Session 10: The Incidence, Prognosis and Treatment of Malignant Tumours
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
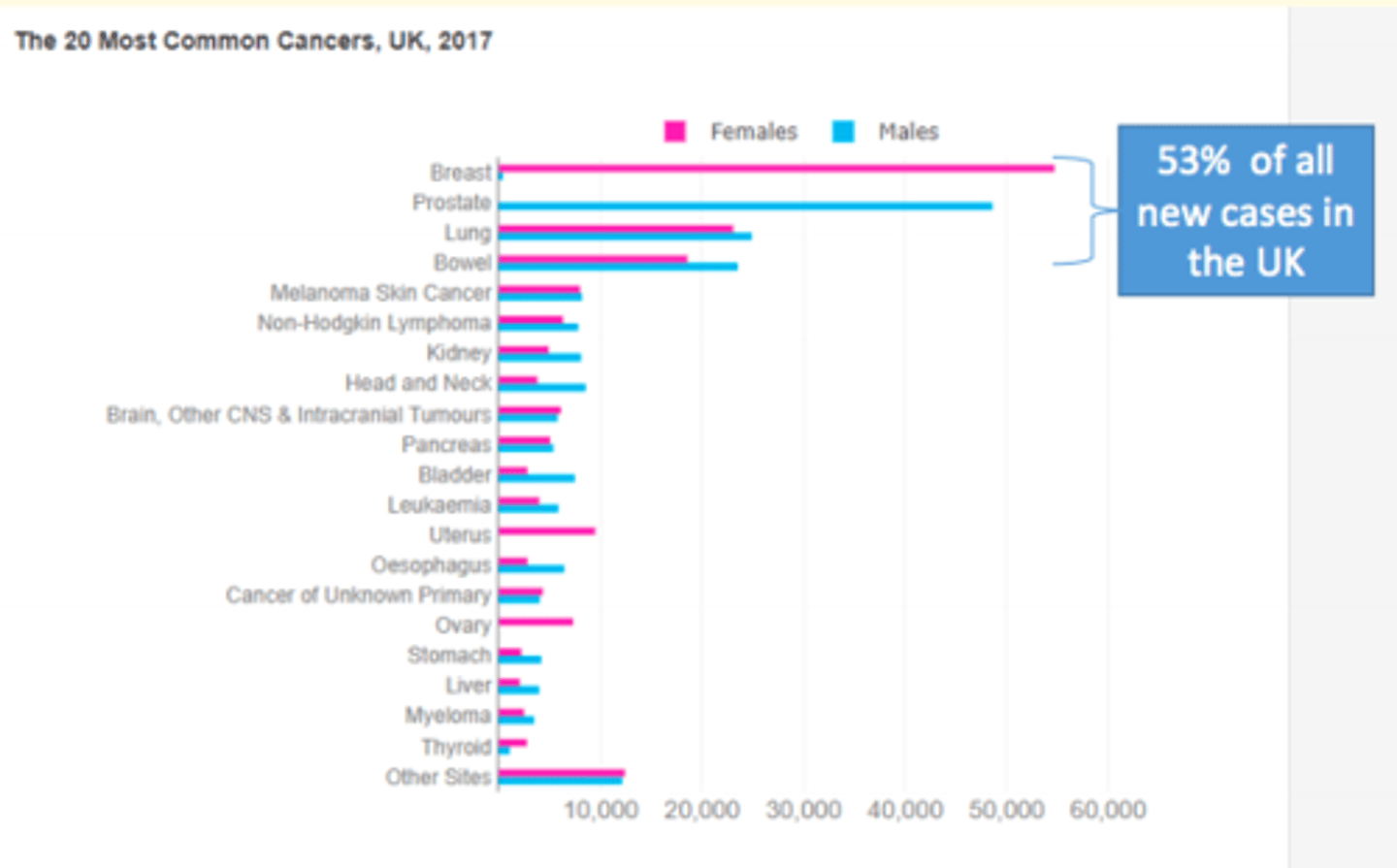
Incidence of new cancer diagnoses in the UK
In 2017, new diagnoses in England continued to increase from 303,135 in 2016 to 305,683 new cancer diagnosis.
Changes in the rate of people dying from cancer in England
The rate of people dying from cancer in England has decreased from 275.2 deaths per 100,000 in 2016 to 270.1 deaths per 100,000 in 2017.
Although the incidence of cancer is increasing, the cancer survival rate is at its ___ ever
Although the incidence of cancer is increasing, the cancer survival rate is at its highest ever
Significant improvements over the past 15 years
Most common cancers in the UK
Breast and prostate cancer
What is the gold standard for survival rate (cancer)
The percentage of people alive 5 years since their diagnosis is gold-standard
Clinical endpoints for survival data (cancer)
- Overall survival
- Progression free survival
- Event free survival
- Death
- Remission
- Clinical response
- Disease progression
Factors to consider include when predicting outcome of cancer
- Age and performance status
- Comorbidities
- Genetic mutations, including targetable demographics e.g., race/ethnicity
- Tumour site
- Tumour type
- Grade (differentiation)
- Tumour stage
- Availability of effective treatment
- Socioeconomic factors
- Economic and healthcare considerations
- Drug availability/licensing
- Clinical trials - active & accessibility
What type of prognostic indicators can be found in a cancer report
Grading
Staging
Margin status
Hormonal or gene status (as in breast cancers)
Why are the prognostic indicators in a cancer report necessary?
Valuable information to the patient and clinician
Helps to guide treatment
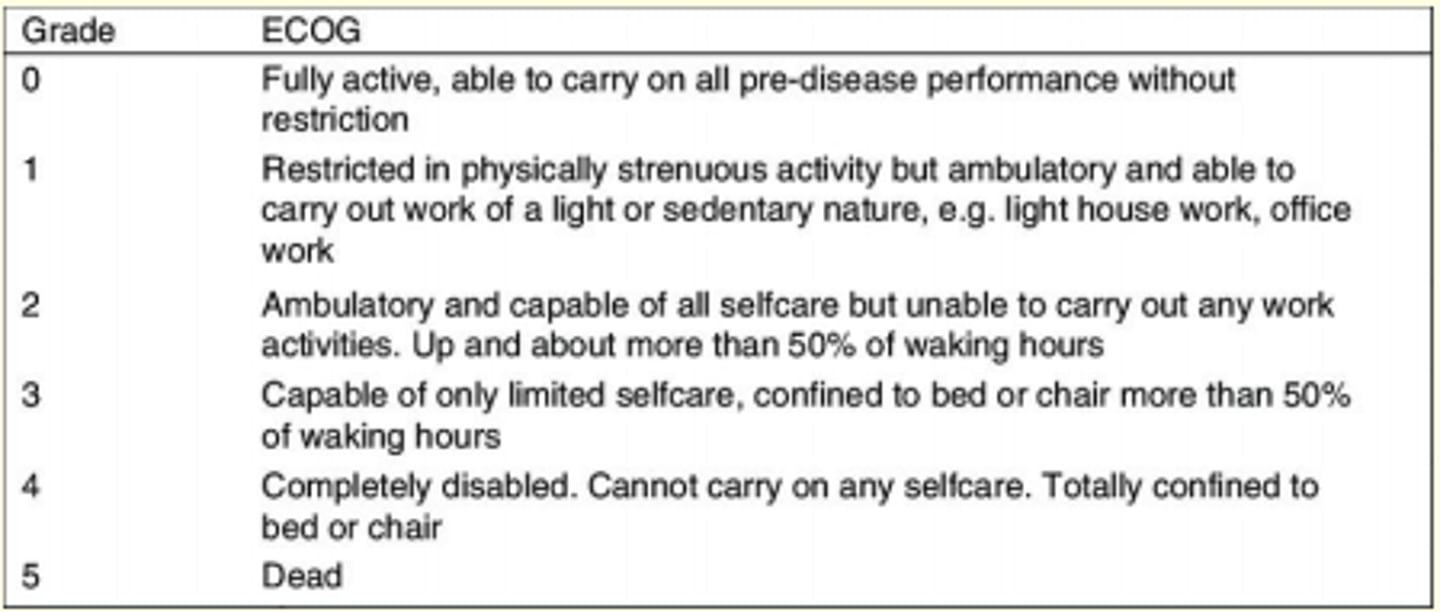
ECOG performance scale
0 (fully active) - 5 (dead)
What is a prognosis
Likely course of a disease or diagosis
Biopsy
Small amount of material used to give primary diagnosis.
