Wound/Drain
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
Intentional

Unintentional

Neuropathic
defined as pain that results as a direct consequence of a lesion or disease affecting abnormal functioning of the peripheral nervous system (PNS) or central nervous system (CNS).
Venous Leg Ulcer
Common in elders
Result of chronic venous hypertension
Persistent inflammation
Hemosiderin Deposits
Lipodermatosclerosis

Diabetic Foot Ulcer
common in diabetes
hyperglycemia
micro/macroangiopathy
neuropathy
infection
foot deformities

Arterial Ulcer
reduced blood supply
ischemia, necrosis
little exudate
atrophic skin
common in diabetes
pain

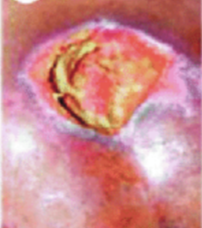
Pressure Sore
area of tissue necrosis
caused by prolonged soft tissue compression
Local ischemia, moisture
Multi morbid and elderly
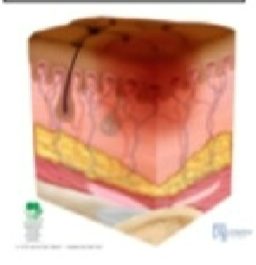
Stage 1
skin is unbroken but red and inflamed
Stage 2
Skin is broken on the top layers of skin only
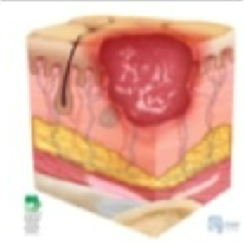
Stage 3
Injury extends down to the tissue under the skin

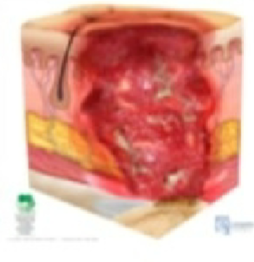
Stage 4
Loss of skin and tissue; exposed bones, cartilage or tendon.
Open Wound
Closed Wound

Acute

Chronic

Incision
Cutting or sharp instrument; wound edges well approximated and aligned; surrounding tissue undamaged; bleeds freely and least likely to become infected
Contusion
Blunt instrument, overlying skin remains intact, with injury to underlying soft tissue; possible resultant bruising and/or hematoma
Abrasion
Friction; rubbing or scraping epidermal layers of skin; top layer of skin scraped away; dirt and germs often embedded and can become infected
Laceration
Tearing of skin and tissue with blunt or irregular instrument; tissue not aligned, often with loose flaps of skin and tissue; frequently contaminated with dirt or other material ground into the wound and likely to become infected
Puncture
Blunt or sharp instrument puncturing the skin; intentional (such as venipuncture) or accidental; consider penetrating object when considering infection probability
Penetrating
Foreign object entering the skin or mucous membrane and lodging in underlying tissue; fragments possibly scattering throughout tissues
Avulsion
Tearing a structure from normal anatomic position; possible damage to blood vessels, nerves, and other structures
Chemical
Toxic agents such as drugs, acids, alcohols, metals, and substances released from cellular necrosis
Thermal
High or low temperatures; cellular necrosis as a possible result
Irradiation
Ultraviolet light or radiation exposure; can cause wet or dry desquamation
Venous Ulcer
Injury and poor venous return, resulting from underlying conditions, such as incompetent valves or obstruction; frequently have significant drainage; compression essential (after arterial flow verified)
Wound
a break or disruption in the normal integrity of the skin and tissues.
Pressure Ulcer
Compromised circulation secondary to pressure or pressure combined with friction; classified by Stages 1–4, Unstageable, and Deep Tissue injury
Arterial ulcers
Injury and underlying ischemia, resulting from a lack of blood flow to the lower extremities secondary to conditions such as atherosclerosis or thrombosis; many have black eschar; increasing blood flow essential for treatment
Diabetic ulcers
Injury and underlying diabetic neuropathy, peripheral arterial disease, diabetic foot structure; located below the ankle
Principles of wound healing
intact skin, careful hand hygiene, body responds adequate blood supply, normal healing is promoted, and extent of damage and the person’s state of health, response to wound is more effective.
Phases of the wound (in order)
Homeostasis
Inflammatory
Proliferation
Maturation
Homeostasis
Occurs immediately after initial injury
Inflammatory Phase
begins shortly after hemostasis and lasts about 2 to 3 days
Proliferation
(repair phase) Lasts for several weeks, new tissue is built to fill the wound space through the action of fibroblasts
Maturation
(remodeling) final phase begins about 3 weeks after injury and can continue for months or years
Local Factors Affecting Wound Healing
Pressure
Desiccation (dehydration)
Maceration (overhydration)
Trauma
Edema
Infection
Excessive bleeding
Necrosis (death of tissue)
Presence of biofilm (thick grouping of
microorganisms)
Systemic Factors (affecting the whole body)
Age
Circulation and Oxygenation
Nutritional status
Wound Etiology
Health status
Immunosuppression/Proinflammatory Conditions
Medication Use
Adherence to treatment plan
Wound Complications:
infections
hemorrhage
Dehiscence and