PERIO W1 CH 1: Periodontium
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
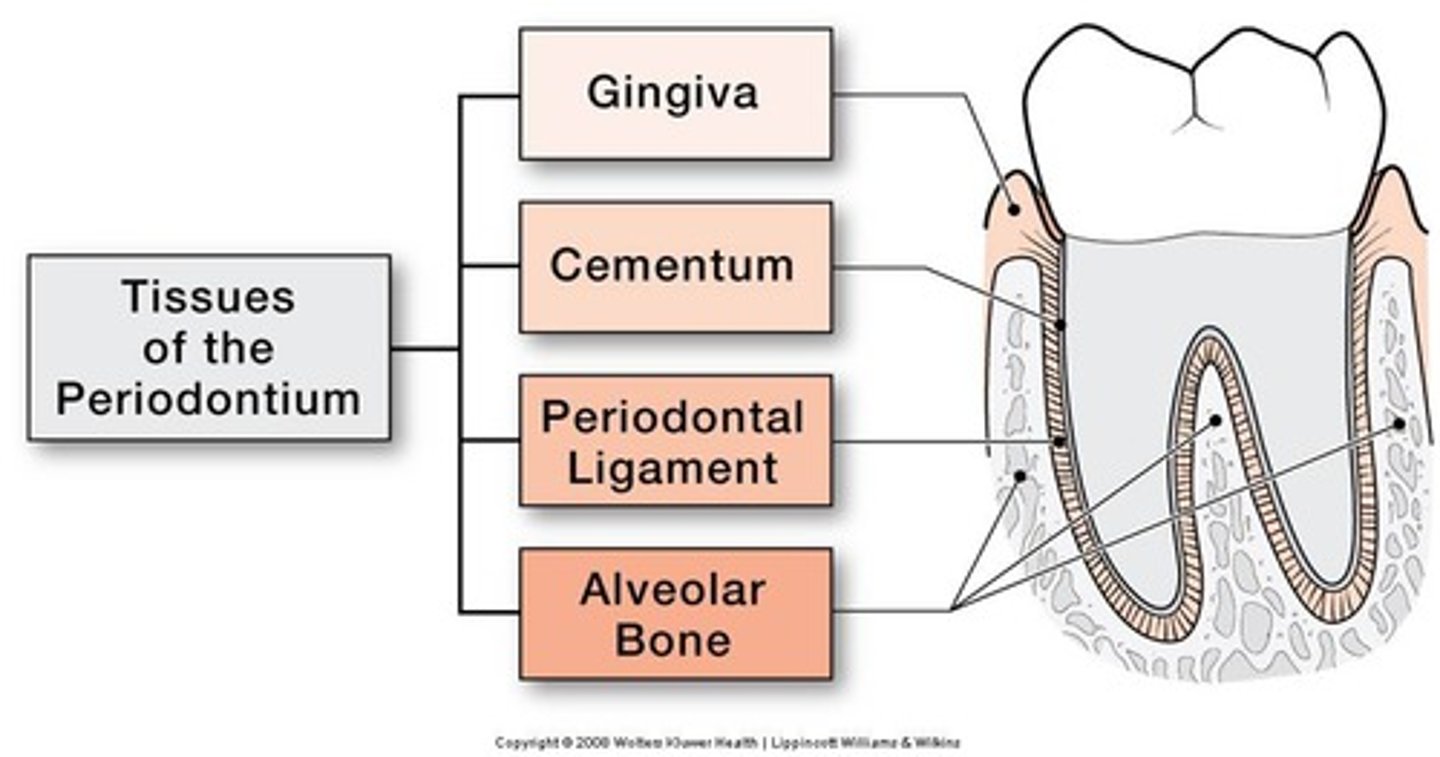
Define Periodontium
functional system (aka multiple structures)
