CNS- Dopaminergic neurotransmission
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
44 Terms
what is the synthesis of dopaminergic neurotransmission?
Tyrosine to L-DOPA→ tyrosine hydroxylase (TH)
• L-DOPA to DA→ aromatic L-amino acid decarboxylase (AADC)
• Vesicular monoamine transporter (VMAT)
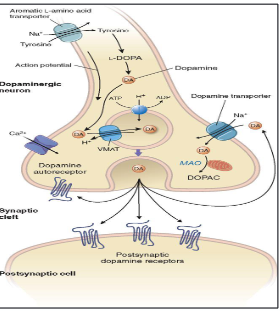
what is the metabolic cycle?
• Dopamine transporter (DAT)→ remove DA form the synaptic cleft
• Monoamine oxidase (MAO) or catechol-O-methyltransferase (COMT)→ DA degradation
what is the nigrostriatal pathway?
Pars compacta of the substantia nigra to striatum
• Stimulation of voluntary movement
• PD
what is the mesocorticolimbic pathway?
• Ventral tegmental area to cerebral cortex, the nucleus accumbens, and other
limbic structures
• Motivation, regulation of affect and reward
• Schizophrenia
what is the tubero-infundibular pathway?
• Arcuate and paraventricular nuclei of the hypothalamus to the median part
of the hypothalamus
• Inhibits the release of prolactin
what are the symptoms of parkinsons disease?
Ataxia – rigidity, bradykinesia
– Resting tremor
– Cognitive impairment (memory, attention, loss of inhibition.)
– Postural instability
– Eventually dementia
• Second most common neurodegenerative disease
Incurable, progressive, not (directly) lethal; life expectancy 10-15 years
what is the physiology of the nigrostriatal pathway?
Striatum - caudate nucleus, putamen and nucleus accumbens
Globus Pallidus - internal (GPi) and external (GPe)
Subthalamic nucleus (STN)
Substantia nigra
what is the direct pathway in the striatum regulate movement?
Inhibition GPi and the SNr by GABAergic neurons
Uninhibited GPe (D2 receptors)→ higher inhibition in GPi and the SNr + inhibition of STN
STN→ don’t excite GPi and the SNr
Inhibition GPi and the SNr → don’t inhibit thalamus→ thalamic neurons become disinhibited→ cortex excitation → movement
what is the indriect pathway in the striatum regulate movement?
Inhibition GPe
Prevent inhibition STN, GPi and SNr
STN→ excites GPi and the SNr
Excitation GPi and the SNr → inhibit thalamus→ thalamic neurons become inhibited→ cortex excitation reduced → suppress unwanted movements movement
what is the pathophysiology of PD?
Loss of dopaminergic neurones of the substantia nigra projecting to the striatum.
– PD onset after ~20-40% dopamine loss
– core motor features of the disease
alpha-synuclein accumulation→ Lewy bodies
what are the causes of PD?
Microbiome–gut–brain axis→ inflammatory gut environment promote aggregation of alpha- synuclein in the ENS
– PD genes→ PRKN, PINK1, SNCA and LRRK2
– Excitotoxic damage (oxidative stress, mitochondrial dysfunction)
– Infection
what is the pharmacology of PD?
PD is irreversible and incurable.
Treatment is management of symptoms
Pharmacological treatment
– DA precursors
– DA receptor agonists
– inhibitors of DA degradation
Non-pharmacological
– Deep brain stimulation (DBS) (Lesion?!)
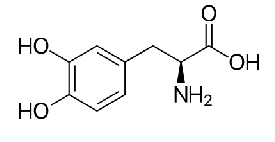
what is L-DOPA?
Dopamine does not cross the blood brain barrier
However, its metabolic precursor, L-DOPA (a.k.a levodopa), does
Converted to DA by AADC
Oral administration
– Risk of conversion in periphery→ ↓ the amount of levodopa BBB (1-3%)
– ↑ the peripheral adverse effects
Coadministration Carbidopa
– inhibitor of AADC in periphery (don’t cross BBB)
what are the adverse effects of L-DOPA/ Carbidopa?