A preliminary grading of the tumour is also given at this stage.
Resection of specimen
Large tissue which is resected surgically with curative intent.
The tumour extent & assessment of metastasis in the tissue provided helps in staging the tumour (including lymphatic spread)
Grading vs staging
Grading = how close tumour correspond to normal cells (done by a pathologist).
Staging = how far has it spread (done by a clinician)
Pleomorphism
Increasing variation in the size and shape of cells and nuclei
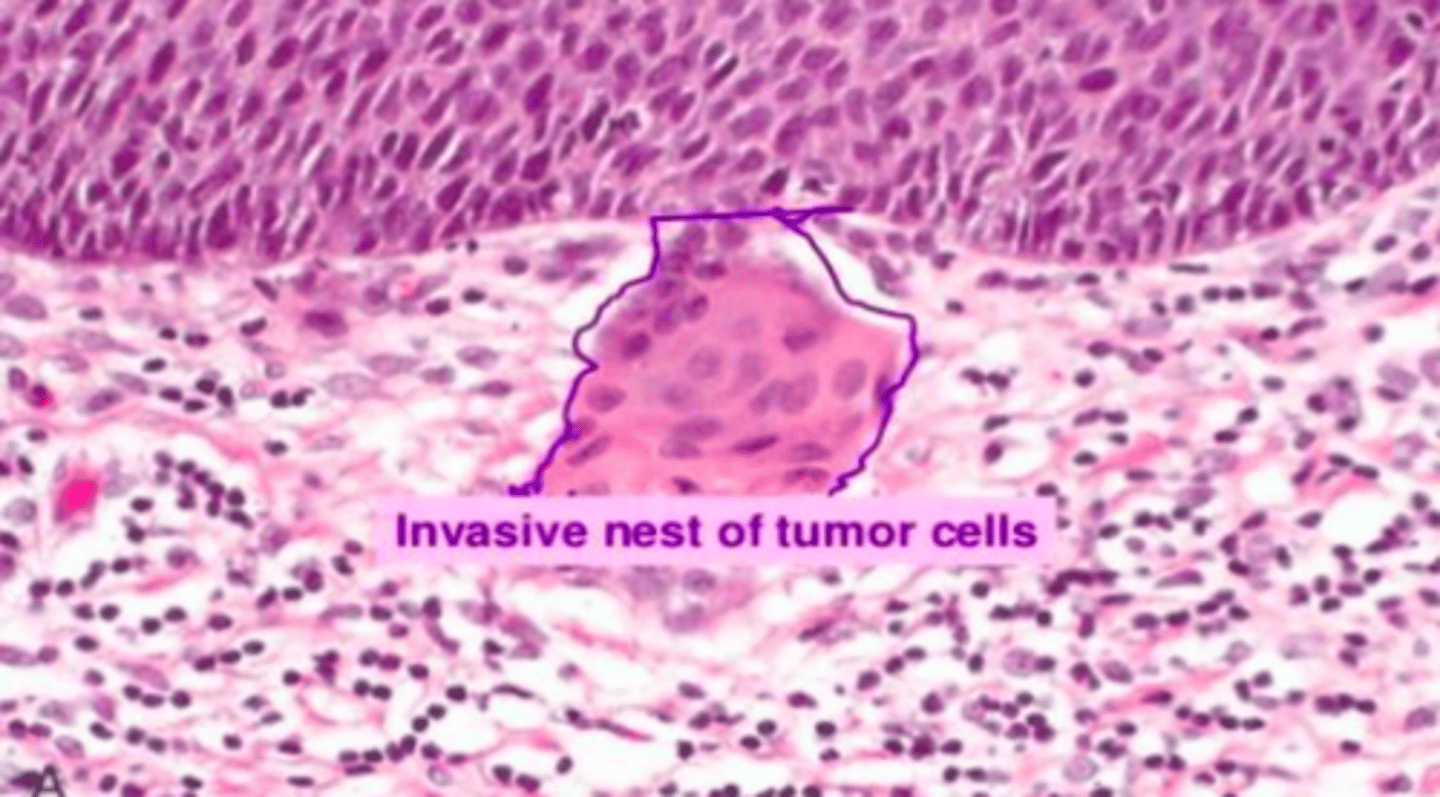
What are the histological characteristics of malignancy (pleomorphism)
- Increased nuclear size
- Increased nuclear to cytoplasmic ratio
- Clumping of chromatin in nuclei
- Increase in mitotic figures including abnormal mitosis
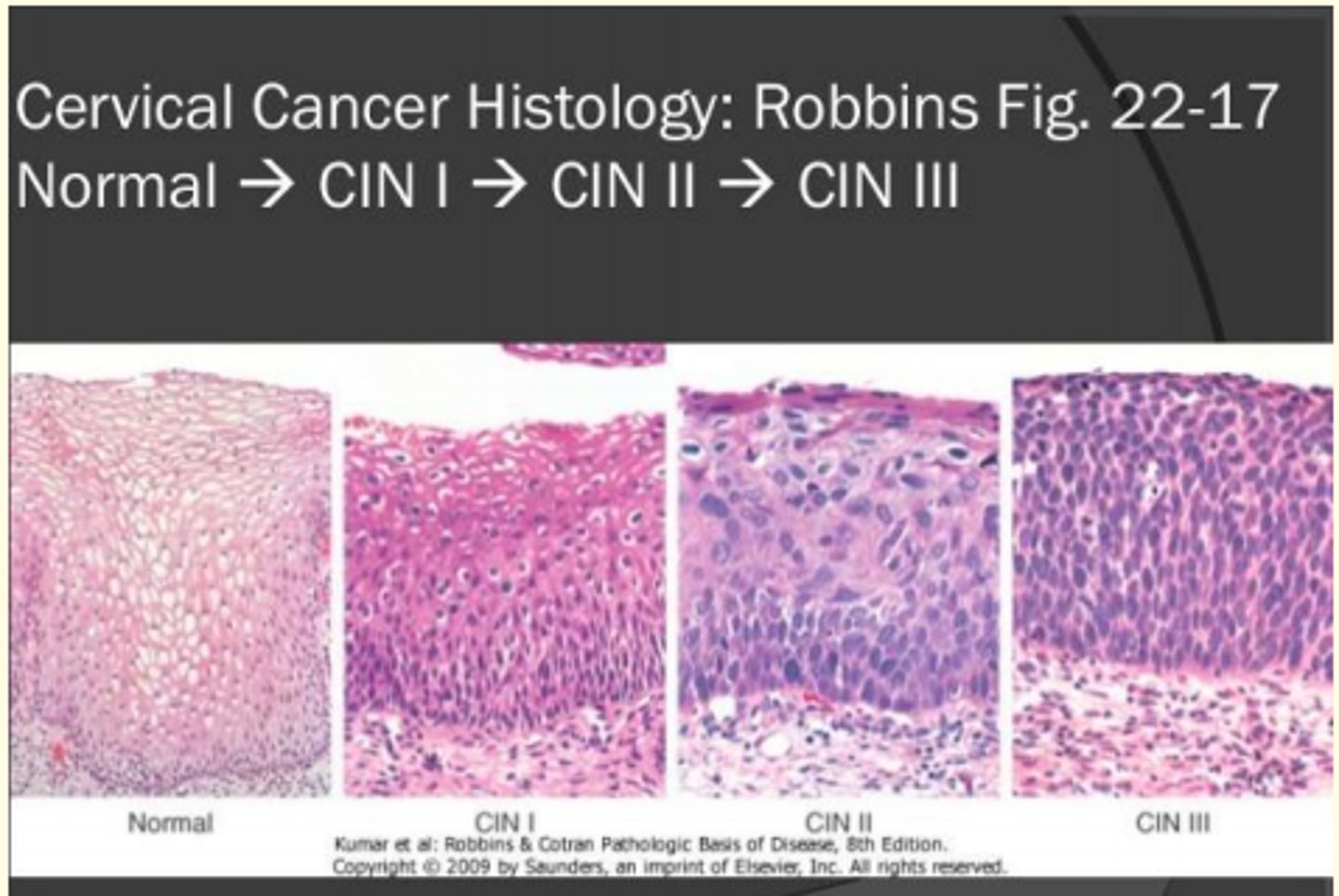
Dysplasia
Abnormal development or growth of cells, tissues, or organs
CIN
Cervical Intraepithelial neoplasia
Squamous cell carcinoma
Malignant tumor of the squamous epithelial cells in the epidermis
Grading
A method for evaluating a tumor based on microscopic examination of the cells
This is broadly based on how a tumour resembles its parent tissue
G1 = well differentiated
G2 = moderately differentiated
G3 = poorly differentiated
G4 = anaplastic carcinoma
Staging of the cancer (TNM)
Tumour staging is a measure of the malignant neoplasm's overall burden.
