Diseases of the Cornea
1/175
Earn XP
Description and Tags
MT 2
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
176 Terms
Which nerve supplies the subepithlelial and stromal nerve plexus of the cornea?
First division (ophthalmic) of trigeminal nerve
Corneal diameter
Vertical = 11.5mm
Horizontal = 12mm
Where does the cornea get its nutrients?
It’s avascular, so the aqueous humor and tear film
Average central corneal thickness =
540 micrometers
5 Layers of Cornea
Epithelium: stratified squamous
non-keratinized
basal cells, wing cells, squamous surface cels
microplica & microvilli that assist in adhesion of the mucin layer of the tears
Corneal stem cells are located at the limbus
Will regenerate following trauma
Bowman layer: acellular superficial layer of stroma composed of collagen
Stroma: makes up 90% of the corneal thickness
Composed of regularly orientated layers of collagen fibrils = clear
Will not regenerate following trauma
Descemet membrane: composed of fine latticework of collagen that is distinct from the stroma
Has two bands, one develops in utero and one that is laid throughout life and serves as basement membrane for endothelium
Endothelium: monolayer of hexagonal cells that are responsible for deturgescence
Treatment for Recurrent Corneal Erosions (RCE)
Debridement: surgical intervention to remove irregular epithelium on active RCE
Phototherapeutic keratectomy-done with excimer laser
Stromal puncture: causes scar tissue which will anchor the epithelium to stroma
Bandage contact lens
Meesmann epithelial dystrophy (juvenile hereditary epithelial dystrophy)
rare
autosomal dominant mutation in gene responsible for producing epithelial keratin
Onset: first year of life
Symptoms: asymptomatic or blurry vision, glare, light sensitivity, discomfort (if cysts rupture onto epithelial surface-which does not occur until adolescence or adulthood)
Presentation: intraepithelial cysts and vesicles
small & filled with degenerated epithelial cell products
Cysts will extend towards the limbus but will be concentrated centrally and interpalpebrally
clear spaces surround the cysts
Complications: recurrent corneal erosions
Treatment:
asymptomatic = no tx
lubrication = for irritation if cyst rupture
debridement for RCE
Lamellar keratoplasty: if significant corneal opacification occurs and leads to reduced visual acuity (rare)
Meesmann epithelial dystrophy (juvenile hereditary epithelial dystrophy) Treatment
asymptomatic = no tx
lubrication = for irritation if cyst rupture
debridement for RCE
other RCE tx
Lamellar keratoplasty: if significant corneal opacification occurs and leads to reduced visual acuity (rare)
Reis-Bückler dystrophy
epithelial-stromal dystrophy
bilateral
onset: 1st decade, but not born with corneal signs
Bowman layer is replaced by connective tissue bands
Symptoms: more symptomatic than epithelial dystrophies
Visual complaints: blurred vision, photophobia and diplopia
Foreign body sensation and pain often due to RCE
Presentation: grey-white geographic subepithelial opacities
more dense central
denser w/ age and for a reticular pattern (cause stromal haze)
rod-like appearance
Corneal sensitivity will be reduced*
inc. corneal thickness
irregular astigmatism
How do you differentiate btwn Reis-Bückler dystrophy and Thiel-Behnke dystrophy?
electron microscopy
Theil-Behnke Dystrophy
epithelial-stromal dystrophy
bilateral
onset: 1st decade, but not born with corneal signs
Symptoms: more symptomatic than epithelial dystrophies
Visual complaints: blurred vision, photophobia and diplopia
Foreign body sensation and pain often due to RCE
less severe then Reis-Bückler
Presentation: curly fibers on electron microscopy
Predominantly affects the central cornea
Opacities will be less defined when compared to Reis-Bückler
