Critical care part 2
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
What are the clinical exam findings associated with parenchymal disease/restrictive pattern?
Acute dyspnoea/tachypnoea
Abnormal heart sounds (gallop, murmur, arrhythmia)
Crackles
(Fever, SIRS, sepsis)
What are the differential diagnoses for parenchymal disease/restrictive pattern?
Oedema > cardiogenic or noncardiogenic
Haemorrhage
Exudate (fungal, bacterial)
Pneumonitis
Neoplasia
Fibrosis
What is included in the minimum database for parenchymal disease/restrictive pattern?
Oxygen
Sedation
SPO2 or arterial blood gas
Frus trial
Thoracic imaging
Haem/biochem
NT pro BNP
What are the clinical examination findings in pleural space disease or restrictive/paradoxical pattern
Tachypnoea
Reduced lung sounds
What are the differentials for pleural space disease?
CHF
Chylothorax
Pneumothorax
Pleural effusion: chyle, pyothorax, FIP, blood, neoplasia
Diaphragmatic rupture
What is included in the minimum database in pleural space disease?
Oxygen
Sedation
SpO2, arterial bood gas analysis
Thoracocentesis: cytology ± culture
Thoracic imaging
Haem/biochem/UA
NT Pro BNP
FeLV/FIV testing
What are the clinical exam findings in chest wall disease/restrictive or paradoxical pattern?
Dyspnoea
Tachypnoea
Shallow/restricted chest movement (pain)
Paradoxical chest wall movement (flail chest)
What are the differentials for chest wall disease?
Trauma (penetrating or blunt eg fractures)
Abscess/wpund
Neoplasia
What is included in the minimum database for animals with chest wall disease?
Oxygen
Occlusive chest bandage and thoracocentesis ± positive pressure ventilation if penetration into pleural space
Sedation, pain control
SpO2 or arterial blood gas
Thoracic imaging (ultrasound, radiographs)
What are the limitations of pulse oximetry?
A good pulse wave is required for an accurate reading. Concurrent problems like cardiac disease or hypovolaemic/distributive shock will decrease the strength of the pulse.
The presence of abnormal haemoglobin eg methaemoglobin may interfere with results
Pigmented skin
Movement
The arterial partial pressure of oxygen should be how many times the fractional inspired oxygen?
FIVE. So on room air (21% oxygen) a normal animal should have a PaO2 of 85-110mmHg
Arterial blood gas analysis also allows measurement of arterial CO2 which allows assessment of what alongside oxygen status?
Ventilation
What anatomic locations should be images in an AFAST?
Diaphragmatic-hepatic
Cysto-colic
Hepato-renal
Spleno-renal
What areas should be imaged in a POCUS?
Chest tube side
Pericardial site
Diaphragmatic hepatic site
What are the 5 borders for PLUS?
Caudal border, defined by the curtain sign
Dorsal border, defined by the hypaxial muscles
The cranial border - not the true border of pleura and lung but the border that is limited by the thoracic limb
The ventral pleural border
The ventral lung border
What ultrasound views are best to rule out pneumothorax?
Dorsal views
What does absence of a glide sign suggest?
Pneumothorax
How can you avoid false positives when assessing the chest for a pneumothorax using ultrasound?
Search for the dorsal border of the lung
Detection of 3 or more B lines is highly suggestive of what?
Alveolar-interstitial disease
What are the criteria for identifying B lines?
Vertical white lines
Originate from the lung surface
Move with the pleura
Extend to the far field
Obscure A lines if A lines are present
Where should yo perform thoracocentesis so you avoid the heart?
7-9th ICS
Why should you enter the pleural space at the cranial aspect of the rib?
As the blood vessels and nerves lie caudal to the rib.
Exudative fluid with a high neutrophil count (>85% neutrophils) with a pH of 6.9 or less is likely due to what?
Pyothorax
A fluid with a low neutrophil count (<30% neutrophils) and a pH of 7.4 or greater is likely due to what?
Neoplastic effusion
Why can frusemide be beneficial in patients with permeability oedema seen in severe pneumonia, acute respiratory distress syndrome and pulmonary trauma?