of tissues that surrounds teeth and attaches them to the jawbone
List the 4 main tissues that make up the Periodontium
1. Gingiva
2. Cementum
3. Periodontal Ligament
4. Alveolar Bone
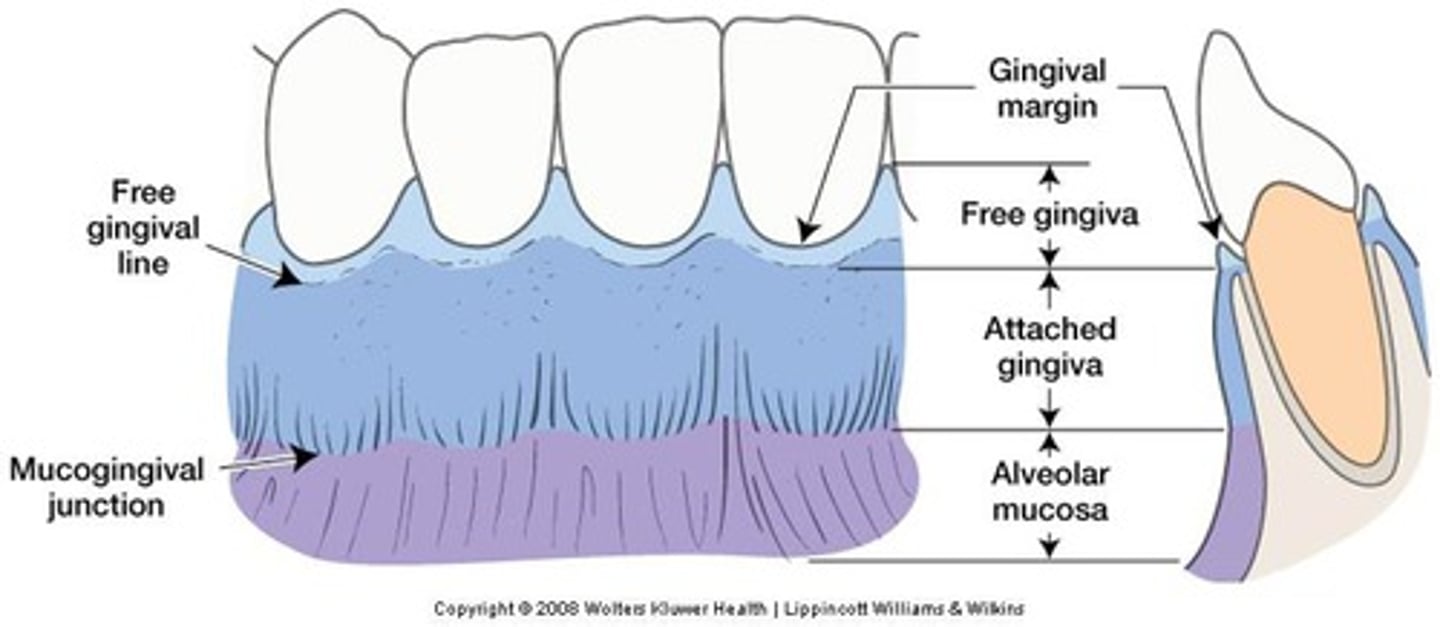
