Special Senses Physiology
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
Vision
The ability to see.
This is because the photoreceptors in the eye or the sensory cells are depolarized at rest.
When activated, they are hyperpolarized.
Unique to the visual system.
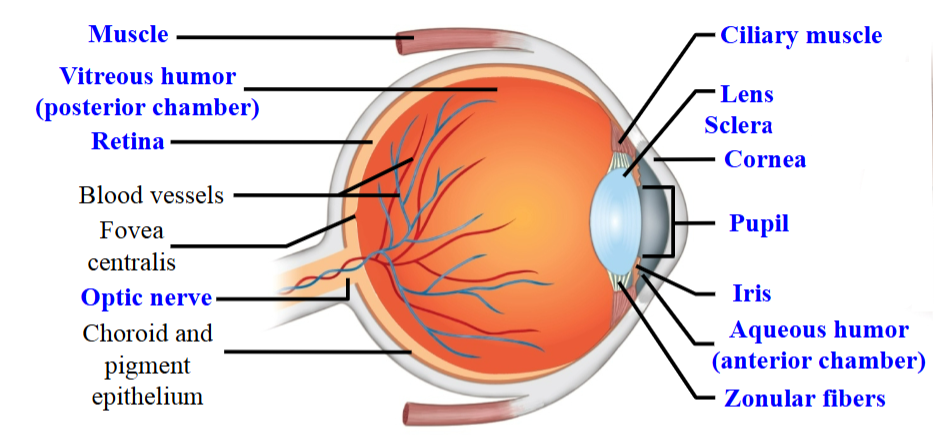
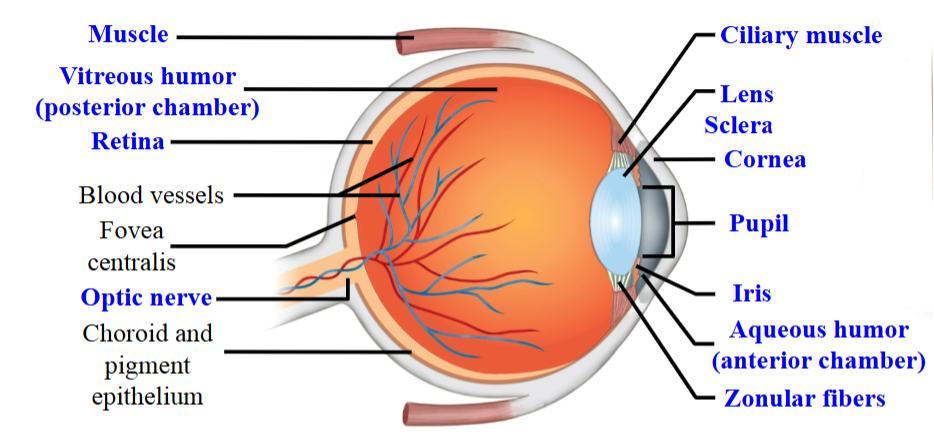
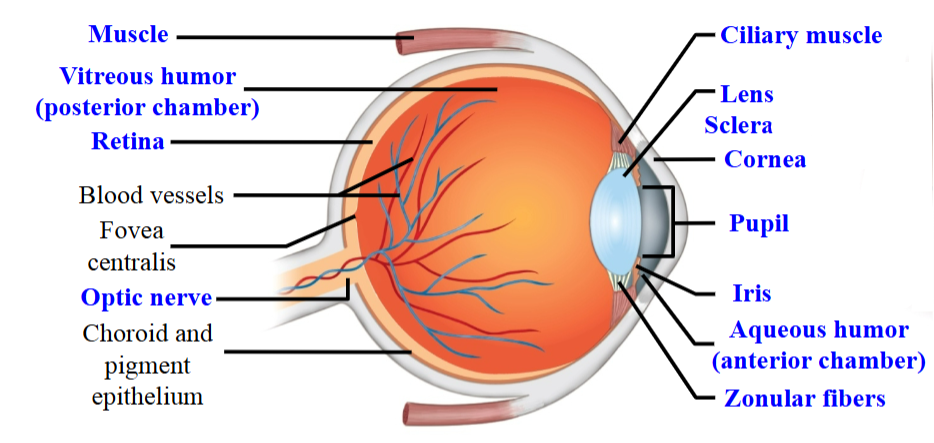
Optical Component
Focuses the visual image on the receptor cells.
Front part of the eye.
Neural Component
Transforms the visual image into a pattern of graded and action potentials.
Back of the eyeball.
Sclera
Membrane surrounding the eyeball.
The extra ocular muscle is attached.
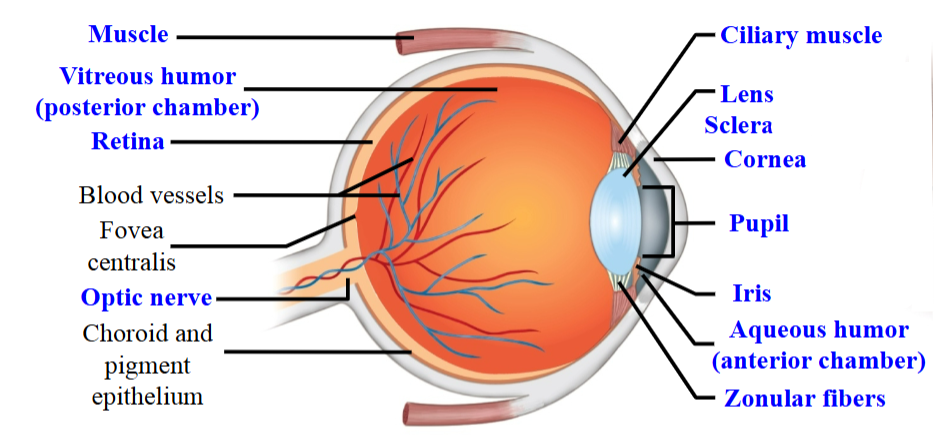
Cornea
The region where the sclera becomes clear at the front region of the eye.
Light waves refract and (hopefully) converge in the area where photoreceptors are packed.
The cornea is static and cannot change - light passes through and refracts a certain amount.
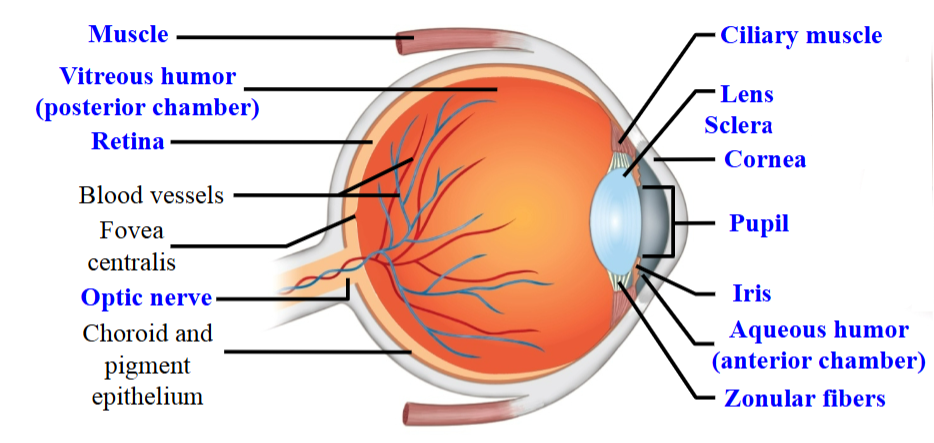
Iris
Gives eyes colour.
Innervated by the autonomic NS.
Aperture that regulates the amount of light.
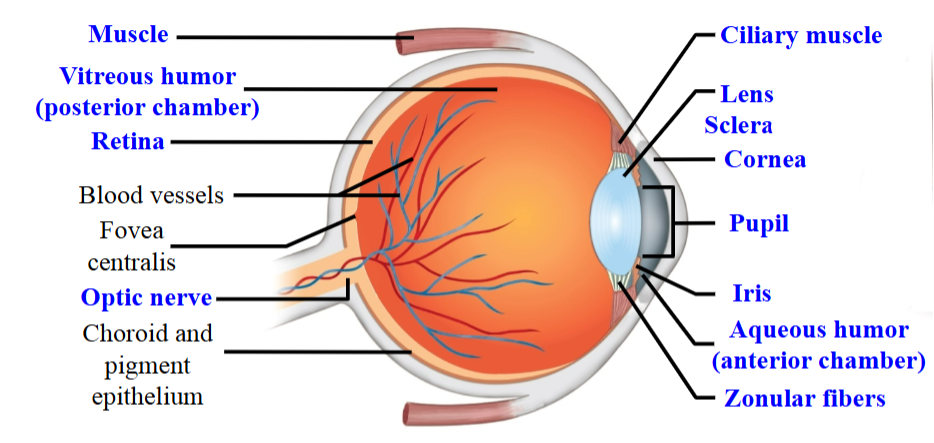
Extra Ocular Muscle
Responsible for eye movements, looking up and down, or side to side.
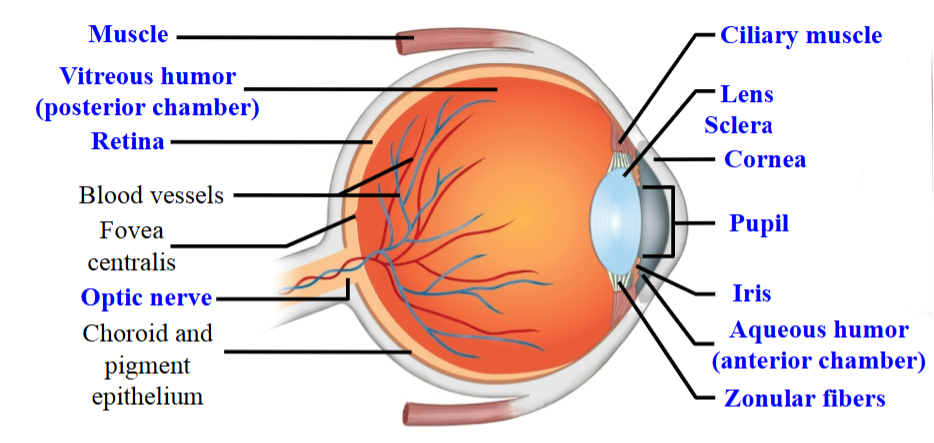
Pupil
The hole that allows light to pass though into the back of the eye.
Size is regulated by the iris.
Is constricted or dilated by contraction of the smooth muscle of the iris.
SNS → Dilate.
PSNS → Constrict.
