critical care pulmonary lecture
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
104 Terms
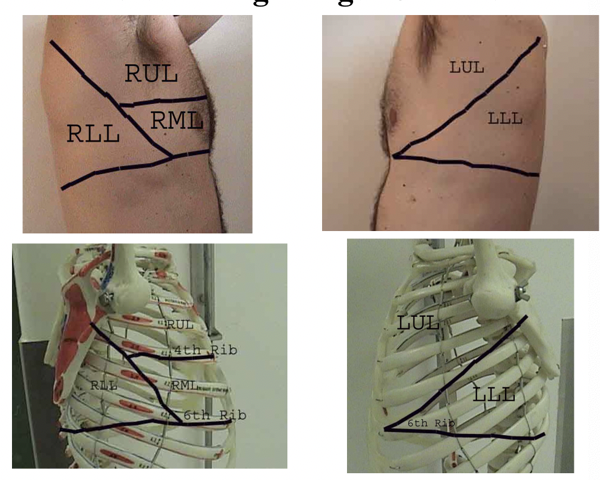
lateral visualizaton of lungs
atelactasis
collapse of alveoli leading to reduced gas exchange
types of atelactasis
obstructive: mucus plug (COPD, PF), forgien body, tumor
non obstructive:
most commonly caused by anesthesia
compressive - pneumothorax, hernia
contraction - scar tissue
adhesice - surfactacnt deficiency
CM:
dyspnea
hypoxia (O2sat 90%)
reduced breath sounds
crackles over area
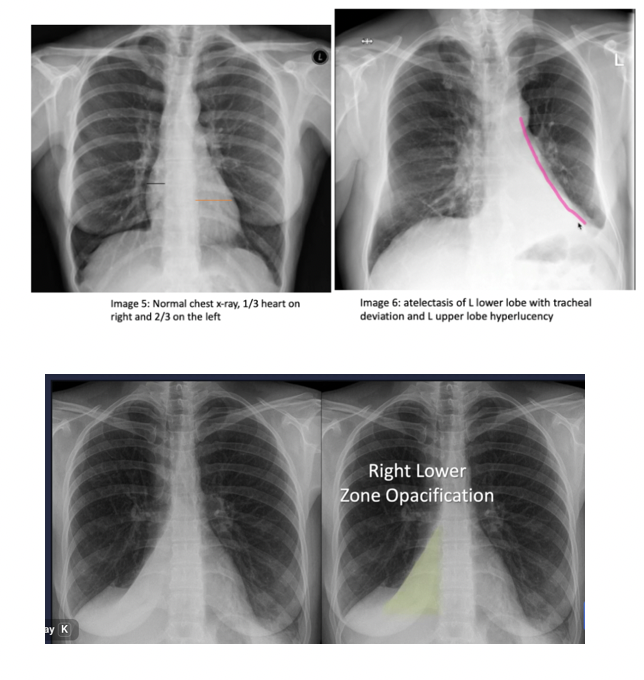
diagnosing atelectasis
chest Xray: colume loss, shift of fissuresm elebated hemidiaphram
ct when unclear: consider risk factors
nurisng interventions for ateleactasis
•Prevention
–Frequent turning
–Early mobilization
–Strategies to expand lungs and manage secretions
–Incentive spirometer
–Voluntary deep breathing
–Secretion management
–Pressurized metered-dose inhaler
-oral care
•Treatment: bronchial hygiene, bronchoscopy for mucus plugging, address underlying cause.
complications and pearls: can predipose to PNA and hypoxemia
acute tracheobronchitis
infammation of the mucus membranes of the trachea usually after a viral infection
patho of tracheobronchitis
Viral: “PAIR”
parainfluenza, advenovirus, influenza, rhinovirus
Bacterial
strep, pneumonea, haemophilus influenza (more likely COPD and smokers
SM
initially dry cough with mucoid sputum
as progresses, dyspnea, stridor, wheezes, purulent sputum

pneumonia
= inflammation of the lung parenchyma
exudate accumulates in teh alveoli
classifications of pneumonia
bacterial
viral
atypical
typical bacterial PNA
bacteria that normally resides in the nasopharynx of healthy people and do not cause a problem
through coughing and sneezing bacteria can travel to lungs causing infection
ss: fever, chills, productive cough, chest pain, dyspnea, shortness of breath.