Size of primary tumor = (T)
Involvement of regional lymph nodes = (N)
Spread (metastasis) of tumor =(M)
All three then constitute the TNM stage which is further divided into stage 1 to stage 4
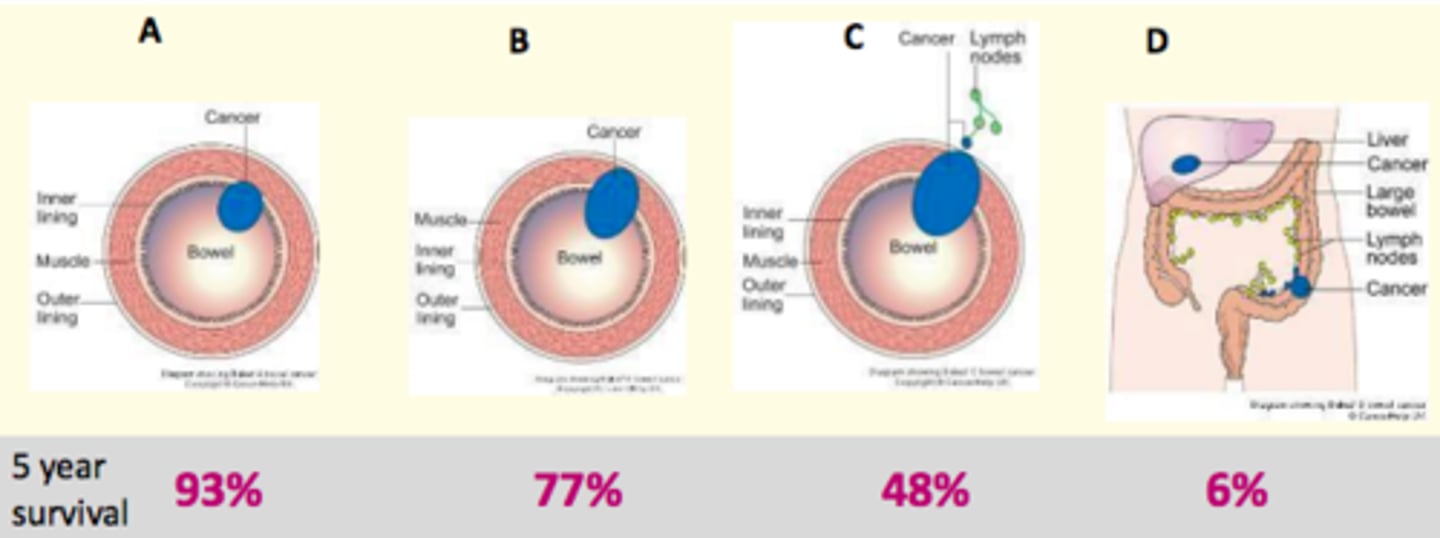
Colorectal cancer staging
Dukes staging
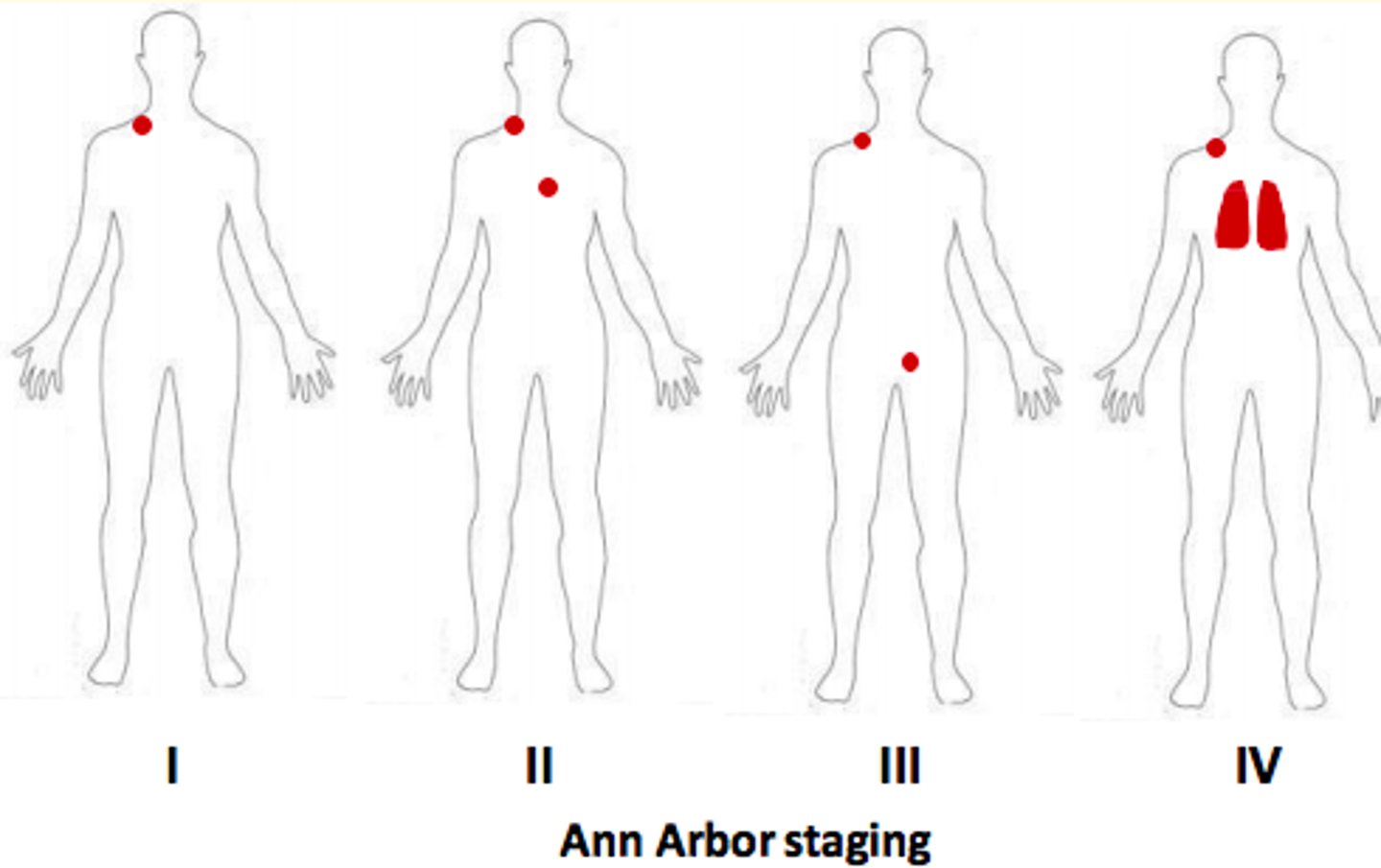
Lymphoma staging
Ann Arbor staging
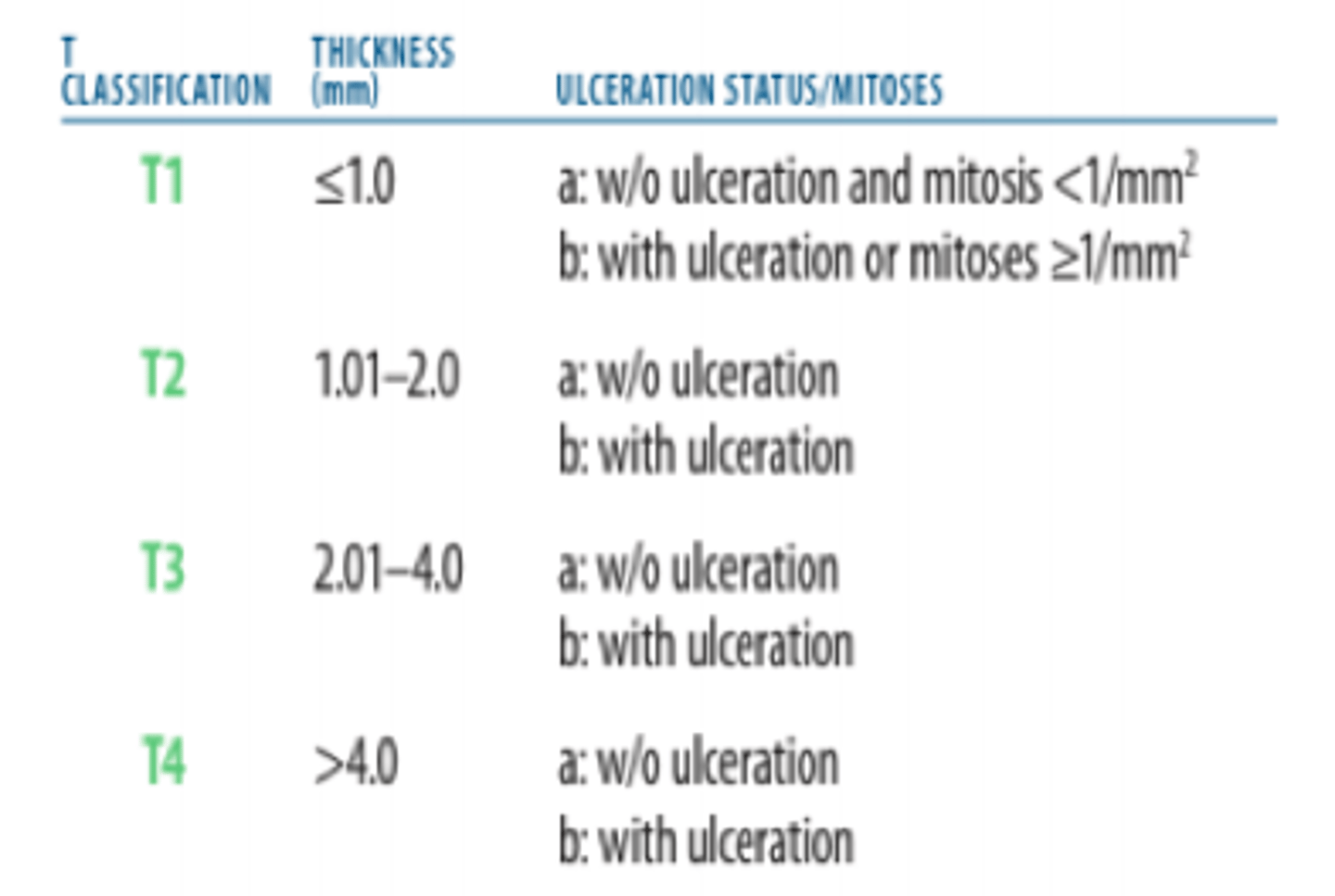
How is the T status of malignant melanoma described?
Described by Breslow's thickness (expressed in mm)
Lymph node (N) status
Regional lymph nodes
