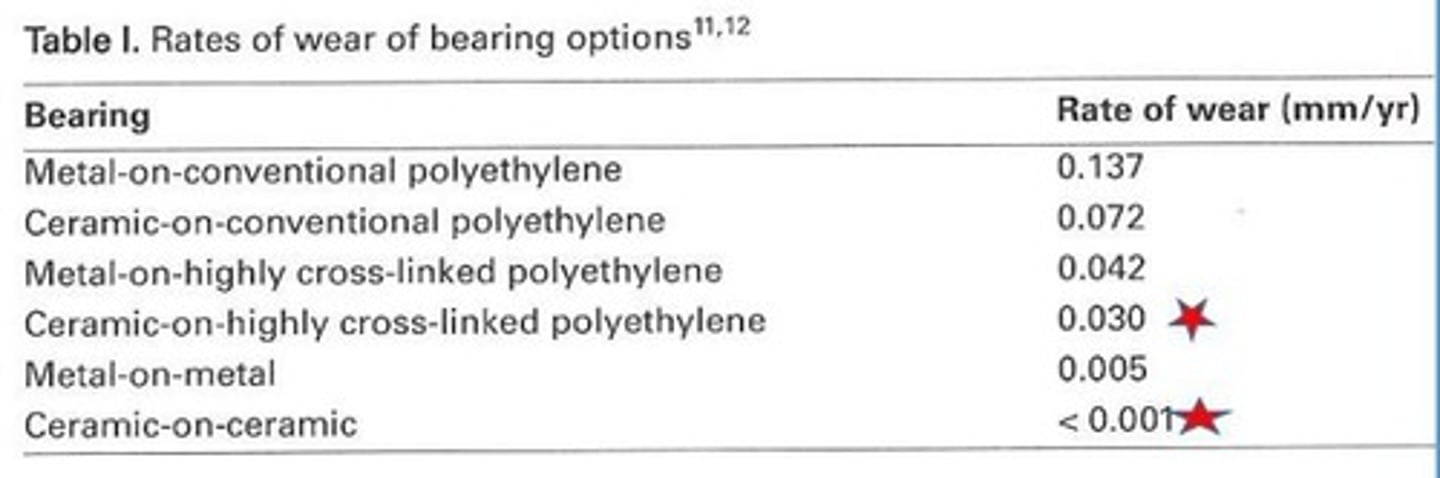
A condition where wear debris from articulating surfaces migrates to the bone implant surface, causing inflammatory responses and osteoclastic bone resorption.
What are polyethylene wear particles?
Particles measuring 0.5-1 micrometer that can lead to bone loss when produced at the articulating surface.
How do metal wear particles differ from polyethylene wear particles?
Metal wear particles are nano-particles and have a lower volume but a higher number compared to polyethylene microparticles.
What is corrosion in the context of biomaterials?
The reduction of structural integrity of implants due to chemical reactions, which can produce toxic corrosion products.
What is corrosion resistance?
The ability of a passivating metal surface to limit the rate of redox reactions at the implant/body fluid interface.
What is biotribocorrosion?
The synergistic effect of tribology (friction and wear) and corrosion, leading to greater material loss.
What is oxidative degradation?
A change in color and properties of materials, often due to exposure to oxygen, especially in UHMWPE liners.
What is pitting?
The formation of very small pores or depressions on a material's surface.
What is adhesive wear?
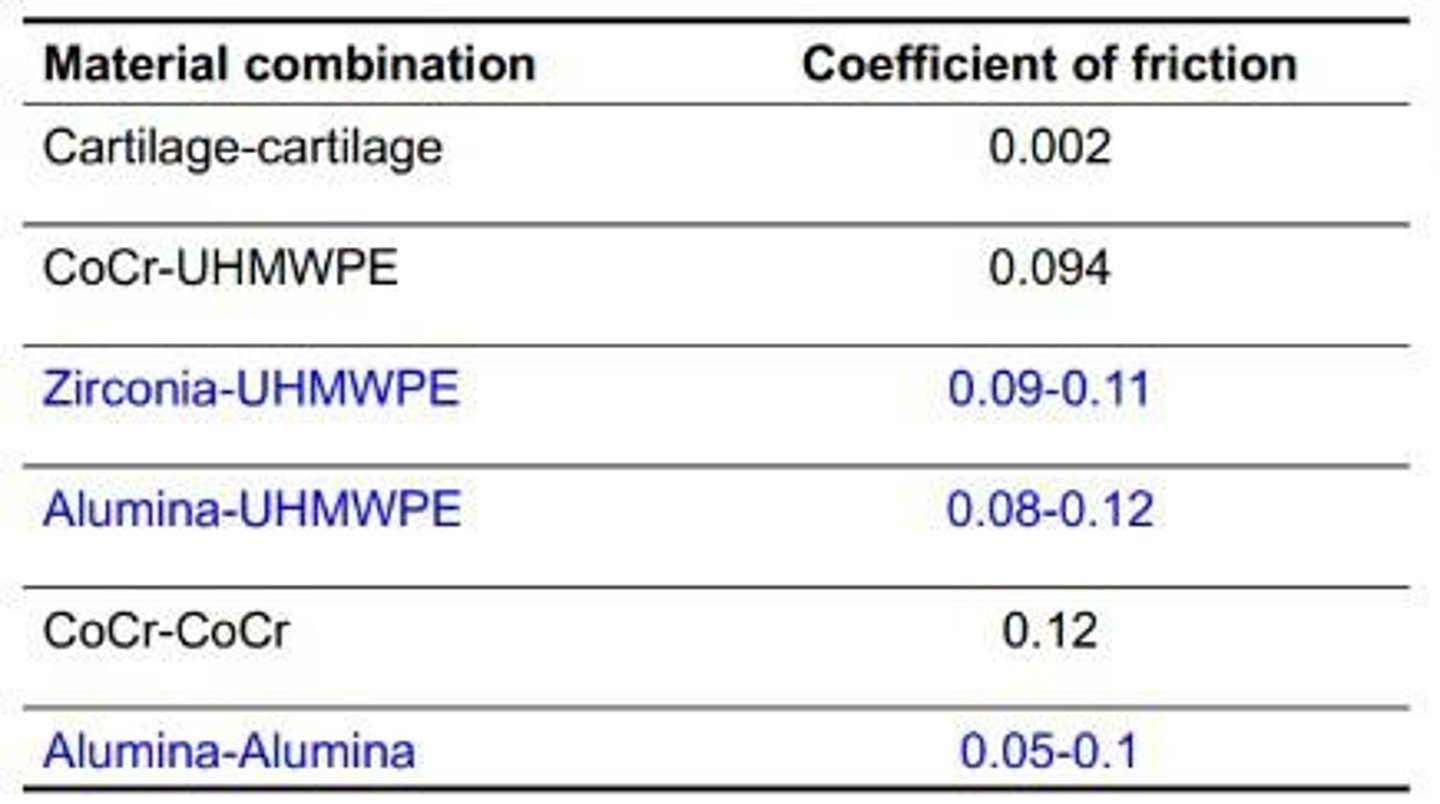
Localized surface damage associated with solid-state welding between two surfaces.
What is fatigue wear?
The breakage of small particles due to fatigue and crack propagation.
What is the lubrication ratio (labda)?
The ratio of lubricating film thickness to average roughness of both surfaces in contact.
What are the general characteristics of polymeric biomaterials?
They offer great versatility in chemistry and processing, are lighter than metals, but face concerns regarding long-term biocompatibility and wear debris.
What is Polymethyl Methacrylate (PMMA) used for?
It is used as bone cement but has limitations due to its low Young's modulus and potential side effects.
What are the advantages of Ultrahigh Molecular Weight Polyethylene (UHMWPE)?
It has a low friction coefficient and is used as a bearing material in total joint replacements.
What is the effect of gamma irradiation on UHMWPE?
It can lead to cross-linking that makes the material more brittle and susceptible to wear and delamination.
What role does Vitamin E play in UHMWPE?
