The Menstrual Cycle
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
Menstrual Cycle Background:
Female infant is born with approximately 1 million oocytes in each ovary
Approximately 400 oocytes are ovulated during a lifetime
Each month the endometrium prepares for the implantation of a fertilized ovum
If fertilization does not occur, the endometrial lining is shed as a menstrual cycle
Physiology:
Endocrine system controls ovarian and uterine cycles through hormones
Gonadotropin releasing hormone (GnRH) is secreted by the hypothalamus
Follicle Stimulating Hormone (FSH) and Lutenizing Hormone (LH) are secreted by the anterior pituitary gland
Estrogen, progesterone, and inhibin are secreted by the ovaries
The Hypothalamus
Called the “control center of the endocrine system”
Located in the center of base of the brain → below thalamus and above pituitary gland
Composes the floor of third ventricle
Functions of the Hypothalamus:
Nerve centers at the anterior and posterior portions of the hypothalamus monitor blood temperature and adjust for abnormal body temperature
Works to balance food intake
Regulates the menstrual cycle and other reproductive functions
secretes hormones into blood that travels directly to the pituitary gland
pituitary gland receives releasing and inhibitory hormones via blood from the hypopophyseal portal system
The Hypophyseal Portal System
AKA: hypothalamo-hypophyseal portal system
group of blood vessels that link the hypothalamus to the anterior pituitary gland
The Pituitary Gland AKA:
Hypophysis
The Pituitary Gland
Size of pea
Two separately functioning lobes
Anterior → adenohypophysis - hormone producing
Posterior → neurohypophysis
Adenohypophysis
Growth hormone
Prolactin
Adrenocorticotropic hormone (ACTH)
Thyroid Stimulating Hormone (TSH)
Follicle stimulating hormone (FSH)
Luteinizing hormone (LH)
Neurohypophysis
Anti-diuretic hormone (ADH)
Oxytocin
The Ovaries
Function as both gonads and endocrine glands
Oogenesis
Production and secretion of estrogen, progesterone, and small amounts of testosterone
Ovarian endocrine functions are responsible for:
female characteristics
regulation of menstrual cycle
pregnancy
Gonadotropin Releasing Hormone (GnRH) AKA:
Luteinizing hormone releasing hormone (LHRH)
Gonadotropin Releasing Hormone (GnRH)
Secreted by hypothalamus
Stimulates the release of FSH and LH from the anterior pituitary gland
Follicle Stimulating Hormone (FSH)
Glycoprotein secreted by the anterior pituitary gland in response to GnRH
Responsible for promoting follicle development within the ovary
Promotes maturation of egg, the cells surrounding the egg that produces hormones that support pregnancy (estrogen and progesterone) and fluid around the egg
As follicles grow, cells in follicle produce an increasing amount of estrogen that is released into the blood stream
Estrogen stimulates the endometrium to thicken prior to ovulation
The higher estrogen levels signal the hypothalamus and pituitary gland to slow FSH production
Luteinizing Hormone (LH)
a gonadotropin secreted by the anterior pituitary gland
needed for follicles to grow and ovulation of the dominant follicle
controls progression of the menstrual cycle
Process of lutenizing hormone:
surge of LH occurs just prior to ovulation that actually triggers ovulation
after ovulation, the remaining cells of the released ovum remain as the corpus luteum
Corpus Luteum produces estrogen and progesterone that support implantation of pregnancy
Progesterone matures endometrium in preparation for implantation of pregnancy
If pregnancy does NOT occur, levels of estrogen and progesterone fall and menstruation occurs
Estrogen AKA:
Oestrogen
Estrogen
CLASS of natural steroid hormones
Estradiol, estriol, estrone
Regulates the growth, development, and function of reproductive system
Ovaries → main source
Corpus luteum and placenta both produce small amounts
Stimulates the endometrium to thicken prior to ovulation
Promotes blood clotting and loss of calcium from bones
Progesterone
Belongs in a class of steroids known as progestogens
Production stimulated by corpus luteum (produced by ovaries)
small amounts also released from the adrenal glands
Prepares body for pregnancy
During pregnancy the placenta begins secreting progesterone at end of 1st trimester
How does progesterone prepare the body for pregnancy?
