SCI: Introduction & Sequelae
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
111 Terms
At what age does SCI incidence peak at?
15-29 years old, 65 or older
SCI occurs at a rate of _____% male, _______% female
80% male, 20% female
What is the most common cause of traumatic SCI?
MVA (followed by falls, violence, and sports-related)

What are some common causes on NON-traumatic SCI?
Vascular dysfunction, spinal stenosis, spinal neoplasms, syringomyelia, infection, neurological diseases (MS, ALS)
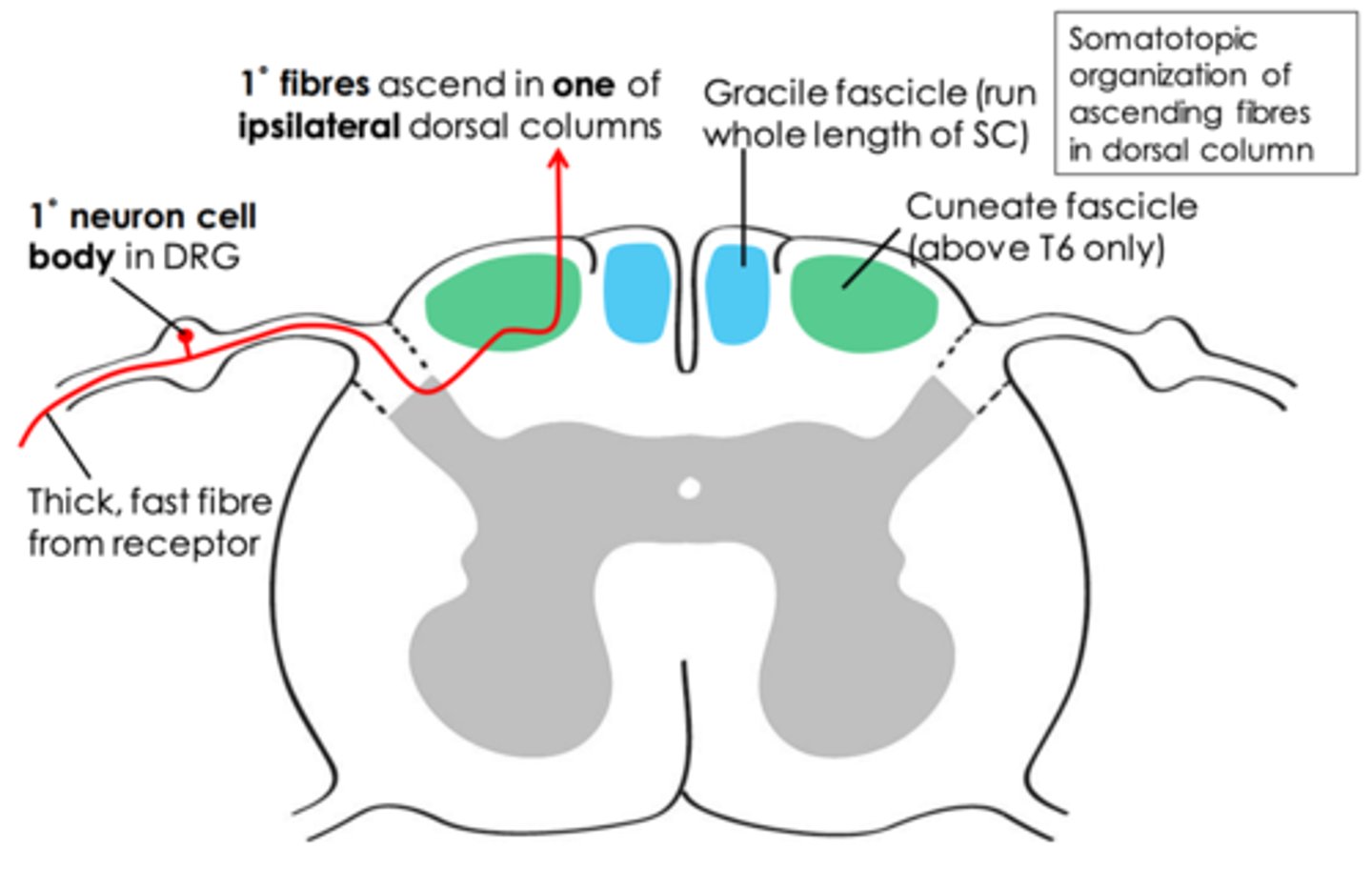
_________ (tract): proprioception (1), vibratory sensation (2), deep touch (3) and discriminative touch (4)
Dorsal column medial lemniscus
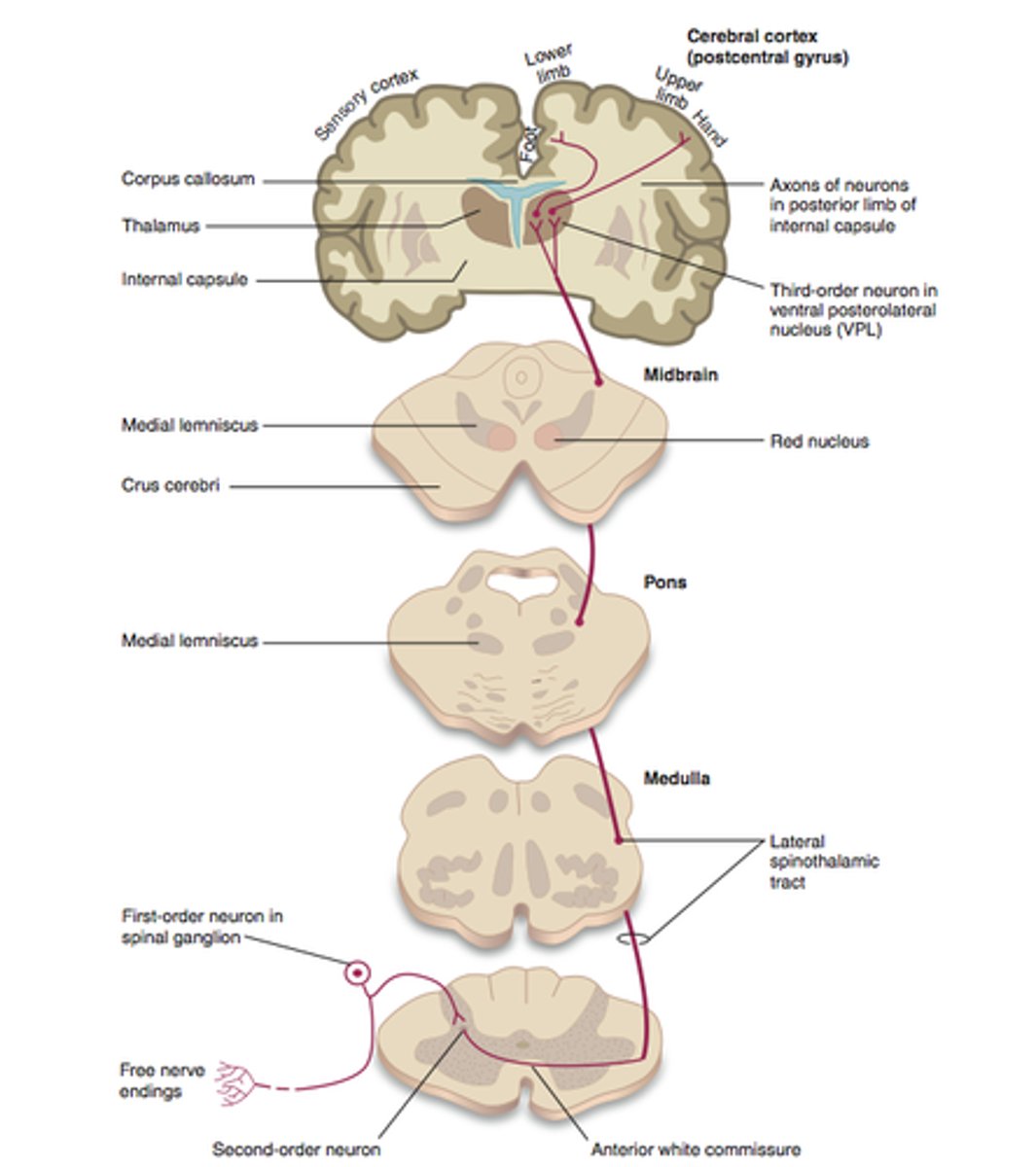
_________ (tract): NOXIOUS STIMULUS (1), temperature (2), and crude touch (3)
Anterolateral system
_________ (tract): pathway of the anterolateral system that functions in discrimination of location & intensity of $ ("sharp pain in my heel, hot water on my hand")
Spinothalamic
_________ (tract): pathway of the anterolateral system that functions in emotional & arousal aspects to medulla-pontine reticular formations ("ouch, that hurts")
Spinoreticular
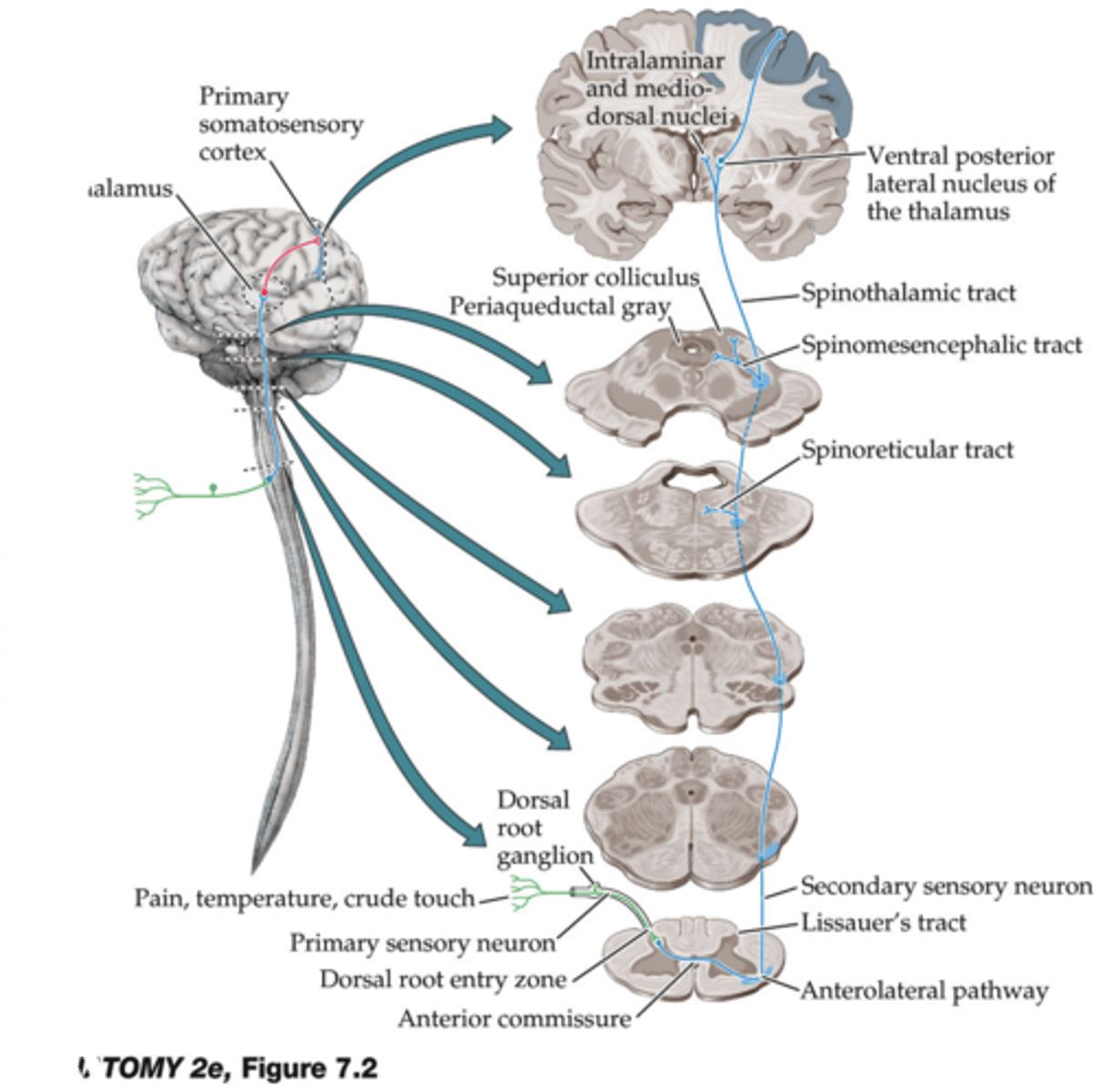
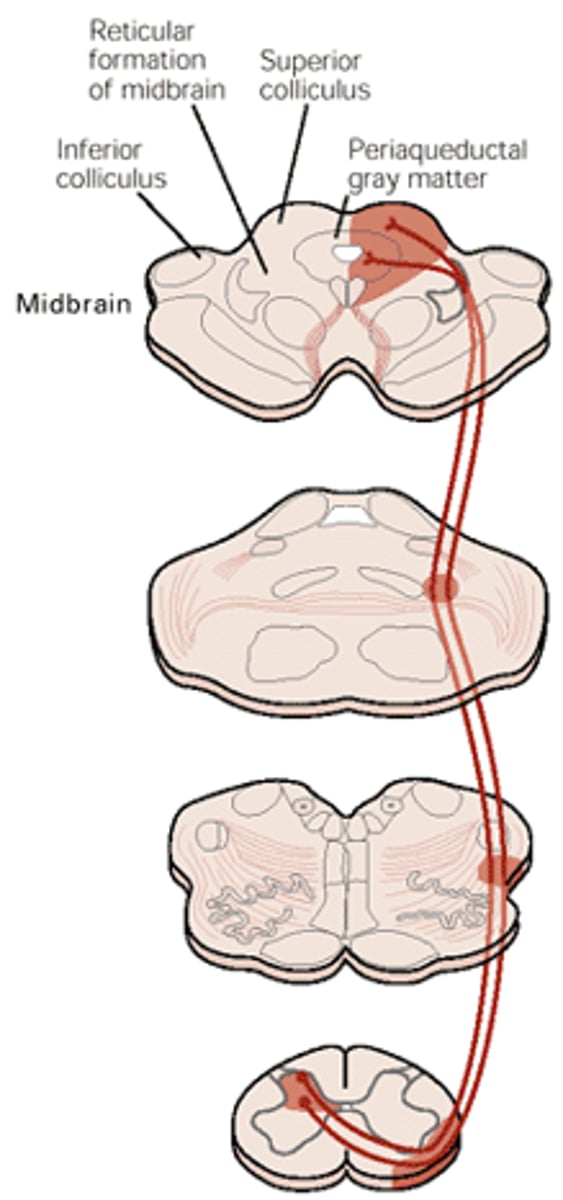
_________ (tract): pathway of the anterolateral system that functions in central modulation of $ to the periaqueductal gray ("aah, that feels better")
Spinomesencephalic
_________ (tract): unconscious proprioception
Dorsal/ventral spinocerebellar tracts
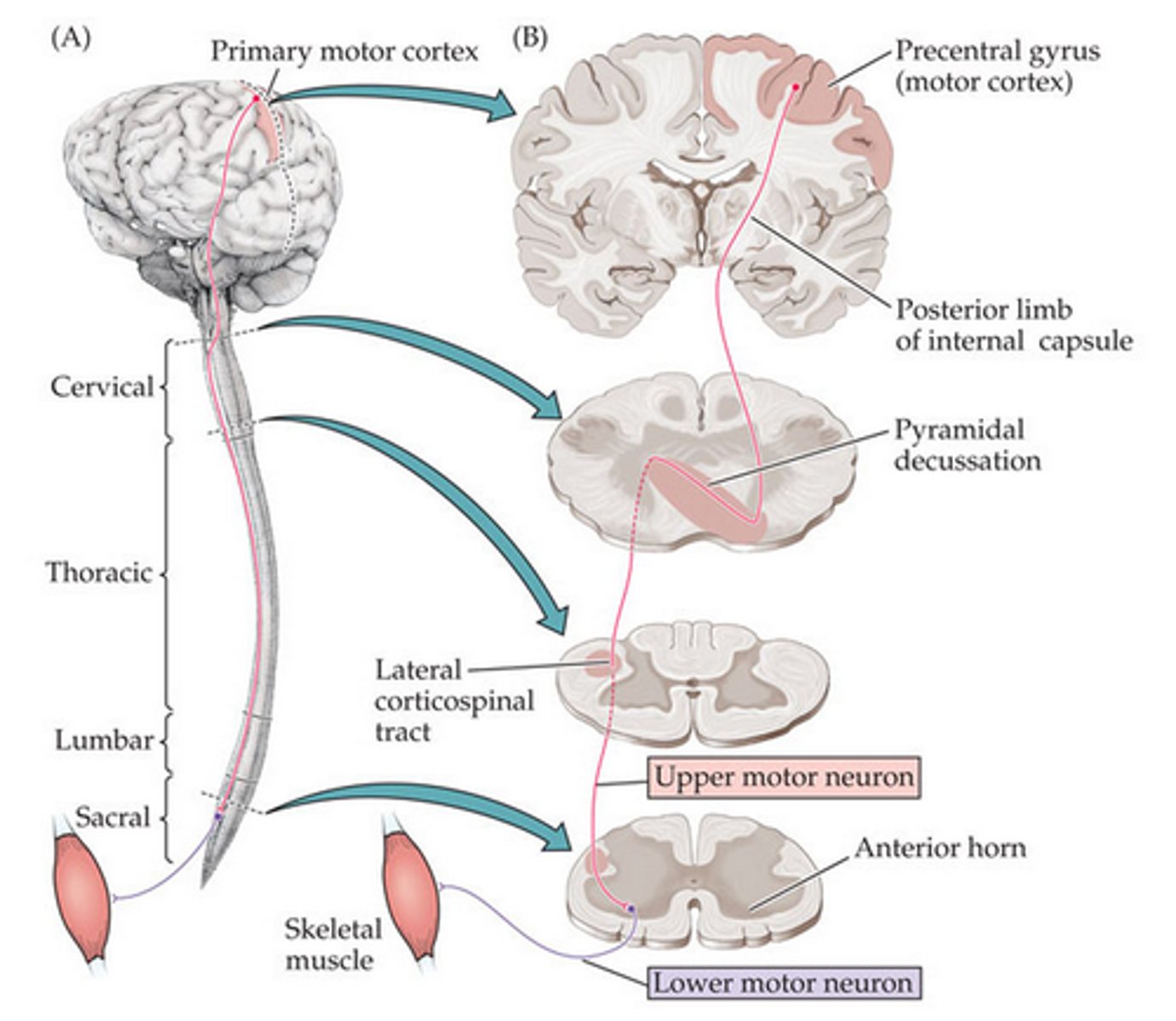
_________ (tract): voluntary movement of the contralateral limbs
Lateral corticospinal
_________ (tract): unconscious movements of limbs; posturing
Rubrospinal
_________ (tract): voluntary trunk control and proximal girdle muscles
Anterior corticospinal