It stabilizes UHMWPE, enhancing its mechanical properties and wear resistance.
What are the characteristics of ceramic biomaterials?
They are inert or bioactive, dense, hard, scratch-resistant, and have low friction and high wear resistance.
What are the general characteristics of ceramics used in biomedical applications?
Ceramics are brittle, very hard, have a very high Young's modulus, low tensile and bending strength, low fracture strength, and are difficult to process.
What is Alumina (Al2O3) used for in total hip replacement (THR)?
Alumina is used as the head and acetabular cup in THR due to its inertness and very high Young's modulus.
What are the properties of Zirconia (ZrO2) in biomedical applications?
Zirconia is inert, has lower Young's modulus, lower wear rates when combined with UHMWPE, and increased fracture toughness when stabilized with Y2O3.
What are Ca-based ceramics and their applications?
Ca-based ceramics, such as hydroxyapatite and tricalcium phosphates, are bioactive and used as synthetic bone substitutes and coatings on metallic devices.
What is the role of bio-glass in biomedical applications?
Bio-glass is designed to bond with bone, induce bone formation, and attract cells to stimulate bone cell development.
What are the general characteristics of metallic materials used in biomedical applications?
Metallic materials have high fracture toughness, heavy weight, low strength-to-weight ratio, and can be stable or biodegradable.
What is Stainless Steel (SS) and its use in biomedical applications?
Stainless Steel is an alloy of iron and carbon, used in temporary devices for bone healing, but has concerns regarding corrosion and high Young's modulus.
What are the advantages of Cobalt-based alloys (CoCr) in biomedical applications?
Cobalt-based alloys offer high fatigue strength, wear resistance, and a self-healing layer due to chromium, making them suitable for bearings and implants.
What makes Titanium (Ti) the golden standard for biomedical applications?
Titanium and its alloys have lower density, good biocompatibility, and are effective for fracture healing, but have poor wear resistance.
What is the significance of Nitinol (Ti-Ni) in biomedical applications?
Nitinol has good fatigue resistance, biocompatibility, and exhibits a shape-memory effect and superelasticity, making it useful for stents and bone plates.