need chest XR
streptococcal is what causes most of PNA*
viral PNA
determined by genetic material they carry
influenza, covid - the virus that causes covid 19, RSV
atypical PNA
mycoplasma or legionella or chlamydial
ss: beyond lungs
HA, fever, pharyngitis, rash joint pain, stomach ss NVD
physcial exam for PNA / ss
assessment: orthopnea (SOB when laying), crackles, increased tactile fremitus (palpable vibration in chest wall), purulent sputum
symptoms: Cough, fever, chills, HA, malaise, fatigue, leuritic chest pain, dyspnea
signs: tachycardia, tachypnea, use of accessory muscles, sputum, abnormal breath sounds
community aquired PNA
• Community setting or within first 48 hours post hospitalization
• Older more at risk
• S. Pneumoniae is the most common cause among adults
• Viral cause in infants and children
health care associated PNA
• Occurs in long term care facilities
• Often caused by multidrug‐resistant organisms
• Early diagnosis and treatment are critical
hospital aquired PNA
• Develops 48 hours or more after hospitalization
• Subtype of health care–associated pneumonia
• Potential for infection from many sources
• High mortality rate
• Colonization by multiple organisms due to overuse of antimicrobial agents
• Pleural effusion, high fever, and tachycardia
• Common with debilitated, dehydrated patients with minimal sputum production
ventilator associated PNA
• Develops 48 hours or more after hospitalization
• Subtype of health care–associated pneumonia
• Potential for infection from many sources
• High mortality rate
• Colonization by multiple organisms due to overuse of antimicrobial agents
• Pleural effusion, high fever, and tachycardia
• Common with debilitated, dehydrated patients with minimal sputum production
Pneumonia in the immunocompromised host
•Common agents include pneumocystis, fungi, and tuberculosis
•Receiving immunosuppressive agents, history of immunosuppressive condition
•Subtle onset with progressive dyspnea, fever, and nonproductive cough
risk factors for PNA
– Heart failure, diabetes, alcoholism, COPD, and AIDS
– Influenza
– Smokers
– Depressed cough reflex: age, anesthesia, sedation, medications, head injury, abnormal; swallow, Intubation
– ABX treatment… secondary infection in oropharynx
– Prolonged immobility
– Supine position ( Pt unable to protect airway)
– ETOH intoxication
– Cystic fibrosis
diagnosing PNA
hostory and hyscial exam
imaging
sputum examination
blood work
treatment for PNA
depending on what type: pharm” ABX or antiviral
oxygen
fluids
bed rest until clinically stable
nursing interventions: small frequent feedings, cough suppressants, antipyretics, bronchodolator’s, montir vs, rest/activity balance, hydration
nursing assessment and complicaions with bacterial Pneumonia
assessment:
•Vital signs
•Secretions: amount, odor, color
•Cough: frequency and severity
•Tachypnea, shortness of breath
•Inspect and auscultate chest
•Changes in mental status, fatigue, edema, dehydration, concomitant heart failure, especially in older adult patients
complications:
Continuing symptoms after initiation of therapy
•Sepsis and septic shock
•Respiratory failure
•Atelectasis
•Pleural effusion
•Delirium
planning and goals for pt with bacterial PNA
improved airway patency
increased activity
maintenance of proper fluid volume
maintenance of adequate nutrition
absense of complications
based on patient outcomes plan for home, community, and transitional care
nursing interventions for patient with bacterial PNA *
oxygen with humidification to loosen secretions
face mask or nasal cannula
coughing techniques
chest physiotherapy *
position changes
incentice spirometry
nutrition
hydration * (infection takes up fluid)
rest
activity as tolerated
pt education
self care
expected outcomes for patient with bacterial PNA
•Demonstrates improved airway patency
•Rests and conserves energy and then slowly increases activities
•Maintains adequate hydration; adequate dietary intake
•Verbalizes increased knowledge about management strategies
•Complies with management strategies
•Exhibits no complications
aspiration PNA
occurs when inhaled food, drink, vomit or saliva into the lungs. more likely if something disturbs your normal gag reflex, such as a brain injury or swallowing problem, or excessive use of alcholhol or drugs
risk factors for aspiration PNA and ss
age >65
chronic disease: CAD, COPD
smoking
weakened 0r suppression of immune system
ss:
coughing episodes with eating
increased fatigue
low grade fever
change in MS
imaging: CXR: infiltrate usually lower lobes RLL>LLL (can see as soon as 2 hours after aspiration
prevention of aspiration PNA
thickened liquids
making sure they go down esophagus
sit upright when eating
good oral hygiene
aspiration management
supportive care, airway protection, consider early antibiotics if bacterial infection suspected
bronchoscopy for large particulate aspiration
standard for removing forgien objects other blockages
aspiration prevention
HOB elevated between 30-45 degrees
limit sedation
avoid stimulation of gag reflex
swallow eval
soft diet, small bites, no straws
critical care clinical practice to prevent tube feeding aspiration
•Before initiating tube feeding, confirm tip location.
