Digestive system (copy)
1/236
Earn XP
Description and Tags
ANP1107B
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
237 Terms
Functions of the digestive system
Take in food
Break it down into nutrient molecules
Absorb molecules into the bloodstream
Rid body of any indigestible remains
Nutrient production
synthesis of vitamins by bacteria that live in the intestine (ie. vitamin K(for clotting factors), Vitamin B, biotin)
production of neurotransmitters, hormones, and hormone-like compounds
hormones like grehlin, cholecystokinin, etc
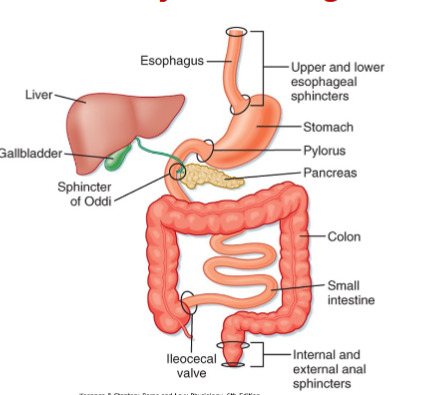
Alimentary canal
mouth
pharynx
esophagus
small intestine
large intestine
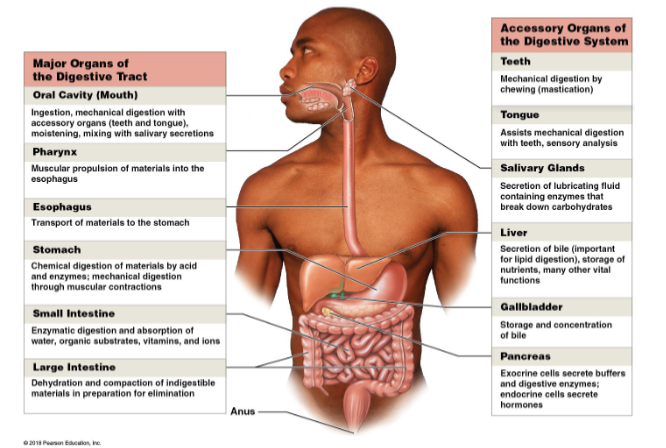
accessory organs
teeth
tongue
salivary glands
liver
gallbladder
pancreas
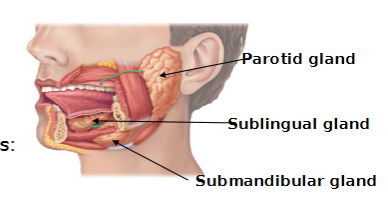
3 salivary glands
Parotid: contains mostly serous cells
Sublingual: contains mostly mucous cells
Submandibular: contains mostly serous cells
Gastrointestinal tract activites
Ingestion
churning due to action of smooth muscles
Mechanical breakdown
Propulsion
swallowing
peristalsis
Chemical Digestion
Absorption
catabolism
segmentation
Compaction (job of the colon/large intestine)and Defecation
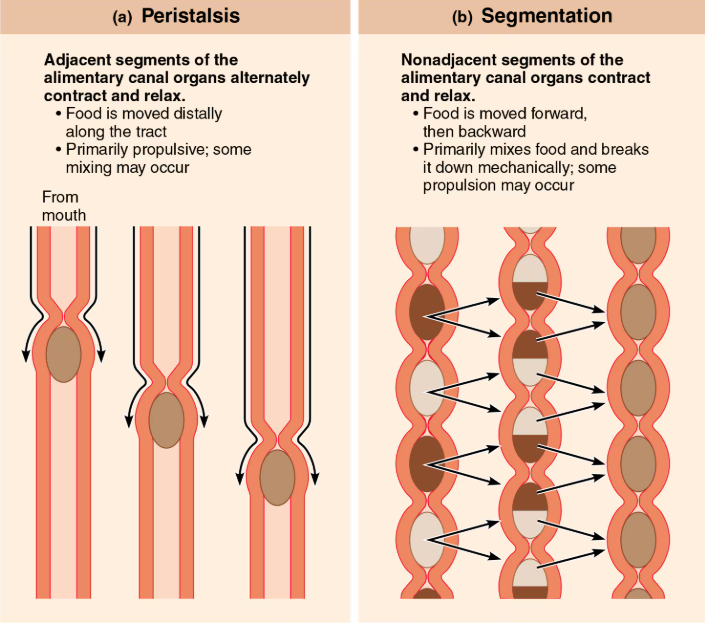
Peristalsis vs segmentation
Peristalsis
involuntary
adjacent segments of the alimentary tract organs alternately contract and relax
some mixing may occur
food is moved forward (distally along the tract)
Segmentation
Nonadjacent segments of alimentary tract organs alternately contract and relax
food mixing (pinching/contraction and relaxation at different points)and breakdown; slow propulsion occurs.
food is moved forward and backward
Peritoneum
serous membrane that lines the abdominal cavity that consists of visceral peritoneum and parietal peritoneum
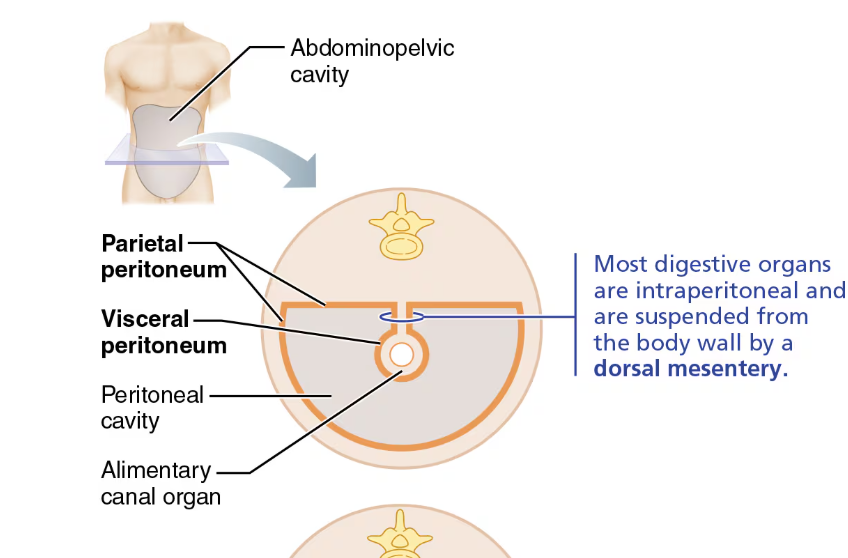
Visceral peritoneum
Membrane on external surface of most digestive organs
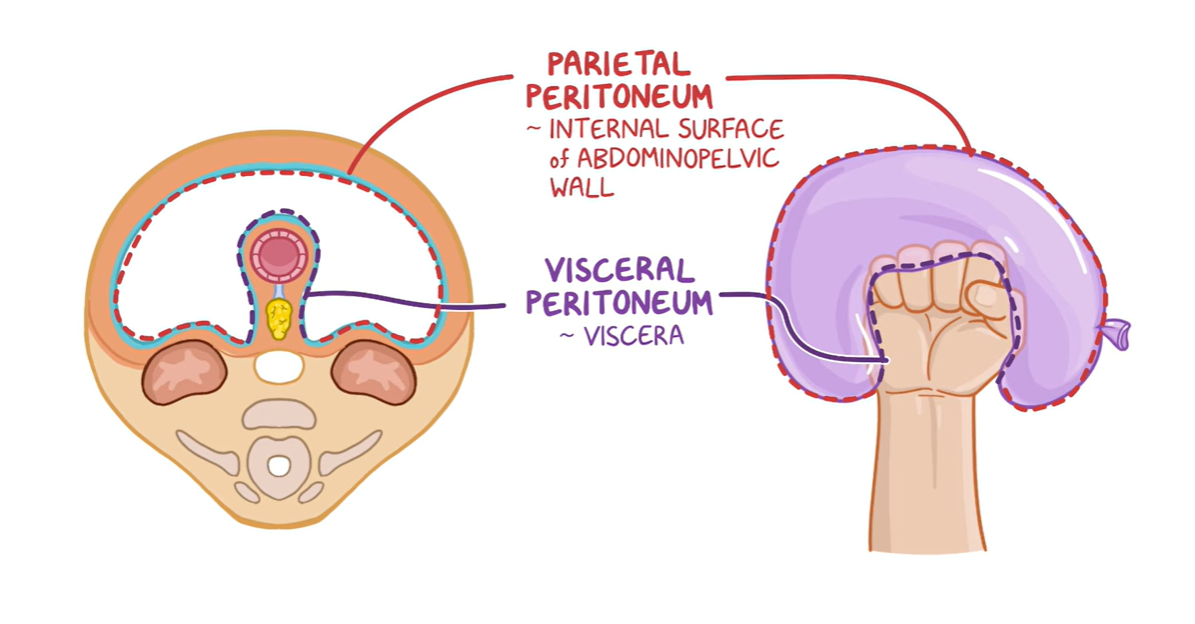
Parietal Peritoneum
membrane that lines body wall
Parietal cavity
Fluid-filled space within abdomen, lined by the peritoneum/ contains most abdominal organs
fluid lubricates mobile organs
Intraperitoneal
organs located within the peritoneum
Retroperitoneal
Located outside of/posterior to the peritoneum
includes most of pancreas, duodenum, and parts of large intestine
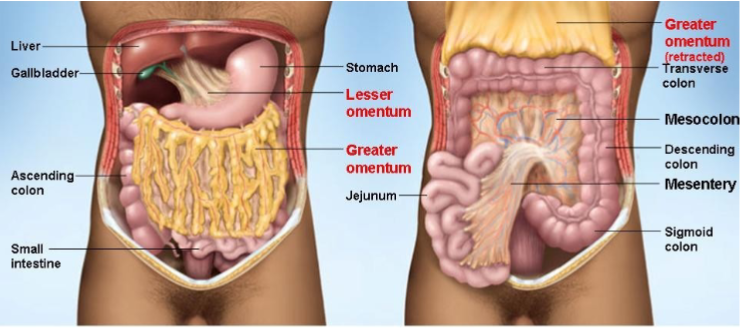
Mesentery
double layer of peritoneum fused together that extends to the organs from the body wall mostly posterior.