Due to its beneficial vasoactive effects including venodilation of the pulmonary veins and may increase perfusion to the ventilated areas of the lung
Why should intravenous fluid therapy be carefully considered in patients with severe parenchymal disease?
As it will tend to increase pulmonary capillary hydrostatic pressure, the major determinant of pulmonary fluid extravasation
What roles in the team are there when performing CPR?
Leader
Compressor
Breather
Drug Pusher
Recorder
Chest compressions are carried out in cycles of two minutes with no breaks. Why is there a short 5-10 second break at the end of each 2 minute cycle?
To assess the ECG and the absence or presence of pules
How much should the chest be compressed by during CPR?
1/3rd to ½
What is the rate of chest compressions per mnute?
100-120
By what two methods can chest compressions work? Outline them.
Cardiac pump and thoracic pump.
Thoracic pump - does not involve direct compression of the heart, instead if moves blood back into the thoracic cavity like bellows or suction
Cardiac pump - direct compression of the heart to try and circulate blood back to it.
What is the breathing rate during CPR?
10 breaths per minute
What is the most important monitor during compressions?
End tidal CO2 monitoring
What does end tidal CO2 monitor for?
Efficacy of compressions and to see if there has been return of spontaneous circulation
What is the aim to maintain ETCO2 over during compressions?
>15mmHg
If the ETCO2 increases to normal or above (ie, >35mmHg) what does this mean?
That spontaneous circulation has returned and compressions may be stopped
What ECG rhythms may be seen during CPR?
Pulseless electrical activity
Pulseless ventricular tachycardia
Aystole
Ventricular fibrillation
Which ECG rhythms are shockable?
Pulseless VT
Ventricular fibrillation
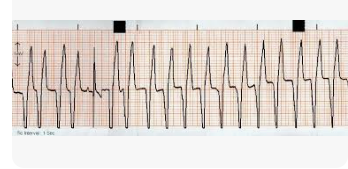
What ECG rhythm is this? Is it shockable?
(Pulseless) ventricular tachycardia
Yes
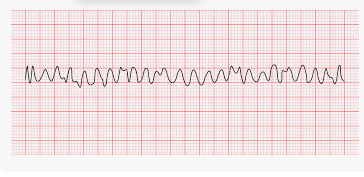
What ECG rhythm is this? Is it shockable?
Ventricular fibrillation
Yes
In asytole and PEA, chest compressions are the most important treatment for both these rhythms but they may be responsive to what?
Adrenaline and atropine
Why should drugs not be administered until the second cycle of CPR?
To ensure that there is oxygenated blood reaching the heart
What is adrenaline?
A vasopressor that causes vasoconstriction
A positive inotrope
A positive chronotrope
A lower dose of what dose of adrenaline is now recommended ever 3-5 minutes (every 2nd cycle of compressions)
0.01mg/kg
What is adrenaline not effective in the face of?
Acidosis - which is why you need to establish circulation to the heart before administration
What is vasopressin & how often should you administer it?
A more specific vasopressor (not affected by acidosis)
Every 3-5 mins (every 2nd cycle)
What is atropine and what does it do?
An anti-cholinergic drug that will act to speed up rate of contraction
Lidocaine can be used in patients with what ECG changes?
Ventricular fibrillation
Pulseless ventricular tachycardia (that is resistant to defibrillation or if there is no defibrillator)
Amiodarone can be used in patients with what ECG changes?
Ventricular fibrillation (that is resistant to electrical defibrillation)
What are the metabolic consequences of a cardiac arrest?
Ischaemia-reperfusion injury which results in global damage to cells but esp the neurons
How many platelets (in the monolayer) per high power field represents a normal platelet count of 150-600×10^9/L
8-15
Give examples of causes of hyperglycaemia
Stress
Hypovolaemia
Endocrine - Cushing’s, DM
Pancreatitis
Drugs - C’steroids
Toxins
Head trauma
Give examples of causes of hypoglycaemia
Sepsis
Puppies/kittens
Hunting dog hypoglycaemia & toy breed hypoglycaemia
Endocrine (hAC)
Toxins - Xylitol
Neoplasia (insulinoma, hepatoma)
Hepatic insufficiency & end stage liver disease
Lab error
What is the difference between intracellular and extracellular potassium concentrations important for?