Opacities will develop in a ring or honeycomb like pattern
Will not present with corneal irregularities or decrease corneal sensation
Reis-Bückler dystrophy and Thiel-Behnke dystrophy Complications
Recurrent corneal erosions in early childhood
Corneal opacifications (worse with Reis-Buckler)
Reis-Bückler dystrophy and Thiel-Behnke dystrophy Treatment
observation
Recurrent corneal erosion treatment: hypertonic salt solution or debridement
Lamellar keratoplasty with significant reduced visual acuity
Lattice dystrophy
Most common of the epithelial-stromal dystrophies
autosomal dominant
Onset: first decade
Assoc. with systemic amyloidosis
Pathophysiology: amyloid deposits accumulate between epithelial basement membrane and Bowman layer and the anterior stroma
Symptoms: blurred vision and pain with recurrent corneal erosions
Presentation: amyloid deposition in anterior stroma
Corneal deposits will be refractile dots that coalesce to form linear lines (makes lattice)
Over time corneal deposits will be surrounded by haze that will eventually fibrous = opacification
Affects central cornea
Reduced corneal sensitivity
Complications: recurrent corneal erosions, blurred vision (due to haze)
Treatment:
observation
RCE tx
lamellar keratoplasty
Granular dystrophy
Onset: first to second decade
1st = granular 1
2nd = granular 2
Pathophysiology: hyaline deposition
Two types: granular 1 and granular 2
Granular 1 Dystrophy
Symptoms:
asymptomatic early on
Eventually develop blurred vision, photophobia, glare and pain with RCE
Presentation: small well defined hyaline deposits (crumb like) in the anterior stroma
There will be a clear space in between the deposits; deposits become more confluent w/ progression
Opacities will extend posterior as the disease progresses
Reduction in corneal sensitivity
Complications: recurrent corneal erosions
Treatment:
observation
Phototherapeutic keratectomy or lamellar keratoplasty
When VA significantly dec
Granular 2 Dystrophy (granular-lattice dystrophy or Avellino dystrophy)
Combination of granular 1 and lattice dystrophy
Symptoms: blurred vision, pain with RCE
Presentation: discrete gray-white opacities made up of hyaline found in the anterior stroma combined with lines in posterior stroma
Deposits will be thorn-like, ring or stellate
Lattice lines develop latter but do not cross as they do in lattice
appear whiter & less refractile
Treatment: observation, treatment of RCE
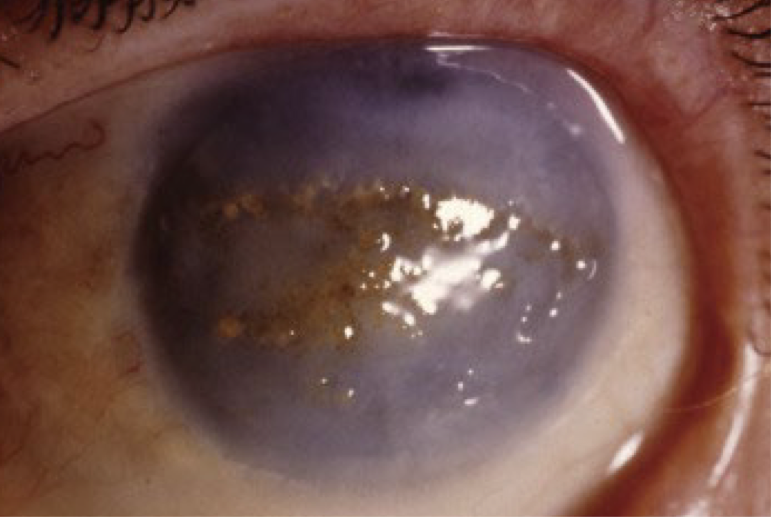
Macular dystrophy
stromal dystrophy
autosomal recessive
Common in Iceland and Saudi Arabia
Onset: first decade
Symptoms:
Blurred vision (significantly in 2nd-3rd decade)
pain w/ RCE
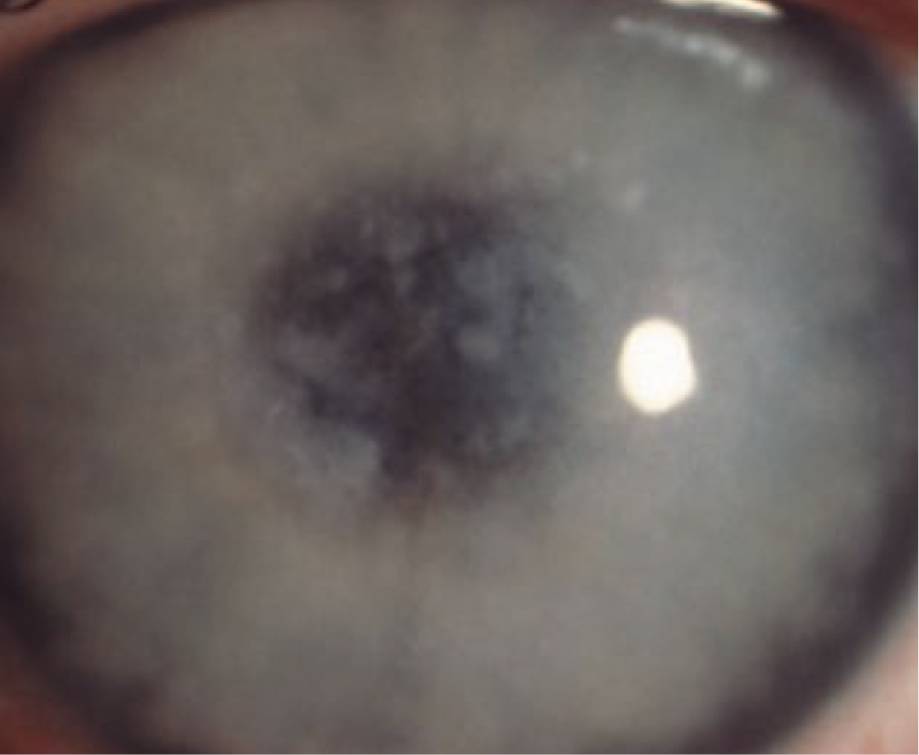
Presentation: deposits made up of mucopolysaccharides
Ill defined gray-white deposits that start in the central cornea and will migrate to limbus
Located in the anterior and posterior stroma
Entire cornea will appear cloudy as corneal collage fibrils are re-arranged
Eventually the collagen fibers will be replaced by fibrotic tissue and the cornea will thin
Decrease corneal sensitivity
Corneal edema will develop late in the disease process due to endothelial dysfunction
Complications: blurred vision, recurrent corneal erosions (uncommon)
Treatment
tx for RCE
Penetrating keratoplasty: recurrence is common
Macular Dystrophy Treatment
tx for RCE (uncommon)
Penetrating keratoplasty: recurrence is common
Schnyder (crystalline) corneal dystrophy
autosomal dominant
Onset: first decade with diagnosis coming in the second to third decade
Symptoms: glare and significant vision loss/change in 6th decade
Presentation: deposits are made up of lipid
Ring like opacity or central comma-shaped crystals
Subepithelial crystalline deposits and elevated blood lipid levels are seen in 50% of pts