_________ (tract): positioning of head and neck via vestibular input
Medial vestibulospinal
_________ (tract): balance via promotion of antigravity postural control and protective extension
Lateral vestibulospinal
_________ (tract): coordination of head and eye movement via visual and auditory info
Tectospinal
_________ (tract): automatic posture and gait-related movements
Rubrospinal
_________: most caudal level with BOTH motor and sensory function
Neurological level of injury (NLI)
Motor level: lowest myotome with a key muscle MMT score >________
>3
Sensory level: most caudal level w/ normal _________ AND _________ sensation
Light touch and pin prick
How do you test light touch?
Q-tip w/ a 3-point scoring system (0: absent, 1: impaired, 2: normal)
How do you test pinprick?
Use of "dull" or "sharp" with safety pin w/ a similar scoring system to light touch
Key muscles chosen for motor testing have ______ levels of innervation for more valid testing
2 levels
How is motor testing scored?
Same as MMT with 0-5, NO (+) or (-)
What are the 5 key muscles of the upper body?
Elbow flexors/extensors, wrist extensors, finger flexors and finger abductors
What are the 5 key muscles of the lower body?
Hip flexors, knee extensors, ankle DF, long toe extensors, and ankle PFs
Which sacral segments determine if an injury is complete?
S4-5
How do you test sensation of the sacrum?
Deep anal pressure
How do you test motor control of the sacrum?
Voluntary anal sphincter contraction
To be considered an incomplete injury, there must be sacral sparing of what?
Either sensory OR motor
According to the ASIA impairment scale, ______ = no motor/sensory S4-5
ASI A Complete
According to the ASIA impairment scale, ______ = no motor preserved >3 levels below motor level bilaterally AND sensory preserved below neurological level and S4-5