Involuntary movements (dyskinesia, after 2 years treatment)
On-off effects: rapid switching from symptomatic to asymptomatic state; more likely in later years L-DOPA treatment
– fluctuations in plasma concentration of levodopa
– co-administration of COMT inhibitors such as entacapone
Acute side effects
– confusion - schizophrenia-like effects
– Nausea
– hypotension
what are older DA agonists?
Bromocriptine (D2), pergolide (D1 and D2), cabergoline
– Caution of cardiac & pulmonary fibrosis
what are newer DA agonists?
– Pramipexole, Ropinirole, Rotigotine (all D3>D2)
– Advantage of no “on-off” effect as observed with L-DOPA.
– May also be co-administered with L-DOPA (especially towards end of L-DOPA effectiveness)
what are side effects of dopamine receptor agonists?
– Impulse control disorders
– Hypotension
– Nausea, drowsiness, dizziness
– hallucinations
Also used for treatment of restless legs syndrome
what is MAO-B?
Usually as an adjuvant drug
• Rasagiline and Selegiline
– improve motor function when used alone
– Increase the effectiveness of levodopa
MAOBIs neuroprotective – may slow disease progression?
Side effects: Nausea & abdominal pain, hyper / hypotension, headache, dry mouth, hallucinations, vertigo
– Selegiline: amphetamine-like effects (toxic metabolite)
– Rasagiline: joint pain
what is COMT?
Entacapone ( peripheral specific), tolcapone (periphery & CNS)
Counteract “end-of-dose” fluctuations in plasma L-DOPA concentrations;
Allows to reduce L-DOPA dose (~30%)
Side effects: fatal hepatic toxicity (tolcapone)
What is amantadine?
Increases release and blocks reuptake of DA
treat levodopa-induced dyskinesias that develop late in the course of the disease
Weak NMDAR antagonist?
what are antimuscarinics?
– Several available to reduce tremor in Parkinson’s
– Trihexphenidyl, benztropine
– Occasionally co-prescribed
what are purinergics?
– Adenosine A2A receptors associated with D2 receptors and suppress their function
– A2A receptor antagonists in trials
what is schizophrenia?
Chronic, often hereditary; can severely disrupt life
Strong evidence of biological disorder
Often associated with other mental disorders: anxiety, guilt, depression, high risk of suicide.
Frequently associated with drug abuse
what are positive delusions of schizophrenia?
Hallucinations (often “hearing voices”)
– Thought disorder (e.g. rambling speech)
– Abnormal and disorganised behaviour
– Catatonia (immobility, purposeless movement)
what are negative symptoms of schziophrenia?
– Low emotional responses
– Inability to experience pleasure
– Reluctance to perform tasks
what are cognitive deficits of schizophrenia?
– Poor memory
– low attention span
what are the causes of schizophrenia?
About 10% heritable; if one monozygotic twin has schizophrenia, about 50% chance the other does.
Multiple genes implicated (~100?)
– synaptic connectivity and glutamatergic neurotransmission
– C4A, neuregulin , dysbindin , DISC-1 , TCF4 and NOTCH4
Environmental factors
– Birth complications
– Maternal virus infection
– Drug use (e.g. cannabis, cocaine)
what is the glutamate hypothesis of schizophrenia?
NMDA receptor antagonists can cause schizophrenia-like symptoms
Disrupted vesicle transporter proteins in glutamatergic synapses (VGLUT1)
Transgenic mice with reduced NMDA receptor expression show schizophrenia-like
symptoms
what is the inflammation hypothesis?
High level of inflammatory cytokines in schizophrenics
Benefit of anti-inflammatories in early schizophrenia; antipsychotics also anti- inflammatory
Vulnerability – stress – inflammation model
Immune-based alteration to neurotransmitter signalling (Glu, DA, NA, etc.)
what is the pharmacology of schizophrenia?