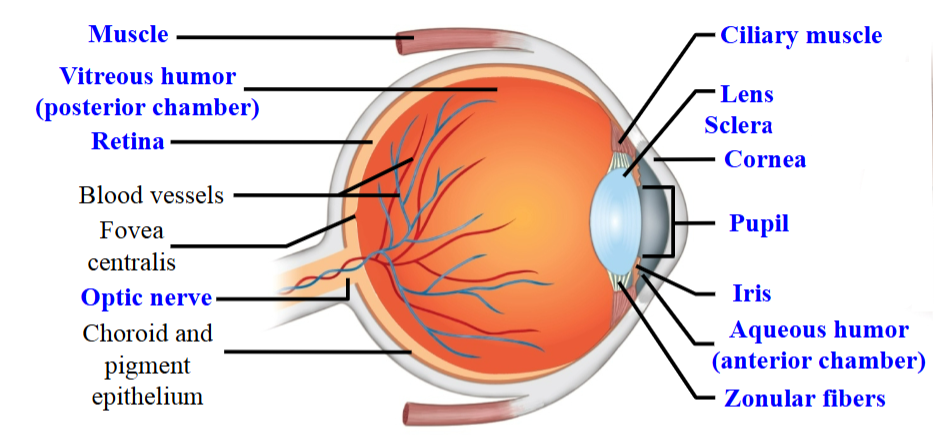
Lens
Works together with the cornea to focus on the visual image on the retina.
The shape and size of the lens can be changed.
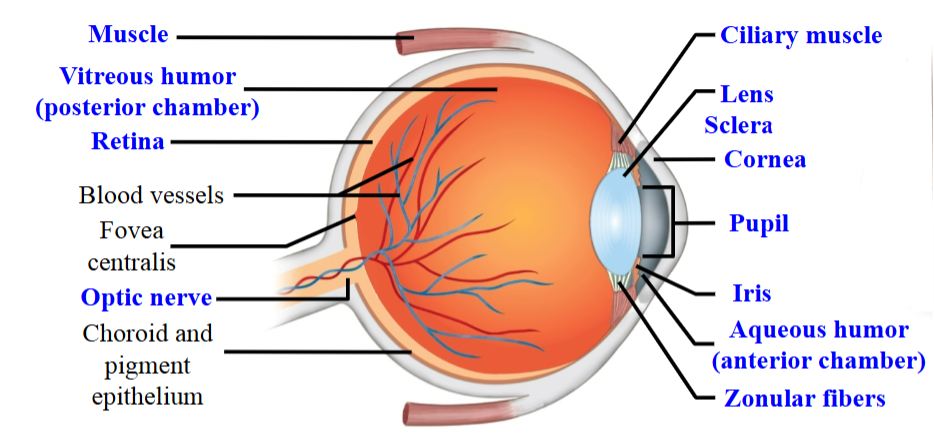
Zonular Fibers
Attracted to the lens are these little fibers.
These fibers are attached to the ciliary muscles.
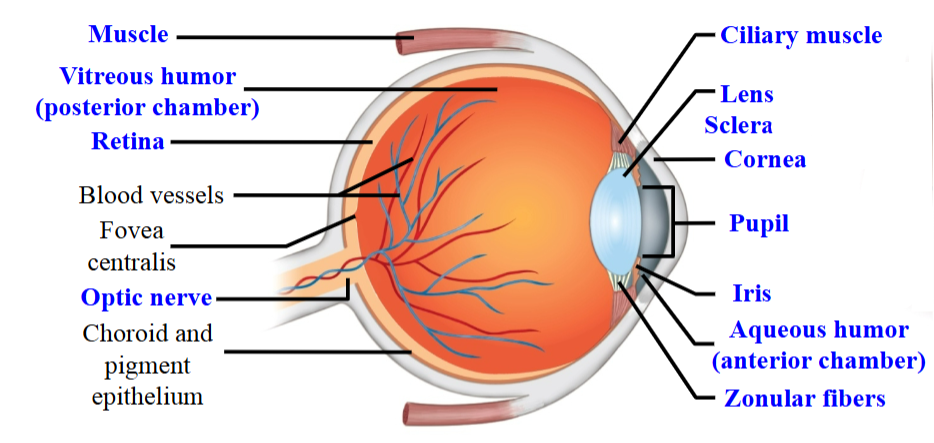
Ciliary Muscles
Can either be released or they can be contracted.
They change the shape of the lens.
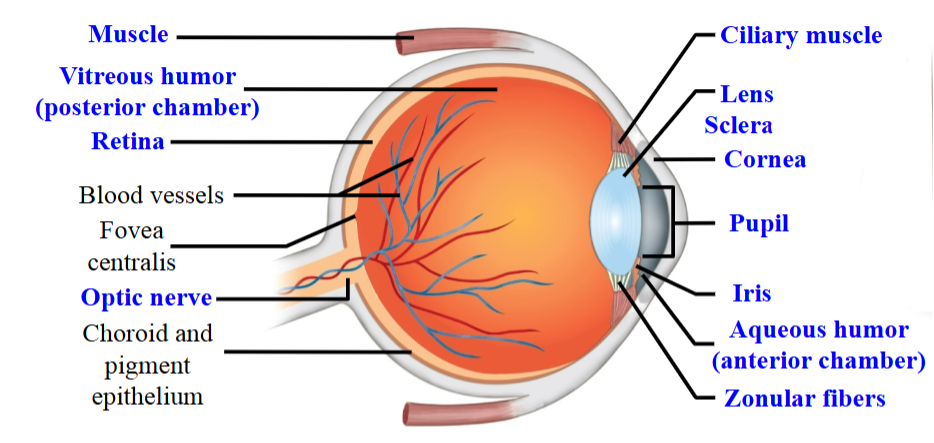
Retina
Located behind the lens against the back of the eye.
Where the photoreceptors are found.
Rods and cones.
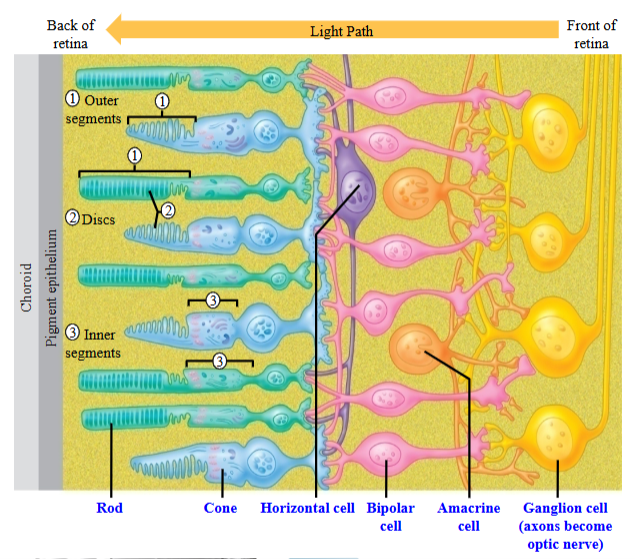
Rods
Activated in low light conditions; very sensitive.
They are monochromatic.
Cones
Activated when there is more light present and responsible for colour vision.
Retinal Ganglion Cells
Activated by rods and cones.
Comprises optic nerve and transmits visual information to the cortex.
Taking information back towards the brain.
Cortex is made up of the axons of retinal ganglion cells.
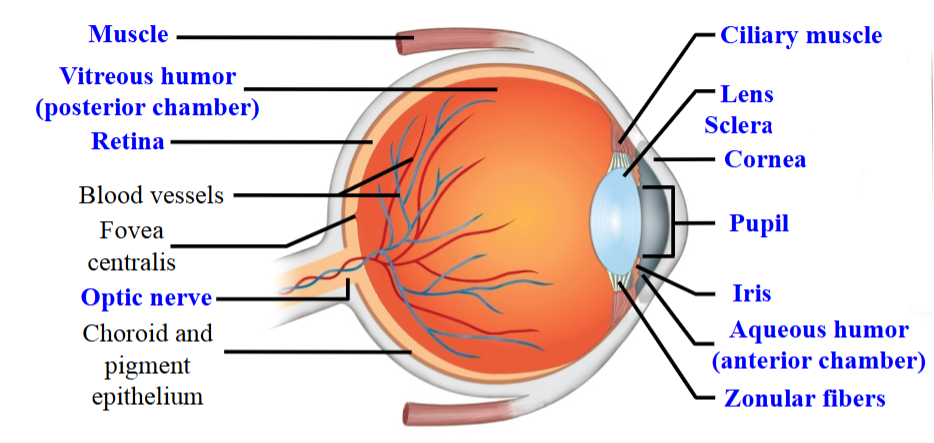
Optic Nerve
Leaves through the back of the eyeball and heads back towards the thalamus.
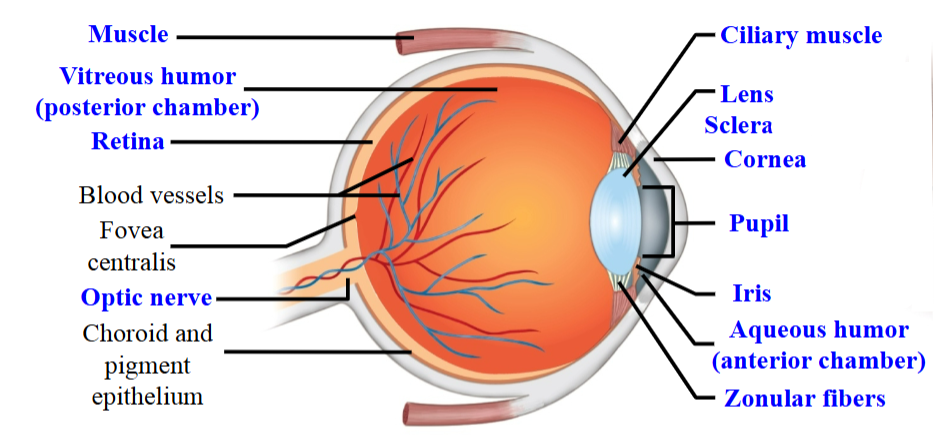
Aqueous Humour
The gap between the lens and the cornea.
Filled with a gelatinous-like fluid.
Vitreous Humour
Behind the lens where there’s a large gap.
Filled with another type of gelatinous fluid.
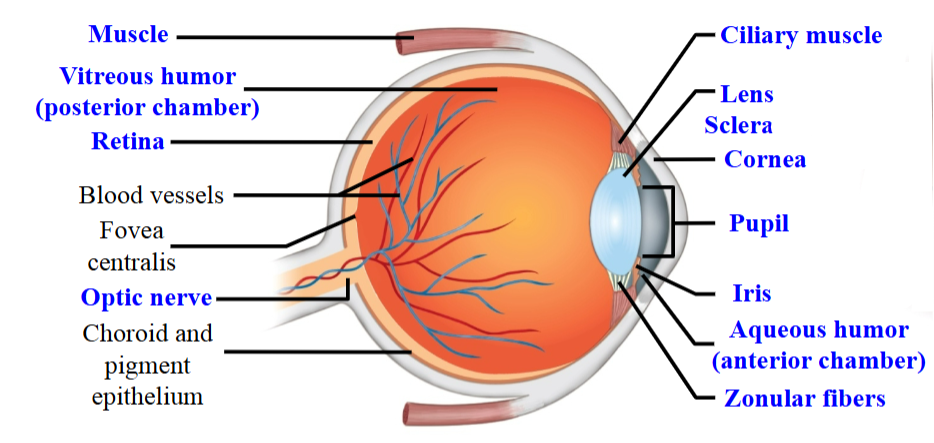
Refraction
Light bends when passing between media of different densities, changing the object's apparent position.