ASI B Sensory Incomplete
According to the ASIA impairment scale, ______ = motor preserved S4-5 OR sparing of motor function >3 levels on one side of the body AND sensory preservation S4-5
ASI C Motor Incomplete
According to the ASIA impairment scale, ______ = AIS C with at least half or more of key muscles below neurological level w/ MMT >3
ASI D Motor Incomplete
According to the ASIA impairment scale, ______ = normal (must have an initial SCI/deficits)
ASI E Normal
According to the ASIA impairment scale, ______ = examination is inconclusive
ASI ND Not Determined
_________: no motor/sensory function at S4-5; the areas of intact motor and/or sensory function below neurological level of injury
Zones of partial preservation
_________: complete areflexia in first 24 hours after SCL --> loss of reflexes, hypotension, piloerection, loss of sweating
Spinal shock (essentially an immediate loss of functions below the level of injury)
As swelling decreases after SCI, a gradual return of _______ will occur within 1-3 days, BUT a ________ in hyperreflexia for 1-4 weeks will occur
function, increase (system has to balance itself out)
_________: pathological LIFE-THREATENING occurrence that involves severe hypertension
Autonomic dysreflexia (AD)
What causes AD?
Normally, afferent input --> lower SC --> reflex results in elevated BP --> $ receptors in carotid sinus and aorta --> vasomotor center in CNS $ and sends message to adjust peripheral resistance --> BP decreases
W/ AD, the CNS never sends the message to adjust peripheral resistance, so the input is not received and BP continues to rise
What are the major consequences of AD?
Seizures, cardiac arrest, subarachnoid hemorrhage, stroke or death
Consider AD if: BP increase of >_____-_____ mmHg
20-30 mmHg (remember, individuals w/ SCI have lower resting BP so "textbook" BP may be high)
