CH 12-13
1/152
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
153 Terms
shock/hypoperfusion
____/_____ describes a state of collapse and failure of the cardiovascular system.
-In the early stages, the body attempts to maintain homeostasis.
-As it progresses, blood circulation slows and eventually ceases.
cardiovascular
homeostasis
slows ceases
shock/hypoperfusion describes a state of collapse and failure of the _____ system.
-In the early stages, the body attempts to maintain _____.
-As it progresses, blood circulation _____ and eventually _____ .
medical
traumatic
•Shock can occur because of ______ or ______ events.
-Heart attack
-Severe allergic reaction
-Motor vehicle crash
Gunshot wound
Perfusion
circulatory
oxygenation
_______ is the circulation of an adequate amount of blood to meet the cells' current needs.
-The body is perfused via the _______ system.
-Organs, tissues, and cells must have adequate _________ or they may die.
systemic
________ circulation carries oxygen-rich blood from the left ventricle through the body and back to the right atrium.
carbon dioxide
cellular damage
•In cases of poor perfusion (shock):
-Transportation of ____ _____ out of tissues is impaired.
-Results in a dangerous buildup of waste products, which may cause ____ ____
bicarbonate
- Carbon dioxide waste products released from cells can combine with water in the bloodstream to form ______ .
- the concentrations become higher as more carbon dioxide is produced and blood moves back toward the lungs.
- Once it reaches the lungs, it breaks back down into carbon dioxide and water and the carbon dioxide is exhaled.
heart
blood vessel arteries
blood
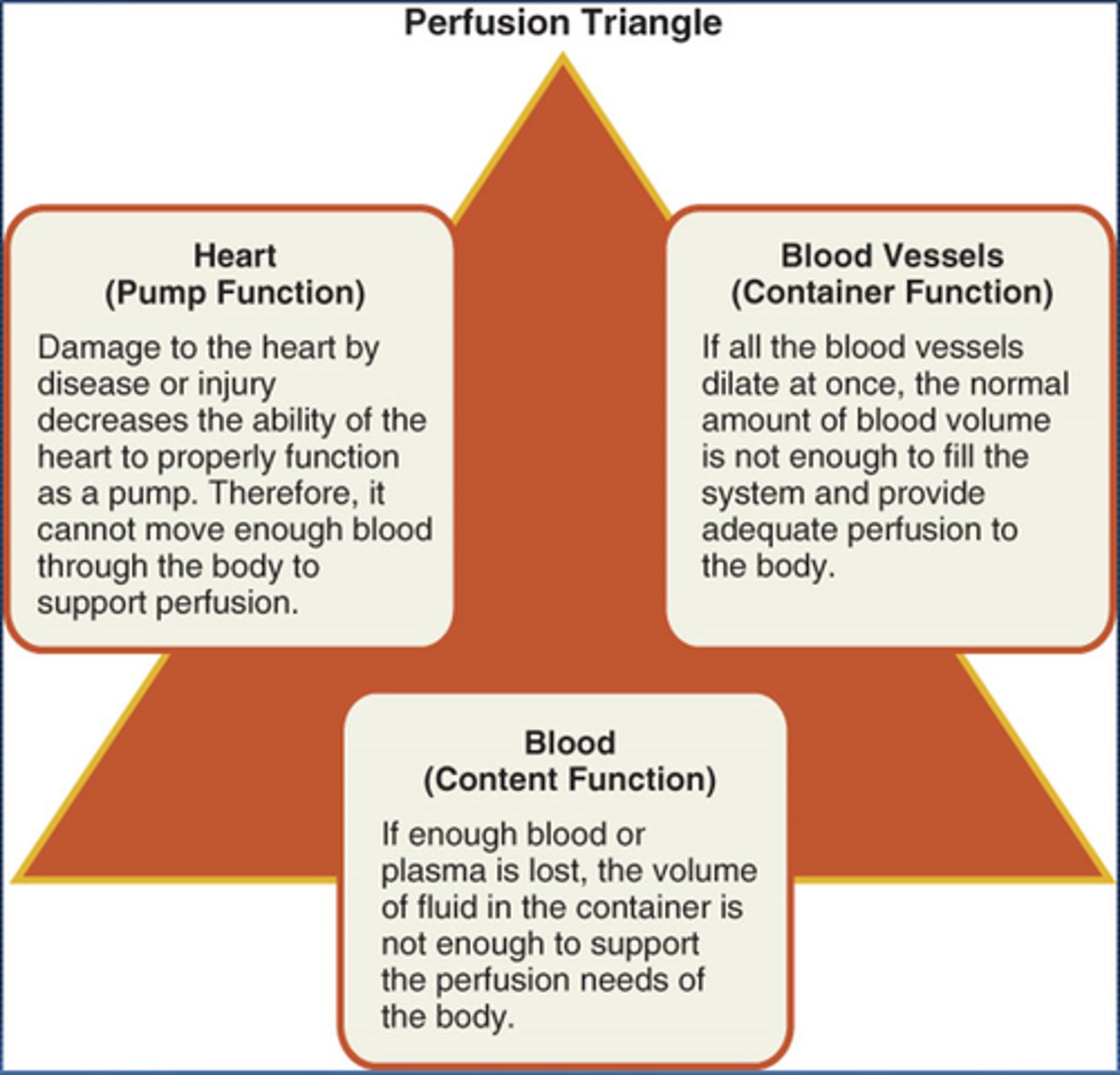
•Cardiovascular system/perfusion triangle consists of three parts:
-Pump (______)
-container/pipes (_______ ______/_____)
- Contents (the _____)
perfusion triangle
The heart (the pump)
The pipes (blood vessels or arteries)
The contents of container (blood)