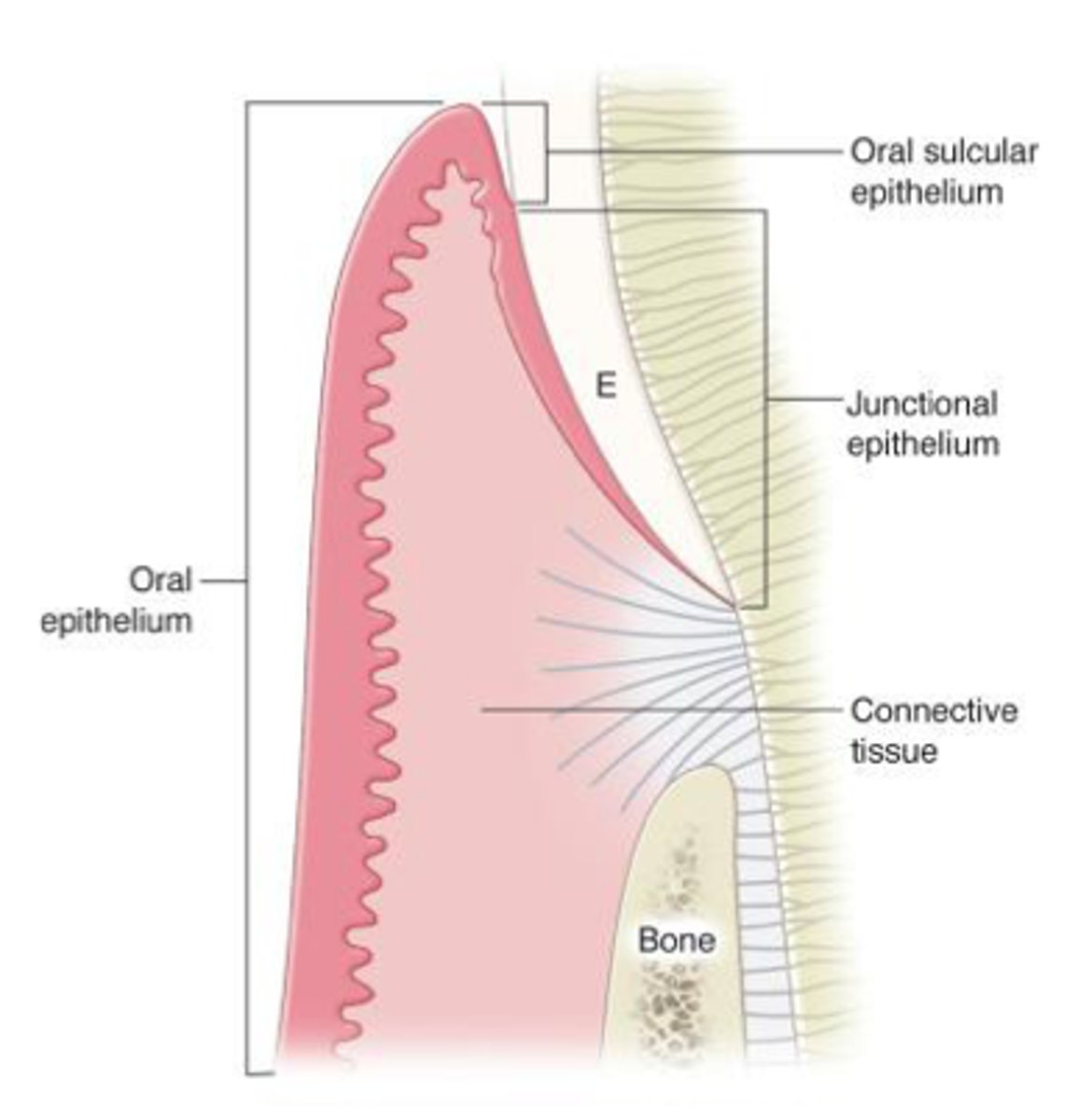
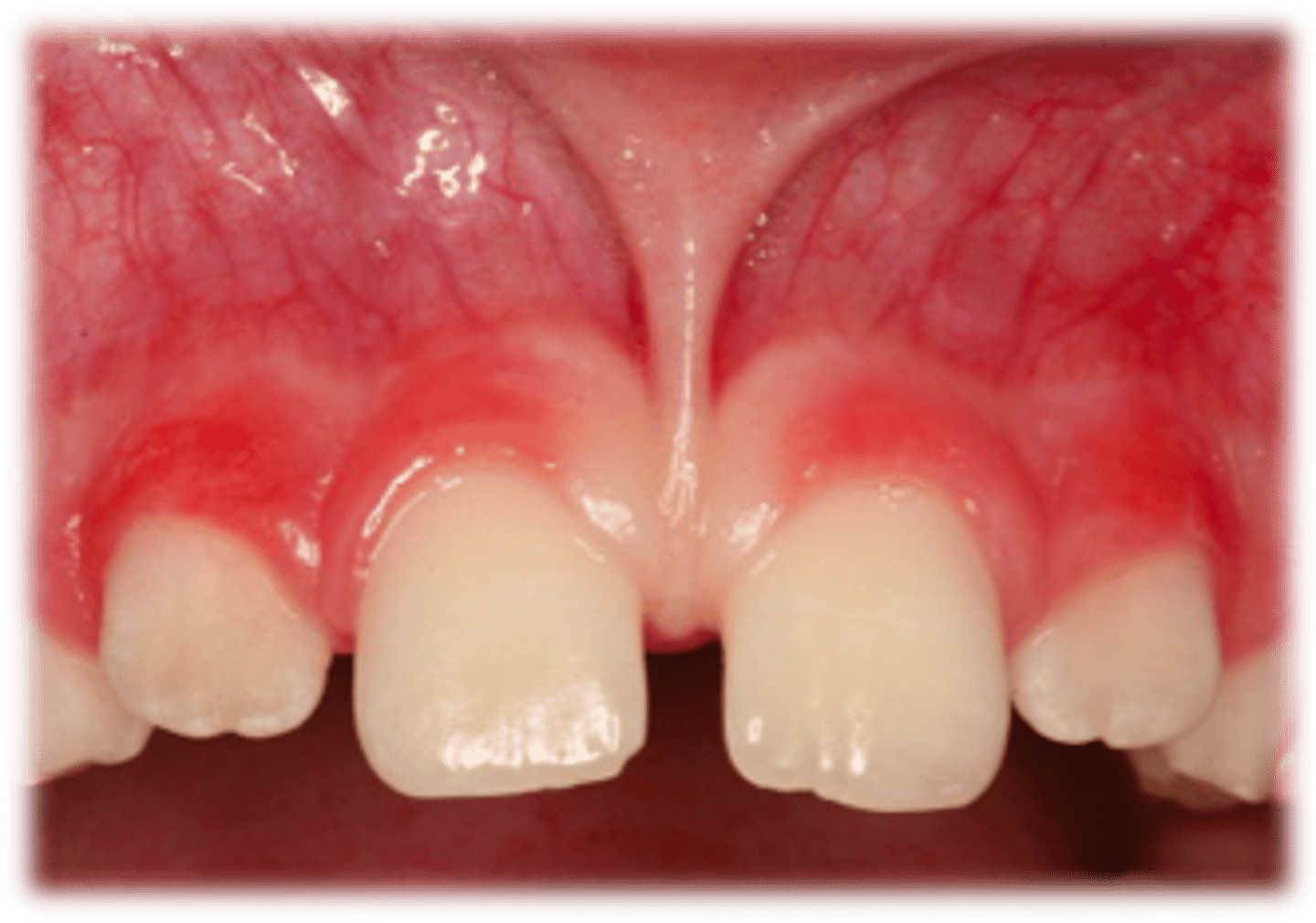
Describe the Gingiva and its function(s)
Gingiva (oral mucosal tissue) is composed of a thin outer layer of epithelium and a thicker layer