**AD occurs mostly in lesions above _______
T6 (greater splanchnic nerve is innervated by T5-T9 and contributes to sympathetic innervation)
When does AD most often occur? (timeline? complete vs incomplete?)
3-6 months post-injury, complete > incomplete
How do we intervene if an individual is experiencing AD?
Sit the individual upright to capitalize on orthostatic hypotension, monitor vitals, find the source of the noxious $
What is the #1 cause of noxious $ in AD?
Catheter blockage (others include: full bladder, tight clothing, sharp object, abdominal binder, E-stim, labor and delivery, sex)
_________: velocity-dependent increase in resistance to passive stretch due to UMN syndrome
Spasticity
Greatest spasticity occurs in first ______ months after SCI, but it plateaus at a year to inform prognosis
6 months (easily triggered by environmental/stress factors; helps OR hinder functional mobility)
What medications are prescribed to patients with spasticity?
Muscle relaxants (baclofen, dantrolene, diazepam), intrathecal baclofen, botox
What are therapeutic interventions for spasticity?
TENS (sensory input to calm the muscle), PROM
The leading cause of death in chronic SCI is _________
Cardiovascular disease
What are the WHO guidelines for exercise following an SCI?
20 min mod-to-vig exercise 2x/wk AND 3 strength training for major muscle groups 2x/wk (fitness)
30 min of mod-to-vig AEROBIC activity 3x/wk (cardiometabolic health)
In individuals w/ a cervical level of injury, they will have a ______ HR at rest with a max HR of _________ with activity...what does this mean clinically?
Low HR, 110-120 bpm -- you can't really use HR as an indication of intensity, so use RPE
True or false: In individuals w/ a thoracic/lumbar level of injury, they will have a HR that matches age-matched norms