When a person is in shock one or more of these will not work properly
blood pressure
___ ____ is the pressure of blood within the vessels at any moment in time
systolic
___ pressure is the peak arterial pressure, or pressure generated every time the heart contracts.
diastolic
____ pressure pressure is the pressure maintained within the arteries while the heart rests between heartbeats.
pulse
25
____ •pressure is the difference between the systolic and diastolic pressures.
- signifies the amount of force the heart generates with each contraction
- < ____mmg Hg may be seen in patients with shock
capillary sphincters
autonomic
•Blood flow through the capillary beds is regulated by the _____ ____
-Under the control of the _______ nervous system
-respond to other stimuli:
•Heat
•Cold
•The need for oxygen and waste removal
heat cold oxygen waste
-Capillary sphincters respond to other stimuli:
•____
•_____
•The need for _____ and _____ removal
oxygen exchange
nutrients glucose
waste removal
•Perfusion requires more than just having a working cardiovascular system.
-Adequate_____ ____ in the lungs
-Adequate ____ in the form of ______ in the blood
-Adequate ____ _____, primarily through the lungs
autonomic
hormones
•Mechanisms are in place to help support the respiratory and cardiovascular systems when the need for perfusion of vital organs is increased.
-Mechanisms include the ______ nervous system and _______.
epinephrine
norepinephrine
pressure
perfusion
hormones like ______ and ______ triggered when the body senses pressure falling.
-Cause an increase in:
•Heart rate
•Strength of cardiac contractions
•Peripheral vasoconstriction
•these actions are designed to
-Maintain _____ in the system
-Sustain ______ of all vital organs
•It is this response that causes all the signs and symptoms of shock.
HR
cardiac contractions
Peripheral vasoconstriction
hormones like epinephrine and norepinephrine triggered when the body senses pressure falling.