•Tube feed patients: residuals Q4h, <150mL before next feeding.
•Avoid bolus Tube feeding
•Draw back 1-2 cc of fluid from tube and check ph.
•Ph of 5.5 =likely in the stomach (where it is more acidic)
•Ph of 6= likely respiratory tract or intestines and repeat x-ray.
pt education/PNA healing timeline
1 week - fever shhould begin to resolve
4 wekks - chest pain and sputum should decrease
6 weeks - cough and SOB decrease, if persists, concider further w/u and alternate diagnosis
3 mo - all ss should be resolved, may still have soem fatigue
6 months - back to normal
what is a lung abcess
pocket of pus in the lung surrounded by inflamed tissue
most are complication of bacterial pna
ss: vary from a mild productive cough to acute illness with foul sputum, leukocytosis, pleurisy, dyspnea, weakness, anorexia, and weight loss,
lung abcess assessment/physical exam
pleural friction rub/ crackles
test: chest XR, sputum culture, bronchoscopy, ct of chest
pleurisy
= inflammatiom of both layers of pleurae
lungs have two layers
visceral pleura – inner
parietal pleura – outer
key characteristic: pleuritic pain and its realtion to resp movement
friction rub can be heard with stethoscope
test: chest XR, sputum, thoracentesis
empyema
•: infected pleural fluid—pus, positive gram stain/culture, low pH, low glucose.
Tuberculosis
caused by a bacterium called Mycobacterium tuberculosis transmitted through aerosolized droplets.
20-40% wold population is effected
higher risk in disadvantages communities
primarily attacks lungs but may effect otehr areas (ei; kidney, spine, brain)
TB disease/active TB
with infection and symptoms
may occur 2-3 months or years after exposure
changes from latent to active due to immune compromise of chronic illness
infectios ss:
cough over 3 weeks
hemoptysis (coughing up blood )
wt loss
night sweats
weakness
fever
Latent TB
person expose to bacteria but immune system keeps under control
bacteria are encapsulated
NOT infetious
10-15% will develop active without treatment
length of treatment for TB
once a week treatment for 12 weeks
pleural effusion
fluid build up in the lungs
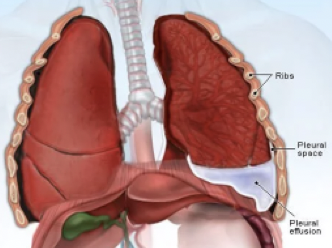
assessment of pleural effusion
inspection: anxious, in distress, trachea may deviate tawards inaffected side
palpation: decreased tactile fremitis and decreased expansion of effected side
percussion: dullness
auscultation: decreased/absent breath sounds or possible rub on affected side
diagnostic studies of pleural effusion
Chest CT gold standard
CXR
U/S
Diagnostic thoracentesis
Pleural biopsy
Bronchoscopy
Malignancy workup
treat: fluid must be tapped
management of empyema
•: antibiotics and surgical drainage (small-bore chest tube +/- fibrinolytics; VATS if loculated)
acute respiratory failure
type 1: hypoxemic —> oxygenation failure
type 2: hypercapnia —> ventilatory failure
type 1 of acute respiratory failure
oxyegenation failure —> impaired oxygen diffusion at the alveolar capilary membrane
breathing air with reduced oxygen content
abnormal hemoglobin
thickening or desteiction of alveolar capilar membrane
PNA, ARDS, HF, Pulmonary embolism
type 2 of acute respiratory failure
ventilatory failure —> inability to blow off CO2
increases resistance to breathing (asthma)
reduced breathing effort due to resp muscle weakness
increased area of the lung that is not available for gas exchange (COPD, obesity hypoventilation syndrome)