prepares endometrium for implantation
decreases the contractility of the uterine smooth muscle
blocks the development of new follicles
makes the vaginal secretions thicker to block sperm
increases basal body temperature
stimulates the development of the alveolar system
inhibits lactation during pregnancy
decreases maternal immune response
stimulates growth of uterine wall and blood vessels
Phases of the Ovarian Cycle:
Follicular phase (Day 1-13)
Ovulatory phase (Day 14)
Luteal phase (Day 15)
The Menstrual Cycle
Reproduction begins at around age 11-13 and ends around age 50
Typical menstrual cycle is 28 days
May range from 21-35 days
If longer or shorter than 21-35 days:
Polymenorrhea - too frequent
Oligomenorrhea - not frequent enough
Polymenorrhea
Menstruation occurring more frequent than every 21 days
Oligomenorrhea
Menstruation occurring less frequent than every 35 days
Phases of Menstrual Cycle:
Menstrual (Days 1-5)
Proliferative (Days 6-13)
Early proliferative
Late proliferative
Ovulation on day 14
Secretory (days 15-28)
Endometrium
Specialized mucosa that varies in thickness and composition through the menstrual cycle
Divided into 2 layers:
Functional
Basal
Functional Layer of Endometrium
Innermost layer of endometrium
Glands and stroma
Appearance changes constantly throughout all phases of menstrual cycle
Endometrial cavity is a potential space between functional layers
Basal Layer of Endometrium
Outermost layer of the endometrium
Thin and hyperechoic
Measuring the Endometrium:
Measure in the midline, sagittal plane with the widest area of the fundus
Stretch out the uterus
Align endometrial cavity with the endocervical canal
Includes all layers of the endometrium
Thickness depends on phase of menstrual cycle
Endometrial thickness during menstrual phase:
2-4 mm
Endometrial thickness during early proliferative phase:
4-6 mm
Endometrial thickness during late proliferative / peri-ovulatory phase:
6-8 mm
Endometrial thickness during secretory phase:
8-15 mm
Menstruating Phase endometrium U/S appearance:
Variable appearance
Thin broken hyperechoic central interface
2-4mm
Early Proliferative Phase endometrium U/S appearance:
Relatively thin, hyperechoic line
Composed of echogenic basal layer next to the central endometrial interface
4-6 mm
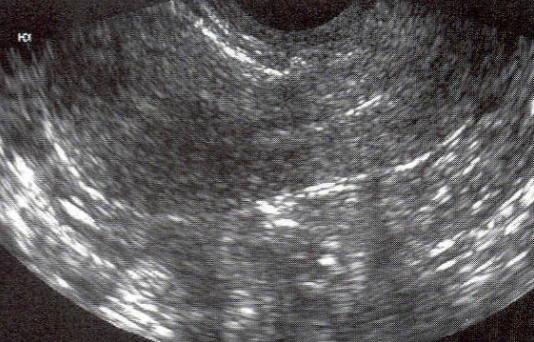
Late Proliferative Phase endometrium U/S appearance:
Becomes more hypoechoic during later proliferative phase
Has a triple layer or “halo appearance”
3 layers:
central thin echogenic line of endometrial interface
hypoechoic functional layer
hyperechoic basal layer
6-8 mm

Secretory Phase endometrium U/S appearance:
Thick, uniformly hyperechoic central band
All 3 layers mentioned in late proliferative phase are all hyperechoic
Maximum thickness of 8-15 mm

Secretory Phase of Menstrual Cycle:
Endometrial glands become tortuous and filled with glycogen and mucin
Uterine artery has a lower pulse rate
Progesterone and Estrogen is present