provides support for organs/hold them in place
provides support for vessels and nerves supplying organs
stores fat
Alimentary canal
extends from mouth to anus
most of the length made up of small intestine
consists of 4 tissue layers
as food moves thru the canal, it is broken down chemically by a variety of juices secreted by the organs of the digestive system
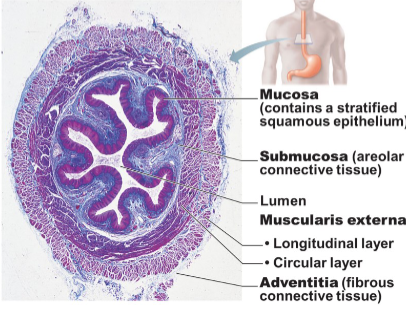
4 basic layers/ tunics of digestive organs
Mucosa(innermost layer) →Submucosa→ Muscularis externa→ serosa
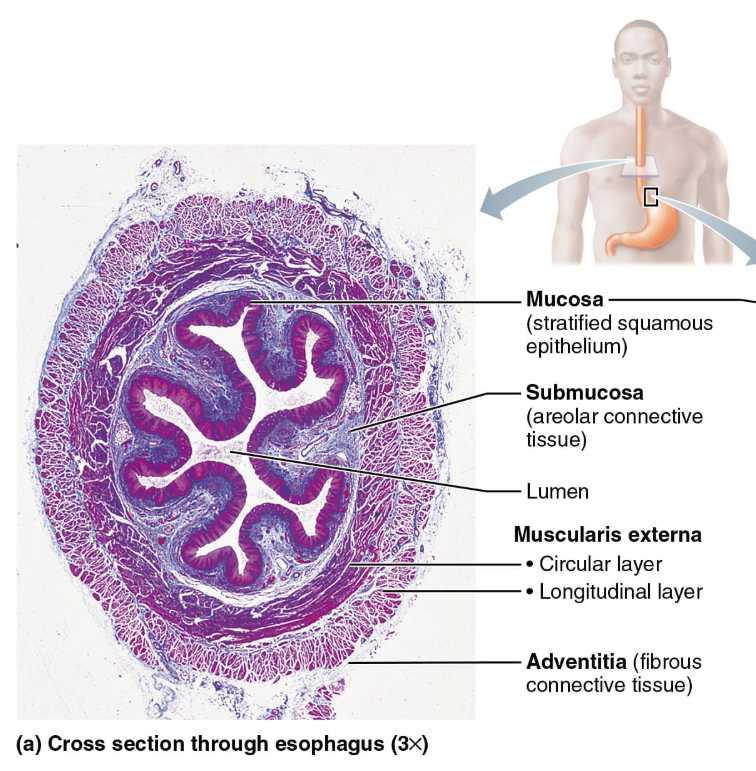
functions of the mucosa
secretion: mucus, digestive enzymes, hormones
absorption: end products of digestion
protection: against infectious disease
3 sublayers of mucosa
Epithelium(avascular)
simple columnar epithelium rich in mucus-secreting (goblet) cells
mucus (protects digestive organs from enzymes; eases food passage)
may secrete enzymes and hormones (e.g. in stomach and small intestine)
Lamina Propria(below epithelium)
loose areolar CT; capillaries for nourishment/absorption
lymphoid follicles (part of MALT)-protection
Muscularis mucosae
smooth muscle that produces local movements of mucosa
Submucosa
areolar connective tissue
blood and lymphatic vessels, lymphoid follicles
submucosal nerve plexus
abundant in elastic fibers (allows stomach to regain shape after large meal)
Muscularis externa
segmentation and peristalsis
inner circular and outer longitudinal layers
sphincters in organ-to-organ junct
Serosa
Visceral peritoneum-outermost protective layer
areolar connective tissue covered with mesothelium
replaced by the fibrous adventitia(area where there is no serosa, just collagen fibers) in the esophagus (adventitia: fibrous connective tissue that ‘binds’ the esophagus to surrounding tissues
What type of organs have both adventitia and serosa
retroperitoneal organs have both adventitia and serosa
serosa on the side facing the peritoneal cavity and an adventitia (fibrous sheath) on the side against the dorsal body wall
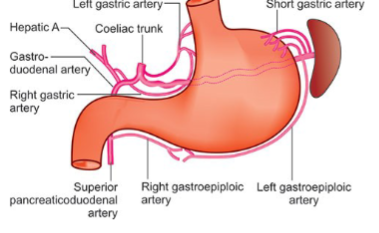
Splanchnic circulation
Splanchnic=related to viscera
portal system=back to back capillary beds
Arteries that branch off the abdominal aorta to serve the digestive organs
Hepatic, splenic, and left gastric of the celiac trunk (serve the liver, spleen and stomach)
Inferior and superior mesenteric (serve small and large intestine)
Venous return from much of the abdominopelvic region is via inferior vena cava.