Image inversion occurs in the eye, where the lens focuses light upside down on the retina.
Lens Focusing Mechanism
When objects are close, corneal refraction alone cannot focus the image on the retina.
The image forms behind the retina, resulting in a blurry image.
The ciliary muscle contracts, surrounding the lens.
This makes the lens shorter and fatter, increasing its refractive power.
The increased refraction focuses the image properly onto the retina.
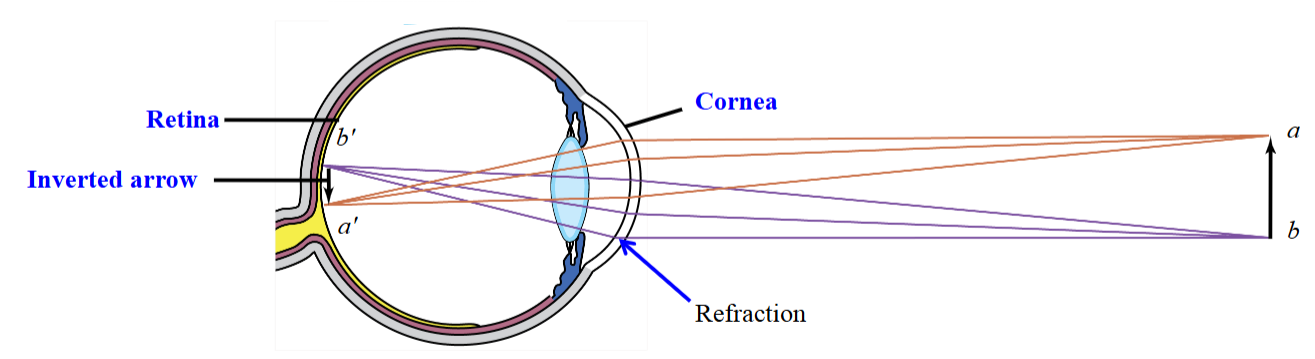
Image in Focus (Relaxed Ciliary Muscles)
Light reflects off and towards the eye, refracting a certain amount.
The ciliary muscles relaxed with tension on the zonular fibers, flattened lens.
Light rays from distant objects are nearly parallel.
When the image hits the cornea, the image is reconstructed on the retina.
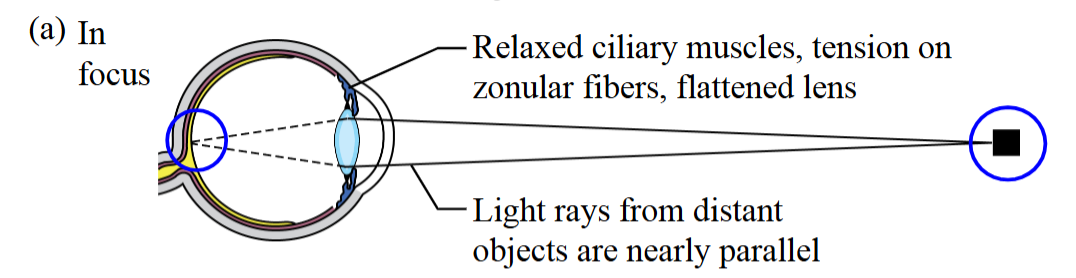
Image Out of Focus (Relaxed Ciliary Muscles)
An object gets closer to the eye.
As a result, the refraction at the cornea is insufficient to allow the image to form.
Instead, it forms on the back of the retina.
The ciliary muscles are relaxed and the light rays from near objects diverge.
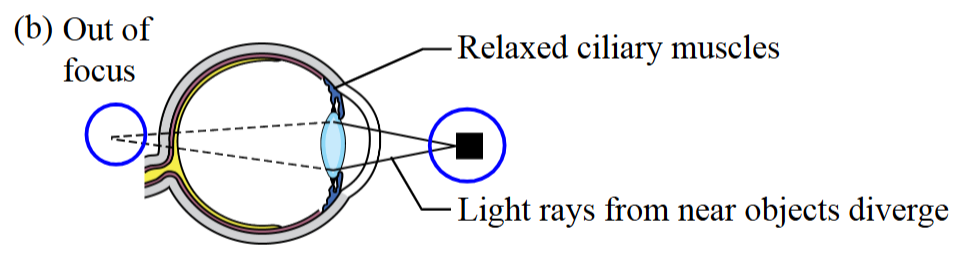
Image in Focus (Constricted Ciliary Muscles)
To see the image clearer, there is a firing of parasympathetic nerves, the ciliary muscles constrict, the zonular fibers slack, and the lens becomes rounder.
This increases the amount of refraction.
Lens becomes spherical.
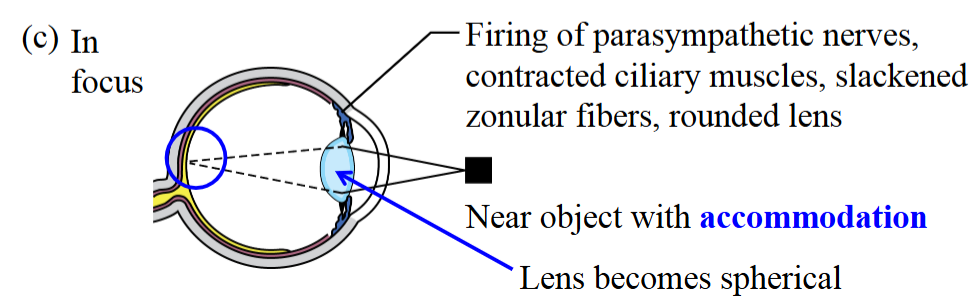
Accommodation
The eye's ability to automatically adjust its focus.
It involves the lens changing shape, becoming more rounded for near vision and flatter for far vision.
Typically goes away at 45 years old.
The ciliary muscles breakdown and the lens is no longer contractable.
Presbyopia
loss of lens elasticity, reducing near vision accommodation.
Caused mainly by aging and ciliary muscle changes.
People without reading glasses hold objects farther away to see clearly.
They rely solely on corneal refraction, as accommodation is impaired.
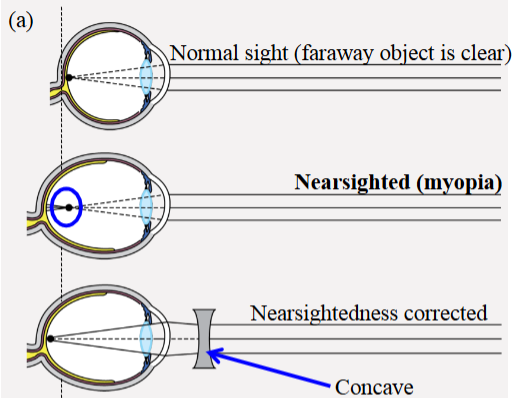
Myopia
Eye is too long for the lens’s focusing power.
Excessive refraction causes the image to focus in front of the retina.
Can see near objects, but not far.
Treated with glasses (concave lens) or laser eye surgery.
Hyperopia
The eye is too short for the lens’s focusing power.
Insufficient refraction causes the image to focus behind the retina, making near objects blurry.
Can see distant objects clearly, but not up close.
Treated with glasses (convex) or laser eye surgery (not as successful).
Astigmatism
Surface of lens or cornea is not smoothly spherical.
Can be corrected with glasses or complex laser surgery.
Glaucoma
Damage to the retina from raised intraocular pressure, typically due to aqueous humour build-up.
Poor drainage causes pressure on the lens, which pushes against the vitreous humour, transmitting force to the retina and photoreceptors, leading to damage.
There is no reliable treatment for glaucoma.
Cataracts
Age-related clouding of the lens; happens later than presbyopia.
Lens cells die and debris accumulates within them.
A grain forms in the lens, reducing the ability to see clearly.
Cataracts Treatment
Treated by removing the lens, cleansing it with a microscopic vacuum, and replacing it with a silicone or artificial lens.
The ciliary muscles and zonular fibers cannot properly activate or innervate the lens for accommodation.
People with cataracts already have reduced accommodation due to presbyopia.
Interneurons
Horizontal, bipolar, and amacrine cells.
Take information from the photoreceptors and transfers the information to retinal ganglion cells that make up the optic nerve.
Information from the retina is taken back to the lateral geniculate nucleus, where they synapse and travel back to the cortex.
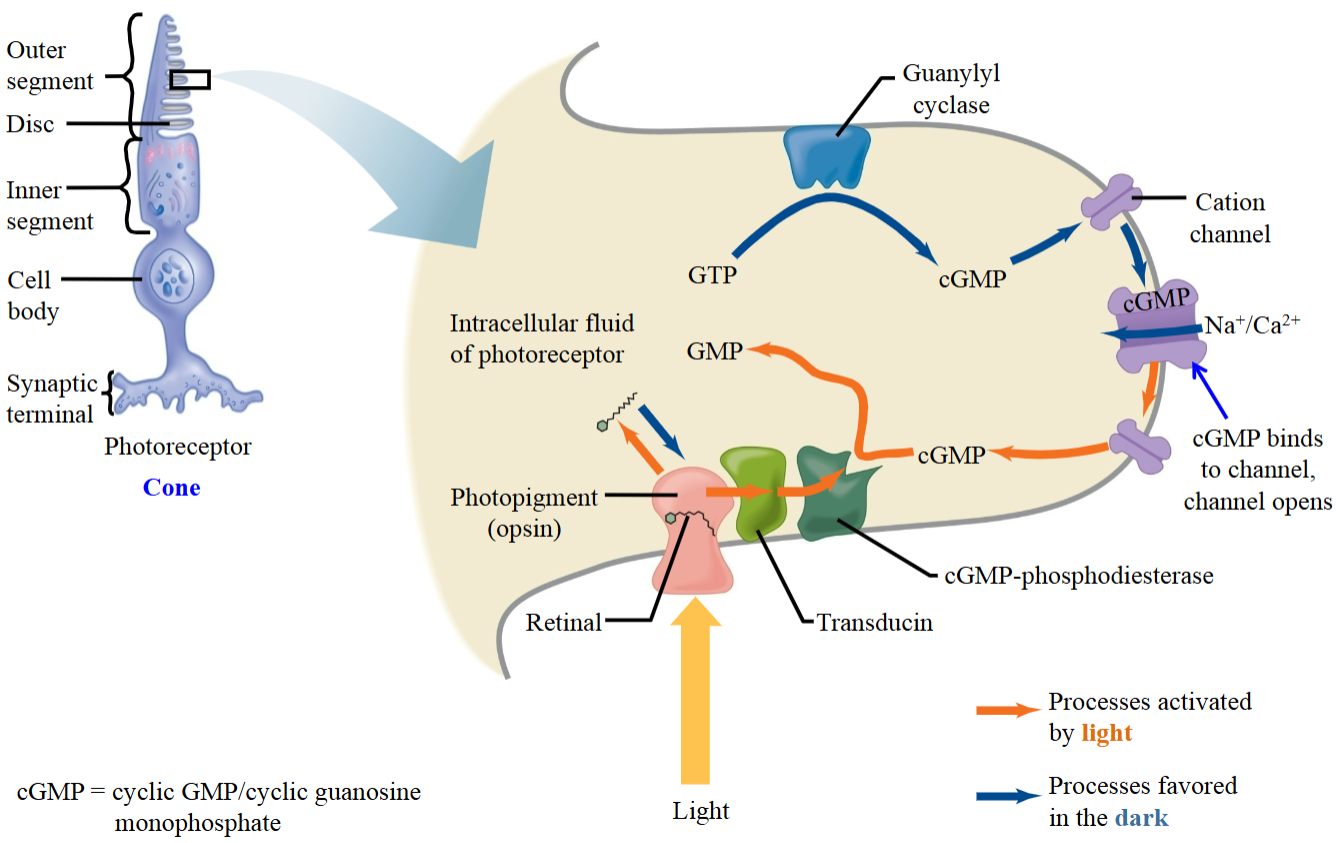
Photoreceptor
The photoreceptor is depolarized at rest or when light is absent.