Central corneal haze
Prominent arcus senilis (gradually moves central and causes haze)
Reduced corneal sensitivity
Treatment: phototherapeutic keratectomy and penetrating keratoplasty

Schnyder (crystalline) corneal dystrophy Treatment
phototherapeutic keratectomy and penetrating keratoplasty
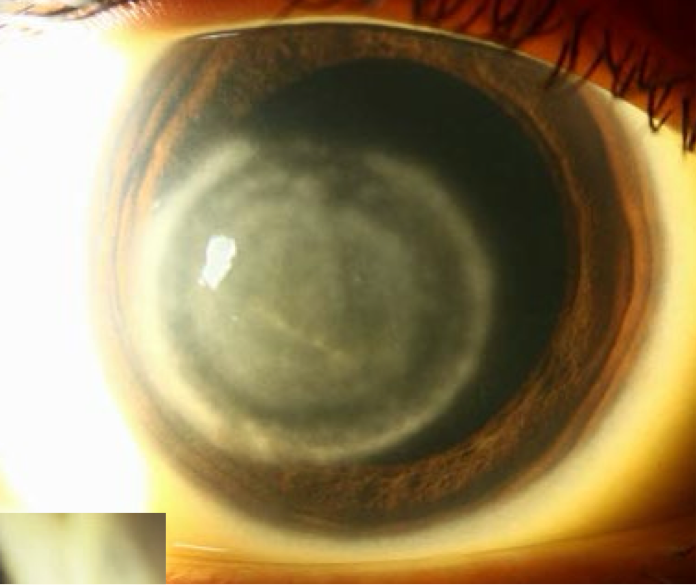
Fuch’s corneal dystrophy
endothelial dystrophy
Inheritance pattern: autosomal dominant
sporadic
More common in females
Onset: early onset presents in third decade
Late onset presents in sixth decade
Symptoms:
Blurred vision that is worse in the morning
Photosensitivity
Pain can develop with disease progression
Presentation: characterized by endothelial cell loss
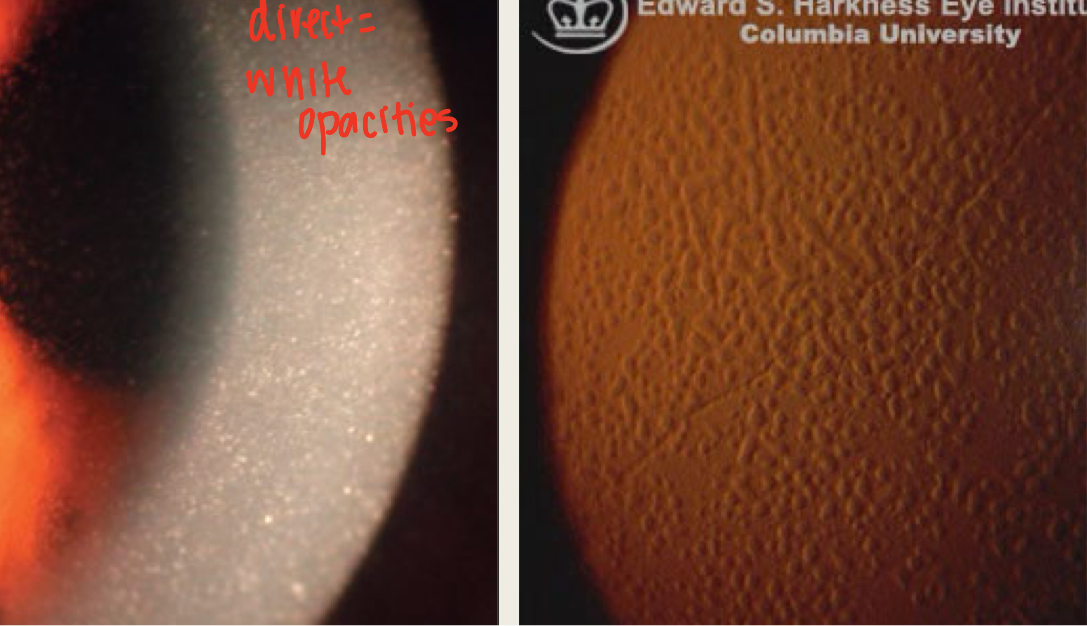
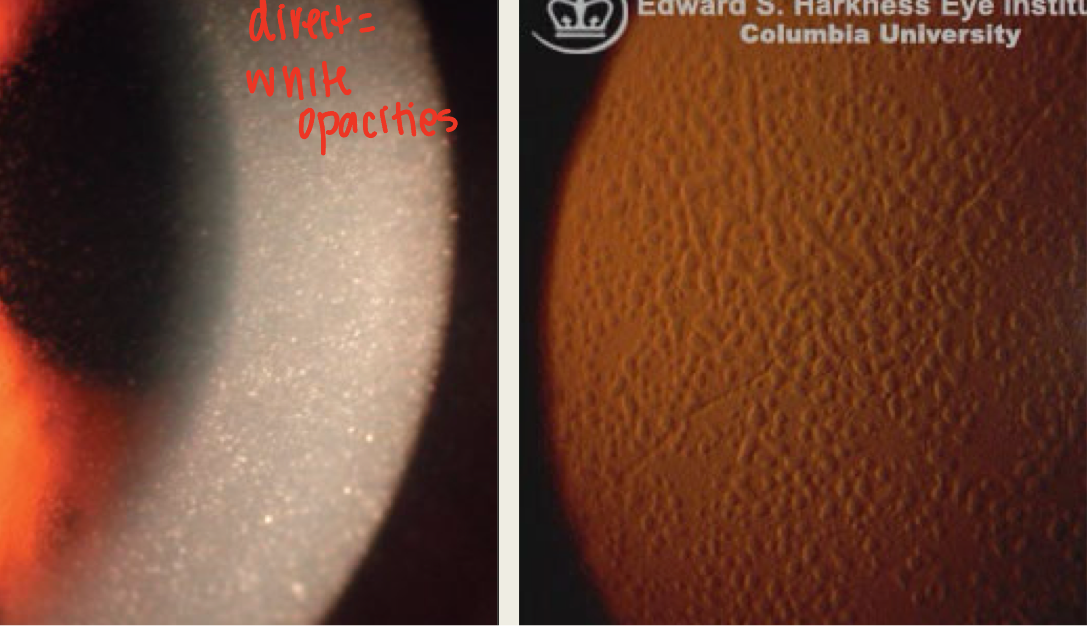
Stage 1: corneal guttata = thickening Descemet membrane that appears dark on specular reflection
starts central & spreads to periphery
usually asymptomatic
Stage 2: corneal guttata and corneal edema
guttata begin to coalesce
Endothelial cells start to change shape and enlarge
Corneal edema begins as endothelial cell count starts to decrease
edema = blurry vision that improves throughout day
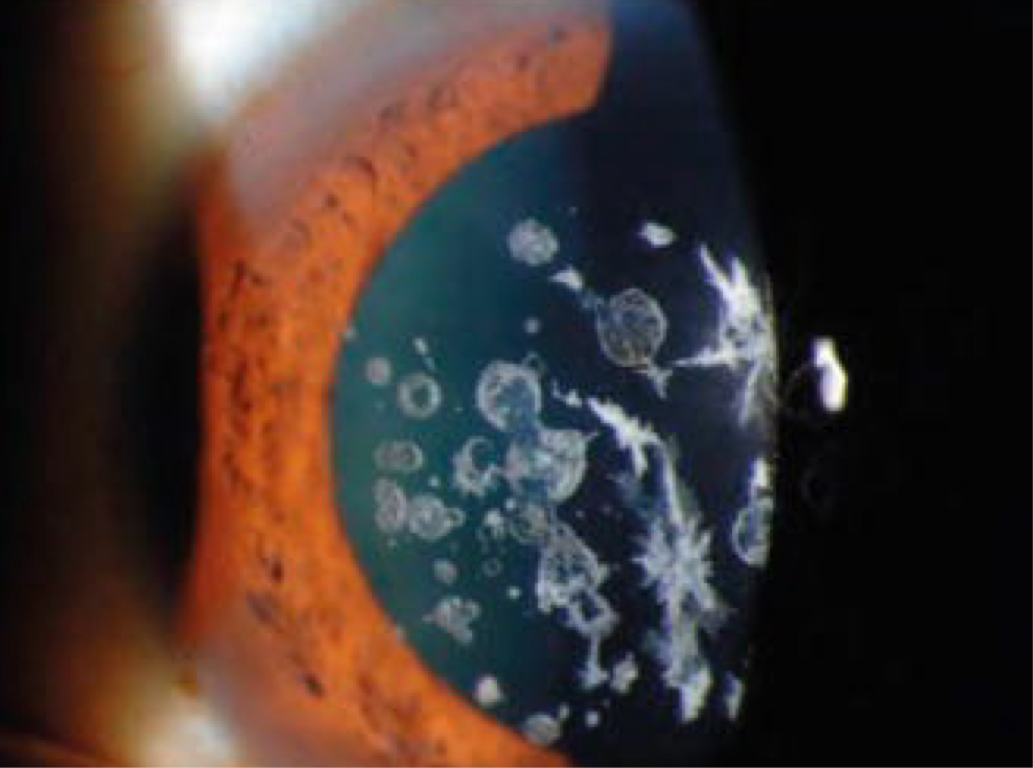
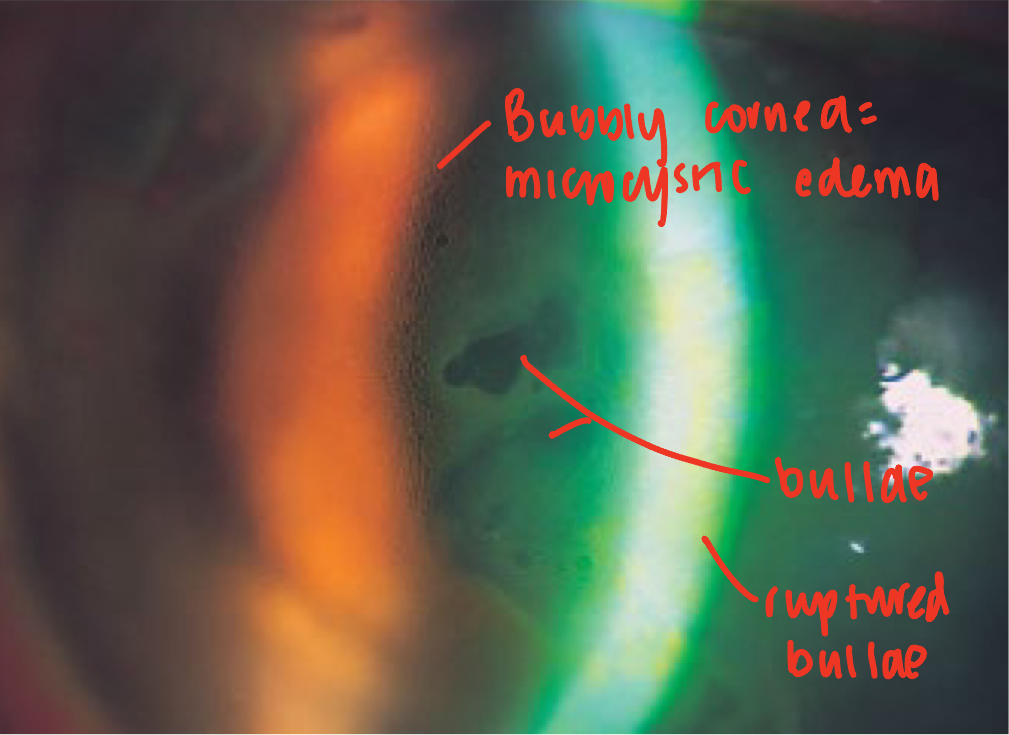
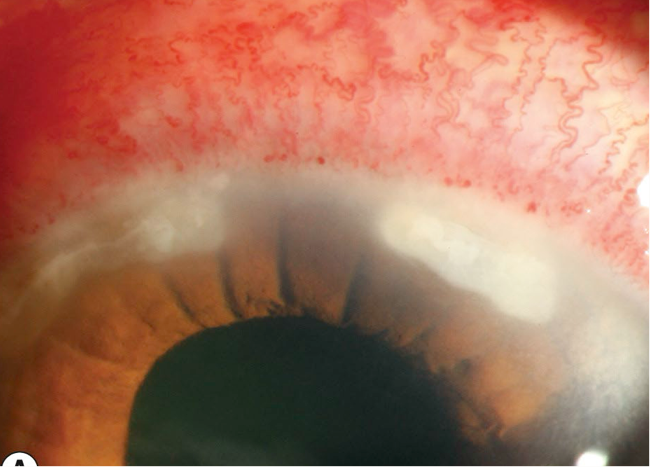
Stage 3: bullous keratopathy
edema causes epithelium to detach from basement membrane
Blister like lesion or bullae develop
Blisters can rupture leading to extreme pain
risk of corneal infection
Epithelial microcyst will be present
Stage 4: Corneal scarring and vascularization
Subepithelial fibrous tissue deposition
from chronic corneal edema
significant reduction in VA
minimal pain
Fuch’s corneal dystrophy Treatment
Stage 1 = observation
Stage 2 = hypertonic salt solution
Stage 3 = bandage contact lens for ruptured bullae
Topical antibiotic if concerned about secondary infection
DSAEK: Descemet membrane-stripping endothelial keratoplasty
DMEK: Descemet membrane endothelial keratoplasty
Stage 4 = PK: penetrating keratoplasty
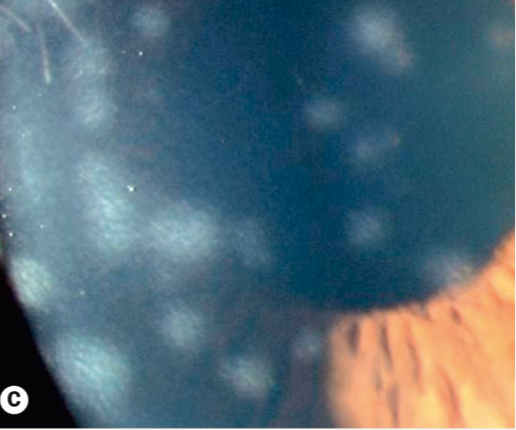
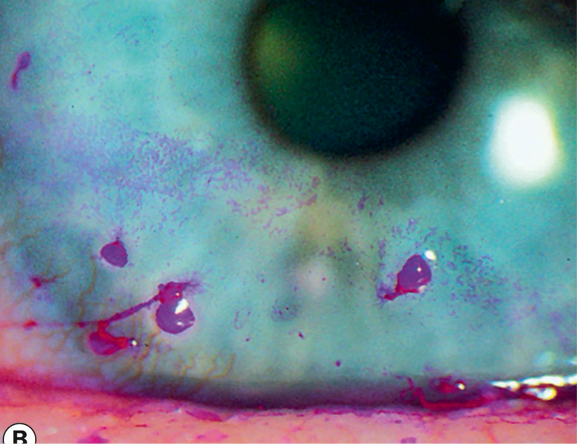
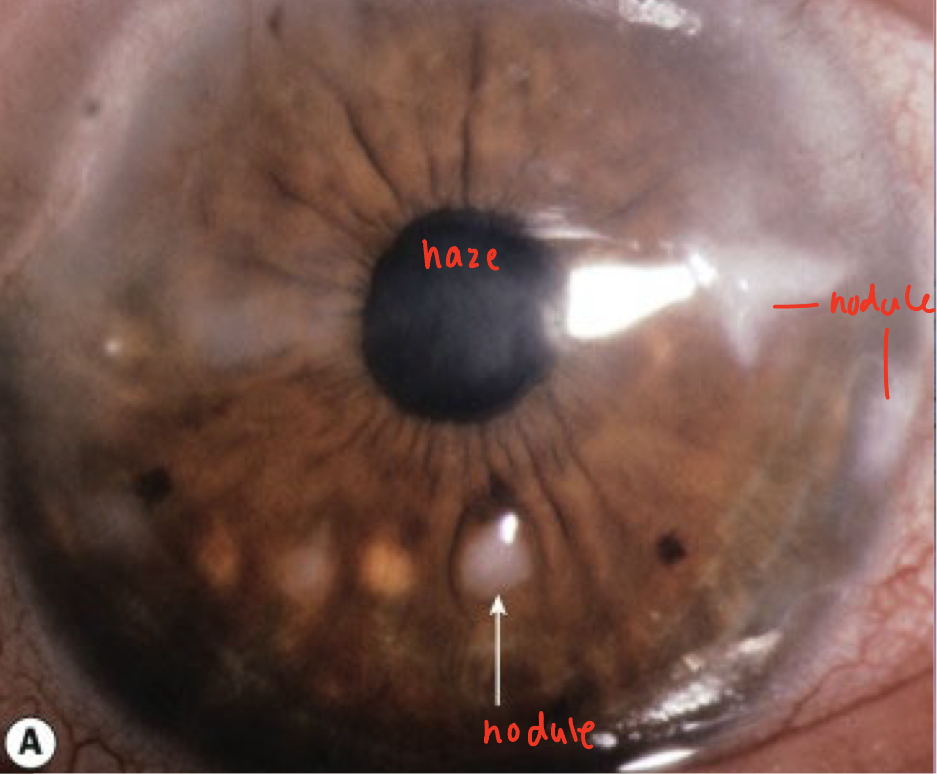
Posterior polymorphous dystrophy (PPMD)
endothelial
Inheritance pattern: autosomal dominant
Onset: first decade
Pathophysiology: abnormal endothelial cell proliferation
The abnormal proliferation causes an abnormal basement membrane to develop and thickening of Descemet membrane
Endothelial cells become more epithelial in nature-develop microvilli
Symptoms:
Asymptomatic
Blurred vision when corneal edema develops
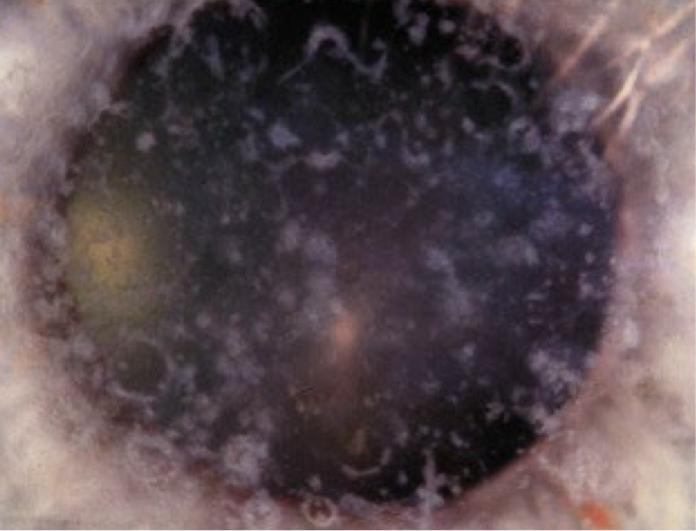
Presentation:
Geographic gray opacities: least common finding
at lvl of Descemet
stromal haze adjacent
May have whirl like pattern
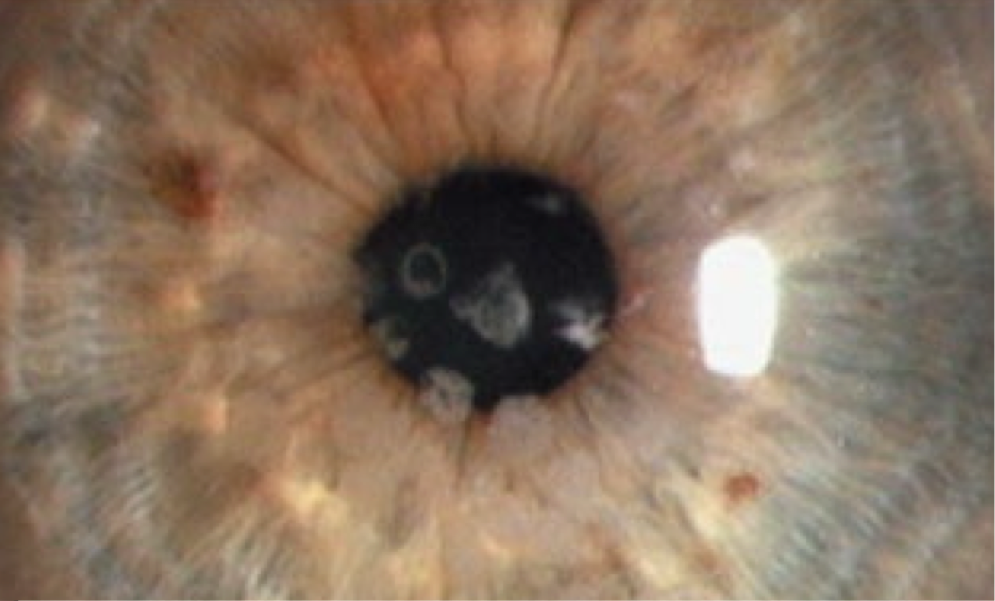
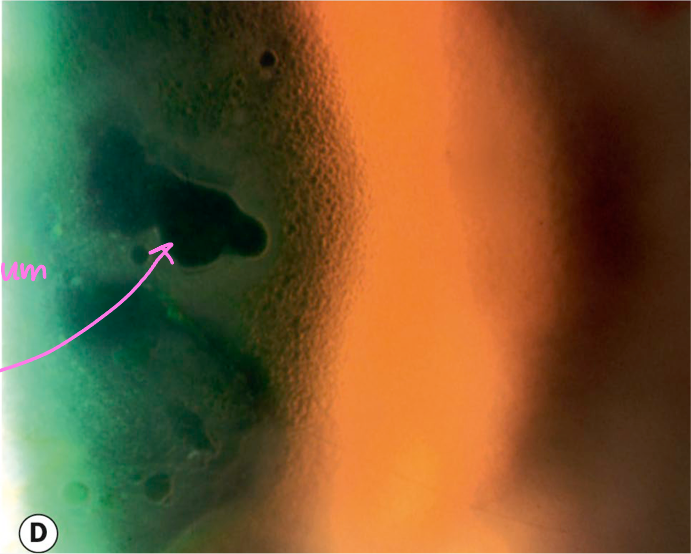
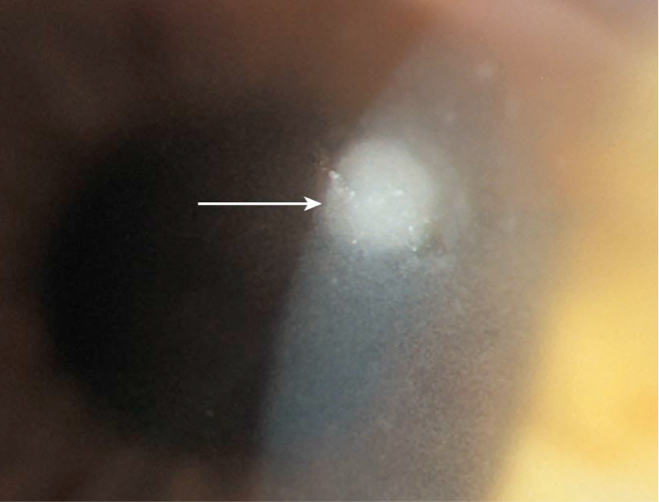
Vesicular lesions: pathognomonic for PPMD
Appears as circular or oval transparent cysts with gray halo-gives a blister appearance
in a line or clusters
Horizontal bands in inferior cornea
Range from 2-10mm in length
Will have a parallel scalloped or flaky edge
Complications: secondary glaucoma or iris abnormalities (migration of endothelial cells causes angle closure)
Treatment:
Observation
Treatment of corneal edema similar to Fuch’s
Treatment of complications

Posterior polymorphous dystrophy (PPMD) Treatment
Observation
Treatment of corneal edema similar to Fuch’s
Treatment of complications
Corneal degeneration
slow and steady deterioration of corneal tissue
occurs in the periphery
Will affect several layers of the cornea
Unilateral and asymmetric
Occurs in older patients
No genetic component
Corneal degenerations share which of the following characteristics with corneal dystrophies?