-Cause an increase in:
•____ ____ (Abrv)
•Strength of ____ _____
•____ ____
shock
perfusion
____ •can result from bleeding, respiratory failure, acute allergic reactions, and overwhelming infection.
-Damage occurs because of insufficient ______ of organs and tissues.
pump failure
_____ _____ causes these
.Cardiogenic shock
Obstructive shock
- Tension pneumothorax
- Cardiac tamponade
- Pulmonary embolism
poor vessel
____ _____ function causes
Distributive shock
- Septic shock
- Neurogenic shock
- Anaphylactic shock
- Psychogenic shock
low fluid
____ ___ volume causes
Hypovolemic shock
- Hemorrhagic shock
- Nonhemorrhagic shock
Cardiogenic
_______ shock
•Caused by inadequate function of the heart
•A major effect is the backup of blood into the lungs.
•Resulting buildup of pulmonary fluid is called pulmonary edema.
heart
backup
pulmonary edema
Cardiogenic shock
•Caused by inadequate function of the _____
•A major effect is the ______ of blood into the lungs.
•Resulting buildup of pulmonary fluid is called ____ ____
pulmonary edema
____ ____ is tje buildup of pulmonary fluid
• leads to impaired respiration, which may be manifested by:
-An increased respiratory rate
-Abnormal lung sounds
edema
_______ is the presence of abnormally large amounts of fluid between the cells in body tissues, causing swelling of the affected area.
cardiogenic
______ shock develops when the heart cannot maintain sufficient output to meet the demands of the body
obstructive
_______ shock
•Caused by a mechanical obstruction that prevents an adequate volume of blood from filling the heart chambers.
•Three of the most common examples:
-Cardiac tamponade
-Tension pneumothorax
Pulmonary embolism
Cardiac tamponade
Tension pneumothorax
Pulmonary embolism
obstructive shock
•Caused by a mechanical obstruction that prevents an adequate volume of blood from filling the heart chambers.
•Three of the most common examples:
- ____ ____
- ____ ____
- _____ _____
cardiac tamponade
_____ _____
-Collection of fluid between the pericardial sac and the myocardium (pericardial effusion) becomes large enough to prevent ventricles from filling with blood.
-Caused by blunt or penetrating trauma
-Signs and symptoms are referred to as Beck triad.
beck triad
____ ___ refers to signs and symptoms of cardia tamponade
- presence of jugular vein distention
- muffled heart sounds
- narrowing pulse pressure where the systolic and diastolic blood pressures start to merge.
pericardial sac
myocardium
ventricles
cardiac tamponade
-Collection of fluid between the ____ ____ and the _____ (pericardial effusion) becomes large enough to prevent _____ from filling with blood.
-Caused by blunt or penetrating trauma
-Signs and symptoms are referred to as Beck triad.(presence of jugular vein distention, muffled heart sounds, and a narrowing pulse pressure where the systolic and diastolic blood pressures start to merge._
pericardium
pericardial sac
Cardiac tamponade occurs when blood leaks into the space between the tough fibrous membrane known as the _______ and the outer walls of the heart, an area called the ____ ___
tension pneumothorax
-Caused by damage to lung tissue
-The air normally held within the lung escapes into the chest cavity.
-The lung collapses, and air applies pressure to the organs, including the heart and great vessels.
lung
chest
pump
tension pneumothorax
-Caused by damage to _____ tissue
-The air normally held within the lung escapes into the _____ cavity.
-The lung collapses, and air applies pressure to the organs, including the heart and great vessels.
- _____ failure
pulmonary embolism
-A blood clot that blocks the flow of blood through pulmonary vessels
-If massive:
•Can result in complete backup of blood in the right ventricle
•Leads to catastrophic obstructive shock and complete pump failure
blood clot
pulmonary
right ventricle
pump
catastrophic obstructive
-A ___ ____ that blocks the flow of blood through _____ vessels
-If massive:
•Can result in complete backup of blood in the ____ ____
•Leads to ____ ____ shock and complete _____ failure
distributive
______ shock
•Results from widespread dilation of small arterioles, small venules, or both (vessel)
•The circulating blood volume pools in the expanded vascular beds.