All organs have a specific lymphatic drainage - often the first sites to be involved by tumour metastasis
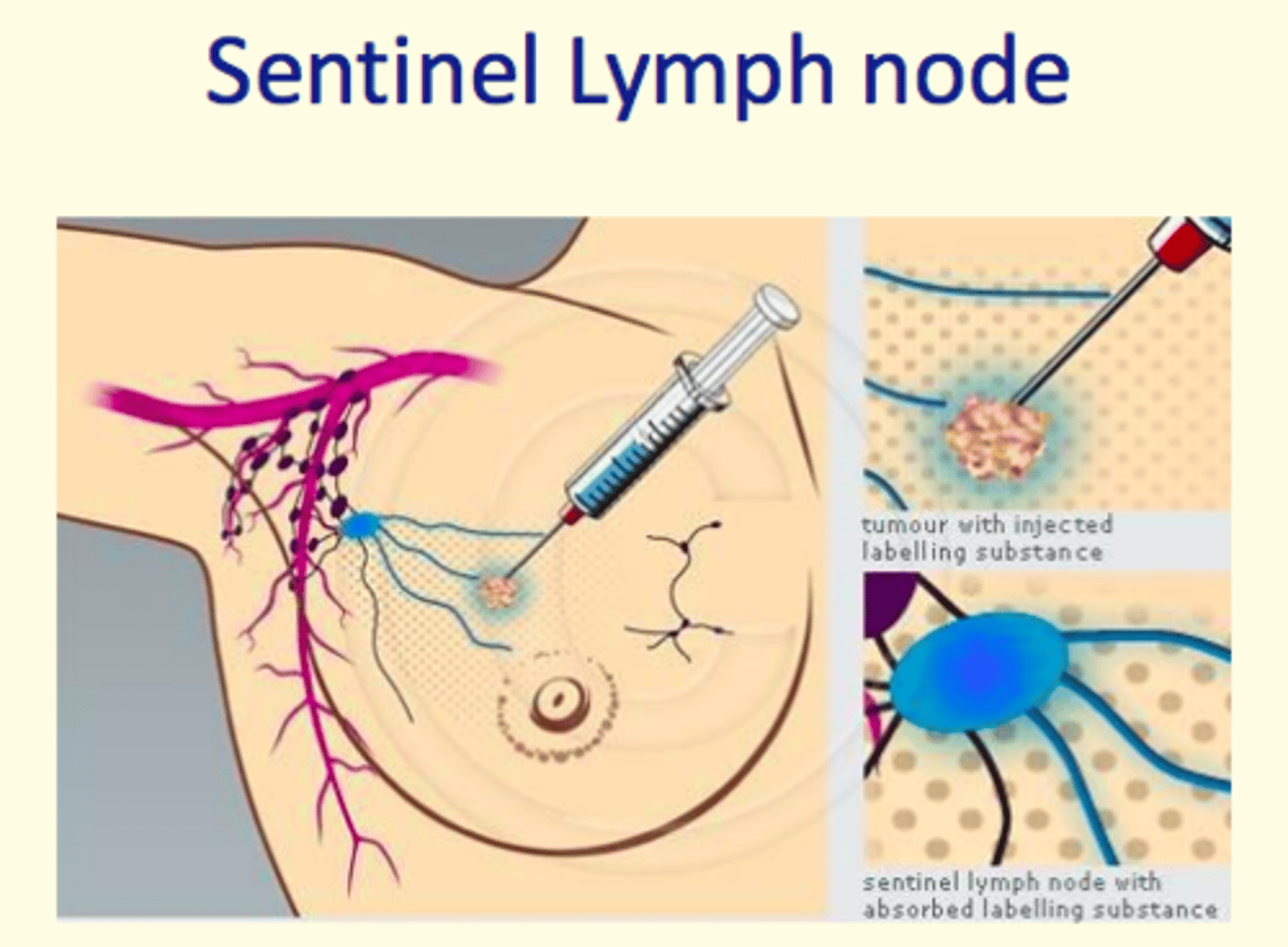
Sentinel lymph node
First node that receives draining from a body area suspected of having a tumor
Sentinel lymph node biopsy
Injection of blue dye and/or radioactive isotope (labelling substance) used to identify the sentinel lymph nodes (sentinel lymph node absorbs labelling substance)
This procedure helps give lymph node (N) status
Distant metastasis (M) status
Affects other organs distant to the primary tumour site
Lymphoma uses Ann Arbor staging.
