Psychopharmacology
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
Define tolerance.
Needing more of the drug to get the same effect.
Define sensitization.
Feeling a stronger effect every time you take the drug.
Define withdrawal.
Symptoms that appear when you stop taking a drug cold turkey (usually the opposite of the drug’s effects).
Define placebo.
An inactive substance that doesn’t do anything on its own, but can if you believe it will.
Identify and describe the three main mechanisms of drug action.
Agonistic: Makes the NT stronger by mimicking it.
Antagonistic: Blocks the NT.
Reuptake Inhibition: Keeps the NT in the synapse for longer.
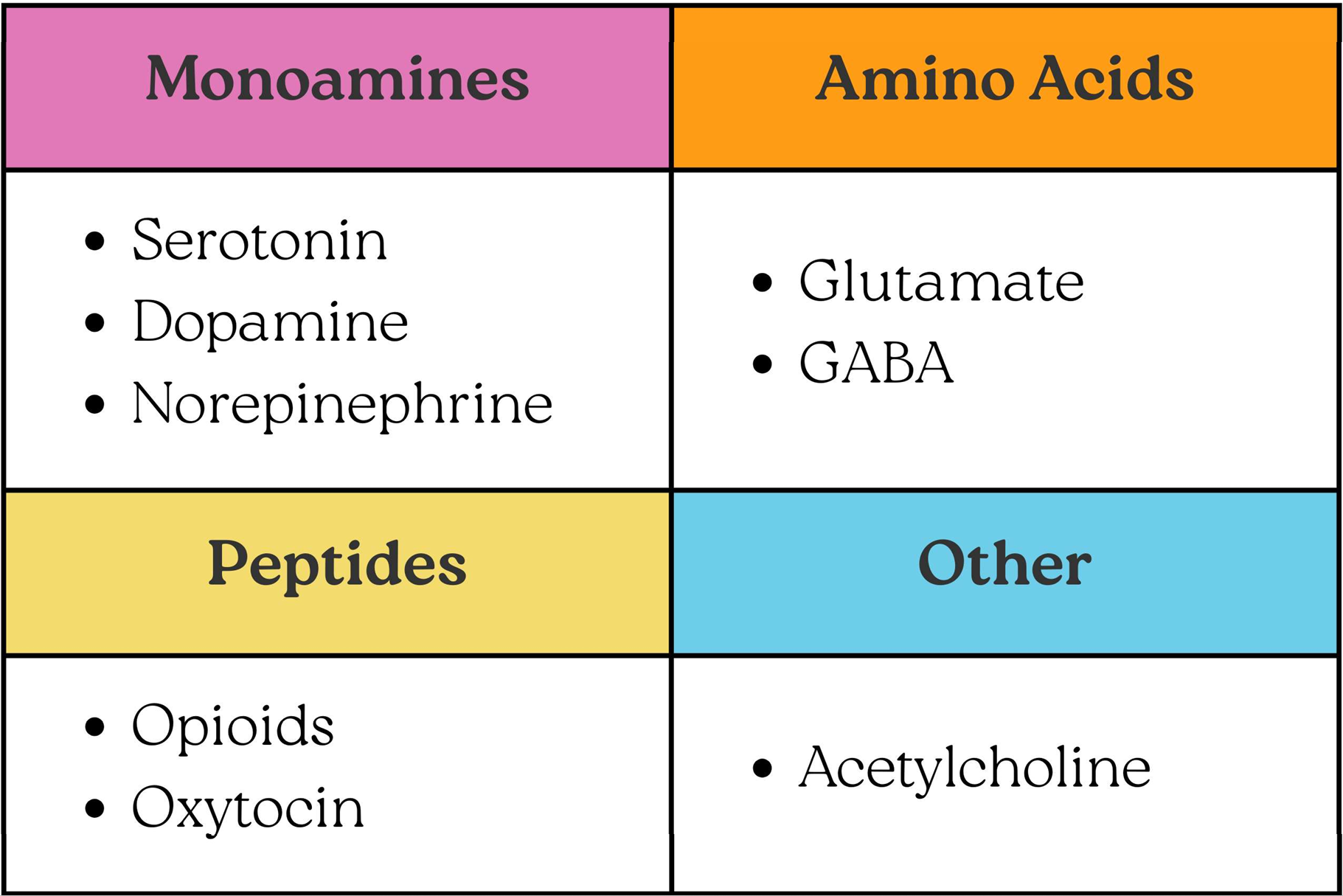
Provide a brief overview of neurotransmitter classification.
Describe the functions of serotonin and identify disorders associated with serotonin dysregulation.
Functions: Inhibitory monoamine NT involved in mood, appetite, sleep, impulse control, obsessive thinking, and sexual functioning.