clinical manifestions of acute respiratory failure
rapid deterioration to hypoxemia, hypercapnia, and resp acidosis
impaired ventilation of perfused mechanisms
CM: use of accessory muscles and decreased breath sounds
dyspnea is the hallmark of acute respiratory failure
early signs of oxygen failure in acute respiratory failure ***
dyspnea/tachycpnea - use of accessory muscles
restlessness
tachycardia/HTN/diaphoresis
changes LOC/mentation restlessness/agitation
HA and fatigue
late signs of oxygen failure in acute resp failure ***
confusion, lethergy
tachypnea - resp arrest
tachycardia - dysrhythmias- bradycardia
central cyanosis (bodies core turns blue ie lips, tongue, mucous membrane)
cool, clammy skin
nursing management of acute resp failure
identify and treat underlying cause
intonation, mechanical vent
nutrition- enteral feedings preffered
reduce anxiety
provide pt a form of communication
prevent complications (turning, ROM, mouth care, skin care)
do imaging and labs - see what electrolytes are
when to intubate:
worsening hypoxemia despite O2
resp fatigue
hypercapnia with acidosis *
altered mental status
prepare for rapid sequence intubation and post intunation strategy
what is ARDS
= a severe form of Acute Resp Failure
Alveolar capillary injury (not caused by cardiac issue)
Damage to the endothelial lining of the alveolar capillary membrane, which increases its permeability
Plasma and proteins leak from capillaries into the interstitial spaces and alveoli
Diffuse alveolar damage
Reduces lung compliance, volume, and normal gas exchange
Rapidly progressive hypoxemia
Noncardiogenic pulmonary edema
(fluid accumulates in the lungs but not caused by a problem with the heart)
significance of ARDS
mortality rate 27-50% unless accurately diagnosed it can prove fatal in the first 48 hours
(covid resemebles )
causes: COPD, PNA, neuromusclar failure, drug OD
etiolofy of ARDS
common causes* =
Aspiration of Gastric Contents*
Pneumonia (COVID) (Bacterial/Viral)*
Inhalation Injury
Oxygen Toxicity
Pulmonary Contusion
Chest Trauma
Fat Emboli
Near Drowning
Shock of Any Etiology *
Sepsis *
Massive Trauma
Disseminated Intravascular Coagulation
Massive Transfusion
Drug Overdose
Acute Hemorrhagic Pancreatitis
Burns
Anaphylaxis
CM/physical assessmemt of ARDS
Hypoxia that doesnt improve with O2!!**
tachypnea
increasing dyspnea.. hyperventilation.. resp distress
initially no adventotious breath sounds
tachycardia
hypertension
restlessness, anxiety
chest XR
chest x-ray appears to resemble pulmonary edema
BNP to distinguish pulmonar edema from ARDS cersis from heart failure
BNP higher in pulmonary edema due to HF
visible bilateral infilrates that quickly worsen
BNP
= brain natiritic peptide
hormone released from the heart when under stress in respinse to increased venticlar pressue and volume
high BNP = heart failure with pulomary edema (but NOT with ARDS)
medical management of ARDS
Intubation, mechanical ventilation with Positive End Expiratory Pressure (PEEP) to keep alveoli open (normally alveoli deflate with breathing out, this keeps them open during expiration to increase gas exchange ie: o2 in and Co2 out)
Treat hypovolemia to keep hemodynamically stable
Turn patient to Prone position
is best for oxygenation,
the weight of the heart, abdominal organs, and diaphragm is shifted away from the lungs,
allowing for better ventilation of the dorsal (back) lung regions that have collapsed d/t atelectasis.
