CVM - Lecture 10: Ischaemic Heart Disease
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
Inadequate blood supply for metabolic demand (O2 requirement)
What is ischaemia?
Low levels of oxygen in the blood
What is hypoxaemia?
They are sometimes used exchangably, as 90% of IHD is due to CAD, but they are not the same by definition
Are Coronary artery disease and ischaemic heart disease the same thing?
A disease due to the obstruction of coronary arteries. This is mostly due to atherosclerosis, but also sometimes due to variant angina: a vasospasm-induced coronary artery blockage
What is coronary artery disease?
Angina pectoris
What is the most common symptom during myocardial ischaemia?
40%
What percentage of total deaths in Australia is due to cardiovascular disease?
25%
What percentage of total deaths in Australia is due to coronary artery disease?
ST segment deviation, also T wave inversion may occur. Later prominent Q waves may occur (greater than 25% of QRS height and width of more than 0.04s)
Which segment or interval of the normal ECG changes most characteristically in cardiac ischaemia?
1. left coronary artery
2. left circumflex artery
3. left anterior descending artery/anterior intraventricular artery
4. right coronary artery
5. right marginal artery
6. posterior intraventricular artery
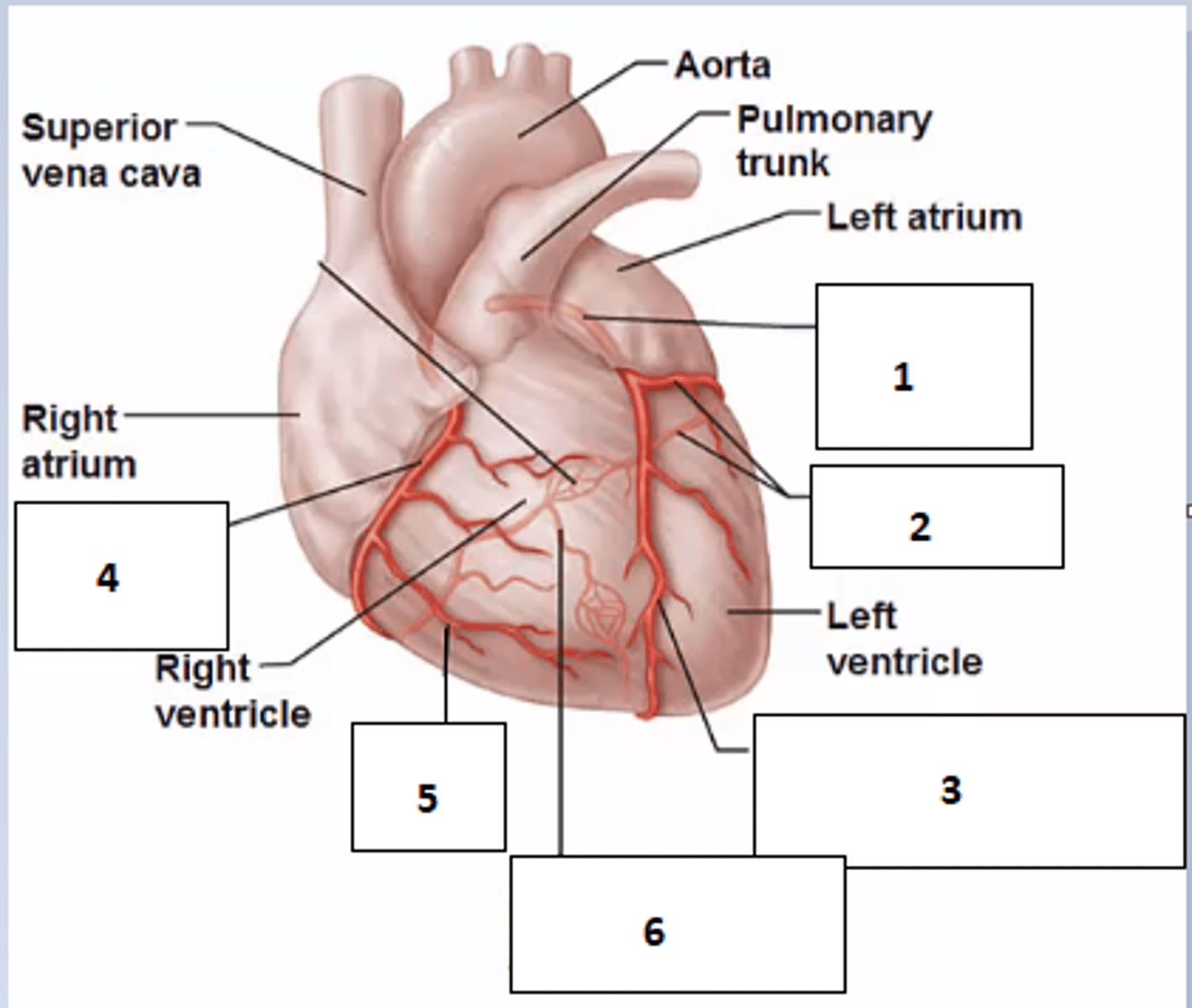
Lateral wall of left ventricle and left atrium
Which are does the Left circumflex branch supply?