of connective tissue that covers the alveolar processes (contains the teeth sockets) of the jaw
fx:
- provides a tissue seal around the cervical portion (neck) of the tooth
- helps hold the tissue against teeth during mastication
- protects underlying tooth-supporting structures of the periodontium from oral environment
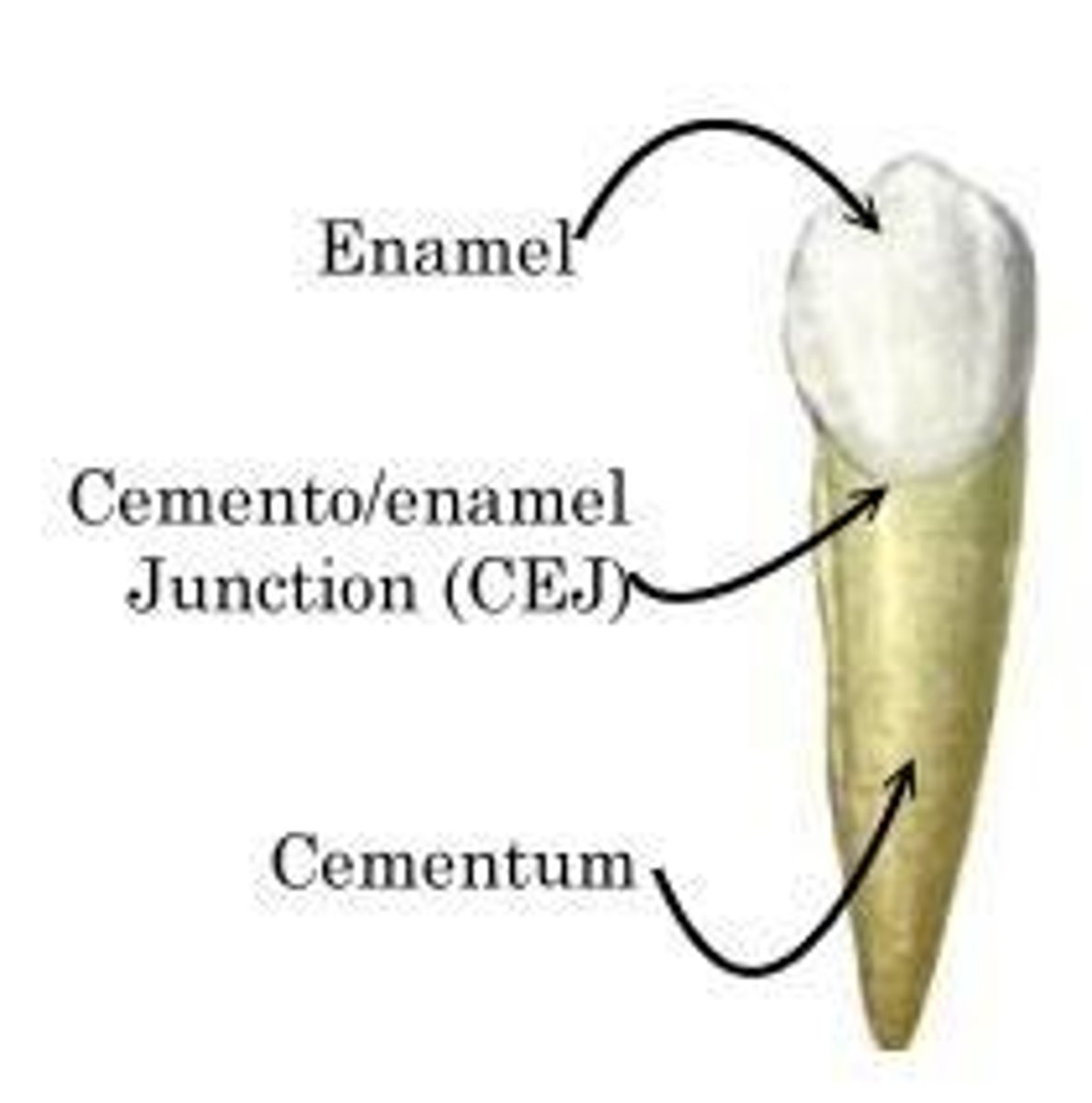
What creates the contour and shape of the gingival margin?