Determining the resting membrane potential of excitable tissues (including cardiac conduction tissue)
Why do serum concentrations of potassium do not necessarily reflect whole body potassium levels?
Due to translocation from the intracellular to the extracellular space
What principle hormone affects potassium excretion in the distal tubule?
Aldosterone
What can cause hyperkalaemia due to decreased urinary excretion?
Anuric/oliguric renal failure
Urethral obstruction
Uroabdomen
hAC
Effusive disorders: pleural, peritoneal, pericardial
GI disease (trichuriasis)
Drug induced: ACE inhibitors, K+ sparing diuretics eg spironolactone
What can cause hyperkalaemia as a result of translocation from intracellular. to extracellular compartment?
Massive cell death
Reperfusion injury following thrombolmbolism
Severe trauma
Tumour lysis syndrome
Heat stroke
Acute mineral acidosis
Insulin deficiency
Drugs > beta blockers
What are the characteristic ECG changes seen with hyperkalaemia?
Prolonged PR interval
Decreased R wave amplitude
Increased T wave amplitude
This progresses to
Atrial standstill (absent P wave)
Widened QRS complexes & bradycardia
What other factors (aside from hyperkalaemia) affect myocardial conduction?
Acid base balance
iCa status
How can you treat hyperkalaemia?
IVFT with Hartmann’s
IV soluble insulin 0.25-0.5iu/kg with 2g glucose per unit of insulin, followed by addition of 2.5% glucose to the IV fluids (takes 20 minutes to work) and glucose needs to be supplemented for 12-24h
IV calcium gluconate to counteract the effect of high K+ on myocardial conduction. Lasts 20 mins
IV sodium bicarbonate at 1-2mEq/kg. Drives potassium intracellular by changing plasma pH
Terbutaline - Promotes intracellular K_ shift through activation of Na K ATPase
What increased losses can cause hypokalaemia?
GIT
V/D
Urinary tract
CRF
Post obstructive diuresis
Drug induced > loop diuretics, penicillins
Mineralocorticoid excess
What can cause translocation from extracellular to intracellular compartments, resulting in hypokalaemia?
Insulin/glucose containing fluids
Alkalaemia
Catecholamine release
What other causes of hypokalaemia are there?
Inappetence and anorexia
Long term admin of IV fluids with low K+ concentrations
What are the mild to moderate clinical signs of hypokalaemia?
Weakness
Lethargy
Ileus
Anorexia
Ventroflexion of the neck in cats
What are the severe clinical signs of hypokalaemia. and at what levels can this be seen?
Respiratory muscle weakness
Hypokalaemia nephropathy
<2.8mmol/l
Potassium should not be infused at a rate greater than what?
0.5mEq/kg/hr
What is the main site for sodium and water homeostasis?
The kidneys
Volume regulation of fluid involves detection of intravascular volume changes at what anatomical sites?
Carotid sinus
Aortic arch
Glomerular afferent arterioles
Cardiac atria
Alterations in what systems are the principal effector mechanisms. of sodium control?
RAAS — increased sodium retention
Sympathetic nervous system — increased sodium retention
Atrial natriuretic peptide — decreased sodium retention
What does an increase in ADH lead to?
Increased body water, by stimulating thirst and increasing water reabsorption in the distal part of the nephron
What is the measured serum sodium concentration a reflection of?
The balance between the amount of sodium relative to the amount of water within the extracellular fluid compartment. It is not a direct indicator of total body sodium content.
When evaluating patients with sodium abnormalities, it is important to make an assessment of volume status of what location?
The intravascular space
Why can vomiting and diarrhoea cause hypernatraemia or hyponatraemia?
Because it depends on the nature of the losses, ie whether they contain more sodium than water or vice versa
The presence and influence of other osmotically active particles in plasma should also be considered when interpreting serum sodium values. This is clinically most relevant when?