Briefly describe each of the stages in this criteria...
Stage 1
Lymphoma in single node region
Stage 2
Two separate regions on one side of diaphragm
Stage 3
Spread to both sides of the diaphragm
Stage 4
Diffuse or disseminated involvement of one or more extra-lymphatic organs such as bone marrow or lungs.
Colorectal cancer uses Duke's staging.
Briefly describe each of the stages in this criteria...
Dukes' A
Invasion into but not through the bowel
Dukes' B
Invasion through the bowel wall
Dukes' C
Involvement of lymph nodes
Dukes' D
Distant metastases
Preferred staging system worldwide for cancer
TNM staging
Tumour stage is a measure of...
Tumour stage is a measure of the malignant neoplasm's overall burden
Neoadjuvant treatment
Treatment provided BEFORE primary cancer treatment (surgery)
Adjuvant treatment
Short course of high-dose of drug treatment AFTER surgery to destroy residual cells and prevent recurrence
Aimed at eradicating subclinical and residual disease
Radiotherapy
Treatment of tumors using doses of radiation; radiation oncology
Focused on the tumour with shielding of surrounding healthy tissue
Shrink tumour as part of neoadjuvant treatment
Why is radiotherapy given in fractionated doses
Minimise damage to normal healthy tissue

When may radiotherapy be the main form of treatment for cancer?
Anal squamous cell carcinoma
When may radiotherapy be used in the palliative care setting?