Anterior wall of LV and anterior 2/3 of intraventricular septum
Which are does the LAD supply?
Inferior and posterior walls of LV, posterior 1/3 of intraventricular septum, right ventricle, right atrium including SA and AV node
Which are does the right coronary artery supply?
Blood flow is mostly during diastole. During systole, perforating branches of coronary vessels get compressed by cardiac muscle and the aortic valves cover their aperture. Perfusion depends on aortic diastolic pressure. 70-80% of O2 is absorbed from blood, leaving little leeway for a drop in O2, due to very high metabolic demand.
Describe coronary perfusion (mechanism, oxygen demand, timing)
up to 25%
How much of supplied O2 is extracted by skeletal muscle at rest?
Vasodilation with increased workload due to metabolic end-product build-up. Endothelial cells play an important role, including secretion of nitric oxide
How does coronary autoregulation work?
- preload
- afterload
- heart rate
- contractility
What are the major determinants of myocardial O2 demand?
- oxygen content of blood
- rate of coronary blood flow (PVR, coronary perfusion pressure, coronary vascular resistance eg. plaque, and duration of diastole)
What are the major determinants of myocardial O2 supply?
- coronary blood flow resistance due to obstruction such as plaque
- decreased coronary perfusion eg hypotension
- low O2 content in blood eg chronic bronchitis
- increased O2 demand eg cocaine
Give 4 causes of cardiac ischaemia
Low O2 -> less ATP -> decreased contractility and relaxation speed -> reduced cardiac output
How does mechanical activity of the heart change in ischaemia?
- Low O2 -> increased lacatate
- Low blood flow -> low clearance of metabolic end products: lactate, adenosine, serotonin -> stimulate pain nerve endings
How does biochemical environment of the heart change and produce pain in ischaemia?
- Less O2 -> less ATP
- Less Na+/K+ ATPase, less Na+/Ca2+ and less Ca2+ATPase activity
- increased resting membrane potential/hyperpolarised state and calcium accumulation in cells
- increased excitability and faster repolarisation
- shorter AP duration
- resulting ST segment deviation and T wave changes
How does electrical activity of the heart change in ischaemia? (include channels) Effects on ECG?
20 minutes
How long can myocardial cells withstand ischaemia before cell death?
Necrotic tissue and fibrous tissue
What causes pathological Q waves?
- stable plaques can grow to occlude greater than 75% of the lumen and cause stable angina
- plaques may rupture and cause occlusion by a thrombus which causes an acute ischaemic event by partial or total occlusion
How can atherosclerotic plaques cause myocardial ischaemia? (stable vs unstable?)
- Chest pain radiating to inner arm and jaw
- burning, crushing, heavy, squeezing, or crushing feeling in chest
- usually diffuse, not localised
- not sharp or stabbing and doesn't wary with breathing
How is angina usually described?
- nausea
- sweating
- anxiety
- fatigue
- tachycardia
What are other common symptoms of myocardial ischaemia?
Sympathetic tone due to hypoxia, pain and potentially hypotension
What causes tachycardia and profuse sweating?