The photoreceptor is hyperpolarized when light is present or in response to a stimulus.
The photoreceptor is more negative when light is present than when light is not present.
Phototransduction (No light) - Step 1
When no light is present, cGMP is generated by guanylyl cyclase.
The enzyme, guanylyl cyclase, converts GTP to cGMP.
cGMP binds to its receptor on the cation channel.
∴ Cation channel opens; Na⁺ and Ca²⁺ flows into the cell.
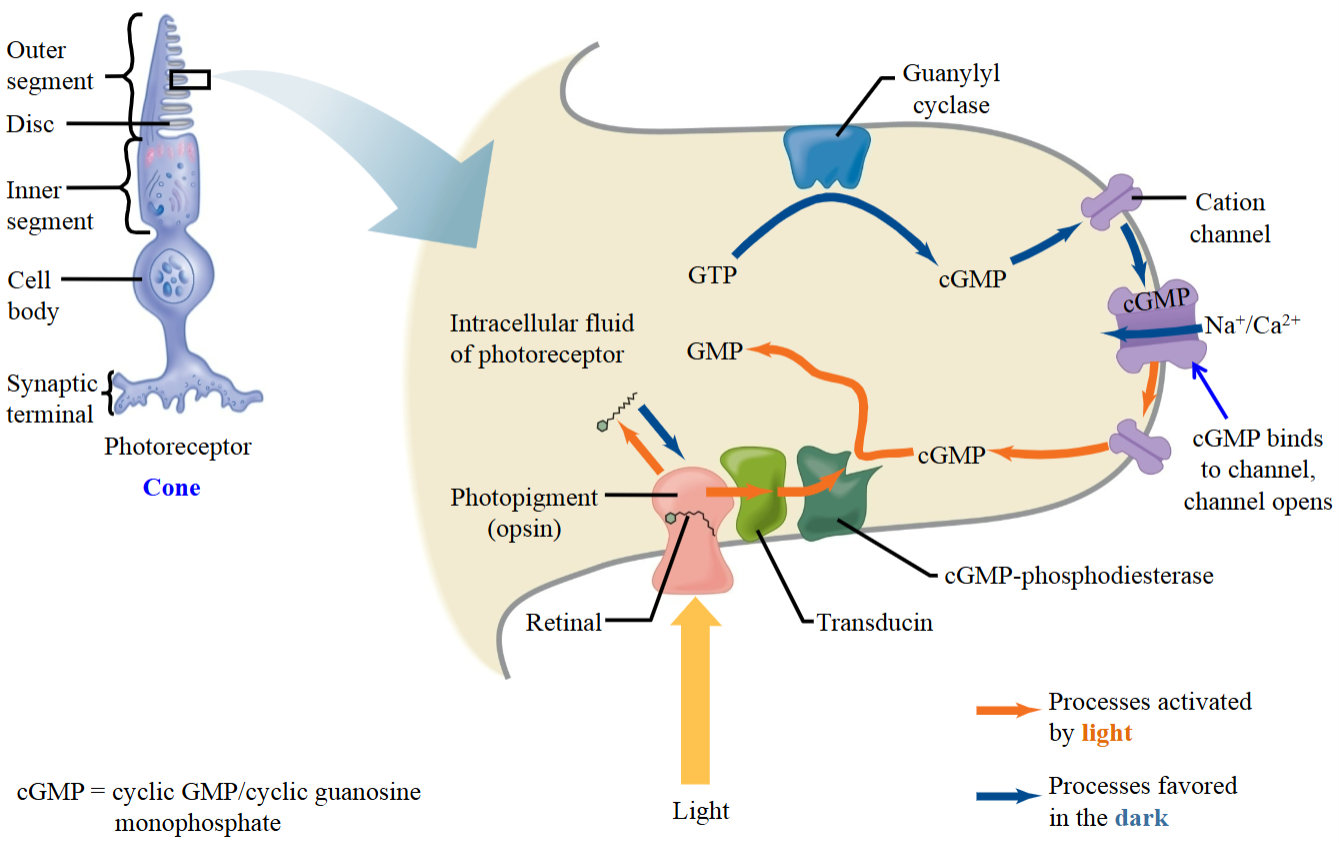
Phototransduction (No light) - Step 2
The photoreceptor depolarizes as the Na⁺ and Ca²⁺ are entering the cell.
When no light is present, the photoreceptors are relatively depolarized.
The membrane potential is -35mV when there is no light present.
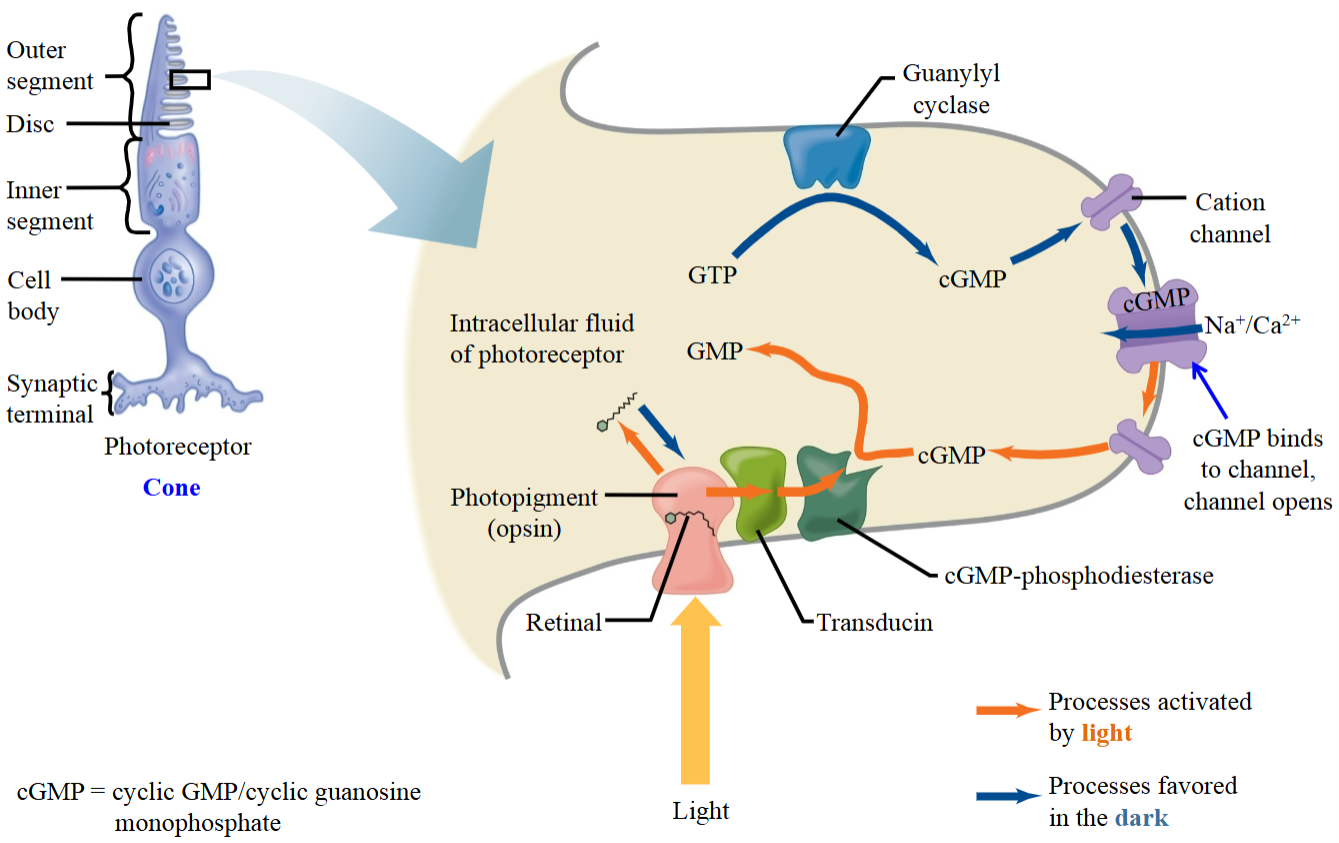
Phototransduction (Light) - Step 1
The discs of the cones contain a photopigment, which has a chromophore called retinal.
When light hits the photopigment, retinal changes from cis to trans.
This activates cGMP phosphodiesterase, an enzyme that breaks down cGMP into GMP.