Venous return from the digestive viscera is indirect via the hepatic portal circulation.
Why does venous return from digestive viscera via hepatic portal circulation
Enteric nervous system (ENS)
Semi-autonomous
Also called the gut brain; enteric neurons that communicate extensively with each other/major nerve supply to GI tract wall that controls motility
Has 2 plexus
linked to CNS via AFFERENT visceral fibers
motor fibers of the ANS
sympathetic impulses
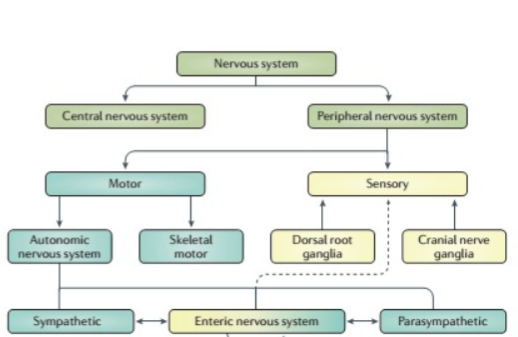
Submucosal nerve plexus (neurons)
contains sensory and meotor neurons/regulates glands an smooth muscles in mucosa
Myenteric nerve plexus
located between circular and longitudinal muscles
provides major nerve supply to GI tract
controls GI motility (pacemaker (sets pace/rhythm) cells and local reflex arcs between enteric neurons)
Short (local)reflexes
in response to stimuli inside the GI tract (internal)
control patterns of segmentation and peristalsis
NS controls digestive activity via intrinsic controls
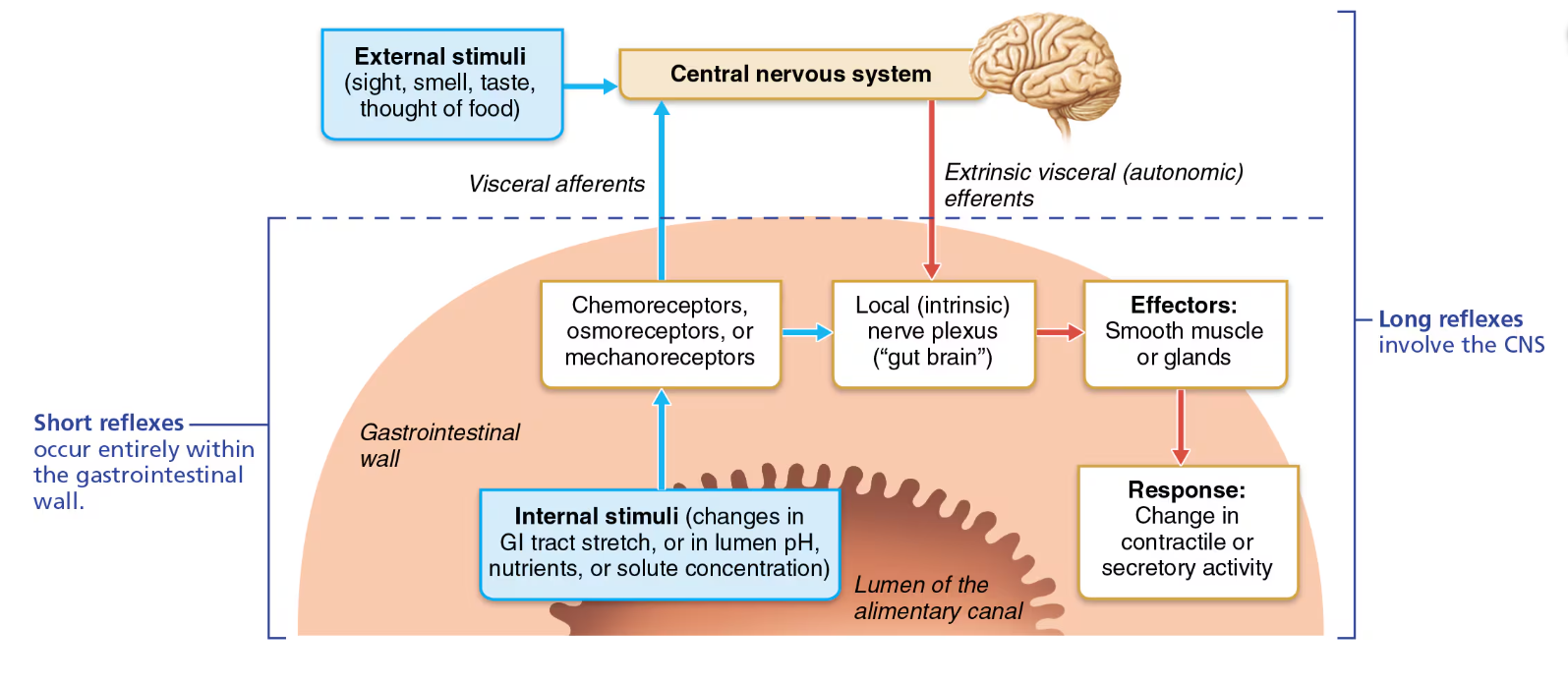
Long reflexes
in response to stimuli inside (internal) or outside(external) the GI tract
involve CNS centers and autonomic nerves
Because GI tract can’t act independently of the body, thus we need long reflexes
NS controls digestive activity via extrinsic controls
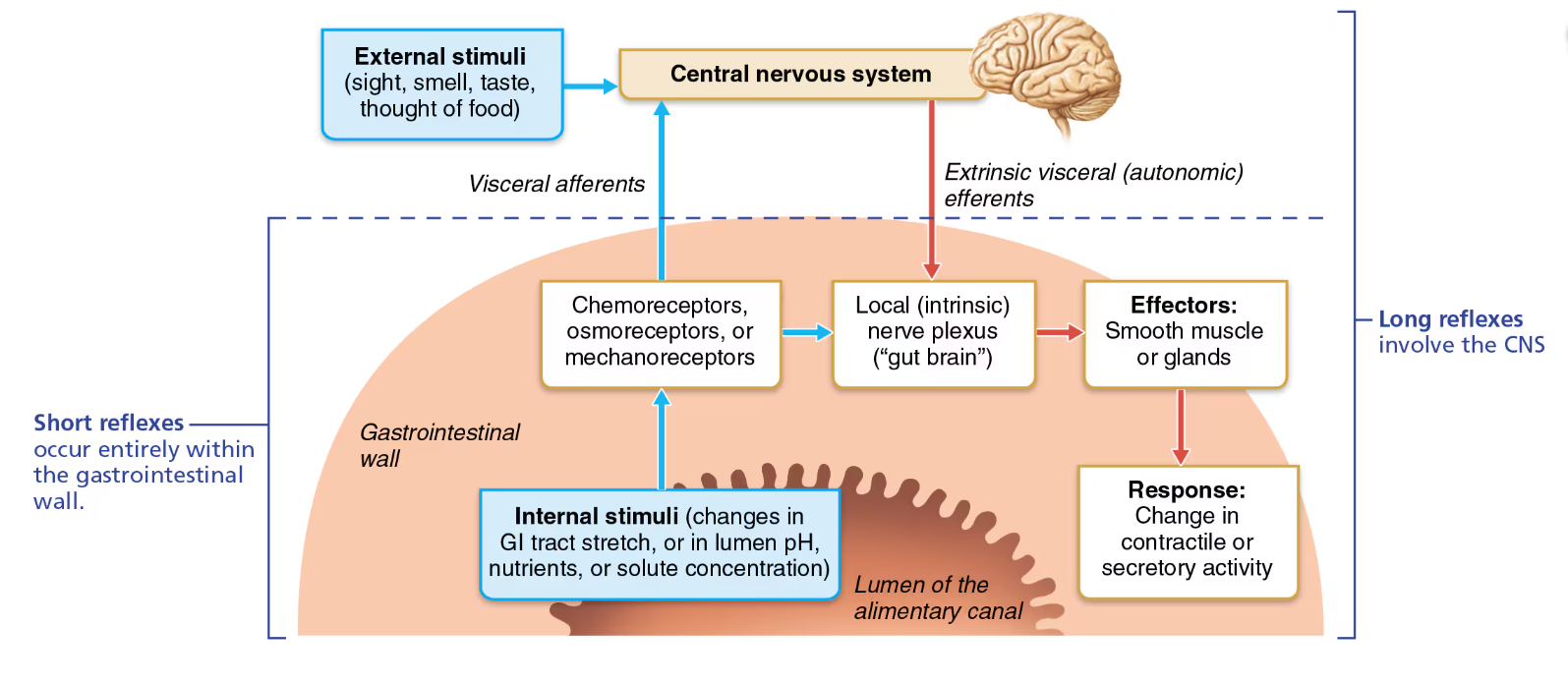
3 key concepts that regulate GI activity
Digestive activity provoked by mechanical/chemical stimuli
Effectors of digestive activity are SM and glands
Nervous system (intrinsic and extrinsic) and hormones control digestive activity
Digestive activity provoked by mechanical/chemical stimuli
receptors in walls of GI tract organs respond to stretch, changes in osmolarity and pH, the presence of substrate and end products of digestion
Effectors of digestive activity are SM and glands
Receptors initiate reflexes that stimulate SM to mix and move lumen contents
reflexes can also activate or inhibit
Anatomy of digestive system
Oral (buccal) cavity
basically your mouth
bounded by lips, cheeks, palate and tongue
oral orifice is the anterior opening
walls lined with stratified squamous epithelia
Don’t contain keratin like epidermis
beginning of digestion and initiation of swallowing
food is chewed and mixed with enzyme-containing saliva
Associated organs include: tongue, salivary glands, teeth
Lips and cheeks
lips (labia): composed of fleshy obicularis oris muscle
oral vestibule(a space): recess internal to lips and cheeks, external to teeth and gums
Cheeks : composed of buccinator muscles
oral cavity proper: lies within teeth and gums