- chronic
- acute
What are the main 2 types of coronary syndrome?
- stable angina pectoris: caused by intermittent ischaemia. Usually due to chronic obstruction by a plaque which occludes 75% or more of the lumen
- usually brief 5-10 minutes
- often exercise induced and predictable by patient
- alleviated by rest and nitroglycerine
What is chronic coronary syndrome? (symptoms, pathology, duration, alleviation)
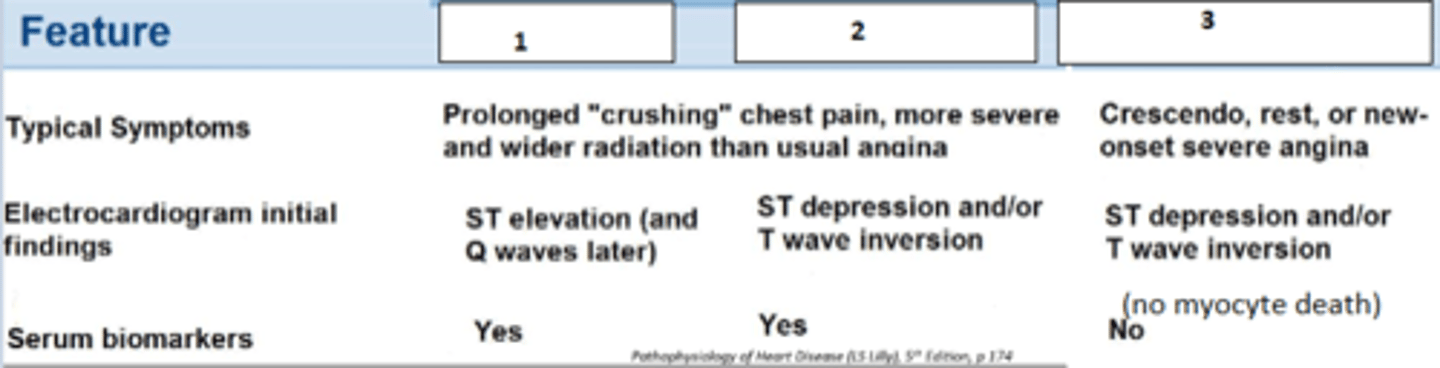
Sudden, unprecedented episode of severe and prolonged angina with 3 progressions:
- Unstable angina
- NSTEMI
- STEMI
Usually does not resolve with rest or nitroglycerine
Usually caused by plaque disruption and thrombus formation occluding 90% or greater of the coronary lumen
- medical emergency
What is acute coronary syndrome? (symptoms, pathology, duration)
- Acute coronary syndrome
- Usually due to plaque disruption and incomplete occlusion
- Pain severe and present at rest
- thrombus breaks down before 20 minutes
- NO cardiac myocytes die
Describe unstable angina
- <20 min
- 20-50 min
- 4h
- 6h
Fill the blanks (timing)
Release of myocardial enzymes from lysed cells
How does myocardial necrosis worsen damage?