Controlling bleeding
Pain relief
The radiation oncologist must select the ___ ___ ___. This must be large enough to cure the cancer but avoid acute and long-term toxicity to the healthy parts of the patient.
The radiation oncologist must select the field of radiation. This must be large enough to cure the cancer but avoid acute and long-term toxicity to the healthy parts of the patient.
There are different types of radiotherapy, give some examples
- Brachytherapy
- Internal
- ARC
- Proton beam
Radiation treatment can have side effects that might not be seen until long after treatment has ended.
Name some examples of these effects...
Cardiac damage after breast cancer
Cognitive/behavioural changes in children
Chemotherapy can be used in the neo-adjuvant or adjuvant setting.
What does this mean?
Neo-adjuvant setting
Prior to surgery to shrink the tumour
Adjuvant setting
Follows surgery and aimed at eradicating the subclinical disease
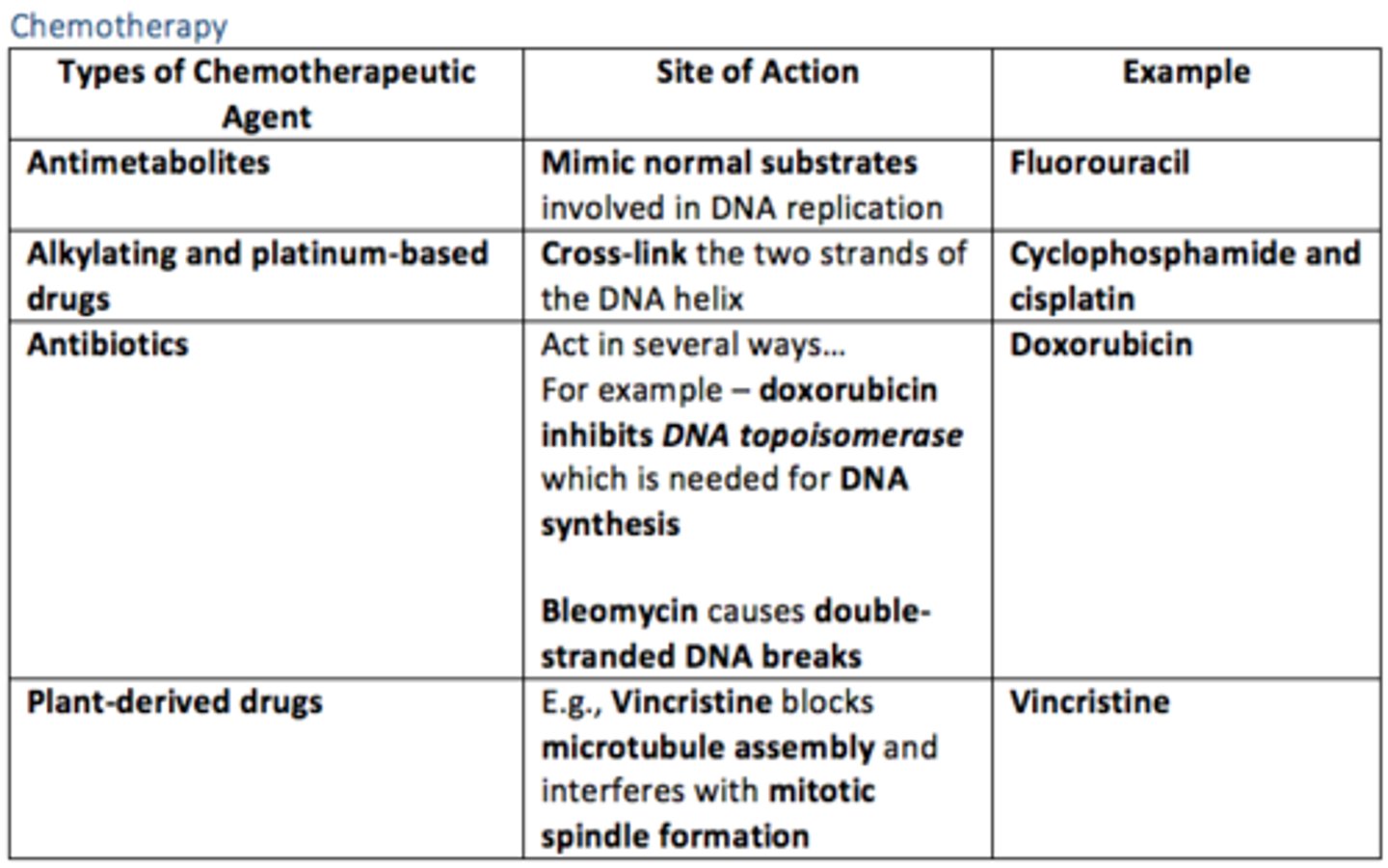
Different types of chemotherapeutic agents
1) Antimetabolites
2) Alkylating and platinum-based drugs
3) Antibiotics
4) Plant-derived drugs
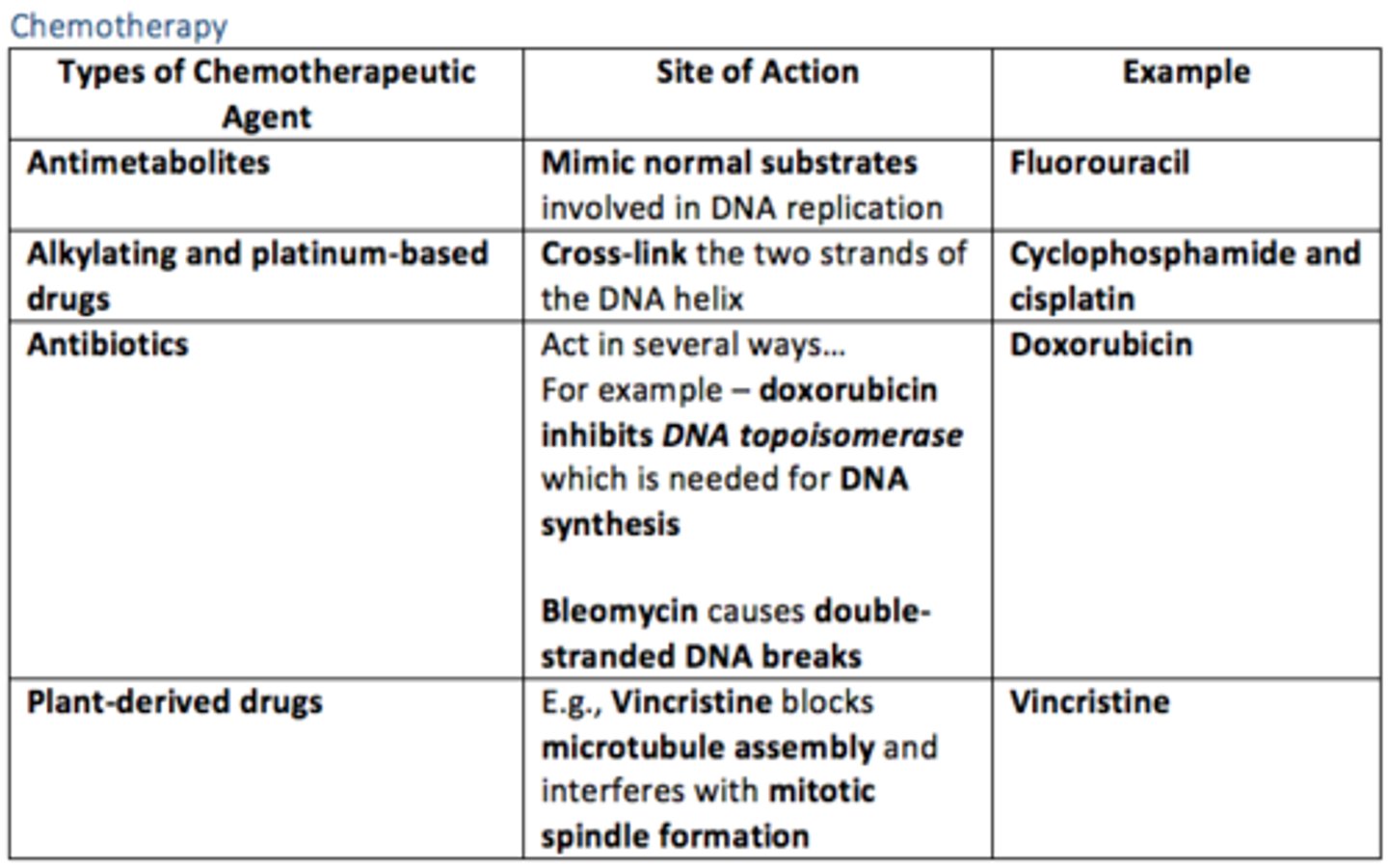
How do antimetabolite chemotherapeutic drugs act?
Mimic normal substrates involved in DNA replication
E.g., Fluorouracil
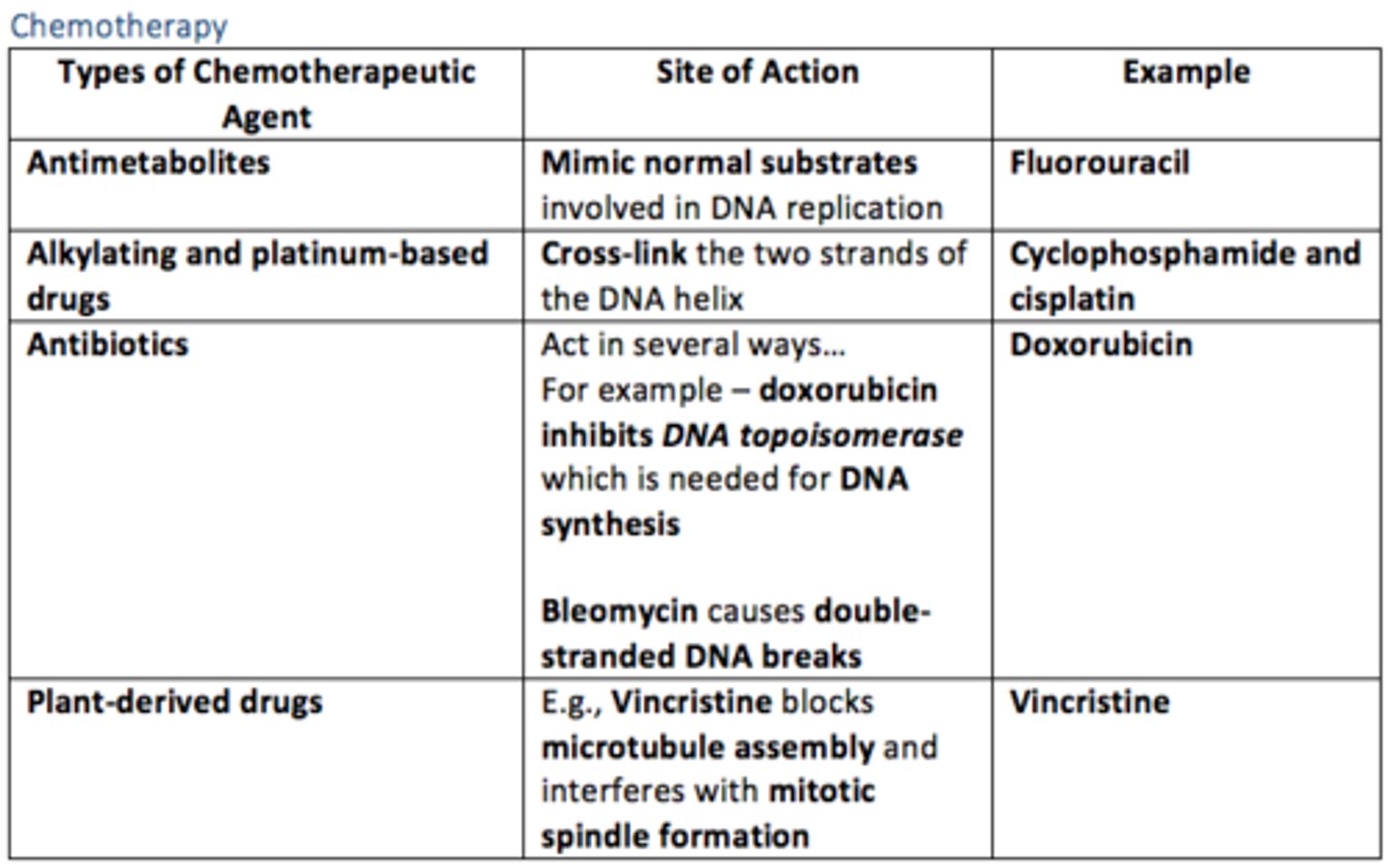
How do alkylating and platinum-based chemotherapeutic drugs act?