lingual frenulum: attaches tongue to the floor of the mouth
labial frenulum: median attachments of each lip to gum
Hard palate
soft palate
Tongue
is a skeletal muscle
has :
intrinsic muscles that change shape of tongue
extrinsic muscles alter the tongue’s position
functions of tongue
repositioning and mixing of food during chewing
formation of bolus
initiation of swallowing, speech, taste
Ankyloglossia (tied tongue)
lingual frenulum is really short
congenital condition
Parts of the tongue
Terminal sulcus marks division between
Body: anterior 2/3 residing in the oral cavity
Root: posterior third residing in oropharynx
Surface papillae (projections of lamina propria covered with epithelium):
1. Foliate—on the lateral aspects of the posterior tongue
2. Vallate—V-shaped row in back of tongue
3. Filiform—whitish, give the tongue roughness and provide friction
4. Fungiform—reddish, scattered over the
tongue
*Vallate, foliate and fungiform papilla contain taste buds involved in detecting the elements of taste perception
taste qualities are found in all areas of the tongue, some regions are more sensitive than others
Salivary glands
secretes saliva which:
cleanses mouth
dissolves food chemicals for taste
moistens food; compacts for taste
begins breakdown of starch with enzyme amylase
Intrinsic (buccal) glands
scattered in oral mucosa
extrinsic (major glands)
lie out the mouth and release their secretion into the mouth via ducts
Glands
composed of 2 types of cells:
serous cells: produce watery secretion, enzymes, ions, bit of mucin
Mucous cells: produce mucus
Composition of saliva
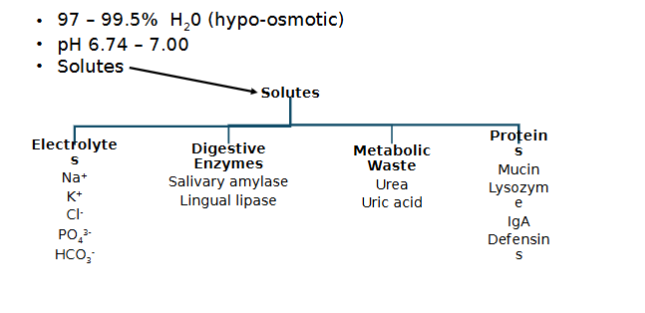
Control of salivation
1500 ml/day can be produced
Minor glands continuously keep mouth moist
When are major salivary glands activated by ANS
salivation is primarily controlled by parasympathetic division
when:
Ingested food stimulates chemo- & mechanoreceptors in mouth, send signals to:
Salivatory nuclei in brain stem that stimulate parasympathetic impulses along fibers in cranial nerves VII and IX to glands
sympathetic fibers (T1-T3)=slow down prod. of saliva/produces thick mucin-rich saliva
parasympathetic=more prod. of saliva
Other stimuli:
Swallowing irritating foods; nausea(protective reflex to protect the mouth/throat to neutralize stomach acid); smell/sight of food or upset GI can act as stimuli
Chemoreceptors are activated by…
acidic substances
mechanoreceptors are activated by
any mechanical stimulus in the mouth
Teeth
lies in sockets(dental alveoli) in gum-covered margins of mandible and maxilla
2 sets of teeth
deciduous(milk) teeth →24 mo.