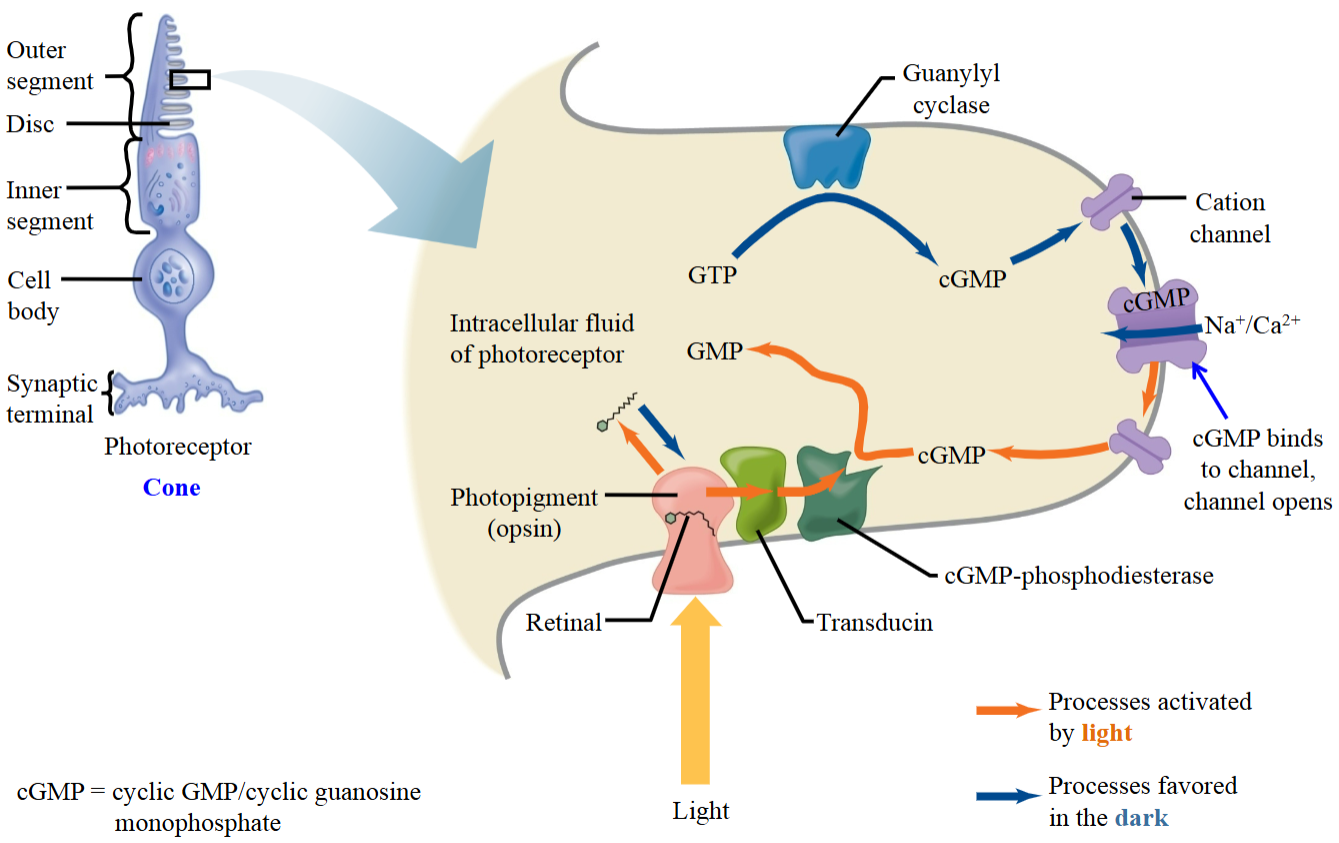
Phototransduction (Light) - Step 2
When light is present, a pathway is activated which reduces the amount of cGMP.
cGMP decreases, making the cGMP-gated Na⁺/Ca²⁺ channels close
No Na⁺/Ca²⁺ influx → less positive charge inside
∴ The photoreceptor is hyperpolarized when light is present.
Neural Pathways in Vision
Light signals are converted into APs through interactions between photoreceptors, bipolar cells, and ganglion cells.
Photoreceptors and bipolar cells only undergo graded responses due to a lack of voltage-gated channels; ganglion cells are the first to fire APs.
Photoreceptors connect to bipolar and ganglion cells via ON- and OFF-pathways.
Differences in ON vs. OFF Pathways
ON-pathway bipolar cells spontaneously depolarize in the absence of input and have inhibitory glutamate receptors (metabotropic).
OFF-pathway bipolar cells hyperpolarize without input and have excitatory glutamate receptors (ionotropic).
Similarities in ON vs. OFF Pathways
In the absence of light, photoreceptors are depolarized, and glutamate is released onto bipolar cells.
When light strikes, photoreceptors hyperpolarize due to decreased cGMP (from activation of cGMP-dependent phosphodiesterase), closing cation channels and reducing glutamate release.
ON-Pathway (In Darkness)
Photoreceptors are depolarized as cGMP opens cation channels (Na⁺, Ca²⁺ influx).
They release glutamate, which binds inhibitory metabotropic receptors on bipolar cells, causing hyperpolarization and reduced neurotransmitter release to ganglion cells.
Ganglion cells are not stimulated to fire APs.
ON-Pathway (In Light)
Photoreceptors hyperpolarize → less glutamate → ON-bipolar cells depolarize, releasing excitatory neurotransmitter onto ganglion cells.
Ganglion cells depolarize and fire APs to the brain.
OFF-Pathway (in Darkness)
Glutamate binds ionotropic receptors on bipolar cells, opening cation channels and causing depolarization.
Bipolar cells release excitatory neurotransmitter, stimulating ganglion cells to fire APs.
OFF-Pathway (In light)
Reduced glutamate → bipolar cells hyperpolarize → decreased excitation of ganglion cells → APs inhibited.
Co-Existence of ON & OFF Pathways
The coexistence of ON and OFF pathways enhances contrast detection and image resolution, especially at edges and borders.
Visual Pathways - Lateral Field
Information from the lateral half of the visual field strikes the nasal region of the retina.
It travels via retinal ganglion cell axons to the optic chiasm, where the two optic nerves meet.
At the optic chiasm, the information crosses to the contralateral side.
It then synapses at the lateral geniculate nucleus (LGN).
Neurons from the LGN relay the information to the visual cortex.
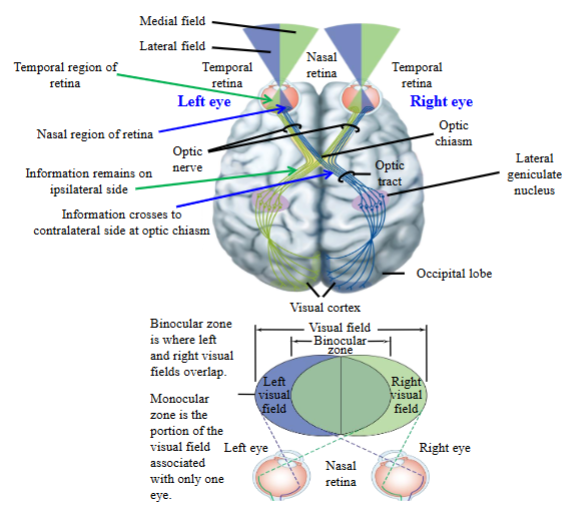
Visual Pathways - Temporal Field
Information goes to the temporal region of the retina.
It travels back to the optic chiasm, but does not cross the optic chiasm.
It stays on the same side, or the ipsilateral side.
It foes to the ipsilateral geniculate nucleus, where is synapses.
The information goes to the visual cortex in the occipital lobe.
Hearing
Hearing relies on the physics of sound and the physiology of the ear, auditory nerves, and brain regions that process sound.
Sound energy travels through molecules in a medium—usually air.
Speech is the movement of air molecules.
Without molecules, there is no sound.
Tuning Fork
Striking a tuning fork sets nearby air molecules into motion, creating zones of compression and zones of rarefaction.
These alternating high- and low-pressure areas form oscillations in the air, producing sound.
The pitch depends on where the tuning fork is struck.
Zones of Compression
Where the air molecules are tightly packed or closer together.
Zones of Rarefraction
Regions where there are relatively few air molecules.
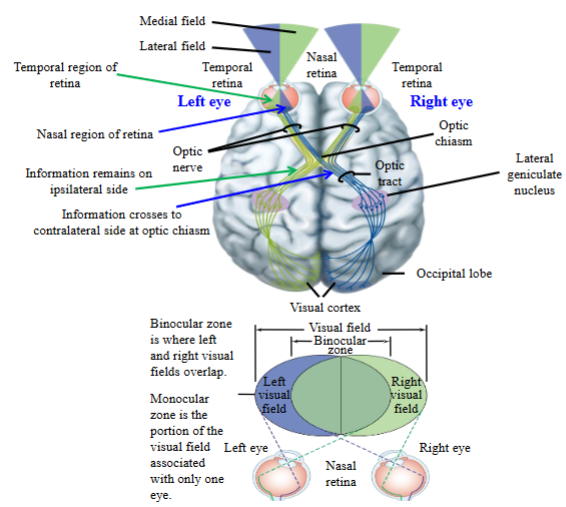
Amplitude
Determined by how many air molecules are within one of the zones of compression.
The difference between pressure of molecules in the zones of compression and rarefraction.
Amplitude = Loudness.
Frequency
Determined by the distance between the zones of compression.
The faster the vibration, the hgiher the pitch.
Number of cycles per second = frequency = pitch.
Pressure vs. Time
The number of cycles per second represents the frequency (length).
The amplitude (width) represents the loudness of the sound.
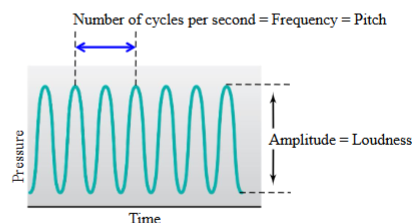
External Auditory Canal
Funnels the zones of compression and zones of rarefaction towards the middle and inner ear.
The sound travels along the external auditory canal and hits the eardrum.
Tympanic Membrane
It vibrates in and out as air molecules push against it,
The “in and out” of the eardrum will be consistent with the frequency and amplitude of the sound.
Increased frequency = eardrum moves quickly.
Decreased frequency = eardrum moves slowly.
Malleus
The malleus is attached to skeletal muscles and the eardrum.
A small bone in the middle ear which transmits vibrations of the eardrum to the incus.
Incus
Attached to the malleus.
A small anvil-shaped bone in the middle ear, transmitting vibrations between the malleus and stapes.
Stapes
Attached to the stapedius muscle and the incus.
A small stirrup-shaped bone in the middle ear, transmitting vibrations from the incus to the inner ear.
Tensor Tympani Muscle and Stapedius Muscle
The tensor tympani and stapedius muscles can contract to protect the ear from sustained loud sounds by dampening movement of the middle ear bones.
However, they do not protect against sudden loud noises (like a bang), as they can't contract quickly enough in time.