Also Increases end-expiratory lung volume
Improves bronchial draining
Improves functional residual capacity
Improves gas exchange
Opens collapsed alveoli
frequent repositioning to safeguard integumentary system. Improves oxygenation
Nutritional support, enteral feedings preferred
Reduce anxiety, sedation, paralysis
Supportive care
halmark sign of ARDS
hypoxia that doesnt improve with O2
non-invasive positive pressure ventilation
ventilatory support without intubation
positive pressure keeps airways & alvioli
CPAP: pushes O2 in using single continuous pressure
improves oxygenation (does not remove co2)
used for sleeo apnea
BIPAP: helps move air in and out
high pressure on inhalation, lower pressure on exhaltion
helps remove CO2
used for COPD
critical lab values for mechanical ventilation
PaO2 <55 mm HG (norm values 80-100 mmHg)
PaCO2 >50 MM HG (norm values 35-45 mmHg)
Vital capacity <10ml/kg (norm 50 ml/kg)
(reduced vital capacity= weakness of respiratory and diaphragm muscles to have enough force to draw air in and out of lungs)
Negative inspiratory force (NIF) < - 25 cm H2O (norm NIF is - 60 to -100 cm H20)
The NIF= measures the strength of respiratory muscles and diaphragm, by quantifying the maximum negative pressure generated during inhalation effort
FEV <10ml/KG ( Forced Expiratory Volume)
ss that indicate a need for mechanical ventilation
•Typically…Dyspnea(SOB),Tachypnea, LOC changes
•Apnea or bradypnea
•Respiratory Failure /Compromised airway
•Emergency
•Respiratory distress with confusion
•Increased work of breathing when other interventions have failed.
•Confusion with the need to protect the airway.
•Shock
•Control patient’s respirations during Surgery or Procedures
medications for patients of mechanical ventilation
Narcotics/ Opioids
Pain Management
Benzos
Sedation, amnesia, muscle relaxants
Paralytics
Paralytics/Versed paralyze respiratory muscles, Patient MUST HAVE a Sedative
Corticosteroids
Reduce inflammation, suppress immune system, studies are +/– for use of steroids
Inotropes
Balance carefully: Nitrates/ Pulmonary HTN, and Dopamine will maintain BP
Bronchodilators
Albuterol, DuoNeb treatments allow smooth airways to relax.
Diuretics
Help to increase renal excretion, decrease pulmonary edema & reduce preload.
Dobutamine/Dopamine
for Hypotension
Nitroglycerine / Nitroprusside
For Pulmonary Hypertension
potential complications/things to look for when monitoring ventilator
vent problems:
volume/rate depending of pt condition/ARDS
oxygen is priority!
alteractions in cardiac finction
decrease in venous return
VS and fluid volume assessment
barotrauma/Pneumothorax
high airway pressure may cause alveoli to rupture
pulmonary infection
weaning from ventilator
process is dependant on spontaneous breathing
vent rate is gradually decreased until pt breathes on own without use of vent
pressure support is maintained during weaning
nursing management of ventilation patients
improving O2 and ventilation
positioning
least affected area of lung is most dependent position
semi recombent/elevate HOB
reposition every 2 hours
prevent desaturation
hyper oxygenate before suctioning
minimize acticity
secretion clearence
hydrate, humidifym neb treatment, mucolytics, chest PT, suction
prevent complications
hospital and ventilator aquired PNA
oral care: 12% chlorohexidine swabs and brush teeth
endotracheal intubation
•Passing an endotracheal tube through the nose or mouth into the trachea
•Protects airway, provides patent airway, access for mechanical ventilation
•Facilitates removal of secretions,
•Maintain cuff pressure between 20- and 25-mm Hg
•Intubation for no longer than 14 to 21 days (after will require a tracheostomy)
short term
tracheotomy
long term breathing support
surgical procedure where an opening is make into the tracheo
allow removal of secretions
reasons for it:
long term mechanical ventilation for weeks or longer
severe COPD, ICU stay, neuro disease
may have upper resp obstriction
benifits
more comfortable long term
decrease risk of vocal injury
easier suctining and airway care
high risk for aspiration - keep HOB elevated at >30%-45%
suctioning w/ trache
patient should NOT be routinely suctioned
invasive procedure: can cause infection (PNA), atelectasis, airway injury, hypoxia, dry membraines
pt are suctioned ONLY AS NEEDED basis if:
visable secretion in andotracheal tube
onset of resp distress
suspected aspiration of secretions
increase in airway pressure
adventitious vreath sounds
increase in resp rate/sustained coughing (normal RR = 12-22)
sudden decrease in O2 levels
responding to alarms/patient saftey
if cause of an alarm cannot be determoned, ventilate the pt manually until problem is corrected (with ambu bag)
oxygen is priority
check the pt 1st!!