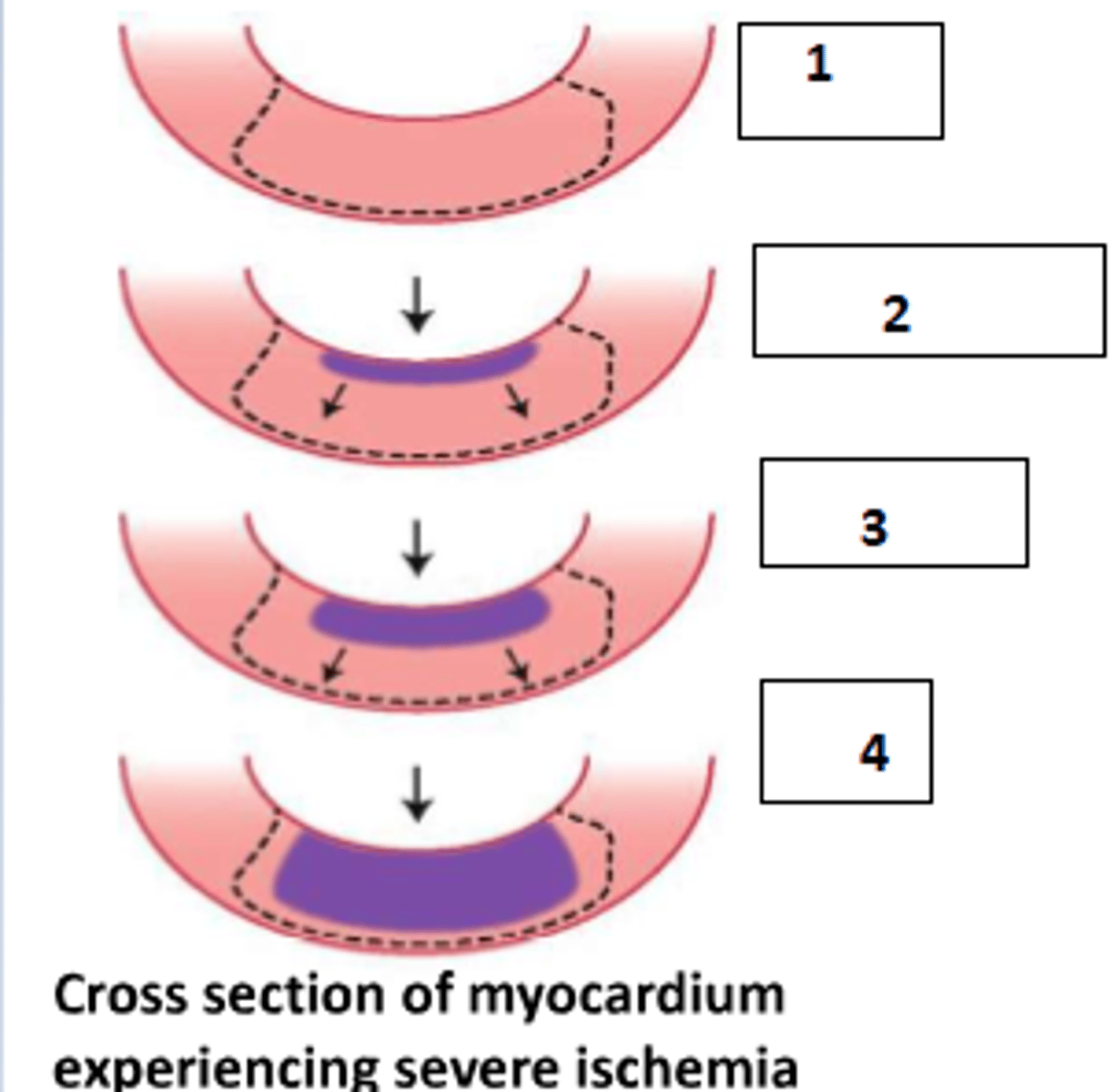
- Subendocardial region
- This is because this region is furthest from the coronary blood supply
Which area of the myocardium is most vulnerable to ischaemic injury and ususally dies first? Why?