32 permanent teeth→ develop by 6 yrs
Mastication(must know)
process of chewing that tears and grinds food into smaller fragments
production of bolus (lump) easy to swallow
Mechanical mastication
closed lips and cheeks
teeth
tongue
Chemical mastication: enzyme
breakdown of starch by salivary amylase
breaking of fats by lingual lipase (in the stomach but with the enzyme produced in the mouth)
incisors
chisel shaped tooth for cutting
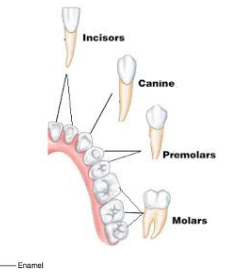
Canines
fanglike tooth that tear or pierce
Premolars (bicuspids)
posterior to canines
broad crowns with rounded cusps used to grind and crush
Molars
broad crowns, multiple rounded cusps: best grinders
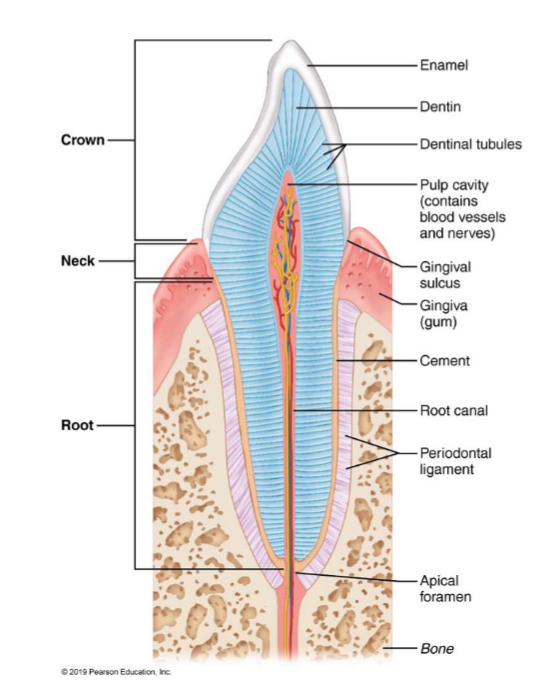
2 major regions of a tooth
crown: exposed part above gingiva (gum)
outermost part=enamel(contains hydroxyapatite minerals)
no cells/organic material
dentin: sensitive to stimuli
periodontal ligament: fibrous connective tissue
Root: portion embedded in jawbone-connected to crown by neck
Digestive process of the mouth
ingestion
mechanical breakdown by chewing
initiates propulsion by swallowing
starts chemical digestion of polysaccharides
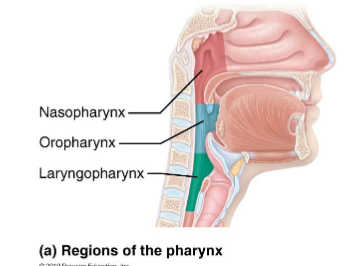
Pharynx(throat)
allows passage of food, fluids, and air
food passes from mouth into oropharynx and then into laryngopharynx
stratified squamous epithelia lining with mucus (bc of goblet cells) producing glands
external muscle layers consists of 2 skeletal muscle layers
inner layer of muscles runs longitudinally
outer pharyngeal constrictors encircle wall of pharynx
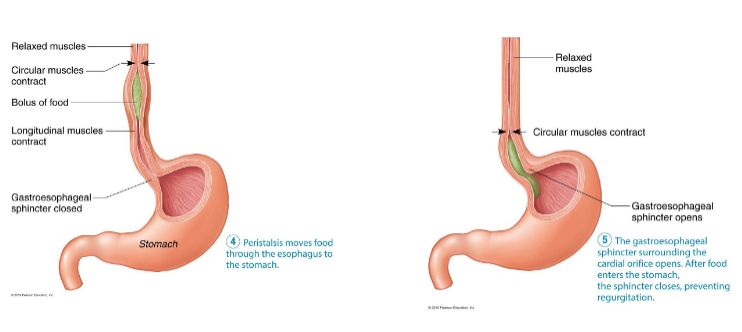
Esophagus
Flat muscular tube (~25 cm) that runs from laryngopharynx to stomach
food moves via peristalsis
collapsed when not involved in food propulsion
pierces diaphragm at esophageal hiatus(opening in diaphragm)
joins stomach at cardial orifice
has all 4 alimentary canal layers unlike mouth and pharynx
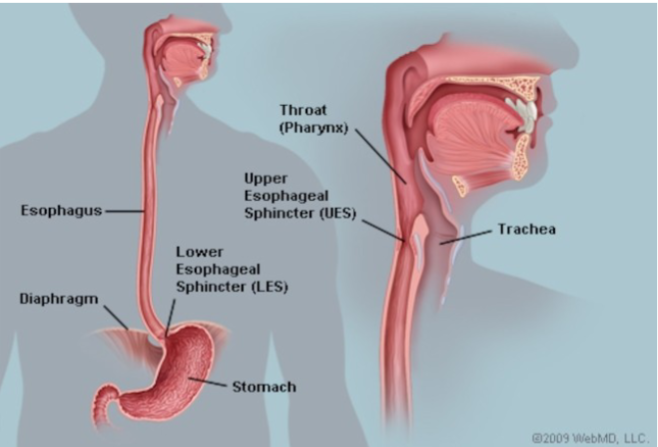
lower esophageal sphincter
AKA Gastroesophageal (cardiac) sphincter
surrounds cardial orifice
keeps orifice closed when food is no swallowed
mucus cells on both sides of sphincter help protect esophagus from acid reflux
Hiatal hernia
a structural abnormality in which the superior part of the stomach protrudes slightly above the diaphragm.
Since the diaphragm no longer reinforces the sphincter, gastric juice may enter the esophagus, particularly when lying down.