Evaluating diabetic patients as in these patients the elevated serum glucose acts as an osmotically active particle and draws water into the vasculature, leading to the dilution of the serum sodium.
For every 1mmol/l increase in glucose, how much will the serum sodium be reduced by?
Approx 0.3-0.4mmol/l
What is pseudohyponatraemia?
An artefact that occurs when serum sodium is measured by flame photometry methology in patients with concurrent hyperlipidaemia or hyperproteinaemia.
When can you see clinical signs associated with sodium abnormalities?
When they are severe and especially if they develop rapidly.
What are the principle signs that are seen with sodium abnormalities?
Neurological
Why do neurological signs occur with hypernatraemia?
Because the increased tonicity of the extracellular fluid leads to movement of water out of brain cells which leads to cerebral dehydration
Why do neurological signs occur with hyponatraemia?
Because the decreased tonicity in the extracellular fluid promotes movement of water into the brain, with the development of cerebral oedema
What is an important determinant of the severity of clinical signs in sodium disorders?
The rate of change in sodium
If a sodium abnormality develops slowly, the brain has time to compensate and clinical signs may not be seen. What happens when hypernatraemia progresses gradually?
The brain generates intracellular substances called idiogenic osmoles which prevent fluid loss.
If hyponatraemia develops slowly, how can the brain cope?
By losing osmotically active particles.
When a serum sodium abnormality has been gradual in onset, the serum sodium should be corrected slowly, with a maximum change of what rate of sodium per hour in either direction?
0.5mEq/l sodium per hour.
If hypovolaemia is present alongside a sodium abnormality, how should you avoid rapid changes in the patient’s serum sodium?
Choose a fluid that has a sodium concentration close to the animal’s sodium.
Hypernatraemia patients 0.9% NaCl is suitable
Hyponatraemic patients Hartmann’s solution or Lactated Ringers.
Once an animal with a sodium abnormality’s intravascular volume status is resotred, the serum sodium concentration can be returned to normal over a period of what?
34-48h
What should hypernatraemic patients be encouraged to do to regain their free water?
Drink !
What should you do if a hypernatraemic patient is unable to drink and regain their free water by that route? Eg, in neurological disease
Free water must be administered using hypotonic fluids such as 0.45% NaCl or 5% dextrose in water
Why does chloride play an important role in acid base balance?
Due to its interactions with renal sodium and bicarbonate administration
When can you see artefactual hyperchloraemia?
In patients receiving KBr therapy for seizures
Hypochloraemia is of clinical relevance because of what reason?
Its effects on acid base balance
These patients are prone to developing a metabolic alkalosis (particularly if concurrent hypovolaemia with avid sodium retention)
Why are hypochloraemic patients prone to developing a metabolic alkalosis if there is avid retention of sodium?
As sodium is reabsorbed, the nephron must also reabsorb or regenerate anions to maintain electroneutrality. The anion reabsorbed is principally chloride, but in situations of chloride depletion bicarbonate is regenerated instead = predisposing to the development of alkalaemia.
Clinically - this is seen in patients with severe vomiting that develop a significant hypochloraemic metabolic alkalosis
Why should 0.9% NaCl be used as the resuscitative fluid of choice in patients with a hypochoraemic metabolic alkalotic syndrome?
Because this aid the restoration of acid base balance, as the higher chloride concentration allows the kidneys to excrete bicarbonate whilst continuing active sodium retention.
In acid base balance, carbon dioxide is excreted by where?
Through the lungs
In acid base balance, the hydrogen is excreted by where?
The kidneys
What buffers does the body have to facilitate handling of the daily acid load?
Bicarbonate > most important
Constantly regenerated and added back into the circulation by the kidneys
Haemoglobin and plasma proteins
Acidaemia is defined as a blood pH less than ?7.35
Alkalaemia is defined as a blood pH more than ?
7.45
What is metabolic acidosis or alkalosis?
When the process leading to the acid base disturbance involves abnormalities of acid/alkali other that CO2