Both are non-inflammatory
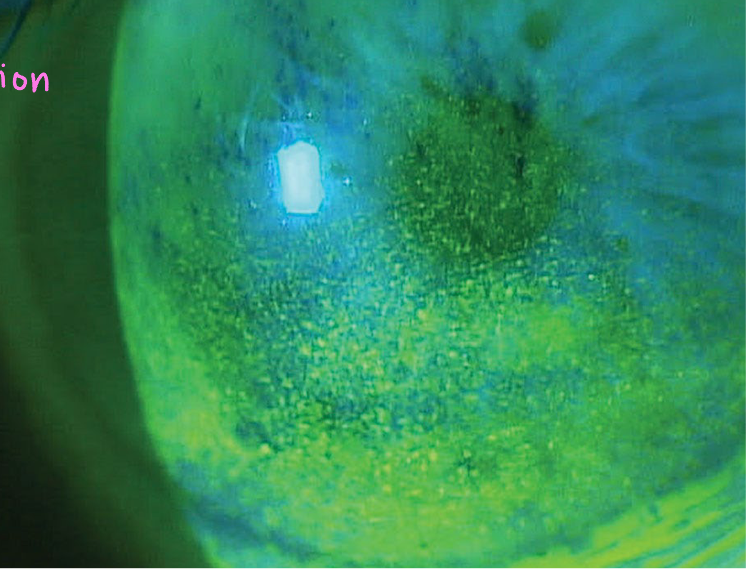
Punctate epithelial erosions
tiny epithelial defects
stain with fluorescein or Lissamine Green/Rose Bengal
Early sign of corneal compromise
Can be located throughout the cornea (area helps determine cause)
Superior PEEs=
vernal keratoconjunctivitis, SLK, floppy eyelid
Interpalpebral PEEs=
dry eye
Inferior PEEs=
chronic blepharitis
Diffuse PEEs=
viral infection
Central PEEs=
contact lens related
Punctate epithelial keratitis (PEK)
swollen epithelial cells
Presentation: granular, opalescent swollen epithelial cells
stains with Lissamine Green/Rose Bengal; variable with fluorescein
punctate staining will be seen
Seen with: viral infections, Thygeson superficial punctate keratitis
Subepithelial infiltrates
non-staining inflammatory cells
unclear margins
Located below epithelium
Inflammatory cells are released from limbal vasculature
Seen with: adenoviral keratoconjunctivitis, HZO, marginal keratitis
Filaments
Mucus strands attached to the cornea
Will attach where there is an epithelium break
Tear debris will surround mucus strand
Commonly seen with dry eye, SLK
Superficial punctate keratitis
non-specific round corneal epithelial disruption of round morphology
commonly seen w/ corneal disease
has inflammation with it
only difference from PEEs
Epithelial edema
swelling of cornea
Will present as small epithelial vesicles
seen w/ endothelial compromise
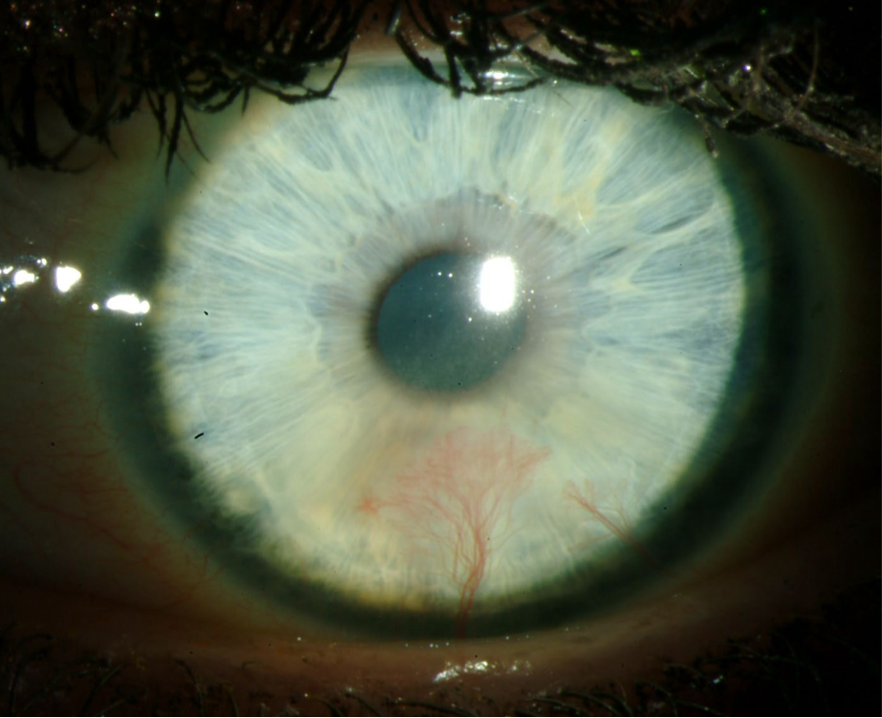
Corneal Neovascularization
blood vessel growth onto cornea at limbus
Sign of chronic ocular irritation or hypoxia
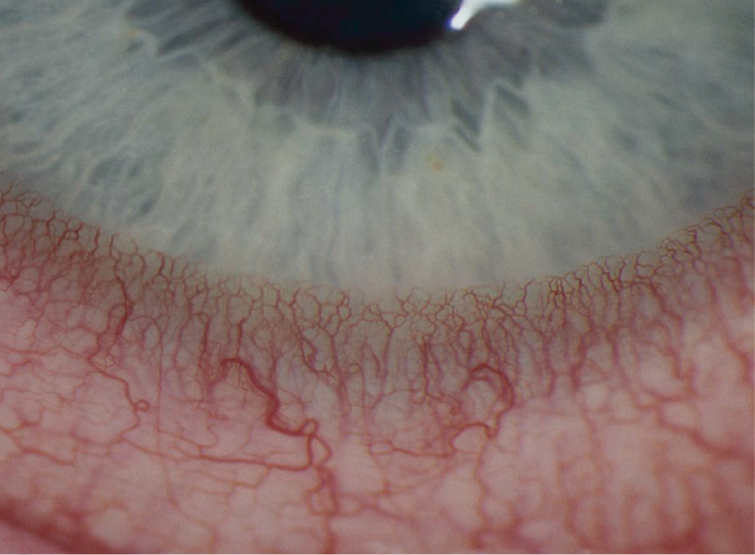
Pannus
superficial neovascularization with subepithelial degeneration

Deep Infiltrates of cornea
inflammatory cells, cellular debris, and tissue necrosis located in the anterior stroma
appear white to grey
conj. hyperemia will also be present
Corneal Ulceration
excavation of corneal tissue w/ epithelial defect
seen with deep infiltrate
Melting of cornea
Tissue disintegration
in severe corneal disease
Corneal infiltrate may or may not be seen
Folds in Descemet
dark, deep-appearing, criss-cross lines in posterior stroma
cornea can appear hazy d/t corneal edema
commonly seen after surgery
Breaks in Descemet
from corneal enlargement (infantile glaucoma), birth trauma (forceps), or keratoconus
Descemetocele
protrusion of Descemet membrane into the anterior layers of the cornea
seen w/ severe ulceration
Corneal dystrophies
group of slowly progressive, usually bilateral corneal opacification that may cause decreased vision and discomfort
typically only affect one layer of cornea
Starts out in the center of the cornea and migrate to the periphery
Non-inflammatory
Genetic with majority being autosomal dominant
Occurs in younger patients
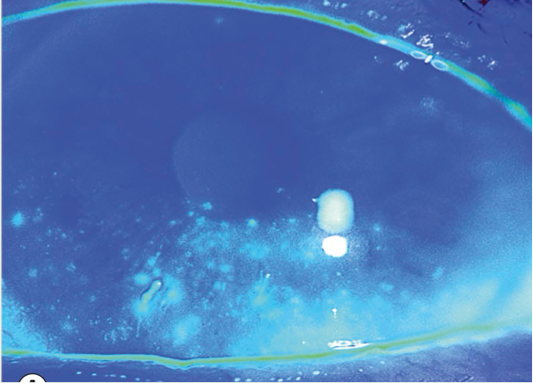
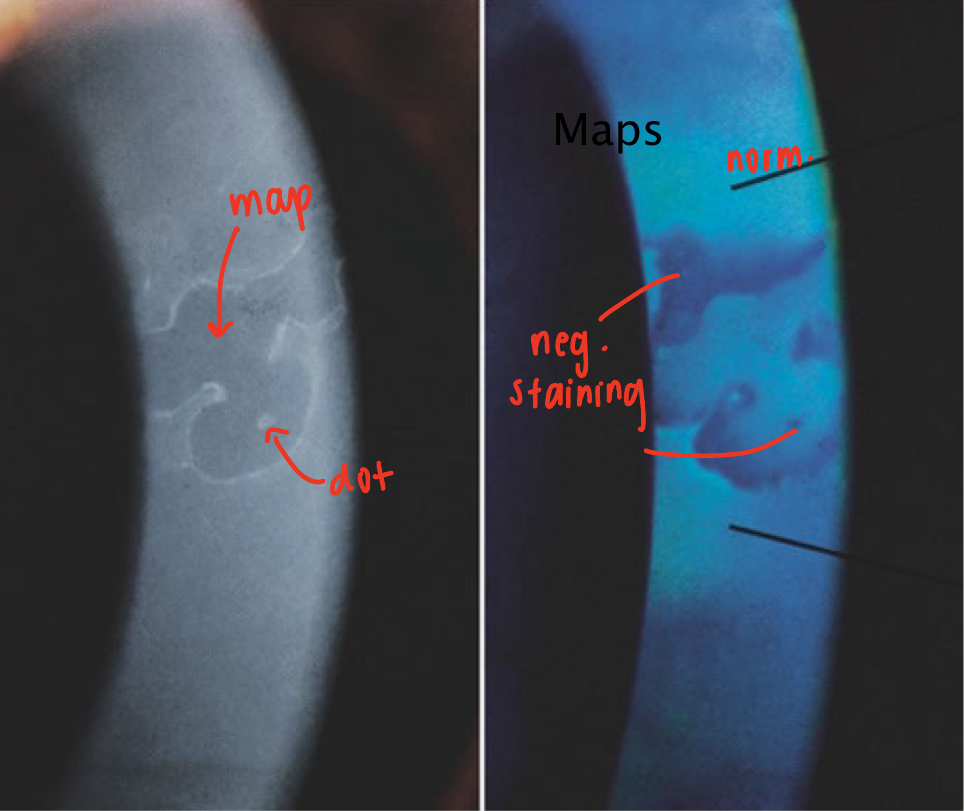
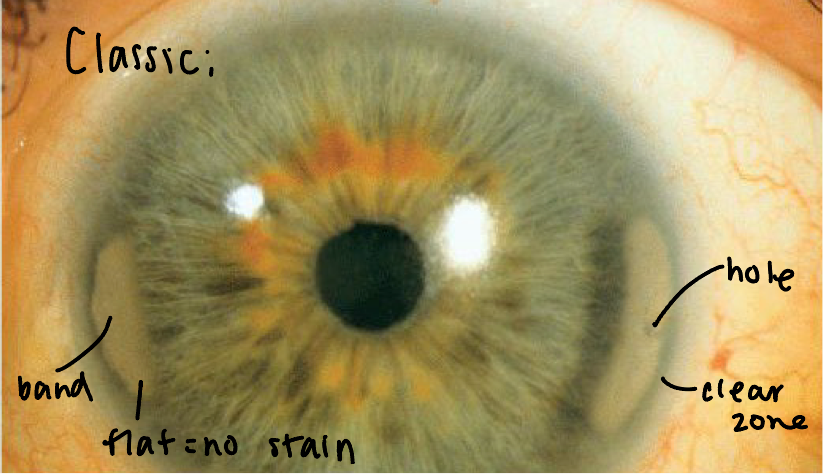
Epithelial Basement Membrane Dystrophy (Cogan or Map-Dot-Fingerprint)
most common; affects 40% of population
in 70% of individuals over 50
Onset: 2nd decade
More common in females
Inheritance pattern: no clear inheritance pattern
Can be due to trauma and some consider condition more of a degeneration
Pathophysiology: synthesis of an abnormal basement membrane
Faulty adhesion between the basement membrane and epithelium
BM extends into epithelium & causes it to heap up
elevated tissue = map
Migrated cellular material becomes trapped and develops dots and other cystic changes
Adjacent rows of thickened and elevated epithelium will develop into fingerprints
Symptoms: asymptomatic
if progressed: blurry vision worse in AM, diplopia, dry eye, foreign body sensation
Presentation: maps, dots or fingerprints
Maps: appear as large geographic lesions
Dots: commonly seen with maps
Fingerprints: appear as line
commonly seen in isolation
Due to elevated epithelium, lesions will appear to have negative staining
Complications: recurrent corneal erosions (RCE) in inferior third