4 alimentary canal layers of esophagus
Esophageal mucosa contains SSE that changes to simple columnar epithelium at the stomach
Esophageal glands in submucosa secrete mucus to aid in bolus movement
Muscularis externa: skeletal muscle superiorly; mixed with skeletal and smooth in middle; smooth muscle inferiorly
due to swallowing of voluntary and involuntary phases
example of structure and function
Has adventitia instead of serosa
Deglutition
AKA swallowing
Pharynx & esophagus: passage of food from mouth to stomach
Major function of both organs is propulsion that starts with deglutition (swallowing)
Involves the tongue, soft palate, pharynx, esophagus, 22 muscle groups & 2 phases
2 phases of deglutition
Buccal phase
voluntary contraction of tongue
ends when bolus leaves the mouth and stimulates tactile receptors in posterior pharynx
Pharyngeal-esophageal phase
involuntary
control swallowing center in medulla and lower ponds

How is passage of food regulated
2 sphincters: upper and lower esophageal sphincters
peristalsis: (involuntary muscle movements controlled by oblongata) and facilitated by mucus produced by submucosal glands
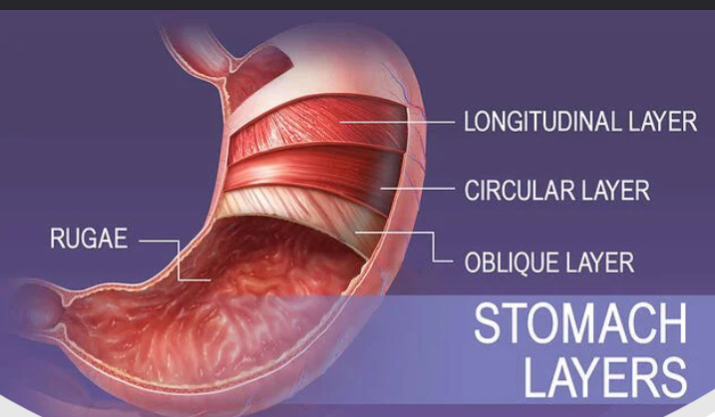
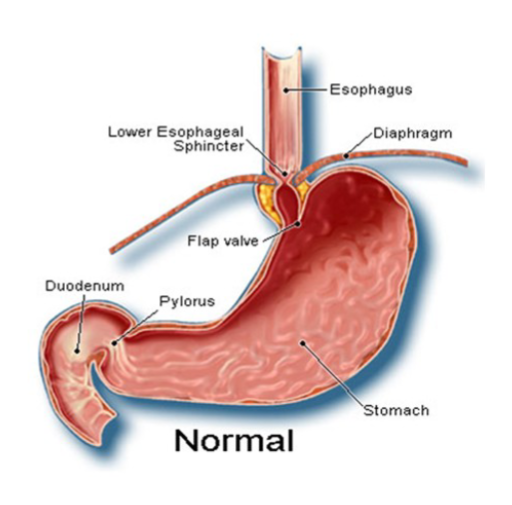
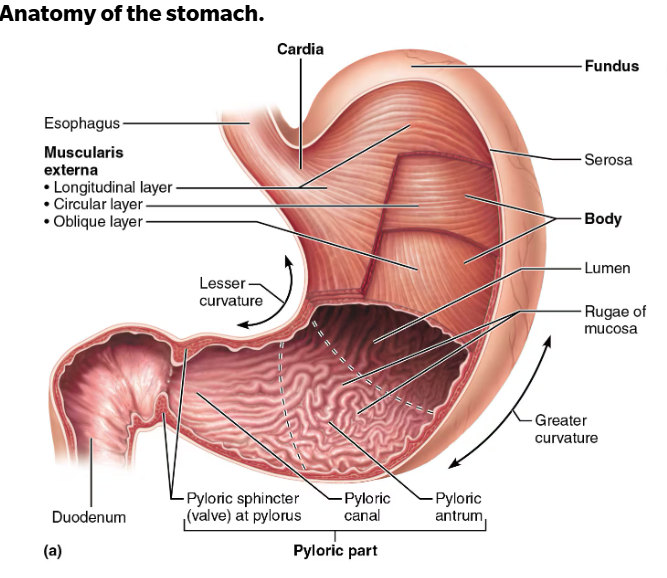
Stomach
3 layers: longitudinal, circular, and oblique layer
a temporary storage tank that starts chemical breakdown of protein digestion
Converts bolus of food to paste-like chyme (bolus + gastric juice)
Empty stomach has ~50 ml volume but can expand to 4L
When empty, stomach mucosa forms many folds called rugae
helps stomach expand for larger meals
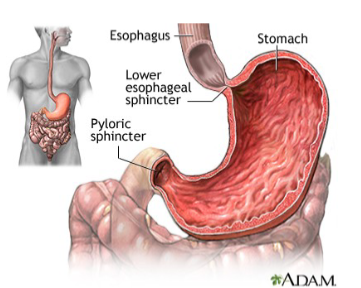
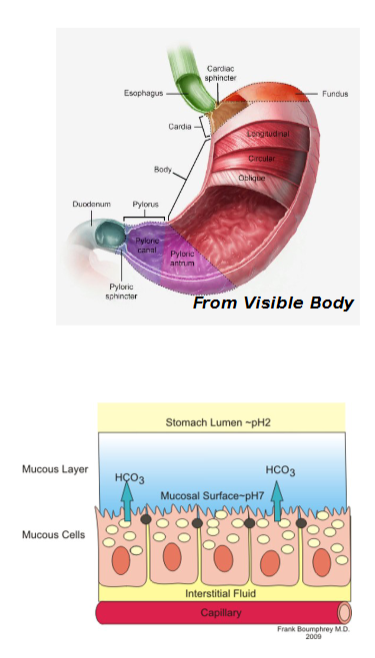
Major regions of the stomach
Cardial part (cardia): surrounds cardial orifice
Fundus: dome-shaped region beneath diaphragm
Body: midportion. major part for mixing food
Pyloric part: wider and more superior portion of pyloric region, antrum, narrows into pyloric canal that terminates in pylorus
Pylorus is continuous with duodenum through pyloric valve (sphincter controlling stomach emptying)
Greater curvature: convex lateral surface of stomach
Lesser curvature: concave medial surface of stomach
Lesser omentum(curvature)
runs from liver to lesser curvature of stomach, where it becomes continuous with visceral peritoneum
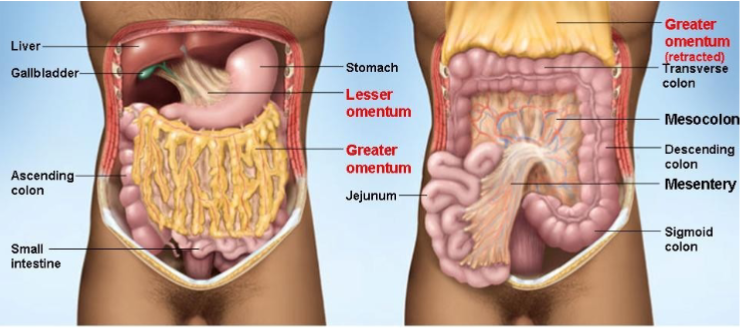
Greater omentum(curvature)
drapes inferiorly from greater curvature over intestine, spleen, and transverse colon; blends with mesocolon (mesentery that anchors large intestine to abdominal wall)
basically covers anterior part of abdominal cavity
Contains fat deposits and lymph nodes
ANS supplies what part of stomach