- Tissue perfusion decreases.
vessel
vascular beds
perfusion
distributive shock
•Results from widespread dilation of small arterioles, small venules, or both (_______ shock)
•The circulating blood volume pools in the expanded ______ _______
- Tissue _______ decreases.
septic
_______ shock
-Occurs as a result of severe infections in which toxins are generated by bacteria or by infected body tissues.
-Toxins damage vessel walls, causing increased cellular permeability.
-Vessel walls leak and are unable to contract well.
-Widespread dilation of vessels, in combination with plasma loss through the vessel walls, results in shock.
infection
toxins
vessel
permeability
contract
dilation
plasma
septic shock
-Occurs as a result of severe ______ in which _____ are generated by bacteria or by infected body tissues.
-Toxins damage _____ walls, causing increased cellular ______ .
-Vessel walls leak and are unable to ______ well.
-Widespread _____ of vessels, in combination with _____ loss through the vessel walls, results in shock.
neurogenic
_______ shock
-Usually the result of high spinal cord injury
-Causes include:
•Brain conditions
•Tumors
• Pressure on the spinal cord
Spina bifida
-Muscles in the blood vessels walls are cut off from the nerve impulses that cause them to contract.
vessel
contract
neurogenic shock
-Usually the result of high spinal cord injury
-Causes include:
•Brain conditions
•Tumors
• Pressure on the spinal cord
Spina bifida
-Muscles in the blood _____ walls are cut off from the nerve impulses that cause them to _____ .
anaphylactic
_______ shock
-Occurs when a person reacts violently to a substance to which he or she has been sensitized.
-Sensitization means becoming sensitive to a substance that did not initially cause a reaction.
-Each subsequent exposure tends to produce a more severe reaction.
anaphylactic
injection
sting
ingestion
inhalation
•_______ shock
-Four categories of exposure include:
•_____(tetanus antitoxin, penicillin)
•_______(wasps, bees, hornets, ants)
•______(fish, shellfish, nuts, eggs, medication)
•_______(dust, pollen, mold)
Anaphylactic
Cyanosis
•______shock
-Develops within minutes or even seconds of contact with substance
-Second phase reaction can occur 1 to 8 hours after initial reaction.
-Signs are very distinct.
-______(blue discoloration of skin) is a late sign.
_______ shock
psychogenic
_______ shock
-Caused by a sudden reaction of the nervous system.
-Produces temporary, generalized vascular dilation
-Results in fainting (syncope)
-Some causes are serious and others are not.
NS
vascular
syncope
heartbeat
aneurysm
psychogenic shock
-Caused by a sudden reaction of the _______ (abrv)
-Produces temporary, generalized _______ dilation
-Results in fainting (_______)
-Some causes are serious and others are not.
-Life-threatening causes include irregular ______ and brain ______.
-Non-life-threatening events include receipt of bad news or experiencing fear or unpleasant sights (such as blood).
hypovolemic
circulatory
Hemorrhagic
thermal
Intravascular
Dehydration
_______ shock
•Result of an inadequate amount of fluid or volume in the ______ system
•________ causes and nonhemorrhagic causes
•Occurs with severe ______ burns
-_________plasma is lost.
•________, the loss of water or fluid from body tissues, can cause or aggravate shock.
Fluid loss may be a result of severe vomiting and/or diarrhea.
respiratory insufficiency
____ ____
•A patient with a severe chest injury may be unable to breathe in an adequate amount of oxygen.