Due to the hemidesmosomes inability to anchor the epithelium to the anterior stroma
occurs in 3rd decade
Symptoms of RCE: severe pain, usually upon waking
Presentation: epithelial defect-stains with fluorescein
Treatment: depends on the symptoms
none if asymptomatic
artificial tears for blurry vision, dry eye, FBS
for mild/RCE prevention:
Hypertonic salt solution (helps keep the epithelium anchored to the stroma)
Topical steroids
Oral tetracycline/doxycycline
EBMD Treatment
Asymptomatic: none
Blurred vision, foreign body sensation and dry eye symptoms: artificial tears
For mild cases/RCE prevention:
hypertonic salt solution (keeps anchored)
topical steroids
oral tetracycling/doxycycline
For moderate to severe cases/history of RCE:
Debridement: surgical intervention to remove irregular epithelium on active RCE
Phototherapeutic keratectomy-done with excimer laser
Stromal puncture: causes scar tissue which will anchor the epithelium to stroma
Bandage contact lens
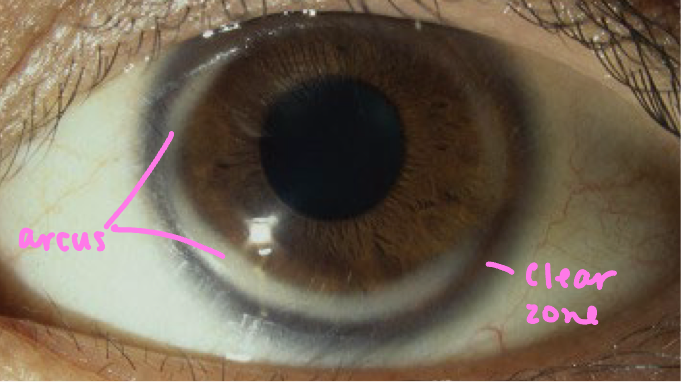
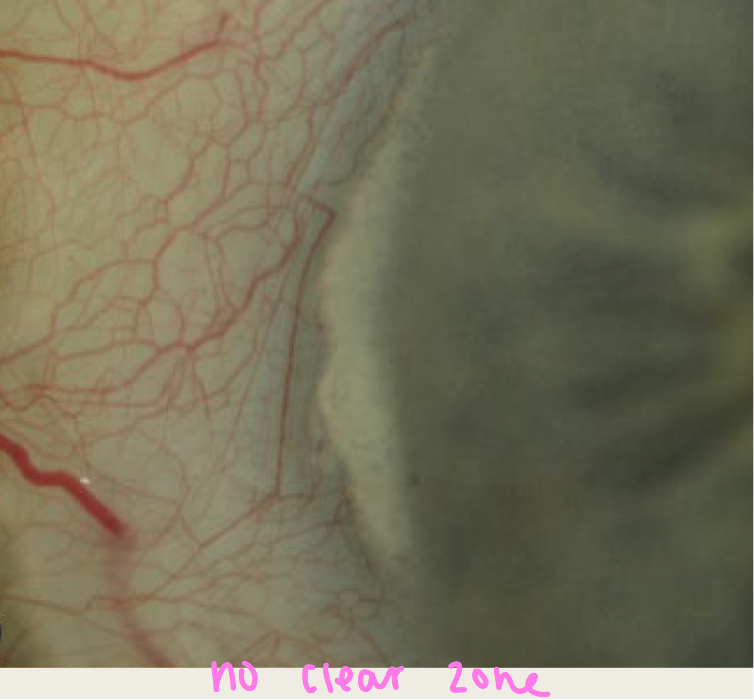
Arcus senilis
most common peripheral corneal opacity
Symptoms: None
Onset: all ages
Younger individuals: related to systemic disease (high lipids)
Older individual: no systemic association
Presentation: stromal lipid deposition
Starts superior and inferior and progressed circumferentially
Will be 1mm wide
Will have a clear zone between corneal opacity and limbus
Treatment: none unless suspect systemic association
Vogt limbal girdle
common peripheral corneal opacity
Onset: elderly individuals
Found in 60% of individuals over the age of 40
Symptoms: asymptomatic
Presentation: whitish crescentric limbal bands made up of chalk like flecks
Occurs at 9 and/or 3 o’clock
More common nasal, can go temporal
May present with holes within the lesion; gives “swiss cheese” appearance
Treatment: none
Crocodile shagreen
Onset: elderly individuals
Symptoms: none
Presentation: greyish-white, polygonal stromal opacities that resemble crocodile skin
Opacities are ill defined (hazy) and separated by clear spaces
in anterior stroma
Treatment: none

Band keratopathy
Symptoms: asymptomatic until advanced disease occurs and then the patient presents w/ irritation (once migrated over visual axis)
Causes:
Ocular: anterior uveitis, glaucoma, phthisis bulbi, chronic corneal edema and keratitis
Age: common in elderly
Metabolic: hyperparathyroidism, vitamin D toxicity, sarcoidosis, end stage renal failure
Presentation: calcium salts in Bowman layer, epithelial basement membrane and anterior stroma; starts nasal & temporal
Clear zone between deposits and limbus
Will have transparent holes within deposits
Gradual extension to central cornea
Advanced lesions become nodular and elevated = neg stain
Treatment: chelation
Removal of the epithelium and calcium then EDTA is applied until calcium is removed
Band keratopathy Treatment
Chelation: Removal of the epithelium and calcium then EDTA is applied until calcium is removed
chemical will cause abrasion
Spheroidal degeneration
common in males
Cause: UV light; more common in those who spend hours outdoors
Symptoms:
asymptomatic
Blurred vision in individuals with advanced cases
Presentation: amber colored granules in anterior stroma
Granules replace Descemet membrane
In advanced disease corneal opacification and central spread will occur
Lesions will also protrude above the corneal surface
foreign body sensation
Treatment:
UV protection
Superficial lesions: phototherapeutic keratectomy
Advanced disease: Lamellar keratoplasty or penetrating keratoplasty
Spheroidal degeneration Treatment
UV protection
Superficial lesions: phototherapeutic keratectomy
Advanced disease: Lamellar keratoplasty or penetrating keratoplasty
Salzmann nodular degeneration
Average age of onset: 59 years old
Female>Male
Cause: chronic corneal irritation or inflammation
Trachoma, chronic blepharitis, chronic allergic keratoconjunctivitis, dry eye
Symptoms: dryness, foreign body sensation, decreased vision