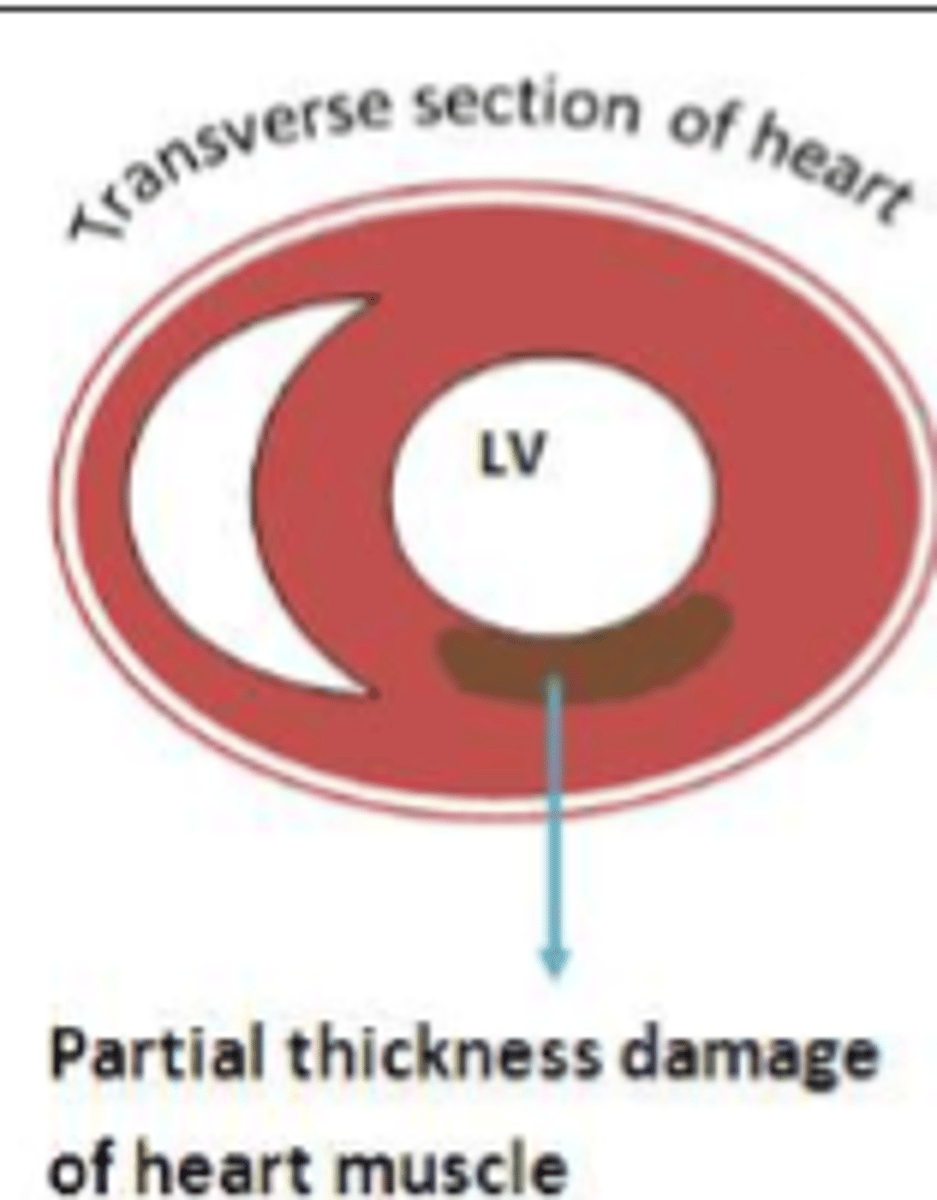
Subendocardial - NSTEMI (limited to inner third/half)
What kind of MI?
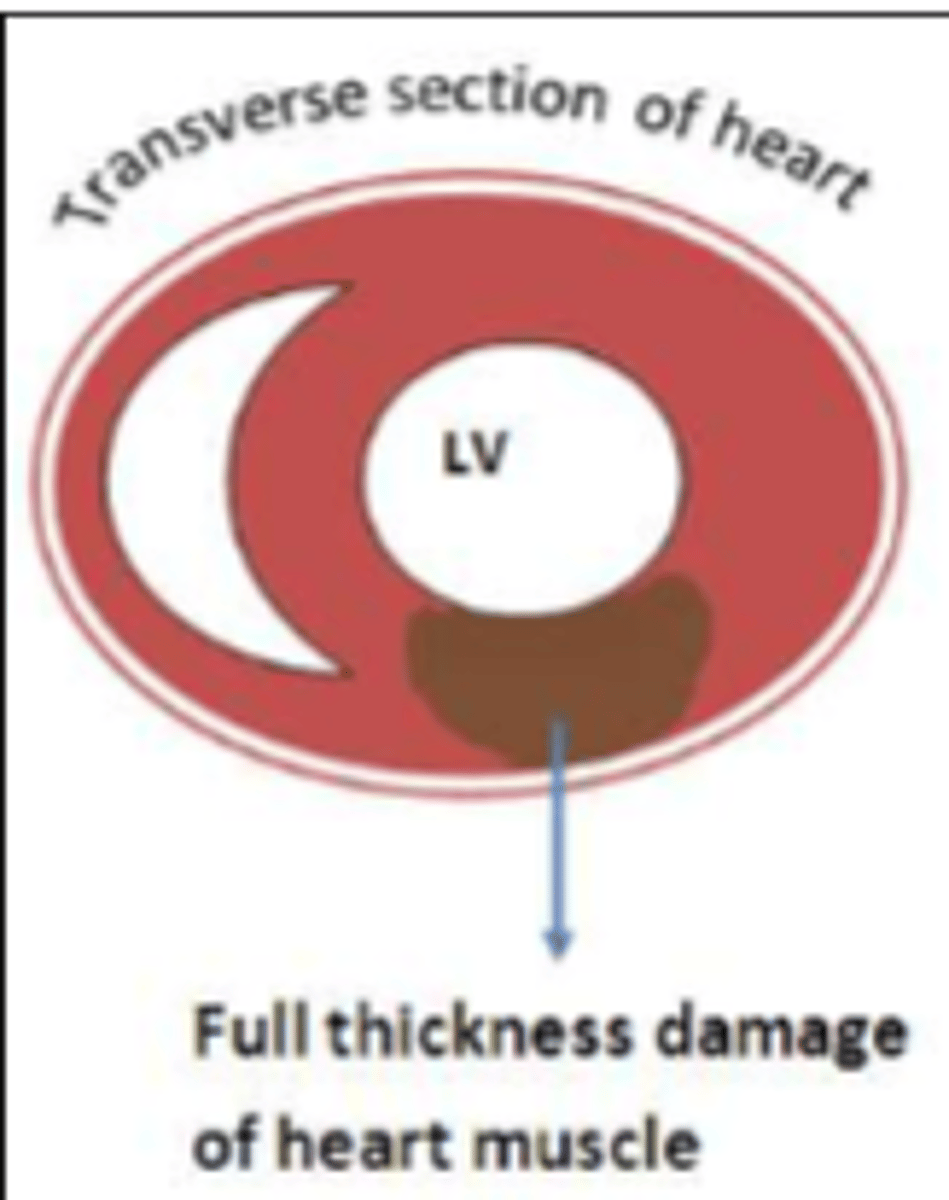
Transmural - STEMI (More than half of the wall affected)
What kind of MI?
Difference: presence of biomarkers (mainly cardiac troponin T&I) indicating cell death in NSTEMI but not in UA
In common: ST-segment depression, severe pain>20minutes, similar other symptoms of angina
What is the diagnostic difference between UA and NSTEMI? What presenting features are in common>
- STEMI
- NSTEMI
- Unstable angina (UA)
Fill the blanks
Previous/old myocardial infarction
An otherwise normal ECG with prominent Q-waves indicates what?
Cardiac troponin T & I (cTNT + cTNI)
What is biomarker of choice for MI?
appears at 3-4 hours, lasts for about 2 weeks
When does troponin start to appear at measurable levels in blood after MI? How long does it remain?
Since levels remain elevated for 2 weeks, it is difficult to distinguish when another MI has occured. Here CK-MB is useful, as it has a shorter half-life in the blood (~72 hours)
What is the main drawback of using troponin? What is the alternative?
- cardiogenic shock
- rupture of myocardial wall
- arrhythmias
- pericarditis
- formation of thromboembolism
- rupture of papillary muscle
- ventricular aneurysm
- congestive heart failure
What are some of the complications of myocardial infarction? give 5
Decreasing cardiac oxygen demand by reduced preload and afterload: peripheral vasodilation -> decreased peripheral vascular resistance -> decreased pre- and afterload
Decreased cardiac oxygen demand by decreasing contractility and heart rate: negative chronotropic, dromotropic and inotropic by blocking effects of endogenous beta agonists/catecholamines
How do beta-blockers help to treat MI? Give two mechanisms
- O2 supplementation
- angioplasty
- fibrinolytic drugs (eg streptokinase, tissue plasminogen activator - tPA, urokinase - UK)
- bypass surgery
Name 3 treatments which aim to restore O2 supply to the heart