potential complications for mechanical ventilation
shock:
resp failure
pleurisy: inflamation of the pleura (membrane around lungs)
pleural effusion: accumulation of excess fluid
empyema: accumulation of puss in pleural space
Pneumothorax
air in the pleural space
inspection: trachea is deciated towards unaffected side, anxious, holding chest
palpiation decrease in tactile fremitis and decrease in thoracic expansion of affected side
percussion: hyper resonance over chest wall (loud percussion)
auscultation: decreased or absent breath sounds of affected side
need chest XR and CT scan
treat: chest tube, O2
pulmonary embolism
Occurs when a blood clot gets wedged into an artery in the lungs. Most caused by blood clots from the deep veins in the legs causes a Deep Vein Thrombosis (DVT) that gets released and travels to lungs. Multiple clots may be involved.
SS of puomonary embolism
tachycardia, S3 or S4 gallop
dyspnea
rales
pleuritic chest pain
cough
hemoptysis
diaphoresis
leg pain
cyanosis
fever
anxiety/fear
syncope
asymmetric pitting lower extremity edema
prominent superficial collateral vessels
tenderness to palpation along the deep venous system
+ Homans’ sign
(calf pain with dorsiflexion of foot with knee straight)
(poor predictive value; reliability only 50%)
diagnostic testing for PE
D-dimer
indicated in there is a clot
fibrin * from clot shows up
ECG
CXR
ABG
spiral ct
pulmonary arteriogram
risk factors for PE
venous stasis
sedentary lifestyle
prolonged immobilization
periods of sitting/traveking
vericose veins
hypercoagubility
injury
tumor
increased platelet count
venous enothelial disease
thrombophlebitis
vascular disease
forgien bodies
HF
Postoperative/postpartum
prevention and treatment of PE
in hospital
active leg expercises
mobility with PT
early ambulation
anticoagulant therapy
compression devices
treatment
measures to improve resp and vascular stasus
provide O2
ECG monitoring
IV access
anticoagulation therapy
heparin/warfarin
thrombilytic therapy
streptokinase alteplase
sugical
embolectomy
nursing managemnt for PE
encourage ambulation
passive leg exercise
moniter thrombolytic therapy
VS q2 hours
PTT q 4 hours (make sure we are not thinning blood too much)
O2 therapy
cough and deep breathing
IS
pulse ox
sarcoidosis - pleural involvement
Sarcoidosis is an immune disorder meaning the immune system is dysfunctional and forms granulomas.
What is a granuloma?
A granuloma is a small clump of immune cells that forms when the body tries to wall off something it sees as foreign but can’t get rid of. Granulomas are made up of macrophages and other immune cells.
Think of it as the body building a fence around a problem
• Sarcoidosis is an interstitial lung disease that is inflammatory multisystem, granulomatous
why are granulomas a problem?
take up space in the lungs, make lung tissue stiff, restricting lung expansion and impair gas exchange
cause: unknown
occurs between ages of 20-40
treatment of granulomas
no ss= no treatment
moderate to severe ss = corticosteroids
supress immune system
pulmonary arterial hypertension
= progressive disease characterized by high blood pressure in the pulmonary arteries, leading to symptoms like shortness of breath, fatigue, and chest pain.
pulmonary artery mean pressure > 25 mmHg
normal = 8-20
idopathic or secondary to existing cardiac or pulmonary conditions like COPD
CM and diagnostic testing of Pulmonary Arterial HTN
CM:
dyspnea
substernal chest pain
weakness, fatigue, syncope, and signs of right heart failure
Diagnostic tests
chest XR
pulmonary function test
ECG and echocardiogram
cardiac catheterization with measurement of right heart pressure
management of pulmonary HTN
supplemental O2 with activity
central venous access for prostanoids: active lipid mediators that regulate inflammatory respinse
meds:
calcium channel blockers
Phosphodiesterase inhibitors: medications that cause blood vessels to relax and widen, improving circulation and lowering blood pressure.