Sympathetic fibers via splanchnic nerves via the celiac plexus(ganglion)
Parasympathetic fibers are supplied (resting and digesting) via vagus nerve(1 of 12 cranial nerves)
Blood supplies what part of stomach
arterial supply of blood is provided celiac trunk system
venous drainage: drain hepatic portal vein
Muscularis externa
is modified
Three layers of smooth muscle
Circular, longitudinal & inner oblique layer allows stomach to churn, mix, move & physically break down food
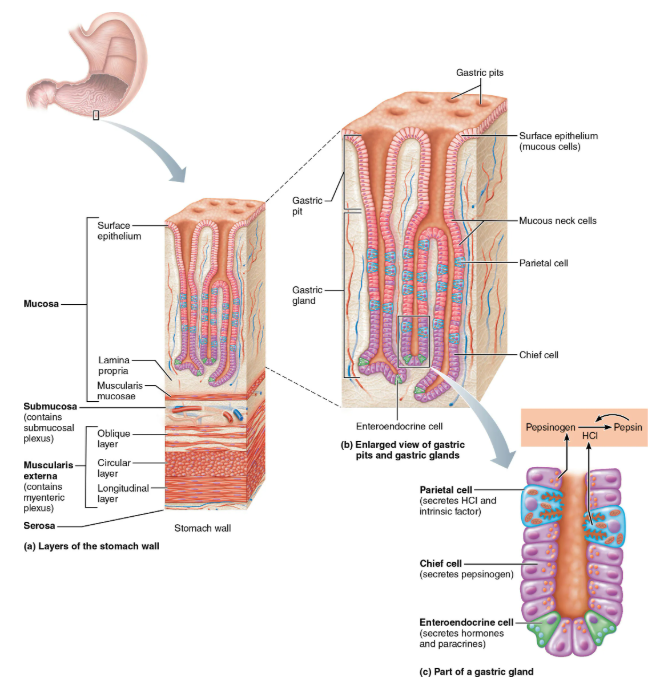
Mucosa layer
also modified
lines the lumen
Simple columnar epithelium entirely composed of mucous cells
Secrete 2-layer coat of alkaline mucus
Surface layer traps bicarbonate- rich fluid layer that is beneath it
Dotted with gastric pits, which lead into gastric glands that produce gastric juice
Microscopic anatomy of stomach
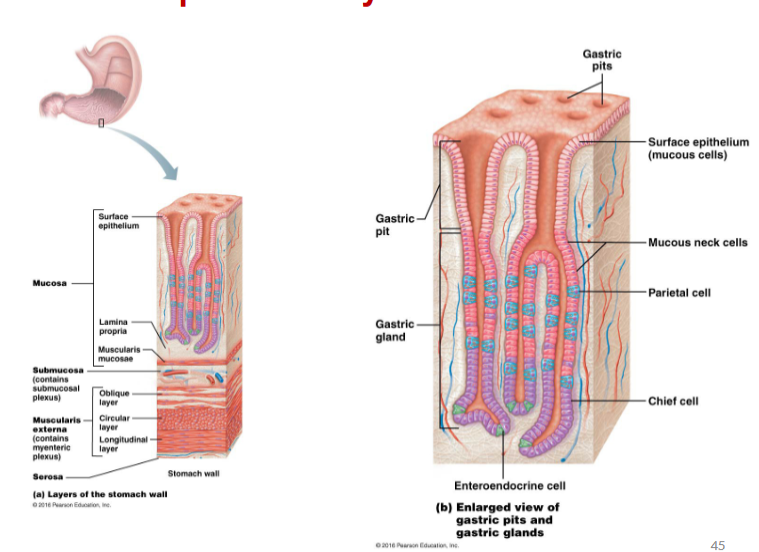
Glandular cells of the stomach
Mucous neck cells
parietal cells
chief cells
enteroendocrine cells
Mucous neck cells
Secrete thin, acidic, slightly soluble mucus of unknown function
helps lubricate and protect gastric glands
different from mucus of the surface epithelium
specialized stem cells
Parietal cells
secrete Hydrochloric acid (HCl), which denatures protein, activates pepsin, breaks down plant cell walls, and kills many bacteria
secretes Intrinsic factor: a glycoprotein req. for necessary absorption of vit. B12 in small intestine(ilium)
without it=pernicious anemia
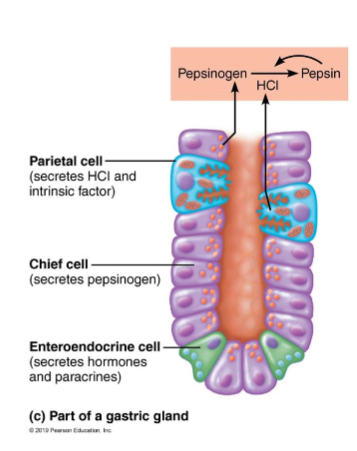
Chief cells
secrete Pepsinogen (activated to pepsin by HCl & by pepsin itself
+ve feedback mechanism that is limited by amount of pepsinogen present
-ogen: inactive form
secretes gastric lipases (digests ~15% of lipids)
Enteroendocrine cells
secrete Hormones:
gastrin (needed for HCL secretion; opening of pyloric sphincter, regulating stomach’s secretion and motility)
ghrelin (stimulates appetite, gastric motility and opening) & somatostatin
Paracrines: histamine and serotonin
paracrine: acts on structures close by
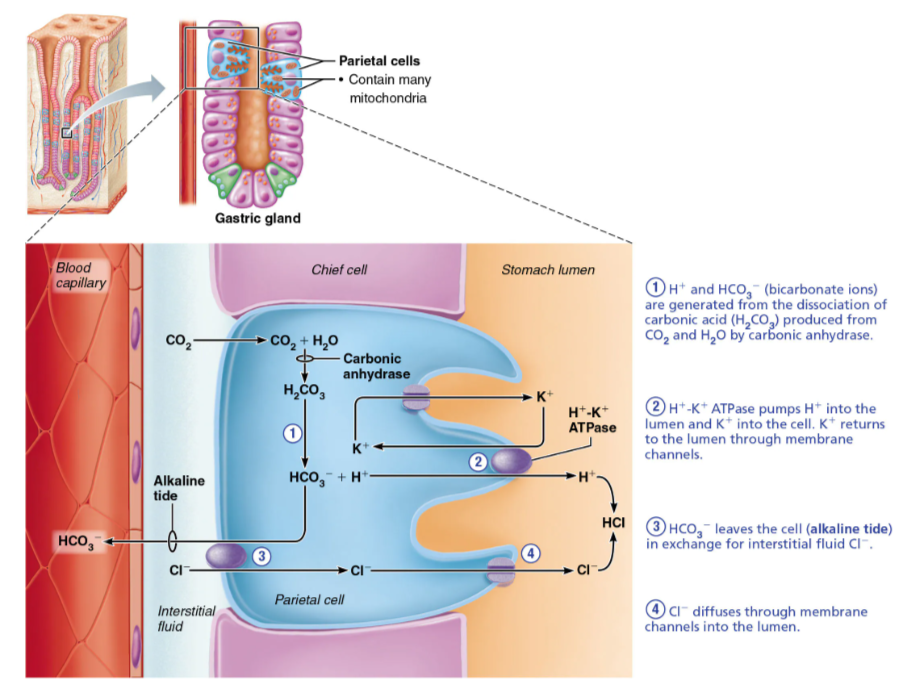
HCL formation
Parietal cells pump H+ (from carbonic acid breakdown) into stomach lumen via H+/K+ ATPase (proton pumps)
– As H+ is pumped into stomach lumen, HCO3- is exported back to blood via Cl− and HCO3- antiporter
• Resulting increase of HCO3- in blood leaving stomach is referred to as alkaline tide
– Cl− is pumped out to lumen to join with H+, forming HCl
Carbonic anhydrase forms carbonic acid
H2CO3 (carbonic acid) → HCO3- + H+ (bicarbonate + hydrogen ions)
H+ + K+ ATPase(antiporter) pumps:
H+→ the lumen
K+→ the cell.
(K+ returns to the lumen through membrane channels)
Cl- in the interstitial fluid is exchanged for intracellular HCO3-.