What are the properties of Porous Tantalum (Ta) in biomedical applications?
Porous Tantalum is inert, corrosion-resistant, and mimics trabecular bone structure with high porosity, but has high manufacturing costs.
What is Oxinium and its application in biomedical devices?
Oxinium has a wear-resistant oxide layer, low Young's modulus, and is used in bearing parts and femoral components.
What are cemented implants and their characteristics?
Cemented implants use PMMA as cement, require a stiff material with high Young's modulus, and are typically used for older patients.
What is the Exeter concept in hip stem design?
The Exeter concept features a pointed stem with a highly polished surface that sinks into the cement mantle for optimal contact.
What are the characteristics of cementless implants?
Cementless implants require good sizing and fixation methods, such as mechanical locks or biological fixation through bone ingrowth.
What are the four phases of tissue-biomaterial interaction after implantation?
The four phases are haemostasis, inflammation, proliferation, and remodeling, occurring at the biomaterial interface.
What is the role of haemostasis in tissue-biomaterial interaction?
Haemostasis creates a natural scaffold for cell attachment, supports cell adhesion, and initiates cellular processes.
What happens during the inflammation phase of tissue-biomaterial interaction?
Cytokines activate inflammatory cells to remove debris and clean the site, releasing growth factors.
What is the significance of the proliferation phase in tissue repair?
During proliferation, growth factors activate the repair and population of biomaterials to restore lost or damaged tissue.
What occurs during the remodeling phase of tissue-biomaterial interaction?
In the remodeling phase, neo-tissue becomes functional tissue, completing the healing process.
What is the importance of surface chemistry in biomaterials?
Surface chemistry influences the absorption and adhesion of biomaterials, enhancing interaction with biological tissues.
What is a multi-factorial disease that involves environmental, genetic, and risk factors?
Atherosclerosis
What process occurs when endothelial cells are activated in atherosclerosis?
Receptors for monocytes are activated, leading to their migration into tissue and transformation into macrophages.
What do macrophages do in the context of atherosclerosis?
They phagocytize modified low-density lipoproteins (mLDL) and release cytokines and growth factors.
What is the consequence of plaque rupture in atherosclerosis?
It damages the endothelial cell layer, triggering coagulation and thrombus formation, which can lead to ischemia.
What characterizes stable plaque in atherosclerosis?
It has a thick fibrous cap and does not rupture, causing gradual narrowing of the lumen.
What characterizes vulnerable plaque in atherosclerosis?
It has a thin fibrous cap and is prone to rupture, potentially leading to myocardial infarction.
What is percutaneous transluminal coronary angioplasty (PTCA)?
A procedure where a balloon is inflated to compress plaque and widen the lumen.
What are the short-term failures associated with PTCA?
Elastic recoil of the vessel wall, acute thrombosis, and acute dissection.
What is restenosis?
The re-obstruction of a blood vessel after treatment, occurring in about 40% of patients post-PTCA.
What is the purpose of stents in vascular procedures?
To keep the vessel open after PTCA and prevent restenosis.
What is the role of Nur77 in smooth muscle cell (SMC) growth?
Nur77 inhibits SMC growth and promotes endothelial survival.
What are bare-metal stents (BMS)?
Stents that can become covered by cells, leading to in-stent restenosis.
What are the mechanical properties of stainless steel (316L) used in stents?
Good mechanical properties, corrosion resistance, but concerns include non-MRI compatibility and allergic reactions.
What advantages do CoCr alloys have over stainless steel in stent fabrication?
Higher tensile strength, ultra-thin strut fabrication, and excellent radial strength.
What is the shape memory effect in Nitinol stents?
Nitinol stents can expand and contract, allowing for self-expansion.
What is a drug-eluting stent (DES)?
A stent that releases medication to inhibit SMC proliferation and reduce the risk of restenosis.
What are biodegradable stents (BDS) designed to do?
Eliminate the need for re-dilation or removal surgery and reduce inflammatory responses.
What is the role of innate immunity in response to biomaterials?
It provides immediate protection without memory and attacks foreign materials.
What is adaptive immunity?
A response that adapts to challenges, recognizes cells, and has memory for future encounters.
What does the coagulation cascade involve?
Fibrin deposition and activation of blood platelets to close gaps in damaged endothelial cells.
What are neutrophilic granulocytes (PMN) and their role in immunity?
They are aggressive immune cells that phagocytose bacteria and are part of the first line of defense.
What is the function of monocytes/macrophages in the immune response?
They are long-lived cells that phagocytose pathogens and produce cytokines to attract other immune cells.
What are biofilms in the context of biomaterial-associated infections?
They are communities of bacteria that adhere to surfaces, grow, and can impair immune responses.
What is immunomodulation?
The adjustment of immune responses to prevent excessive inflammation or insufficient response.
What is the role of antimicrobial coatings on biomaterials?
To prevent bacterial colonization and adherence, reducing the risk of infection.
What are antimicrobial peptides (AMPs)?
They disrupt bacterial membranes and have a broad spectrum of activity against bacteria.