-An insufficient concentration of oxygen in the blood can produce a life-threatening situation as rapidly as vascular causes of shock.
anemia
_____ is an abnormally low number of red blood cells.
hypoxia
_____ occurs because blood is unable to deliver adequate amounts of oxygen to the tissues.
carbon monoxide
cyanide
•Certain types of poisoning may affect the ability of cells to metabolize or carry oxygen:
-___ ___poisoning
-____ poisoning
compensated
decompensated
•The stages in the progression of shock:
-______ shock: early stage when the body can still compensate for blood loss
-______ shock: late stage when blood pressure is falling
-No way to assess when effects are irreversible
Must recognize and treat shock early
compensated
_____ shock signs and symptoms
1. agitation
2. anxiety
3. restlessness
4. feeling of impending doom
5. altered mental status
6. weak, rapid (thready), or absent pulse
7. clammy skin
8. pallor with cyanosis about the lips
9. shallow, rapid breathing
10. air hunger (SOB), esp. if there is a chest injury
11. nausea or vomiting
12. capillary refill longer than 2 sec. in infants and children
13. marked thirst
14. narrowing pulse pressure
decompensated
_____ shock signs and symptoms
1. falling BP (sys. BP of 90 mm Hg or lower in adult)
2. labored or irregular breathing
3. ashen, mottled, or cyanotic skin
4. thready or absent peripheral pulses
5. dull eyes, dilated pupils
6. poor urinary output
BP
• ___ (abrv) may be the last measureable factor to change in shock.
-When a drop in blood pressure is evident, shock is well developed.
-Particularly true in infants and children
-Expect shock in many emergency medical situations
fractures
abdomoninal/chest
spinal infection
heart attack
anaphylaxis
•Also expect shock if a patient has any one of the following conditions:
-Multiple severe _____
-_____/_____ injury
-_____injury
-A severe _____
-A major _____ _____
-_____
oxygen
hypoperfusion
ALS
airway
breathing
shock
circulatory
rapid pulse
high priority
trauma
•Primary assessment of shock
-Provide high-flow ____ to assist in perfusion
-For ______, treat aggressively and provide rapid transport
-Request _____ (abrv) as necessary
-Form a general impression.
-Assess the _____ to ensure it is patent.
-Assess ______ .
-An increased respiratory rate is often an early sign of impending ____.
Assess patient's _____ status.
-A ____ ____ suggests compensated shock.
-In shock or compensated shock, the skin may be cool, clammy, or ashen.
-Assess for and identify any life-threatening bleeding and treat it at once.
-Determine if patient is _____ ___, if ALS is needed, and which facility to transport to.
-Trauma patients with shock or a suspicious MOI generally should go to a ____ center.
vital
monitoring
•Secondary assessment
-Begins by repeating the primary assessment, followed by focused assessment
-If a life-threatening problem is found, treat it immediately.
-Obtain a complete set of baseline ____ signs.
-Use _____ devices.
cardiovascular
oxygen
warm
reassessment
-Determine what interventions are needed.
-Focus on supporting the _____ system.
-Treat for shock early and aggressively by:
•Providing ____
•Keeping the patient _____
bleeding
open airway
stabilization
breathing pulse
spinal
backboard
•As soon as you recognize shock, begin treatment.
-Follow standard precautions.
-Control all obvious _____.
-Make sure the patient has an ____ ____
-Maintain manual in-line _____ if necessary, and check ____ and ____.
-Comfort, calm, and reassure the patient.
-Never allow patients to eat or drink anything prior to being evaluated by a physician.
-If ____ immobilization is indicated, splint the patient on a ____.
Provide oxygen and monitor patient's breathing
chronic lung
nitroglycerin
hypotensive
•Patient cannot generate the power to pump blood throughout the circulatory system.
•____ ____ disease will aggravate cardiogenic shock.
•Patients in cardiogenic shock should not receive _____; they are _______.
low
weak
cyanosis
anxiety
nausea
high flow oxygen
ventilations
transport
ALS
heart attack
cardiogenic shock
•Patients usually have:
-____ blood pressure
-____ , irregular pulse
-_____ about lips/underneath fingernails
-___
-_____
•Place the patient in a position that eases breathing as you give ___ ____ _____
•Assist _____ as necessary.
•Provide prompt _____.
•Consider meeting _____ en route to hospital.
•Provide calm reassurance to a patient with a suspected ____ ____
cardiac output
high flow oxygen
surgery
pericardiocentesis
•For cardiac tamponade:
-Increasing ____ ____ is the priority.