Presentation: superficial stromal opacities that progress to elevated whitish to blue-grey nodular lesions
nodules are round or elongated
Nodules of hyaline tissue and are located anterior to Bowman layer
Treatment:
lubrication
Surgery: superficial keratectomy, phototherapeutic keratectomy or lamellar keratoplasty
smooths surface
Salzmann nodular degeneration Treatment
lubrication (dry)
Surgery: superficial keratectomy, phototherapeutic keratectomy or lamellar keratoplasty
smooths surface of cornea
Corneal ectasias
non-inflammatory (white eye)
progressive
always bilateral but asymmetric
Characterized by corneal thinning and bulging of the cornea
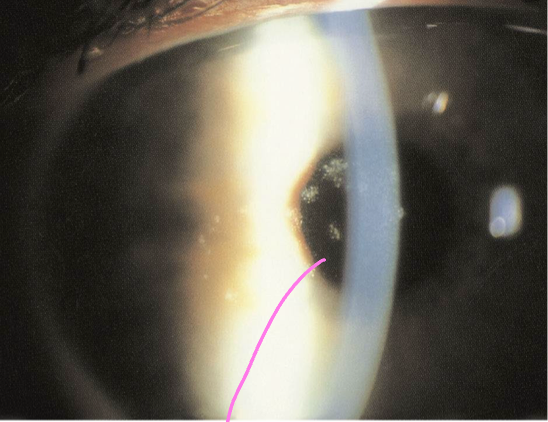
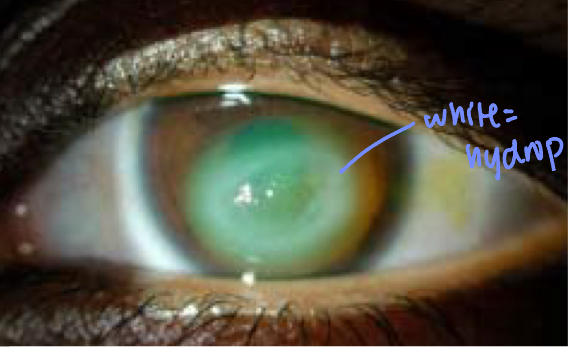
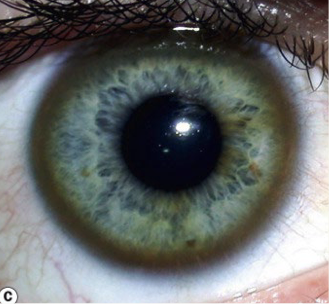
Keratoconus
Inheritance pattern: autosomal dominant
Onset: teens to twenties
Systemic association: Down Syndrome, Ehlers-Danlos, Marfan syndrome and Osteogenesis imperfecta
Ocular association: vernal keratoconjunctivitis and eye rubbing
Symptoms: blurred vision with multiple spectacle changes
Pain will be reported with complications
Presentation:
Refractive findings: high amounts of myopia and irregular astigmatism (see scissoring)
Steep Keratometry readings
Mild: <48 D
Moderate: 48-54 D
Severe: >54D
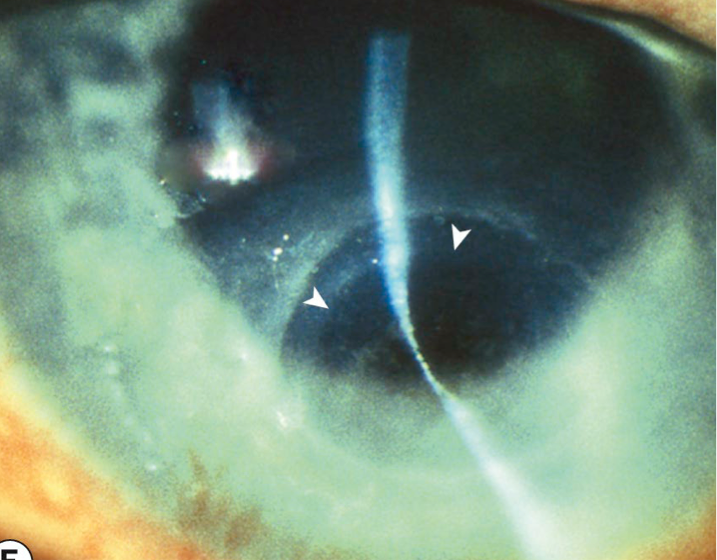
Slit lamp findings:
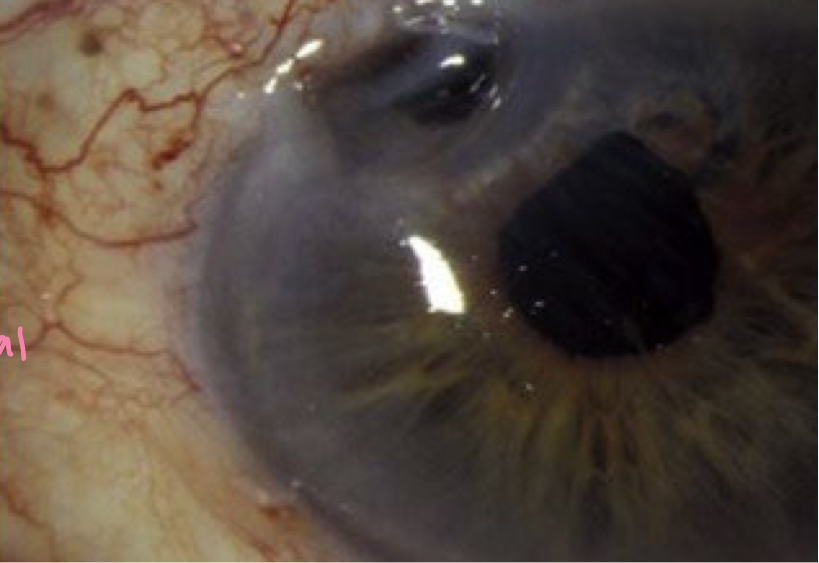
Conical corneal protrusion inferior
Stromal thinning inferior and scarring
Fleischer ring = iron deposit at base of cone
Vogt’s striae = vertical lines in Descemet
Munson sign = lid V shape in downgaze
Charleaux sign = Oil droplet when viewing red reflex
Corneal topography: inferior steepening and distortion of Placido’s disc
Complications:
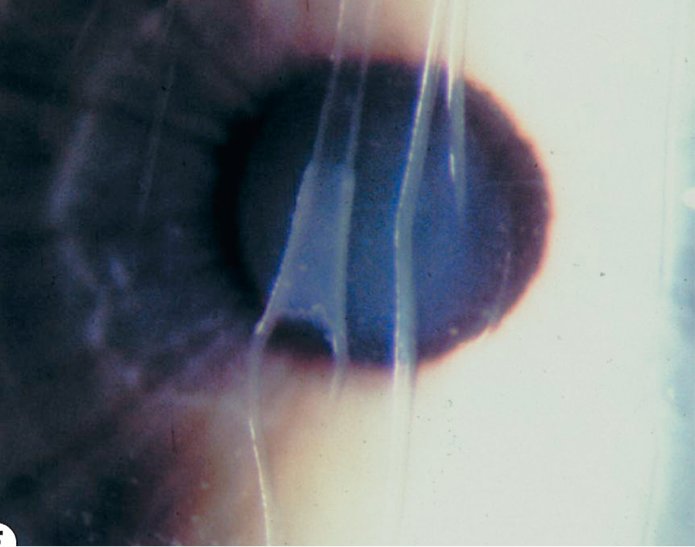
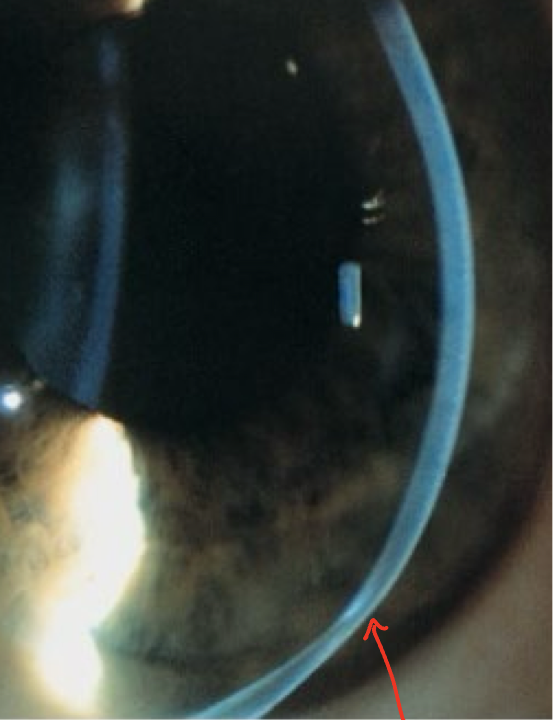
Hydrops: breaks in Descemet membrane causing aqueous into the stroma resulting in stromal edema
Pain, photophobia, epiphora, dec vision
Corneal haze, conj. hyperemia, ant chamber rxn
Treatment:
Spectacles: best corrected visual acuity is reduced in keratoconic patients
Rigid contact lens: creates a spherical and regular refractive surface over an irregular cornea
Scleral lenses: large contact lens that rest on sclera
Intacts: half circle pieces of polmethylmethacrylate (PMMA) inserted into mid-stroma to flatten cornea
Corneal cross linking: UVA strengthens cornea via oxidation
Penetrating keratoplasty (PK)

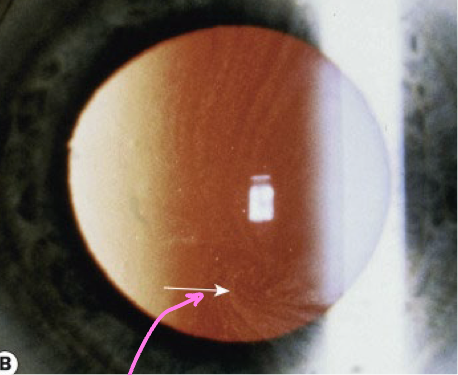
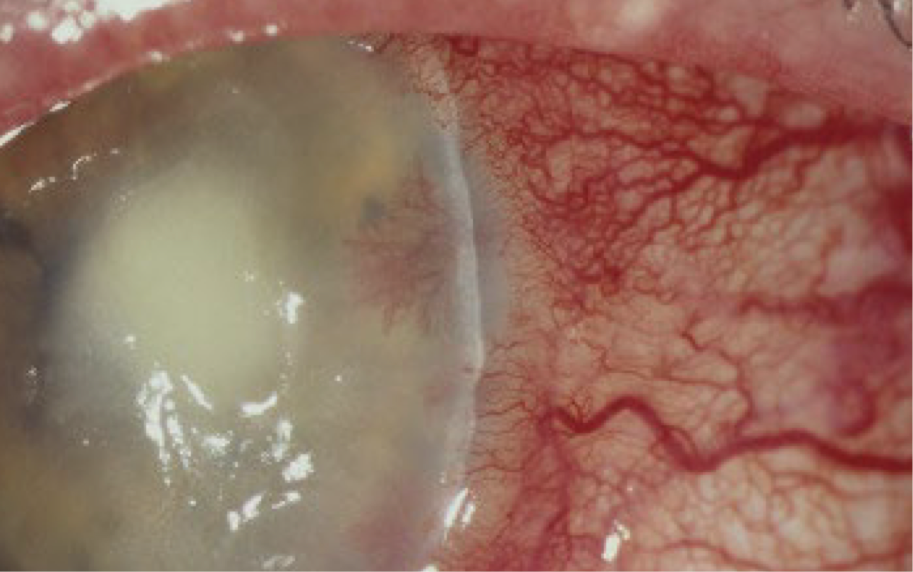
Hydrops
breaks in Descemet membrane causing aqueous into the stroma resulting in stromal edema
complication of keratoconus
Occurs in approximately 3% of keratoconic patients
Seen in advanced keratoconus
Symptoms: pain, photophobia, epiphora and decreased vision
Presentation: corneal haze
Conjunctival hyperemia, anterior chamber reaction
Treatment (heal in 6-10wks):
Topical cycloplegics (helps with pain control)
Hypertonic salt ointment
Topical antibiotic solutions (helps prevent secondary infection)
Topical NSAID
Topical corticosteroid
Bandage contact lens
Keratoconus Treatment
Spectacles: best corrected visual acuity is reduced in keratoconic patients
Rigid contact lens: creates a spherical and regular refractive surface over an irregular cornea
Scleral lenses: large contact lens that rest on sclera
vault cornea to create regular refractive surface
Intacts: half circle pieces of polmethylmethacrylate (PMMA) inserted into mid-stroma
flattens cornea
requires clear visual axis
removable
Corneal cross linking
halts progression
Riboflavin with UVA exposure will strengthen the cornea
Cornea is strengthen by increasing covalent bonds by oxidation
stability improves
can be done by removing corneal epithelium (better results) or keeping it
Penetrating keratoplasty (PK)
Removal of the entire diseased/scarred cornea and replaced with a donor cornea
Complications: PEEs, GPC, wound leak, shallow ant. chamber, iris prolapse, uveitis, inc. IOP, Khodadoust line from rejection
What do rigid contact lens allow for?