Cementoenamel junction (CEJ)
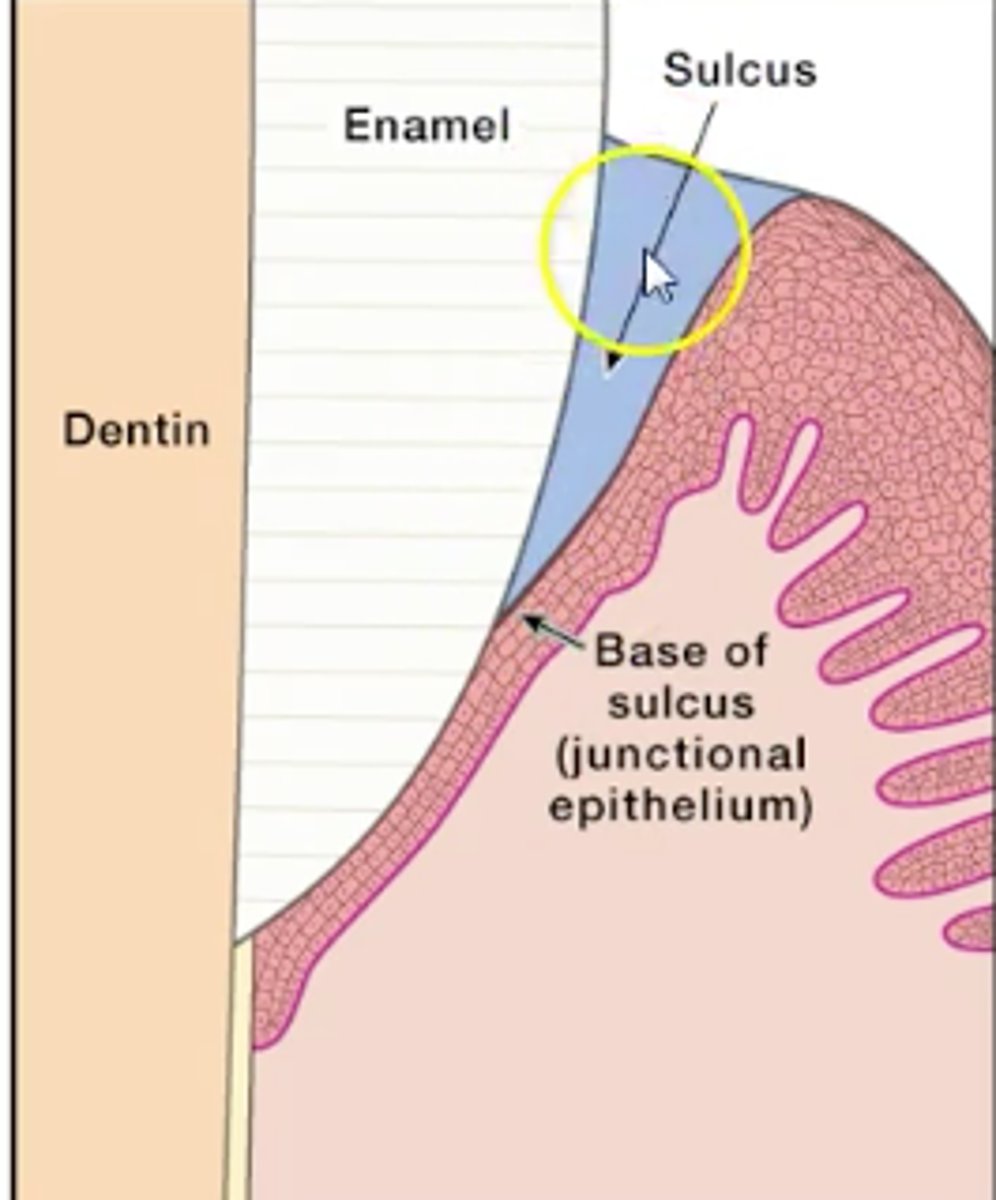
How is the gingiva attached to the tooth?