-Apply ___ ____ ____
-____ is the only definitive treatment.
-_______ uses a needle to withdraw blood.
•Advanced skill; rarely performed in the field
hypoxia
chest decompression
•For tension pneumothorax:
-Apply high-flow oxygen to prevent _____.
-____ ____ is required.
-Ask for ALS early in call if available, but do not delay transport.
hospital
oxygen
ventilation
blankets
sepsis
treating septic shock
•____ management is required.
•Use standard precautions and transport.
•Administer high-flow ____ .
•____ support may be necessary.
•Use ____ to conserve body heat.
•Use "____ team" if available.
spinal cord
hospitalization
airway
immobilization
breathing
body heat
circulation
treating neurogenic shock
•For the ____ ____ injury patient, use a combination of all known supportive measures.
•____ will be required for a long time.
-Obtain and maintain a proper ____ .
-Provide spinal ____ .
-Assist inadequate ____ .
-Conserve ____ ____
-Ensure the most effective ____ .
-Transport promptly.
epinephrine
oxygen
ventilation
treating anaphylactic shock
•Administer _____ .
•Promptly transport the patient.
•Provide high-flow _____ and _____ assistance en route.
•A mild reaction may worsen suddenly.
•Consider requesting ALS backup, if available.
fainting
Psychogenic
treating **** shock
•In an uncomplicated case of _____ , once the patient collapses, circulation to the brain is restored.
•____________ shock can worsen other types of shock.
•If the patient falls, check for injuries.
•If the patient reports being unable to walk after a fall, suspect another problem.
-Transport the patient promptly.
-Record all initial observations and try to learn from bystanders:
•If the patient complained of anything
•How long the patient was unconscious
-
external
warm
internal
airway
treating hypovolemic shock
•Control all obvious _____ bleeding.
•Keep the patient ____ .
•Recognize ______ bleeding and provide aggressive support.
•Secure and maintain an _____ , and provide respiratory support.
•Transport as rapidly as possible.
airway
obstructions
BVM
supplemental oxygen
. Treating respiratory insufficiency
1. Immediately secure and maintain the _____.
2. Clear the mouth and throat of any _____, including mucus, vomitus, and foreign material.
3. If necessary, provide ventilations with a _____.
4. Administer _____ _____, and transport the patient promptly
mask/mimic
•The EMT must use caution when caring for older patients.
•Older patients have more serious complications than younger ones.
•Illness is not just a part of aging.
•Many older patients take medications that ____/____ signs of shock.
B
1.The term "shock" is MOST accurately defined as:
A.a decreased supply of oxygen to the brain.
B.cardiovascular collapse leading to inadequate perfusion.
C.decreased circulation of blood within the venous circulation.
D.decreased function of the respiratory system leading to hypoxia.
A
2.Anaphylactic shock is typically associated with:
A.urticaria.
B.bradycardia.
C.localized welts.
D.a severe headache.
D
3.Signs of compensated shock include all of the following, EXCEPT:
A.restlessness or anxiety.
B.pale, cool, clammy skin.
C.a feeling of impending doom.
D.weak or absent peripheral pulses.
C
4.When treating a trauma patient who is in shock, LOWEST priority should be given to:
A.spinal protection.
B.thermal management.
C.splinting fractures.
D.notifying the hospital.
C
5.Potential causes of cardiogenic shock include all of the following, EXCEPT:
A.inadequate heart function.
B.disease of muscle tissue.
C.severe bacterial infection.
D.impaired electrical system.
A
6.A 60-year-old woman presents with a BP of 80/60 mm Hg, a pulse rate of 110 beats/min, mottled skin, and a temperature of 103.9°F. She is MOST likely experiencing:
A.septic shock.
B.neurogenic shock.
C.profound heart failure.
D.a severe viral infection.
C
7.A patient with neurogenic shock would be LEAST likely to present with:
A.tachypnea.