Prostanoids ( prostaglandins mediate inflammation).
Cor Pulmonale
restriction of pulmonary arteries leading to pulmoary HTN —> inceased resistance to right ventricle
= enlargement of right ventricle leads to increased resistance and right sided HF
does not eject as much blood bc the muscle is larger and not enough blood can get in
types of thoracic surgery
pneumonactomy
lobectomy
segmental resection
wedge resection
lung colume reduction - end stage emphysema
post op nursing care following thoracic surgery
positioning
elecate HOB 30-45 desgrees
change position from back to side frequently
self care
arm and shoulder exercises
pain relief pedalities
acticity - rest balce
avoid bronchial irritats
follow up care
smoke cessation
nursing care wth chest tube
•Pain Control**
•Narcotics/ Local for tube placement
•NSAIDS for tube duration
•Anxiety treatments prn
•Nurses are responsible for keeping tubing connections patent and ensuring they are not compressed or kinked - position your patient well
•Ensure the drainage system is always below the level of the client’s chest to use gravity to drain air and fluid from the pleural space.
•Monitor the levels of fluid in water seal and suction control chambers – sterile water may need to be added prn
•Vital signs, pulmonary assessment, insertion site evaluation
•Daily x-rays
•Q Shift (or sooner) measurements of drainage
•Document the quality of drainage – sanguineous, serosanguinous, yellow, clear or opaque
encourage IS and ROM with arms
chest tube complications
bubbling in water seal chamber of chest tube system —> indicates air leak
subQ emphysema or crepitis —> leakage of air into the sub Q tissue
chest tube emergency care
if drainage system spills over —> encoruage p to take a few deep breaths with forceful exhalations and coughs
sett up a new system and change pt over
should the drainage system break, submerg the distal end of tubing into a bottle of sterile water (kept at bedside)
complications of chest tubes
infection at insertion site
PNA from poor pulmonary toilet
frozen shoulder
systemic hypotesion with rapid high volume drainage
chest tube removal
Suction usually discontinued, patient on water seal for 6-24 hours prior to removal
Chest x-ray prior
Lungs re-expanded; pleural drainage ceased
Pre-medicate*
Pre-educate about upcoming events
Sutures holding tube in place are cut, as patient exhales a deep breath the tube is removed.
Occlusive dressing placed over the wound
Pleura self-seals usually – wound heals in several days – offer NSAIDS prn
blunt chest trauma
•involves forceful impact from dull objects (like car crashes, falls) causing compression/shearing, leading to bruises, fractures, internal damage without skin break
penetrating chest trauma
pierces the skin with sharp objects (knives, bullets) creating open wounds, causing direct tissue damage, infection risk, and potential organ perforation, with mechanisms differing in energy transfer and injury pattern.
pulmonary contusion and rib fractires
•Contusion causes alveolar hemorrhage/edema; rib fractures cause pain and hypoventilation leading to atelectasis.
•Manage with pain control, pulmonary hygiene, and respiratory support as needed.
Flail Chest
multiple contiguous rib fractures causeing paradoxical chest wall motion - creating a loose, disconnected piece of bone that moves opposite way you breathe
ribs are floating
paradoxical movement - making it hard to breathe
inhale = chest moves out
exhale = chest moves in
high risk for resp failure
open pneumothorax
penetrating thoracic injury that causes air to enter from the outside in
closed pneumothorax
air enters the pleura space without an outside wound
causes:
traumatic impact (MVA) or
spontaneous rupture of lung tissue
primary spontaneous: without history of lung diease
secondary: with history of lung disease
tension pneumothorax
complication of open and closed
worsening pneumothorax where air connot escape
increaing intrathoracic pressure
pressure starts to displace heart, good lung, and trachea
—> tracheal deviation*
emergceny situation
diagnosis & CXR findings
absent lung parkings, visceral pleural line of CXR, ultrasounds shows “lung point” (location of chest wall)
ct more sensitive for small pneumothorax
ABG
decrease in PaO2
increase in PaCO2
hemothorax
blood in pleural space collapsing ling - trauma or post op