True!!
Orthostatic hypotension: decrease >____/____ mmHg from NORMAL BP within _______ minutes of sitting upright or standing
>20/10 mmHg, 3 minutes
What is the cause of orthostatic hypotension?
Pooling with lack of muscle pumps in LE, altered baroreceptor sensitivity, poor sympathetic control (T2-L6) and decreased upright tolerance
What are some S/S of orthostatic hypotension? (hint: x5)
Lightheaded or feeling faint, pale or "out of it," nausea or feeling unwell, blurred vision, ringing in ears
How should you intervene if a patient is experiencing orthostatic hypotension?
Lower from sitting or standing --> supine w/ legs elevated (others include: massage calves to create manual muscle pump, trial abdominal binder or TED hose, medication)
How should upright activity tolerance be gradually progressed?
1. Raise the head of the bed
2. Recline WC w/ elevating leg rests
3. Standing frame or tilt table
4. Eventually upright manual WC
5. Standing or gait
Respiratory impact: C1-2
Mechanical ventilation
Respiratory impact: C3-4
Initial mechanical ventilation until spontaneous respiration returns
Respiratory impact: C5-8
Intact diaphragm w/ weak cough
What are possible complications that coincide with the respiratory impact of SCI?
Difficulty speaking, tracheostomy, unable to cough effectively
True or false: patients post-SCI have poor temperature control
True!! This results in an increased risk of hypothermia and hyperthermia
Patients post-SCI are also unable to ID hot or cold below the sensory level, so what should you educate them on?
Hot and cold packs, seat heaters and vents in cars, sunscreen, hydration and shade
_________: formation of bone in soft tissues, usually near joints, below level of the lesion
Heterotropic ossification
What are S/S of heterotropic ossification?