Associated Disorders: Mood, anxiety, eating, and paraphilic disorders, OCD, and PTSD.
Describe the functions of dopamine and identify disorders associated with dopamine dysregulation.
Functions: Inhibitory / excitatory monoamine NT involved in mood, personality, reward centre*, and movement*.
Associated Disorders: Substance use, psychotic, and mood disorders.
* Nucleus Accumbens is our reward centre.
* Substantia Nigra → Striatum is the key dopamine pathway for movement.
Describe the functions of norepinephrine and identify disorders associated with norepinephrine dysregulation.
Functions: Excitatory monoamine NT involved in arousal / alertness, mood, and stress (fight-or-flight).
Associated Disorders: Mood disorders and PTSD.
Describe the functions of glutamate and identify disorders associated with glutamate dysregulation.
Functions: Excitatory AA NT involved in movement, emotion, learning, and memory.
Associated Disorders: AD and mood disorders.
Describe the functions of GABA and identify disorders associated with GABA dysregulation.
Functions: Inhibitory AA NT involved in memory, mood, sleep, and motor control.
Associated Disorders: Anxiety disorders and PTSD.
Identify and describe medications classified as antidepressants, including their mechanism of action, examples, clinical uses, and additional considerations.
Selective Serotonin Reuptake Inhibitors (SSRIs)
Mechanism of Action: ↑ Serotonin (via reuptake inhibition).
Examples: Fluoxetine (Prozac), Paroxetine (Paxil), Sertraline (Zoloft).
Clinical Uses: Depressive, anxiety, eating, and paraphilic disorders, PTSD, and OCD.
Considerations: Safest / least side effects.
Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs)
Mechanism of Action: ↑ Serotonin & Norepinephrine (via reuptake inhibition).
Examples: Venlafaxine (Effexor), Duloxetine (Cymbalta).
Clinical Uses: MDD (esp. if severe), anxiety disorders, and PTSD.
Considerations: Might not be good for patients with hypertension / high BP.
Tricyclic Antidepressants (TCAs)
Mechanism of Action: ↑ Serotonin & Norepinephrine (via reuptake inhibition).
Examples: Amitriptyline (Elavil), Imipramine (Tofranil), Clomipramine (Anafranil).
Clinical Uses: MDD, OCD.
Considerations: Side effects can be pretty bad and overdose is lethal.
Monoamine Oxidase Inhibitors (MAOIs)
Mechanism of Action: ↑ Serotonin, Norepinephrine, and Dopamine (via breakdown of MAO enzyme).
Examples: Phenelzine (Nardil), Isocarboxazid (Marplan).
Clinical Uses: Treatment resistant depression.
Considerations: MAO also breaks down tyramine, because tyramine can raise BP. If we inhibit MAO, this may trigger a hypertensive crisis.
Identify and describe medications classified as antipsychotics, including their mechanism of action, examples, clinical uses, and additional considerations
1st Generation / Conventional Antipsychotics
Mechanism of Action: ↓ Dopamine (via antagonistic action of D2 receptors).
Examples: Chlorpromazine (Thorazine), Haloperidol (Haldol).
Clinical Uses: Schizophrenia.
Considerations: Can cause severe side effects, such as extra-pyramidal symptoms, tardive dyskinesia, grogginess, difficulties thinking, and blurred vision.
2nd Generation / Atypical Antipsychotics
Mechanism of Action: ↓ Dopamine (via antagonistic action of D3 / D4 receptors).
Examples: Clozapine (Clozaril), Risperidone (Risperdal), Olanzapine (Zyprexa).
Clinical Uses: Schizophrenia, atypical bipolar, and weight gain for anorexia.
Considerations: Side effects less severe than 1st gen.
Identify and describe medications classified as mood stabilizers, including their mechanism of action, examples, clinical uses, and additional considerations.
Lithium & Anticonvulsants (e.g., valproic acid).
Mechanism of Action: Helps with mood instability by calming down unstable patterns of neural firing.
Clinical Uses: Bipolar disorders / mania.
Additional Considerations: Requires ongoing blood-level monitoring for lithium toxicity and agranulocytosis (low WBC).
Identify and describe medications classified as benzodiazepines (anxiolytics), including their mechanism of action, examples, clinical uses, and additional considerations.
Mechanism of Action: ↑ GABA (via agonistic action).
Examples: Diazepam (Valium), Alprazlam (Xanax), Lorazepam (Ativan).
Clinical Uses: Anxiety disorders and alcohol withdrawal.
Considerations: Doesn’t address the root cause of anxiety, highly addictive, and tolerance builds quickly.
Identify which psychological disorders respond well to medication treatment.
Bipolar disorder / mania.
Schizophrenia.
Identify which psychological disorders do not typically respond well to medication treatment.
PTSD.
Social Anxiety Disorder.
Eating Disorders.