Cl- diffuses through membrane channels into the lumen
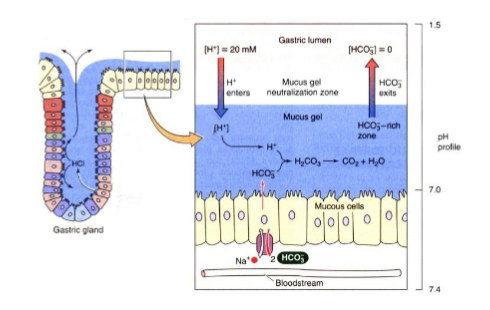
Mucosal barrier of stomach
Harsh digestive conditions require stomach to be protected
Mucosal barrier protects stomach and is created by 3 factors
3 factors that create mucosal barrier
Thick layer of bicarbonate-rich mucus
Tight junctions between epithelial cells
Prevent gastric juice from seeping underneath tissue
Damaged epithelial cells are quickly replaced by division of intestinal stem cells (ISC)
to avoid holes or sores in stomach
Surface cells replaced every 3–6 days
Digestive processes of the stomach
Holding area for food
Propulsion
Mechanical breakdown of food
Chemical Digestion
Absorption
Delivers chyme to small intestine
Propulsion activity of the stomach
exhibits peristalsis
Mechanical breakdown of food in stomach
caused by churning action by smooth muscle of stomach during peristalsis
Chemical digestion of food in stomach
HCl denatures proteins by HCl in preparation for enzymatic digestion
Pepsin: most important protein digesting enzyme is produced by gastric mucosa
In infants: milk protein (casein) is broken down by rennin(chymosin), secreted by stomach glands
Results in curdy substance
gastric and lingual lipases acting in acidic pH of stomach aid in fat digestion
Absorption
Not much absorption in the stomach
2 common lipid-soluble substances:
alcohol and aspirin are absorbed into blood via stomach mucosa
what is the only stomach function essential to life
secretion of intrinsic factor for vitamin B12 absorption
B12 is needed for red blood cells to mature
Lack of intrinsic factor causes pernicious anemia
Treated with B12 injections
How is gastric secretion regulated
Gastric mucosa secretes >3 L of gastric juice/day and are regulated by
Neural mechanisms:
Hormonal mechanisms
Neural mechanisms that controls gastric secretion
Vagus nerve stimulation increases secretion
are parasympathetic
release ACh stimulates output of gastric juice
sympathetic stimulation decreases secretion
Hormonal control of gastric secretion
Gastrin stimulates enzyme and HCL secretion
Gastrin antagonists are secreted by small intestines
3 phases of gastric secretions
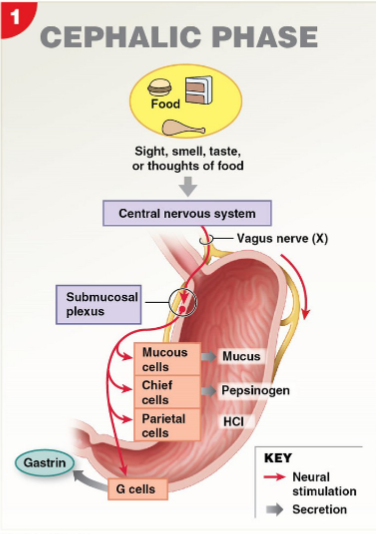
Cephalic (reflex) phase
Gastric phase
intestinal phase
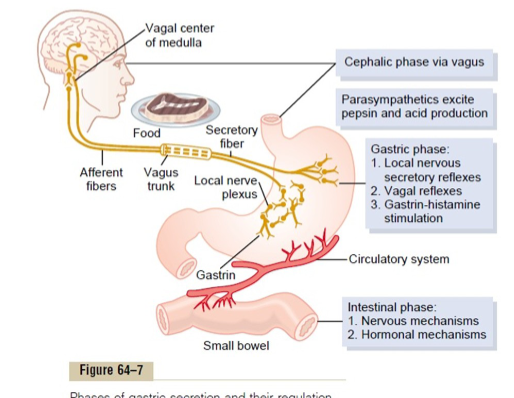
Cephalic (reflex) phase
occurs before food enters the stomach
reflexes triggered by sensory receptors in the head (sight, smell, taste), or by thought
triggers act via vagus nerve to stimulate gastric gland, preparing stomach to begin digestion
Gastric phase
occurs once food enters stomach
Lasts 3–4 hours & provides 2/3 of gastric juice
Stimuli: distension, peptides and amino acids
Stretch (mechano) receptors – detect distention of stomach / initiate neural (both long & short) reflexes
Chemo receptors - chemical stimuli, e.g. peptides, caffeine, & low acidity activation of enteroendocrine (G) cells in lumen of stomach
detects chemical changes in composition of contents in stomach
role of gastrin in stimulation of gastric phase
Buffering action of ingested proteins causes pH to rise, which activates more gastrin secretion
Prods parietal cells to secrete HCl by:
1. Binding to receptors on parietal cells (directly)
2. Stimulating enteroendocrine cells to release histamine (indirect)
Inhibition of gastric phase
Low pH inhibits gastrin secretion
Occurs between meals
Occurs during digestion as negative feedback mechanism
The more protein, the more HCl acid is secreted, causing decline in pH, which inhibits gastrin secretion
Intestinal phase
Begins with brief stimulatory component followed by inhibition
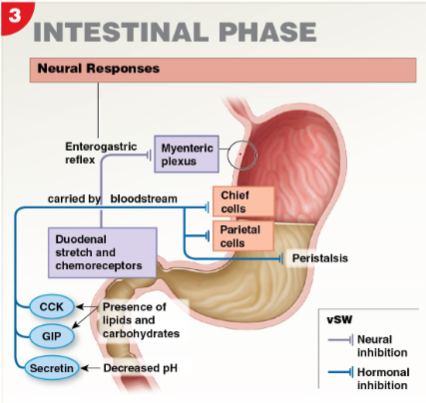
Stimulation of intestinal phase
Partially digested food enters small intestine, causing a brief release of intestinal (enteric) gastrin
Encourages gastric glands of stomach to continue secretory activities
Stimulatory effect is brief and overridden by inhibitory stimuli as intestine fills
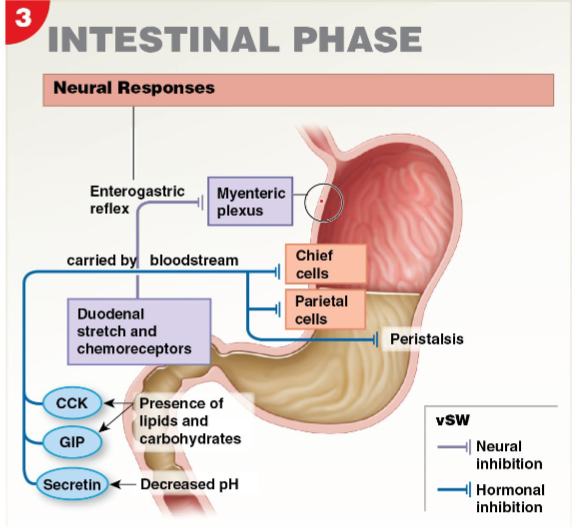
Inhibition by intestinal phase
Four main factors in duodenum cause inhibition of gastric secretions:
Distension of duodenum due to entry of chyme
Presence of acidic / fatty / hypertonic chyme
they prevent massive influx of chyme
inhibition is achieved in 2 ways
enterogastric reflex and enterogastrones
Enterogastric reflex (neural)
Duodenum inhibits acid secretion in stomach by: ENS short reflexes & long reflexes involving SNS and vagus nerve