Cross-link the two strands of the DNA helix
E.g., Cyclophosphamide and Cisplatin
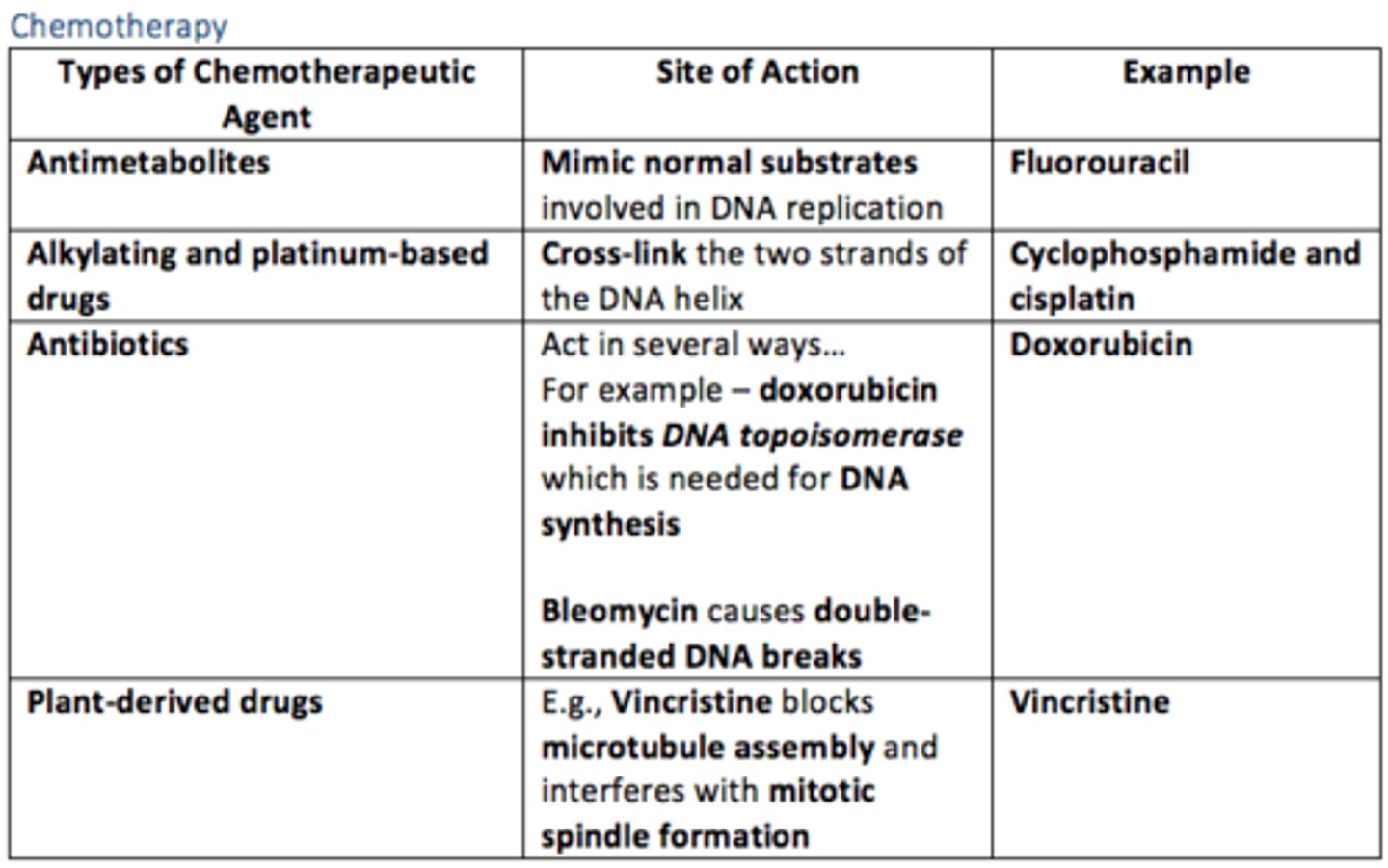
How do antibiotic chemotherapeutic agents act?
Act in several ways...
Doxorubicin = inhibits DNA topoisomerase which is needed for DNA synthesis
Bleomycin = causes double-stranded DNA breaks
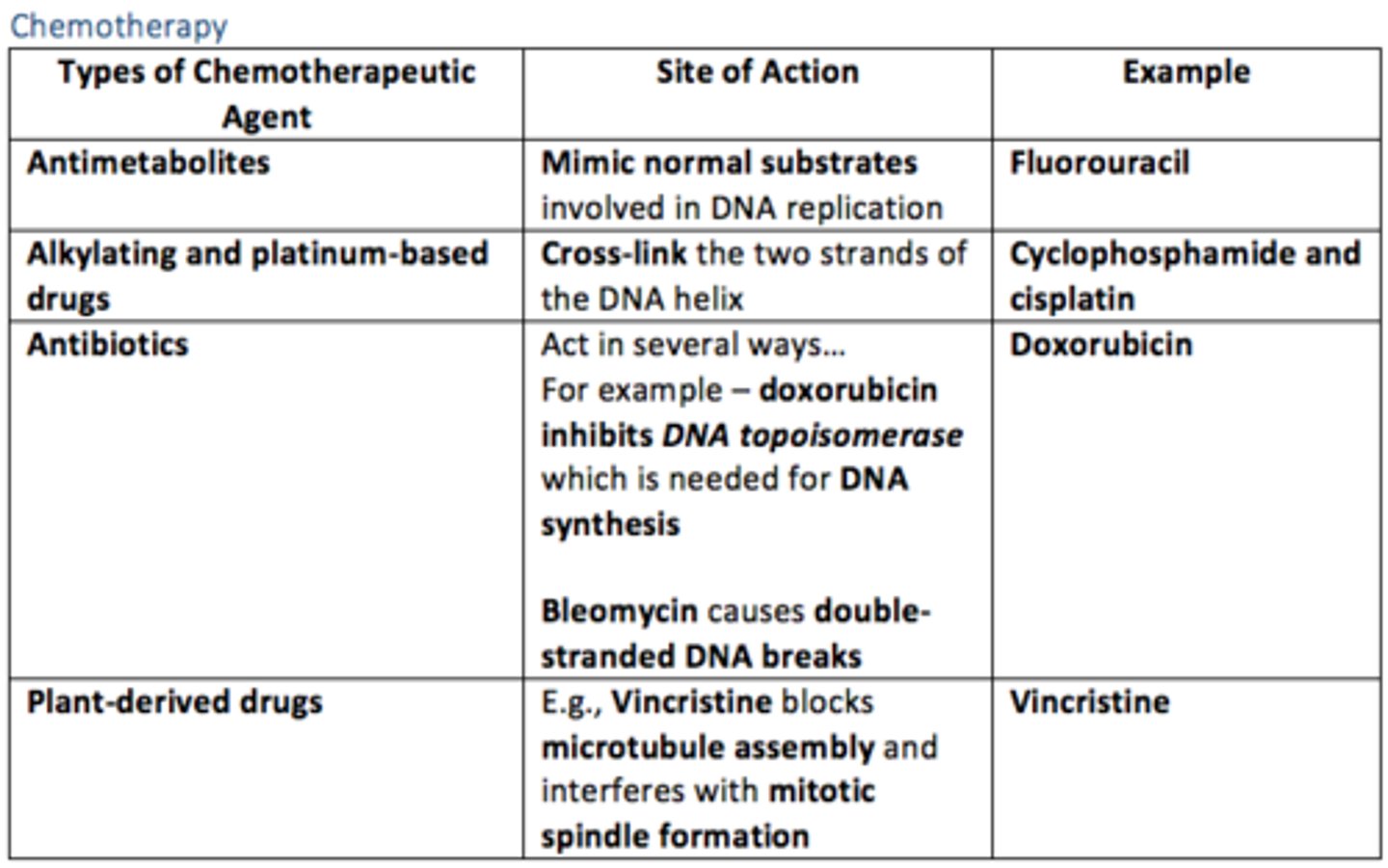
How do plant-derived chemotherapeutic agents act?
Vincristine blocks microtubule assembly and interferes with mitotic spindle formation
Hormonal treatment for cancer
Mostly used to treat tumours that are driven by hormones such as oestrogen and testosterone
They are non-toxic but have side effects
Give examples of hormonal treatment for hormone receptor-positive breast cancer
Selective oestrogen receptor modulators (SERMs) such as Tamoxifen bind to oestrogen receptors and prevent oestrogen from binding
Give examples of hormonal treatment for prostate cancer
Androgen blockage used for prostate cancer
What is targeted cancer therapy?
These are drugs which specifically act against specific molecular targets in cancer cells.
Targeted therapy is split into two main categories...