regular refractive surface
Pellucid marginal degeneration
Onset: adulthood
Symptoms: blurred vision
Presentation:
Refractive error findings: ATR astigmatism
Slit lamp findings: crescentric 1-2mm band of corneal thinning located inferior
between 4 and 8 o’clock
Will be 1mm away from the limbus
Fleischer ring, Vogt’s striae and hydrops are rare
Corneal topography: band of inferior steepening
runs from 4 to 8 o’clock
kissing bird or butterfly topography
Treatment
spectacles
contact lenses: toric soft contact lenses, gas permeable contact lenses, scleral contact lenses
Lamellar keratoplasty
Pellucid marginal degeneration Treatment
spectacles
contact lenses: toric soft contact lenses, gas permeable contact lenses, scleral contact lenses
Lamellar keratoplasty
Keratoglobus
Onset: birth or adulthood
Presentation at birth is associated with Ehler-Danlos, Leber congenital amaurosis & blue sclera
Presentation in adulthood is thought to evolve from keratoconus or pellucid marginal degeneration
Symptoms: decreased visual acuity
Presentation:
Refractive error findings: myopia and irregular astigmatism
Slit lamp findings: globular cornea with generalized corneal thinning
hydrops are rare
corneal diameter is normal
Corneal topography: steepening limbus to limbus
Complications: corneal rupture with relatively mild trauma
Treatment:
spectacles
scleral contact lenses
lamellar keratoplasty

Wilson disease (hepatolenticular degeneration)
Onset: teenage years to early twenties
Cause: deficiency in a copper carrying blood protein that results in excess deposition of copper in tissues especially the liver, brain, and eyes
Systemic presentation: liver disease, neurological symptoms, psychiatric disturbance & death if left untreated
Liver disease: will see yellowing of the skin and sclera, swelling of legs and abdomen, bruising, and prolonged bleeding & excessive tiredness
Neurological symptoms: tremor, involuntary movements, difficulty swallowing & speaking, muscle rigidity
Psychiatric symptoms: depression, schizophrenia, personality changes
Presentation:
Brownish-yellow ring of copper (Kayser-Fleischer ring) in Descemets
May have an associated sunflower cataract
Treatment:
Systemic treatment to lower copper levels
No ocular treatments required
Fabry disease
Inheritance pattern: X-linked
males>females
Cause abnormal tissue accumulation of glycolipid
Systemic manifestations: cardiomyopathy and renal disease
Presentation:
White to golden-brown corneal opacities in a vortex pattern
Other ocular signs: wedge or spoke shaped posterior cataract, conjunctival vascular tortuosity and aneurysms, retinal vascular tortuosity
Treatment:
Treatment of systemic condition
No ocular treatment
Interstitial Keratitis
inflammation of the corneal stroma without primary involvement of the epithelium or endothelium
Inflammation is thought to be an immune mediated response triggered by an antigen
Causes: syphilis, herpes simplex, varicella zoster
Syphilitic Interstitial Keratitis
Primarily seen with congenital syphilis infection but can occur with acquired syphilis infection
Caused by Treponema pallidum
4 Stages:
Primary: sores at the site of the infection
Secondary: skin rash, swollen lymph nodes and fever
Latent: no signs or symptoms
Tertiary: affects organ systems (heart, brain)
Onset: between the ages of 5 to 25
Bilateral in 80% of cases
Symptoms: blurred vision
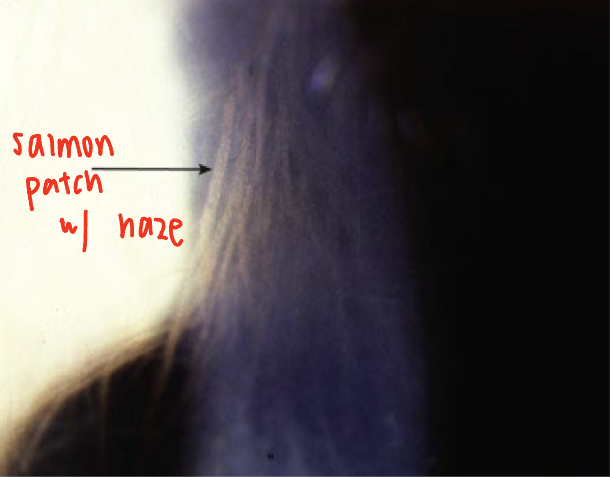
Presentation:
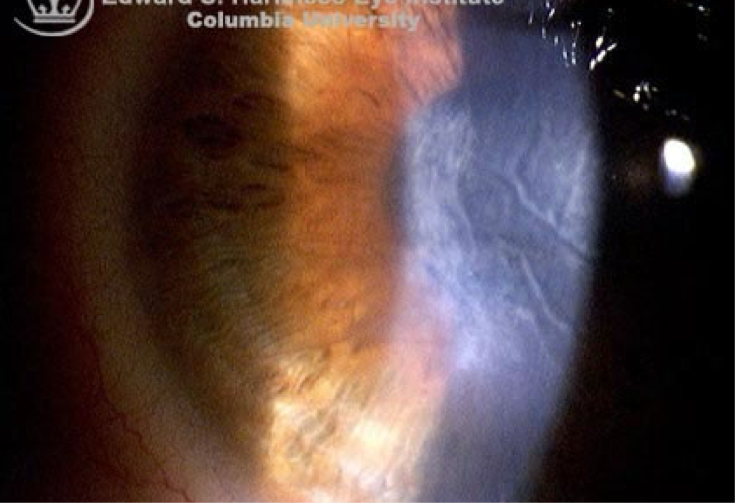
Acute:
Deep stromal blood vessels and corneal edema (salmon patch)
Anterior uveitis with keratic precipitates
Conjunctival injection
Chronic:
Deep corneal haze or scarring
Ghost vessels (deep blood vessels that contain little to no blood)
stromal thinning (can cause perforation)
If recurrence occurs the ghost vessels may fill with blood and may bleed into the cornea
Complications:
deep stromal scarring with thinning
Astigmatism
Band Keratopathy
Treatment:
Lab work up for detecting syphilis
Referral for systemic control of the infection
Topical steroid
Topical cycloplegia
Syphilitic Interstitial Keratitis Treatment
Lab work up for detecting syphilis
FTA-ABS: will determine if the individual has syphilis
RPR or VDRL: will determine if the infection is active or not
Referral for systemic control of the infection
Topical steroid
it’s inflammatory!
Topical cycloplegia
rests ciliary body = pain control
Congenital Syphilis
infection crosses placenta & infects the fetus
Systemic signs:
Early signs: failure to thrive, maculopapular rash, mucosal ulcers
Late signs: sensorineural hearing loss, saddle-shaped nasal deformities, jaw abnormalities - underdeveloped maxillary bone and prominent mandibular bone, teeth abnormalities, joint abnormalities
Ocular signs: anterior uveitis, interstitial keratitis, dislocated/subluxated lens, cataract, optic atrophy, salt and pepper pigmentary retinopathy, Argyll Robertson pupil
HSV 1
affects face, lips, eyes
HSV 2
sexually transmitted
Can be transferred from mother to infant during birth
Resides in neuronal ganglion
trigeminal for the eye
Herpes Simplex Keratitis
Most common infectious cause of blindness in developed countries
Primary infection: typically occurs in childhood
spread by droplets or direct inoculation
Uncommon during the first six months of life due to maternal antibodies
Present as mild fever, malaise and upper respiratory tract symptoms; can have bleph or follicular reaction after age 2
Recurrent infection:
Triggers: fever, hormonal change, UV radiation, trauma
Risk factors for severe disease: topical steroid use, atopic eye disease, immunodeficiency or suppression, malnutrition
Corneal scarring will be seen with every recurrence
VA loss
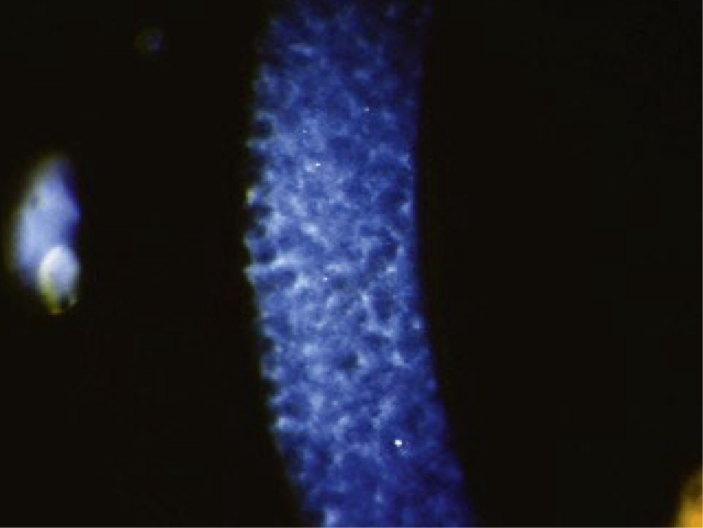
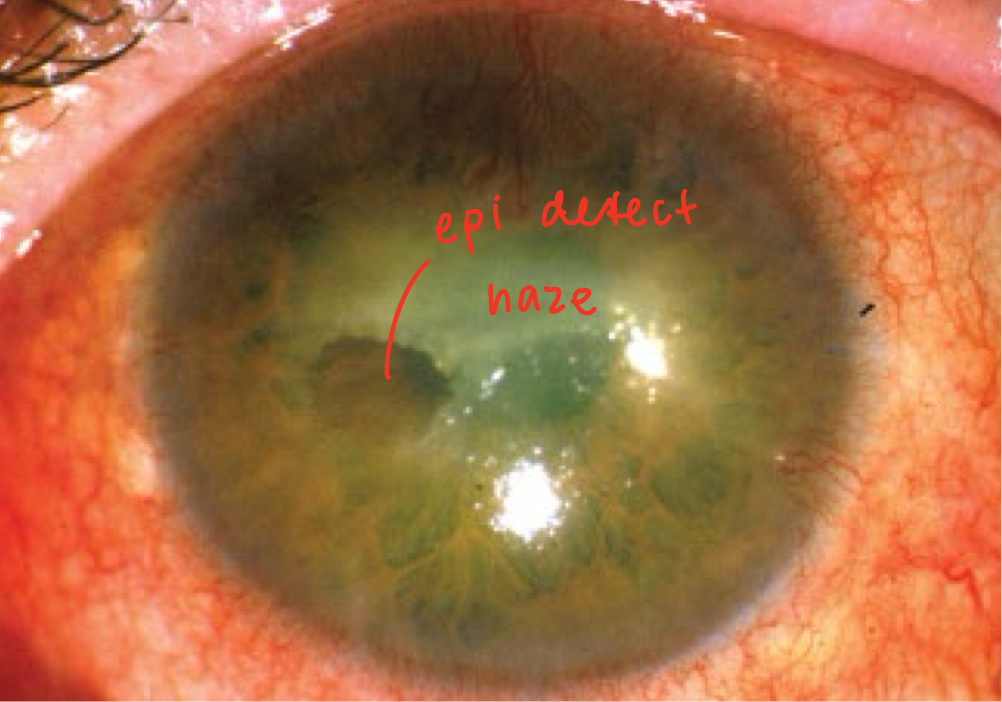
Epithelial Keratitis from Herpes Simplex
Associated with active virus replication**
Symptoms: mild to moderate discomfort, hyperemia, photophobia, tearing and blurred vision; lack of pain
Presentations (in chronological order):
reduced visual acuity
Swollen opaque epithelial cells, will present in a punctate or stellate configuration
Dendritic ulceration-linear branching
Frequently located centrally
Ends of the dendrite (terminal bulbs) will stain with Rose Bengal
Reduction of corneal sensation
Mild subepithelial haze (may take weeks to heal)
Mild anterior chamber reaction
Follicular conjunctival reaction
lid vesicles (can be seen at ulceration)
elevated IOP
Trabecular meshwork’s inflamed
Complications from steroids:
Geographic ulcer
Treatment:
Topical antiviral solution or gel
Topical cycloplegia (for pain of AC rxn)
Debridement for resistant cases
Oral antiviral medications (for when topical isn’t tolerated)
Topical glaucoma medications if IOP is elevated (avoid prostaglandins)

Epithelial Keratitis Treatment
Topical antiviral solution or gel
Topical cycloplegia (for pain of mild ant. chamber rxn)
Debridement for resistant cases
epithelium is removed 2mm from the edge of the ulcer
Oral antiviral medications (for when topical isn’t tolerated)
good for long term, recurrence (PCP needs to maintain their health)
Topical glaucoma medications if IOP is elevated (avoid prostaglandins)
What meds do you never use for treating IOP on a patient with a Herpes reaction/infection?
prostaglandins
Stromal Keratitis from Herpes Simplex
Cause: immune mediated response to viral antigens**
Severe cases may be a reaction to live virus in the stroma
2 Types:
Immune stromal keratitis
Necrotizing interstitial keratitis
Treatment:
Topical steroid (immune rxn, not active infection!)