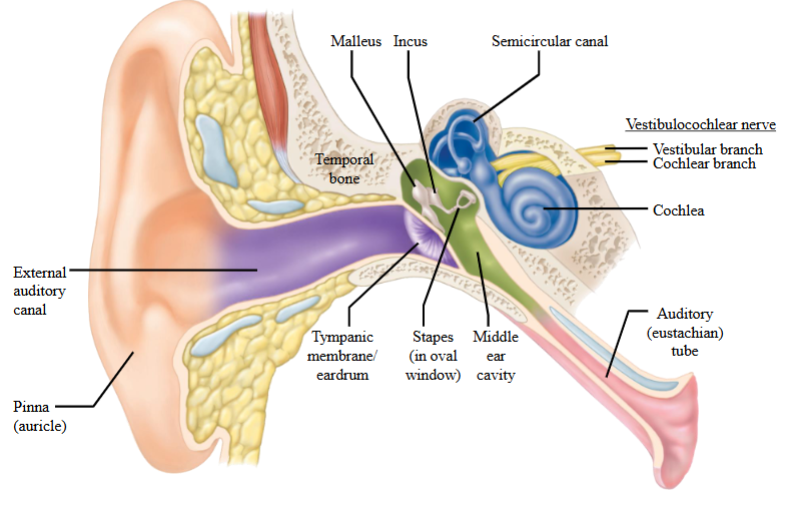
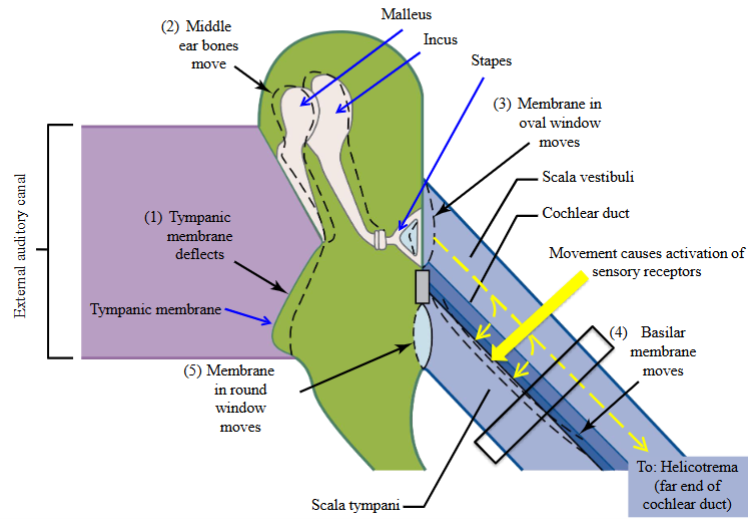
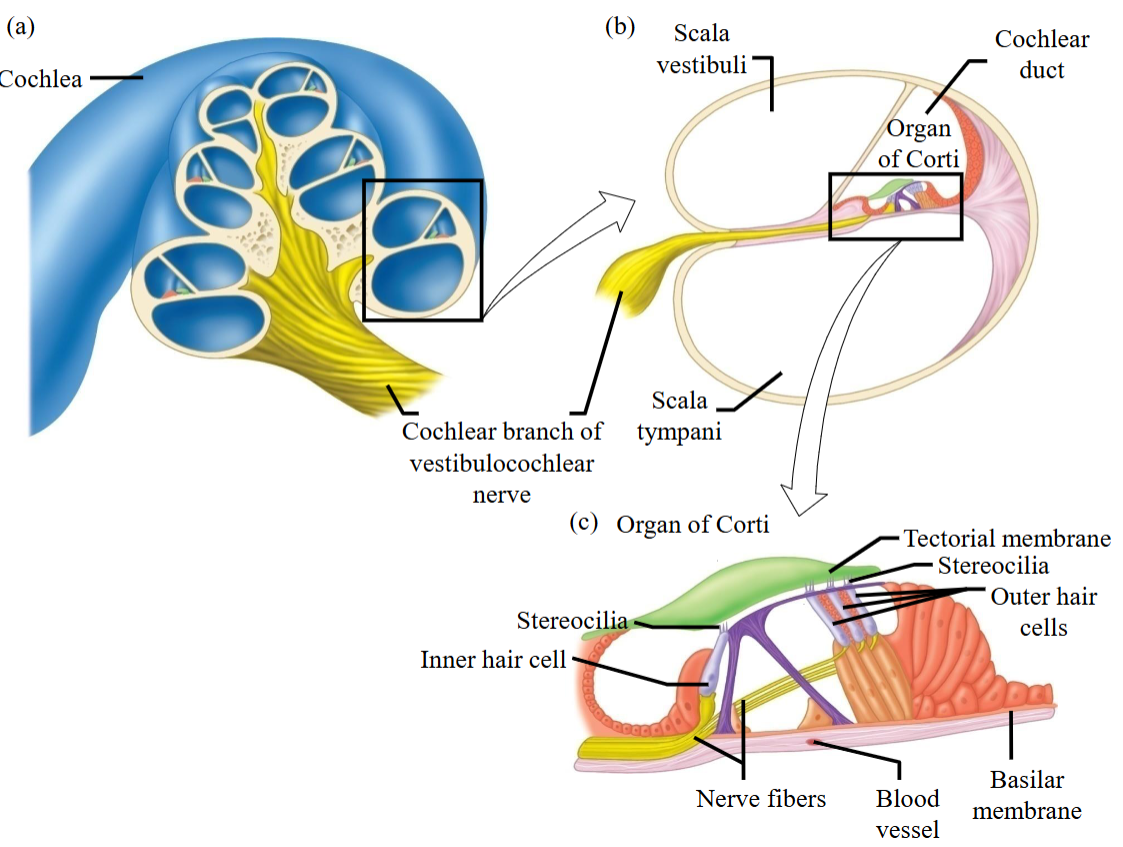
Cochlear Divisions
The cochlea is divided into 3 compartments.
Top compartment: Scala vestibuli.
Middle compartment: Cochlear duct.
Bottom compartment: Scala tympani.
Cochlear Fluid Movement
Sound waves entering the external auditory canal move the eardrum, which in turn moves the middle ear bones.
The stapes pushes against the oval window, causing perilymph to move toward the end of the cochlear duct (helicotrema).
Goes down through the cochlear tract—from the scala vestibuli to the scala tympani.
This downward movement activates the sensory receptors.
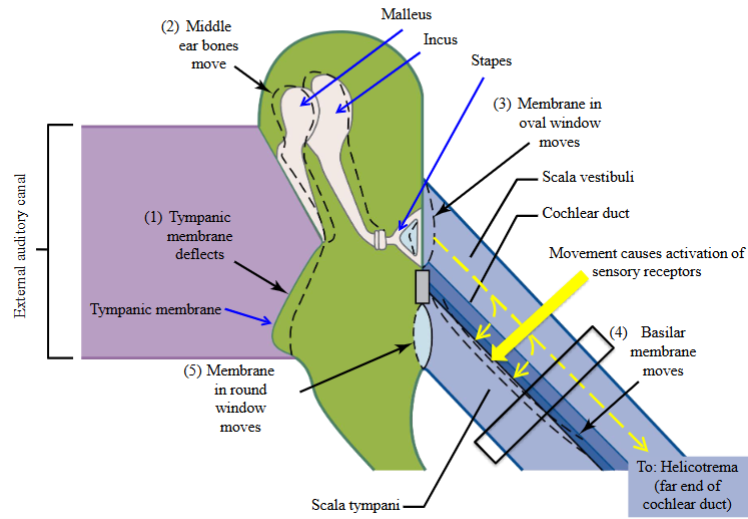
Scala Vestibuli
Full of perilymph (fluid), which has the same composition of the CSF.
Is the superior most duct of the cochlea duct.
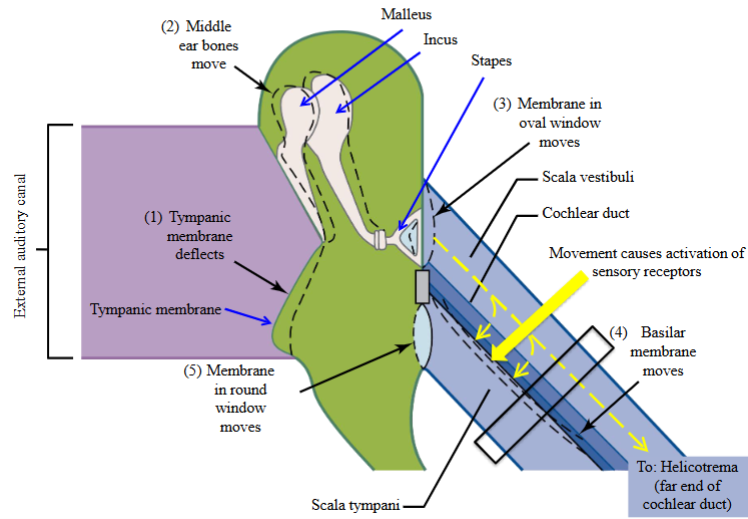
Scala Tympani
The inferior most duct of the cochlea.
It is filled with perilymph.
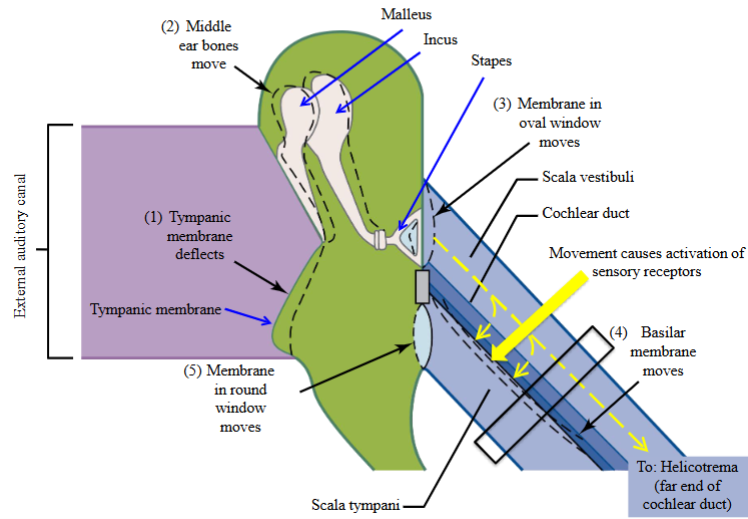
Cochlear Duct
Where the sensory receptors for the auditory system are located.
Filled with endolymph.
A fluid-filled tube within the cochlea of the inner ear.
Organ of Corti
A specialized sensory epithelium that allows for the transduction of sound vibrations into neural signals.
Located within this organ are hair cells.