1) Antibody drugs = manmade versions of immune system proteins, targeting receptors e.g., rituximab
2) Small molecules = target abnormal proteins or enzymes that form on or inside of cancer cells and promote uncontrolled tumour growth e.g., imatinib
Molecular Therapy
If the patient (metastatic colorectal disease) has a mutated form of Kras, the patient does not respond to ___ ___ such as cetuximab and other forms of treatment are required
If the patient (metastatic colorectal disease) has a mutated form of Kras, the patient does not respond to EGFR inhibitors such as cetuximab and other forms of treatment are required
Molecular Therapy
If the patient (metastatic colorectal disease) has the wild-type Kras, ____ is an option
If the patient (metastatic colorectal disease) has the wild-type Kras, EGFR is an option
Personalised treatments aim at giving patients the best treatment according to...
1) Personal medical history
2) Physiological status
3) Molecular characteristics of their tumours
4) Their genome
Personalised medicine demands an increased understanding of genomics, including the risk of adverse drug effects and identifying patients who will survive with reduced treatment
Tumour markers
Tumour markers are released by cancer cells into the blood circulation.
Tumour markers can be used for...
1) Diagnosing conditions
- PSA
- AFP
2) Monitoring tumour burden during treatment & follow-up
- CEA
- AFP
- hCG
- Ca-125
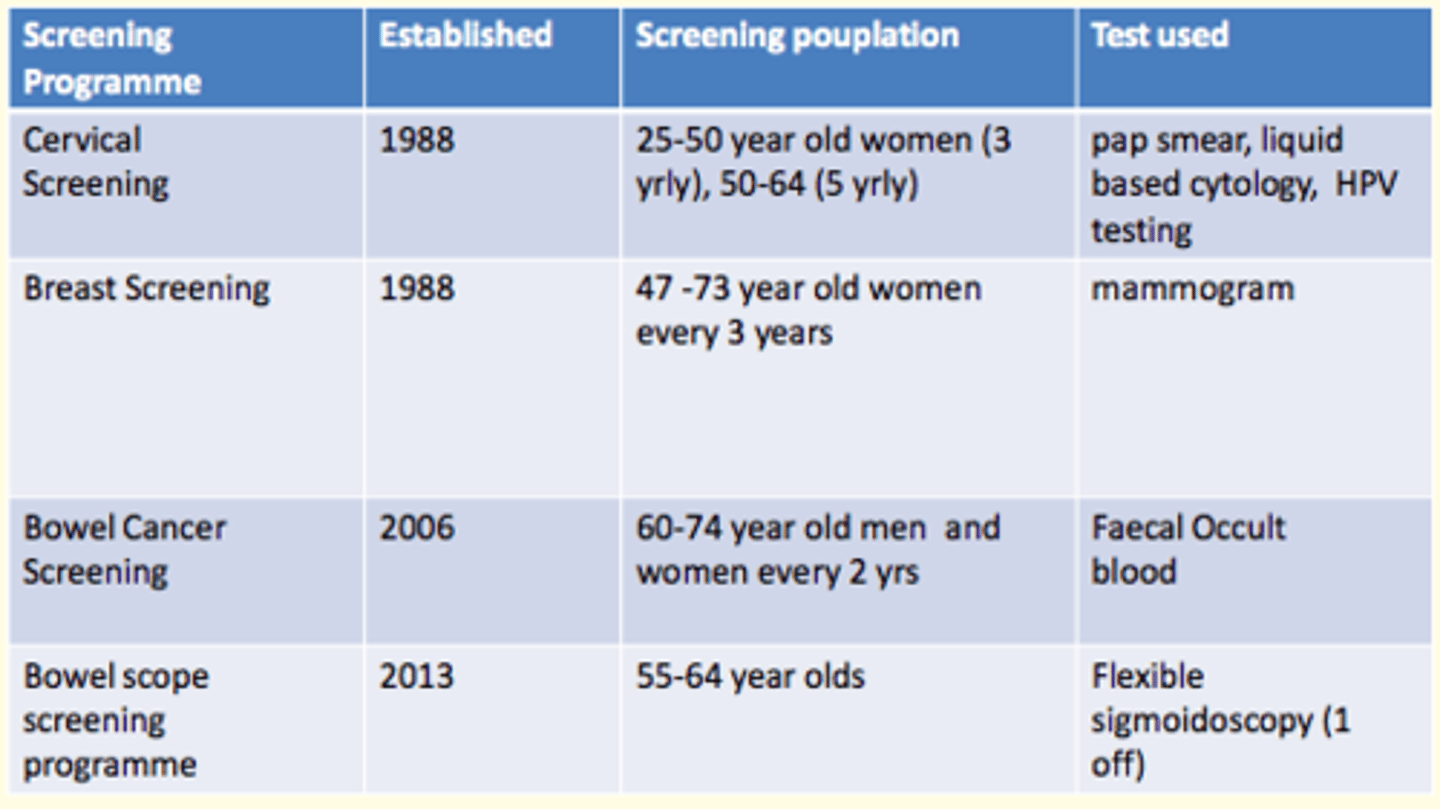
Screening programmes in the UK for cancer
In the UK, screening programmes exist for cervical, breast and bowel cancer
Cervical screening
- PAP smear
- Liquid based cytology
- HPV testing
Breast screening
- Mammogram
Bowel cancer screening
- Faecal occult blood
Bowel scope screening programme
- Flexible sigmoidoscopy
How does the targeted therapy Imatinib (Gleevec) work to treat Chronic Myeloid Leukemia (CML)?
CML shows a chromosomal rearrangement (t9:22) creating an abnormal Philadelphia chromosome in which an oncogenic fusion protein (BCR-ABL) is encoded.
Imanitib (Gleevec) inhibits the fusion protein (BCR-ABL).
Regarding carcinoma of the breast, answer true or false to the following statements...
a) Is the most commonly of ductal type
b) Tubule formation is assessed in grading
c) Occurs between ages of 40-50
d) Abnormalities of retinoblastoma gene may be identified in some cases
e) Is familial in 50% of cases
Regarding carcinoma of the breast, answer true or false to the following statements...
a) Is the most commonly of ductal type = true
b) Tubule formation is assessed in grading = true
c) Occurs between ages of 40-50 = false
d) Abnormalities of retinoblastoma gene may be identified in some cases = true
e) Is familial in 50% of cases = false (these famiial cases are much less common)
Regarding colorectal cancer, answer true or false to the following statements...
a) May be associated with defected DNA mismatch repair genes
b) Occurs most commonly between 40-50 years of age
c) The extent of spread is incorporated into Dukes' staging
d) Is usually a squamous cell carcinoma
e) Has a 95% five year survival rate if confined to the bowel wall
Regarding colorectal cancer, answer true or false to the following statements...
a) May be associated with defected DNA mismatch repair genes = true
b) Occurs most commonly between 40-50 years of age = false (peak age is older than 40-50)
c) The extent of spread is incorporated into Dukes' staging = true
d) Is usually a squamous cell carcinoma = false
e) Has a 95% five year survival rate if confined to the bowel wall = true
Regarding the treatment of malignancy, answer true or false to the following statements...
a) Castration may be helpful in treating prostatic cancer
b) Hormonal manipulation is of little value in the treatment of carcinoma of the breast
c) The major effect of radiotherapy is on tumour cell membranes
d) Most chemotherapeutic drugs affect cell division
e) Neoadjuvant treatment is given after surgery
Regarding the treatment of malignancy, answer true or false to the following statements...
a) Castration may be helpful in treating prostatic cancer = true
b) Hormonal manipulation is of little value in the treatment of carcinoma of the breast = false (tamoxifen is an anti-oestrogen)
c) The major effect of radiotherapy is on tumour cell membranes = false
d) Most chemotherapeutic drugs affect cell division = true
e) Neoadjuvant treatment is given after surgery = false (neoadjuvant treatment is given BEFORE surgery)