Swelling, pain across muscle or joint, warmth near joint, decrease ROM, low grade fever
To treat heterotropic ossification, avoid _________
Overstretching
To prevent pressure injuries in SCI, what should we educate our patients on?
Weight shifts!!
Micturition, the process of voiding urine, is controlled by _________
S2-4
Injury ABOVE S2 results in _________ bladder, while an injury BELOW S2 results in _________ bladder
Spastic or hyperreflexic, flaccid or areflexic
W/ spastic/hyperreflexic bladder, the reflex arc is intact but overactive and the sphincter may have increased tone....what muscle may have a poor coordination with the sphincter?
Detrusor
What is the initial intervention for spastic/hyperreflexic OR flaccid/areflexic bladder?
Catheterization (external condom catheter, suprapubic catheter, and intermittent catheterization later on)
While spastic bladder may result in urine retention (higher risk for UTI), flaccid bladder may lead to ___________
Urinary incontinence
Normal bowel movements occur w/ the following innervation:
- Sympathetic control of colon/rectum: ________
- Parasympathetic control of colon/rectum: _______
T9-L2 (symp), S2-4 (parasymp)
SCI above S2 --> _________ bowel, while SCI at or below S2 --> __________ bowel (note: this is a similar relationship to bladder)
Reflexic (increased tone), areflexic (reduced tone --> incontinence)
W/ a reflexic bowel, suppositories and digital $ are used to elicit a _________
Reflex (note: abdominal massage w/ Valsalva is also beneficial as part of a daily bowel program)
W areflexic bowel, there needs to be digital $ or ___________ as part of a daily bowel program
Manual evacuation (note: fiber, fluid, PA, stool softeners, laxative, and bulking agents may also be beneficial)
Should/should not: BBM program in individuals w/ both reflexic and areflexic NBD
SHOULD!!