B.hypotension.
C.tachycardia.
D.altered mentation.
D
8.A 20-year-old man was kicked numerous times in the abdomen during an assault. His abdomen is rigid and tender, his heart rate is 120 beats/min, and his respirations are 30 breaths/min. You should treat this patient for:
A.a lacerated liver.
B.a ruptured spleen.
C.respiratory failure.
D.hypovolemic shock.
A
9.A 33-year-old woman presents with a generalized rash, facial swelling, and hypotension approximately 10 minutes after being stung by a hornet. Her BP is 70/50 mm Hg and her heart rate is 120 beats/min. In addition to high-flow oxygen, this patient is in MOST immediate need of:
A.epinephrine.
B.rapid transport.
C.an antihistamine.
D.IV fluids._____
A
10.All of the following are potential causes of impaired tissue perfusion, EXCEPT:
A.increased number of red blood cells.
B.pump failure.
C.low fluid volume.
D.poor vessel function.
1960
International Liaison Committee on Resuscitation/ILCOR
•The principles of basic life support (BLS) were introduced in _____.
•Specific techniques have been revised every 5 to 6 years.
The most recent review was conducted by the ____ ____ _____ ___ ____/____ (abrv)
BLS
•Noninvasive emergency lifesaving care
•Used to treat medical conditions including:
-Airway obstruction
-Respiratory arrest
Cardiac arrest
obstruction
respiratory arrest
cardiac arrest
severe bleeding
•Focus is on the ABCs
-Airway (______)
-Breathing (_________ ______)
-Circulation (____ ____ or ____ ___)
CAB/compressions airway breathing
If the patient is in cardiac arrest, then a ______ sequence
4 6
-Permanent brain damage is possible if brain is without oxygen for ___ to ___ minutes.
Cardiopulmonary resuscitation/CPR
____ ____ -Used to establish circulation and artificial ventilation in a patient who is not breathing and has no pulse
circulation
airway
breathing
•CPR steps
1.Restore _______ (perform chest compressions).
2.Open the ______.
3.Restore _________ (provide rescue breathing).
chest compressions
30
2 2.4
100 120
1st step of CPR
Restore circulation by performing ____ _____ to circulate the blood.
i. Perform ____ high-quality compressions to a depth of ___ inches to _____ inches in an adult at the rate of ____ to _____per minute.
rescue breathing
2 1
3rd step of CPR
Restore breathing by providing ____ ___
i. Administer ____ breaths, each over ___ second, while visualizing for chest rise.
cardiac monitoring
intravenous
airway adjuncts
•BLS differs from advanced life support (ALS)
•ALS involves:
-___ ____
-_____ fluids and medications
-Advanced ____ ____
Chain of survival
activation
CPR
defibrillation
Basic
ALS
•AHA's ____ ___ ____
-Recognition and ______ of the emergency response system
-Immediate, high-quality _____
-Rapid _____
-_____ and advanced EMS
-_____and post-arrest care
•If any one of the links in the chain is absent, the patient is more likely to die.
cardiac
respiratory
Although _____ arrest in adults usually occurs before _____ arrest, the reverse is true for infants and children
Automated external defibrillator/AED
____ ___ ___ should be applied to cardiac arrest patients as soon as available.
•If you witness cardiac arrest, begin CPR and apply the *** as soon as it is available.
Manual defibrillator
pediatric
dose attenuating
anterior posterior
•Children
-Apply after first five cycles of CPR.
-___ ___ preferred for infants 1 month to 1 year
•If unavailable, use ______-sized pads and ____-______ system.
•If neither is available, then use an AED with adult-sized pads with ____ ___ placement.
Pacemakers
defibrillators
1
_____ and implanted ________
- Easily recognizable by a hard lump beneath the skin, usually on the upper left side of the chest
- If AED pads are placed directly over the device, the effectiveness of the AED may be reduced and the shock could damage the device,
- Place electrodes at least ___ inch away from the device.