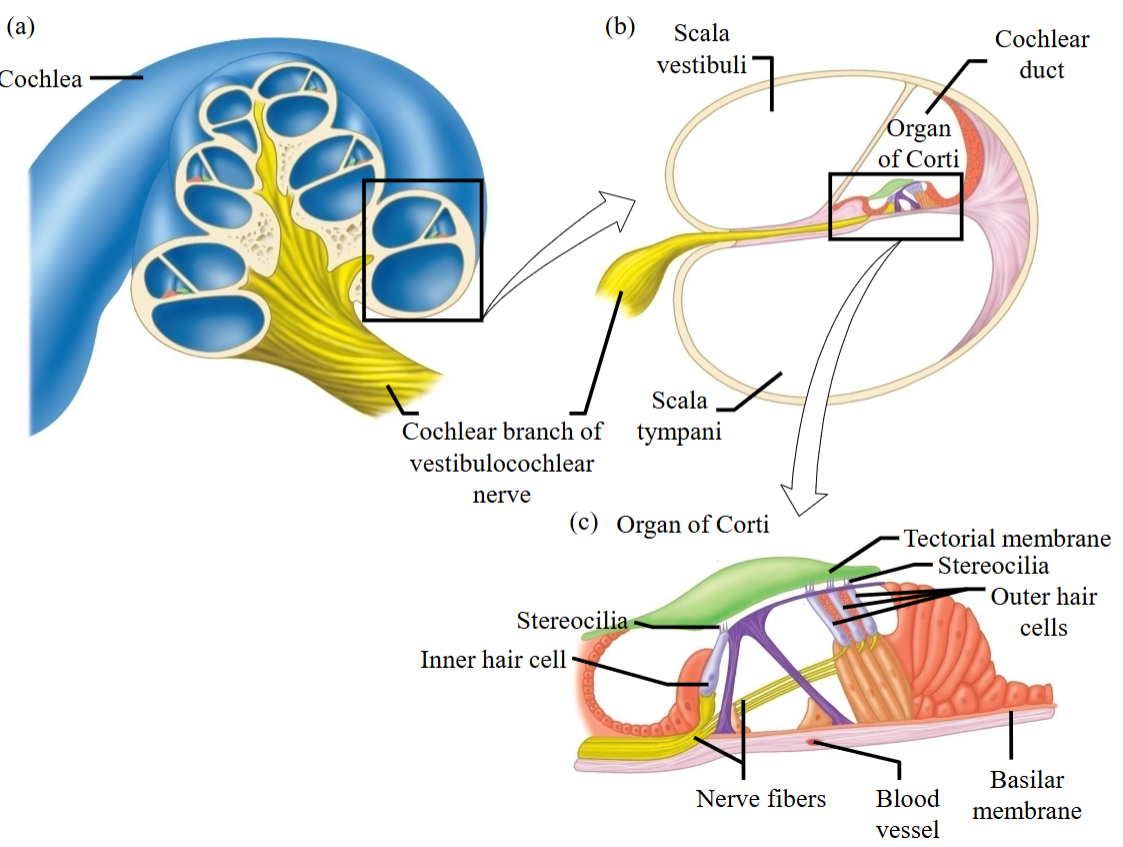
Hair Cells
The sensory receptors for the auditory system are located in the cochlear duct on the organ of Corti.
They have stereocilia protruding from their apical surface.
There are two anatomically distinct groups:
A single row of inner hair cells
Three rows of outer hair cells
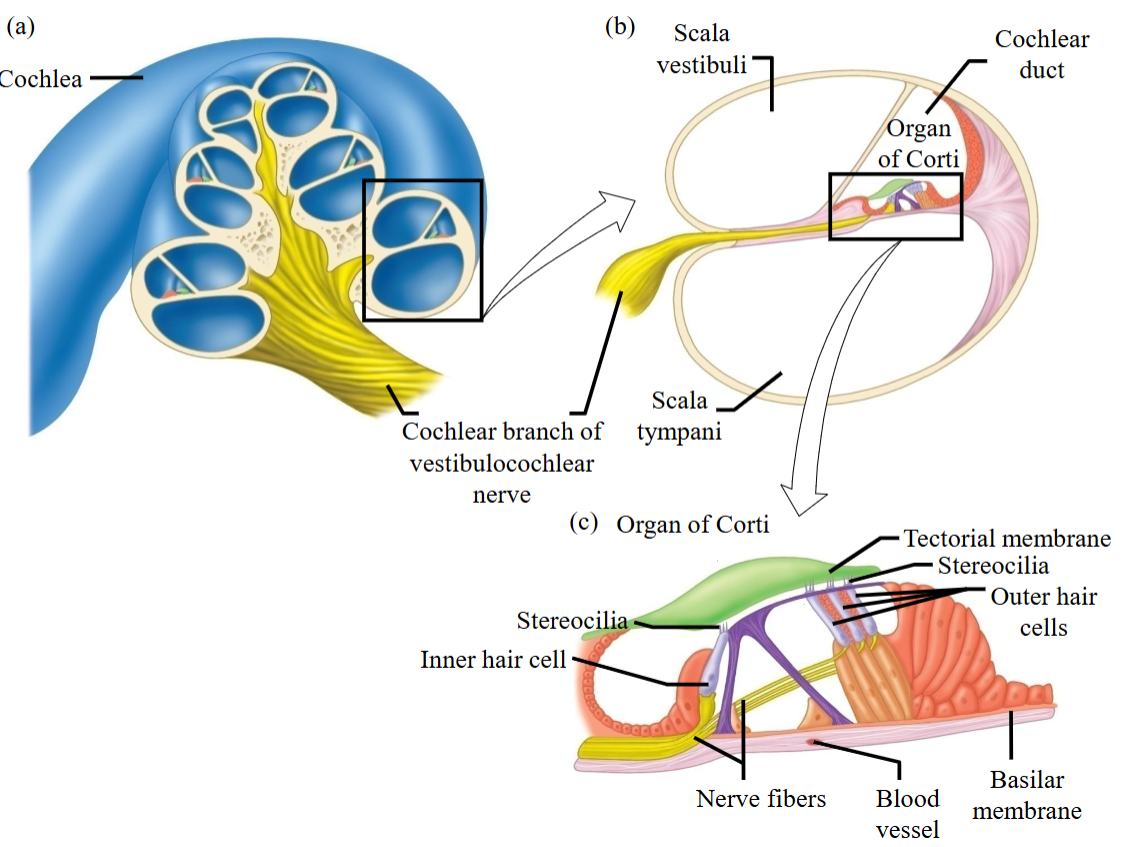
Vestibulocochlear Nerve
Takes auditory information from the ear towards the brain.
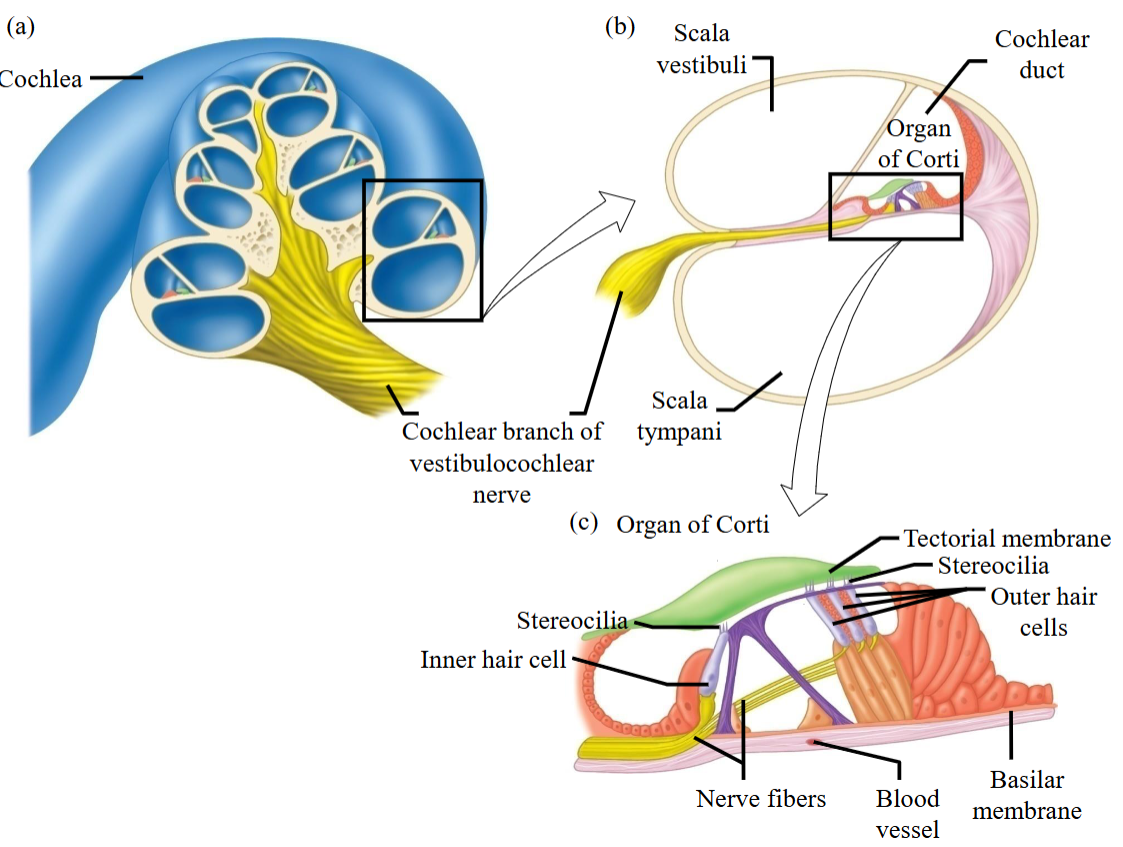
Stereocilia
Extend into the endolymph and transduce pressure waves caused by fluid movement in the cochlear duct into receptor potentials.
Projects into the tectorial membrane.
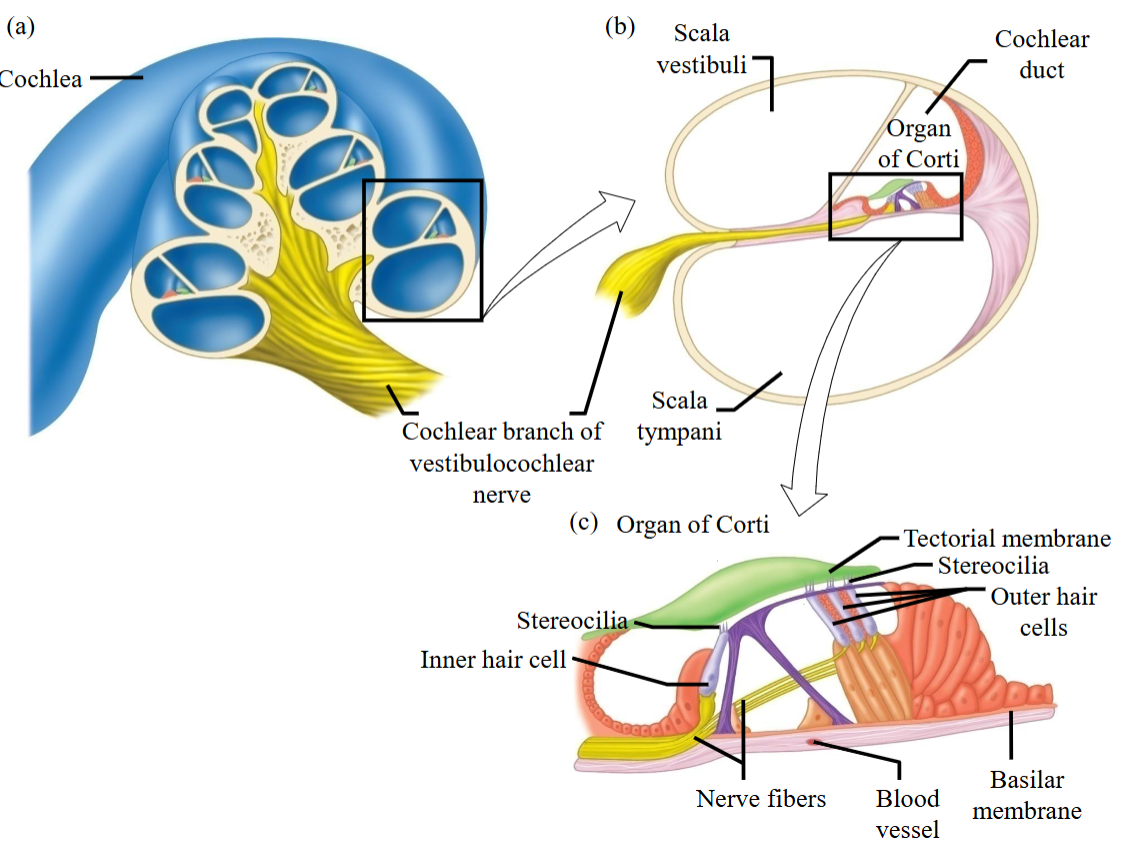
Basilar Membrane
Supports hair cells, serves as the base layer of the organ of Corti, and propagates sound vibrations that allow the brain to interpret sounds.