Should/should not: the optimal frequency of bowel movements per week should account for an individual's lifestyle and premorbid bowel hx
SHOULD!!

Should/should not: mechanical rectal $ for individuals w/ reflexic NBD
SHOULD!!

Should/should not: manual evacuation of stool for individuals w/ areflexic NBD
SHOULD!!

Should/should not: abdominal massage for NBD emptying
SHOULD NOT

Should/should not: Valsalva maneuver for NBD emptying
SHOULD NOT

Should/should not: use of adaptive equipment, including a suppository inserter and adaptive digital stimulator, for individuals with limited hand function or difficulty with reach
SHOULD!!

Should/should not: clinical eval of a commode/shower chair w/ a focus on the individual's current bowel care routine and transfer ability, goals, and individual funcitonality
SHOULD!!

Should/should not: regular PA encouraged as part of a healthy lifestyle
SHOULD!!

Should/should not: standing program for bowel function weighted against other means of PA, as well as against precautions to undertake the activity safely
SHOULD!!

Should/should not: education for individuals w/ SCI, caregivers, and health care providers that is comprehensive to all levels of learneres
SHOULD!!

Should/should not: teach components of the bowel program to individuals w/ an SCI as well as caregivers
SHOULD!!

Should/should not: education on potential complications
SHOULD

Should/should not: education and support for the caregiver considered and completed when appropriate
SHOULD!!

Should/should not: sexual intimacy and considerations related to BBM discussed
SHOULD!!

Should/should not: include psychosocial aspects that are barriers to learning the bowel program in the assessment of NBD, such as cognition, depression, anxiety, pain, literacy, language, and ethnic or cultural issues
SHOULD!!

Should/should not: if an individual w/ SCI is having multiple problems with NBD or is noncompliant with the bowel program, a formal screening tool should be used to assess depression, anxiety, and QOL
SHOULD!!

True or false: individuals w/ SCI expect their health care team to educate on sexual and reproductive health
TRUE!! (in fact, sex remains the highest priority for individuals who are paraplegia and second highest for those w/ tetraplegia)
Psychogenic erection comes from _________ pathways
T11-12 (so, intact below T11)
Reflexogenic erection comes from __________ pathways
S2-4 (may lose this ability w/ injury @ S2-4, BUT can still be treated w/ medications)
Men w/ injuries _______ may have preserved psychogenic and reflexogenic erection BUT poorly coordinated during sex
L3-S1