Antipsychotics
• “First generation” or “typical” antipsychotics
• “Second generation” or “atypical” antipsychotics
• No clear definition between typical and atypical, but relates to:
– Receptor profile
– Extrapyramidal side effects
– Efficacy in treatment-resistant patients
– Efficacy against negative symptoms
what are typical antipsychotics?
Block dopaminergic neurotransmission on D2 receptors – therapeutic efficacy and extrapyramidal adverse effects
what are the different structural classes of typical antipsychotics?
– Phenothiazine class (e.g. chlorpromazine)
– Butyrophenone class (e.g. haloperidol)
– Thioxanthene class (e.g. zuclopenthixol)
– Diphenylbutylpiperidone class – mostly obsolete
– Dibenzoxazepine class – mostly obsolete
what is the mechanism of action of typical antipsychotics?
D2R antagonism of mesolimbic pathway
• ↑ Effective positive symptoms→ hyperactivity of the mesolimbic system
• ↓ Effective negative symptoms→ hypoactivity of mesocortical
what are the extrapyramidal effects of typical antipsychotics?
Involuntary movements, muscle spasms, Parkinson’s-like symptoms
Antagonism of D2 receptors→ disinhibit the indirect pathway
Can be ameliorated by anticholinergics (e.g. procyclidine) and 5-HT1A receptor antagonists (e.g. buspirone)
what are the endocrine effects of typical antispsycotics?
– ↑ prolactin
– Pituitary gland
– breast swelling, pain, lactation (also affects males)
what are the off-target side effects of typical antipsychotics?
Sedation (Histamine H1 receptors)
– Weight gain (H1, 5-HT, mAChR)
– Hypotension (alpha-adrenoreceptors)
– Dry mouth, blkurred vision (mAChR)
– Sexual dysfunction (pretty much all receptors)
what are atypical antipsychotics?
More effective at treating the negative symptoms
Milder extrapyramidal symptoms
Higher incidence of other adverse effects
what are examples of atypical antipsychotics?
Clozapine highly effective, serious side effect of agranulocytosis; now rarely use
Risperidone: causes worse EPS than most 2nd gen.
Aripiprazole unusual as a D2/3 partial agonist, not antagonist
Quetiapine and olanzapine most commonly used; olanzapine more effective but worse side effects
what is the 5-HT₂ hypothesis of atypical antipsychotics?
Newer antipsychotics are better antagonists at 5-HT2ARs than DARs
5-HT2A overactivity: association with PLA2; associated depletion of membrane phospholipids
what is the D2R rapid dissociation hypothesis?
Atypical antipsychotics bind D2 receptors more transiently than typical antipsychotics
what are antipsychotic side effects?
Extrapyramidal effects 1st gen >> 2nd gen
• Parkinsonian dyskinesias 1st gen >> 2nd gen
• Sedation
• Hypotension
• Weight gain 2nd gen > 1st gen
• Diabetes risk 2nd gen > 1st gen
• Sexual dysfunction 2nd gen > 1st gen
what are the other uses of antipsychotic drugs?
bipolar disorder, mania and depression
• psychomotor agitation and severe anxiety
• psychosis associated with Parkinson's disease
• restlessness and pain in palliative care
• nausea and vomiting
• motor tics and intractable hiccup
• antisocial sexual behaviour
• involuntary movements caused by Huntington's disease
what is the future development of antipsychotic drugs?
mGluR₂ and mGluR₃
– Positive symptoms
– ↓ Glu release by receptor activation
– Compensatory NMDAR up-regulation
Agonist mGluR₅
– Positive, negative and cognitive symptoms
– Activation enhances NMDAR function
Inhibitors of phosphodiesterase (PDE10), α 7 nicotinic receptor agonists, histamine H 3 antagonists and 5-HT 6 antagonists