Topical antiviral-if epithelial defect is present
Oral antiviral
Penetrating keratoplasty if corneal perforation occurs
Immune Stromal Keratitis
Symptoms: blurred vision, photophobia, glare and halos
Presentation:
Stromal infiltrates with intact epithelium (neg stain)
Infiltrates can be focal, multifocal or diffuse
Stromal edema
Mild anterior uveitis
Chronic cases can cause stromal vascularization and corneal scarring
Lipid deposition may also be seen
Necrotizing Stromal Keratitis
Presentation:
Dense stromal infiltration
Epithelial defect may or may not be present
Progressive necrosis with corneal perforation
Anterior uveitis with hypopyon
Increase IOP due to trabeculitis
Stromal Keratitis Treatment
Topical steroid (immune rxn, not active infection!)
Topical antiviral-if epithelial defect is present
Oral antiviral
if recurrent & topical not doable
Penetrating keratoplasty if corneal perforation occurs
Endothelial (Disciform) Keratitis
Cause: immune response to viral antigen
Symptoms:
Gradual onset of blurred vision with associated glare around lights
Discomfort-less than with epithelial disease
Hyperemia-less than with epithelial disease
Presentation:
Disc-shaped stromal edema located in the center of the cornea
Epithelium will be intact
Mild anterior uveitis
Granulomatous keratic precipitates
Immune ring of stromal haze (Wessely ring)-signifies deposition of viral antigen and host antibody complexes
Increased IOP d/t trabeculitis
Treatment:
Topical corticosteroid
Topical antiviral
Topical cycloplegic (provide comfort due to AC reaction)
Endothelial (Disciform) Keratitis Treatment
Topical corticosteroid
Topical antiviral
Topical cycloplegic (provide comfort due to AC reaction)
Neurotrophic keratopathy
complication of Herpes infection of cornea
Cause: failure of corneal re-epithelization due to corneal anesthesia
Exacerbated by drug toxicity and reduction in tear production
Presentation:
Sterile infiltrate with overlaying epithelial defect
Borders will be smooth
Stroma under the defect is grey and opaque
stromal will thin
central, interpalpebral
Complications:
Secondary bacterial infection
Corneal thinning with perforation
Scarring
Neovascularization
Treatment:
Discontinue medication if related to drug toxicity
Preservative free artificial tears
Cenegermin-bkbj ophthalmic solution (Oxervate)
Bandage contact lens
Amniotic membrane
Tarsorraphy
Preservative free topical antibiotic for secondary infection
Neurotrophic keratopathy Treatment
Discontinue medication if related to drug toxicity
Preservative free artificial tears
Cenegermin-bkbj ophthalmic solution (Oxervate)
promotes neuron growth
Bandage contact lens
Amniotic membrane
put bandage CLs on after
Tarsorraphy
Preservative free topical antibiotic for secondary infection
HEDS I
Herpes Stromal Keratitis: topical steroids and topical anti-viral provided a faster resolution when compared to topical anti-viral alone
Time frame for the initiation of topical steroids is not crucial
Adding oral anti-viral to topical anti-viral and topical corticosteroid is not beneficial
HEDS II
Herpes Simplex Keratitis: adding oral anti-viral to topical anti-viral does not prevent the patient from developing stromal disease
Oral anti-viral reduces the recurrence of herpetic eye disease
Herpes Zoster Ophthalmicus
Cause: Varicella-Zoster virus
Onset: sixth to seventh decade
Can be seen in younger individuals
Symptoms tend to be worse in older individuals compared to younger individuals
Common in immunocompromised individuals
Resides in cranial nerve ganglia until re-activated
Acute Presentations:
epithelial keratitis (2 days after); psuedodendrites
nummular keratitis (10days after)
stromal/interstitial keratitis (3wks after)
disciform keratitis
Conjunctivitis: follicular and/or papillary reaction
Episcleritis (occurs at the onset of the rash)
Chronic Presentations:
Neurotrophic keratopathy
Mucus plaque keratitis
Acute Shingles
Prodromal phase: occurs 3 to 5 days prior to the appearance of the rash
Will consist of tiredness, fever, malaise and headache
Affected dermatome will experience superficial itching, tingling or burning sensation
Additional symptoms include severe boring or lancing pain that is constant or intermittent
Presentation: painful erythematous areas with a maculopapular rash
Rash will respect the midline
Vesicles will appear within 24 hours
Vesicles will be in grouped together and will coalesce within 2-4 days
Will crust and completely resolve in 2-3 weeks
Eyelid edema of the upper and lower lid
Multiple dermatomes may be involved with immunocompromised patients
Treatment:
Oral antiviral: given within 72 hours of the onset of the rash
Will reduce the severity and duration of the acute episode and risk for post herpetic neuralgia
If a patient presents after 72 hours but still has vesicles, consider prescribing oral antiviral
Topical antibiotic ointment for vesicles
Acute Shingles Treatment
Oral antiviral: given within 72 hours of the onset of the rash
Will reduce the severity and duration of the acute episode and risk for post herpetic neuralgia
If a patient presents after 72 hours but still has vesicles, consider prescribing oral antiviral
Topical antibiotic ointment for vesicles
prevent secondary infection
Epithelial keratitis from Herpes Zoster Ophthalmicus
develops in 50% of patients 2 days after onset of the rash
Will spontaneously resolve in a few days
Characterized by pseudo-dendrites similar to herpes simplex dendrites
Will have taper ends rather than terminal bulbs
Will stain better with Rose Bengal than fluorescein

Nummular Keratitis from Herpes Zoster Ophthalmicus
develops at the site of the epithelial lesions
Occurs 10 days after the onset of the rash
after psuedodendrite stage
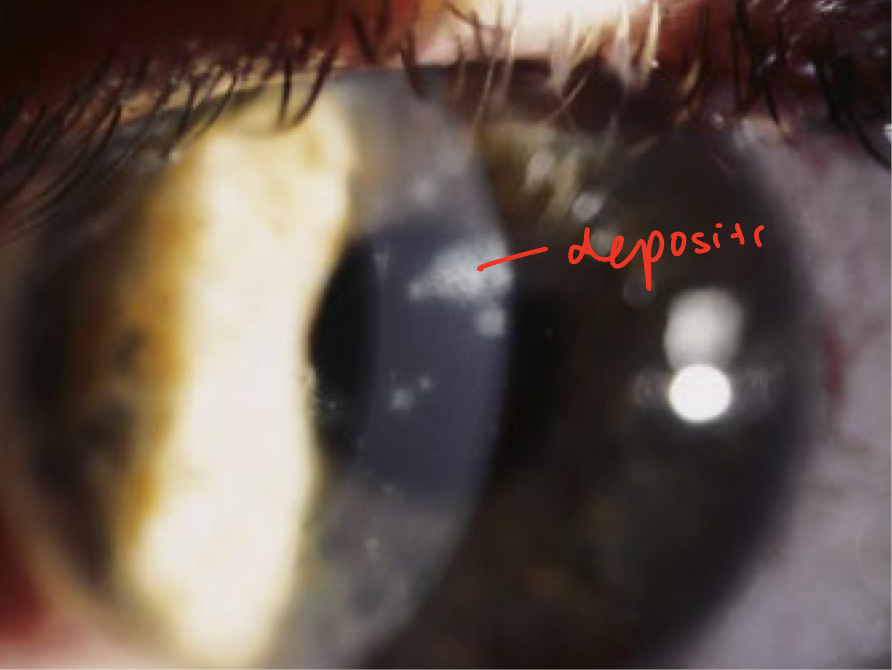
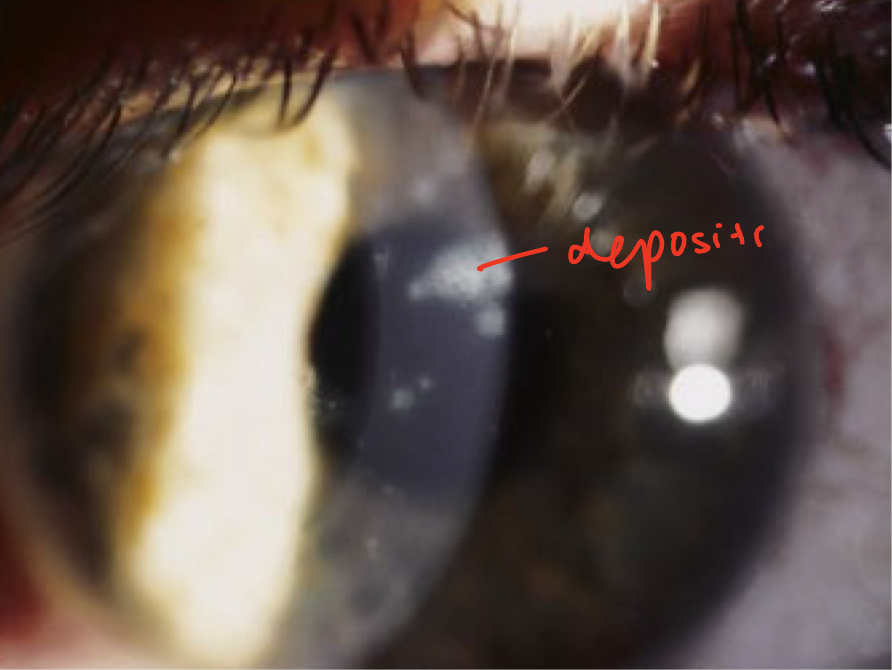
Characterized by fine granular subepithelial deposits
Deposits will have a halo of stroma haze surrounding it
Stromal (interstitial) Keratitis from Herpes Zoster Ophthalmicus
occurs 3 weeks after the onset of the rash
Significant scarring can occur
dec VA
Disciform keratitis (immune mediated endothliitis) from Herpes Zoster
Less common than with HSV
Corneal decompensation may occur
Neurotrophic keratopathy from Herpes Zoster Ophthalmicus
from chronic zoster
Occurs in 50% of patients
Tends to be mild and will resolve over several months
similar to HSV infections
Mucus plaque keratitis from Herpes Zoster Ophthalmicus
chronic
occurs between 3-6 months of onset of symptoms
Elevated mucus plaques that stain with Rose Bengal
If left untreated, plaques will become scars
Acute Treatment of Herpes Zoster Ophthalmicus
Epithelial keratitis: preservative free artificial tears
no active infection = no antibiotic
Nummular keratitis/stromal keratitis/disciform keratitis: topical corticosteroid
Require slow taper to prevent recurrence for nummular and stromal keratitis
Chronic Treatment of Herpes Zoster Ophthalmicus
Neurotrophic keratopathy: same treatment as neurotrophic keratitis in Herpes Simplex
Mucus plaque keratitis: debridement, then topical steroid
Post-herpetic neuralgia
pain that persist for more than one month after the resolution of the rash
Develops in 75% of individual over the age of 70
Presentation: intermittent or constant pain
Pain may be worse at night and aggravated by touch or heat
Treatment: cold compresses
Topical capsaicin cream, tricyclic antidepressants, anticonvulsant medications