Outer hair cells are attached to the membrane at the bottom.
Interpreting Sound - Mechanical Movement
Perilymph movement causes the basilar membrane to move up and down.
This motion makes hair cells move back and forth.
Step one.
Interpreting Sound - Interaction
Stereocilia on the outer hair cells are embedded in the stationary tectorial membrane.
Movement of the basilar membrane causes bending of stereocilia, leading to mechanical deformation.
Step two.
Interpreting Sound - Frequency
Different regions of the basilar membrane vibrate maximally in response to different frequencies.
Hair cells at the point of peak vibration undergo the greatest deformation.
Step three.
Interpreting Sound - Interpretation
This deformation is converted into signals sent to the CNS.
The brain interprets the pattern of hair cell stimulation as a specific sound frequency.
This allows different sound frequencies to be detected along the organ of Corti.
Step four.
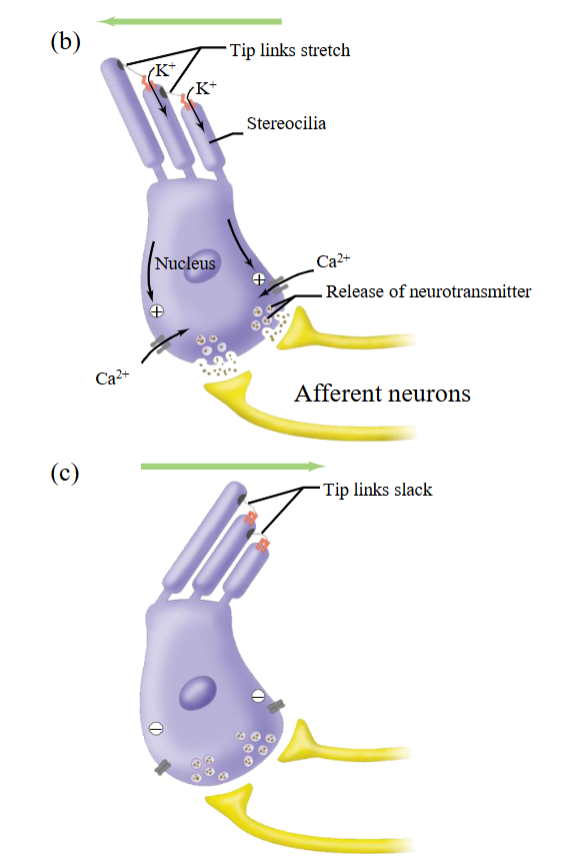
AP - Depolarization
The hair cells move back and forth when the basilar membrane moves.
In the inner ear, K⁺ concentration is higher outside the hair cell—opposite of typical neurons, where K⁺ is higher inside at rest.
Step one.
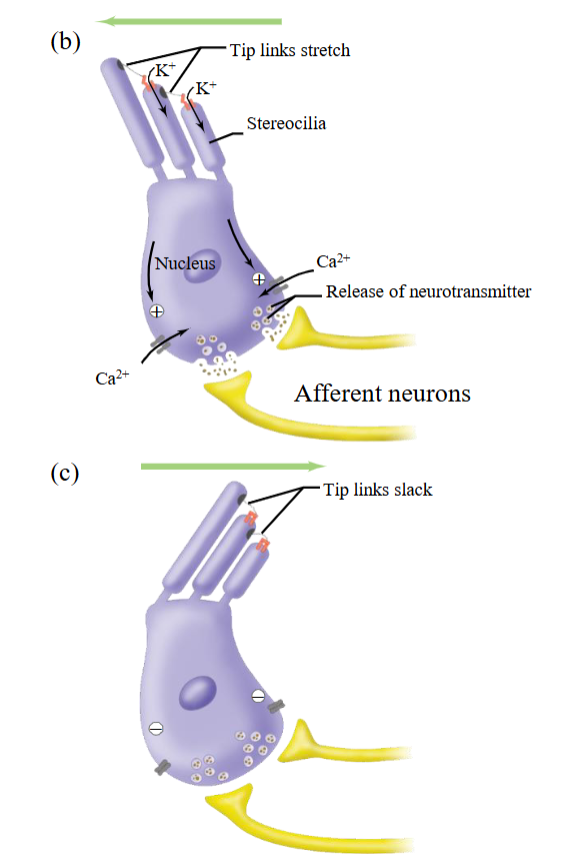
AP - Stereocilia
When stereocilia bend toward the tallest bundle member, mechanically-gated cation channels open, and K⁺ flows into the hair cell down its gradient.
As K⁺ enters, the hair cell depolarizes, generating a graded potential and triggering the release of glutamate onto afferent neurons.
Step two.
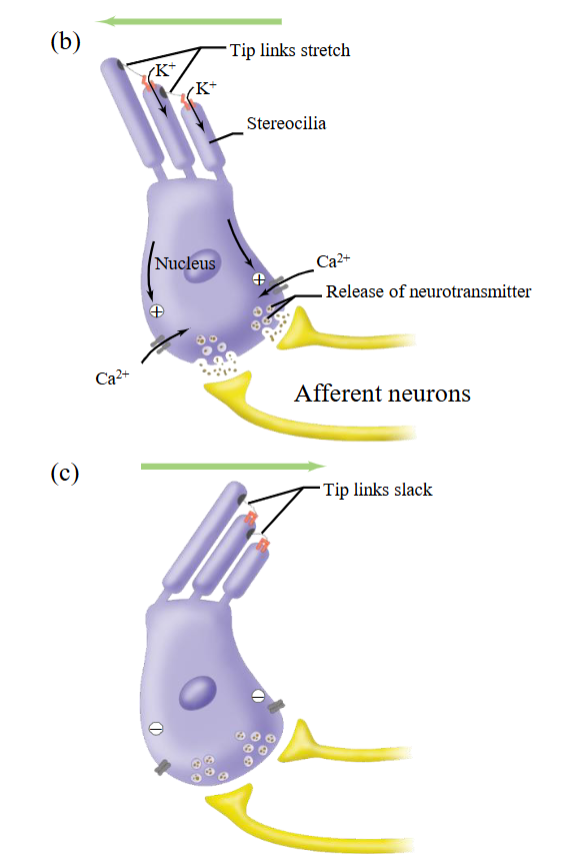
AP - Activation
If enough glutamate is released to bring these afferent neurons to threshold, APs are generated in the vestibulocochlear nerve and travel to the brain.
∴ Activation of the auditory system.
Step three.
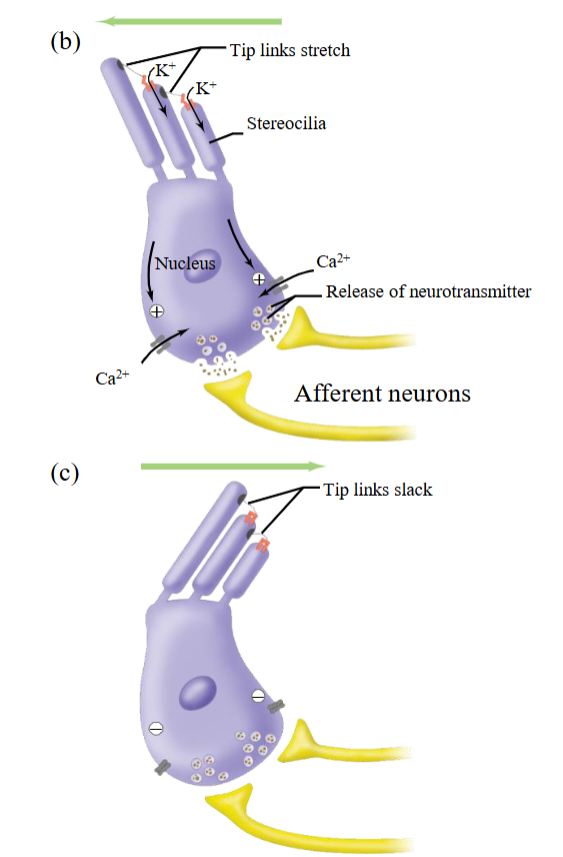
AP - Slack
Bending of the hair cells in the opposite direction closes the channels, allowing the cell to rapidly repolarize.
Last step.
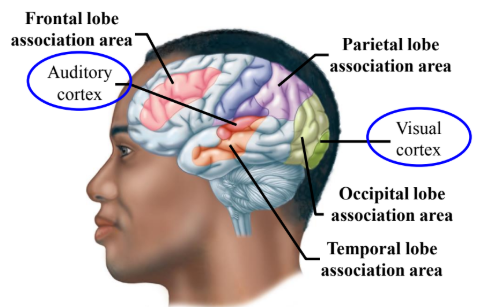
Neural Pathways in Hearing
Cochlear nerve fibers synapse with interneurons in the brainstem.
From the brainstem a multineuron pathway transmits information through the thalamus to the auditory cortex in the temporal lobe.
Hearing Aids
Amplifier placed in auditory canal which activates existing auditory “machinery.”
For people whose auditory machinery in the ear is not as sensitive; eardrum doesn’t move as well.
Cochlear Implants
An externally located audio sensor receives sound input and activates electrodes that physically stimulate the cochlear nerve.
The receiver on the outside of the head bypasses the outer, middle, and inner ear, delivering sound information directly.
It electrically stimulates the vestibulocochlear nerve in a way that preserves sound features for accurate processing by the cortex.