junctional epithelium
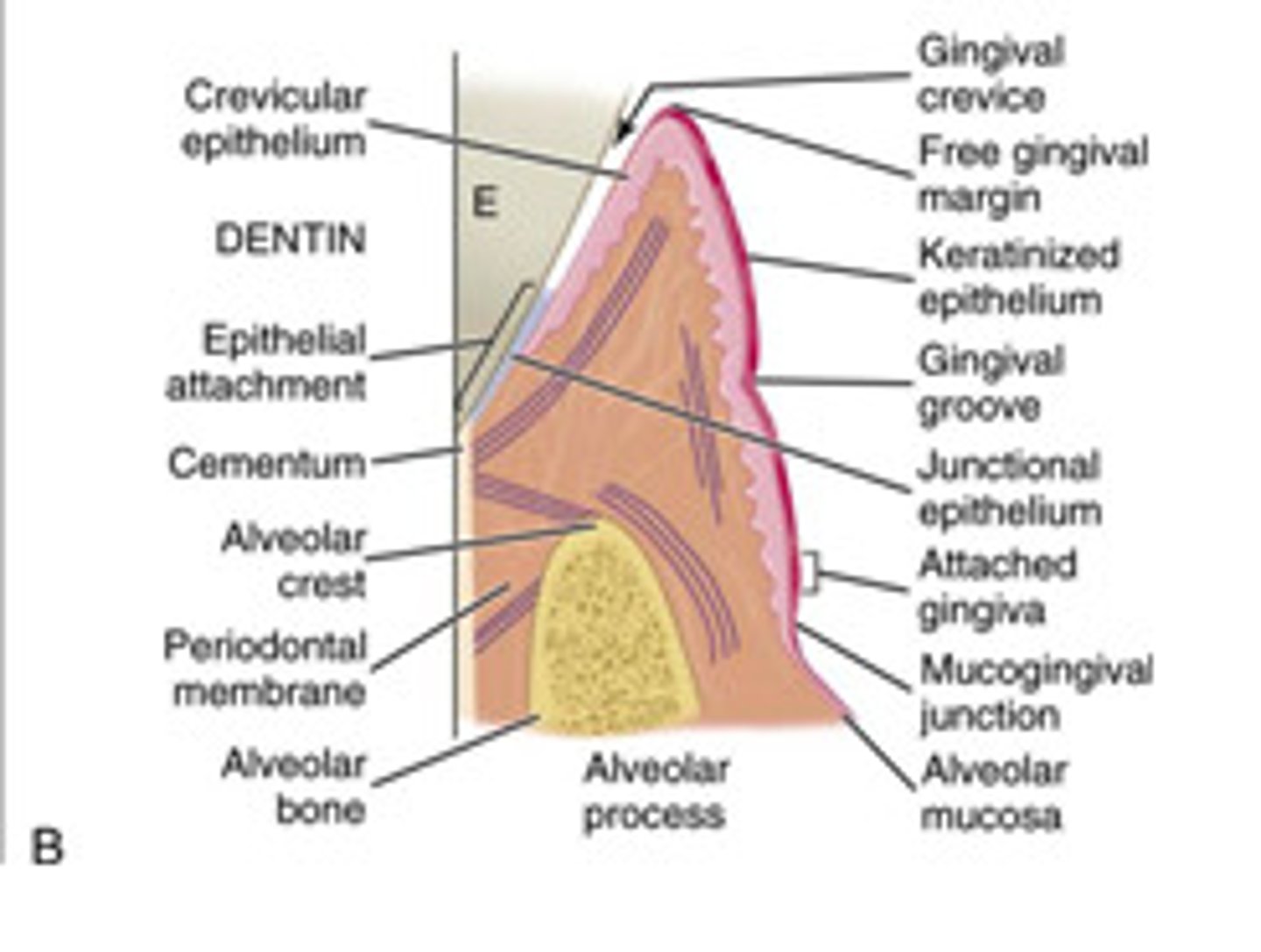
Where is the junctional epithelium located?
At the base of the sulcus where the free gingiva meets the start of the attached gingiva
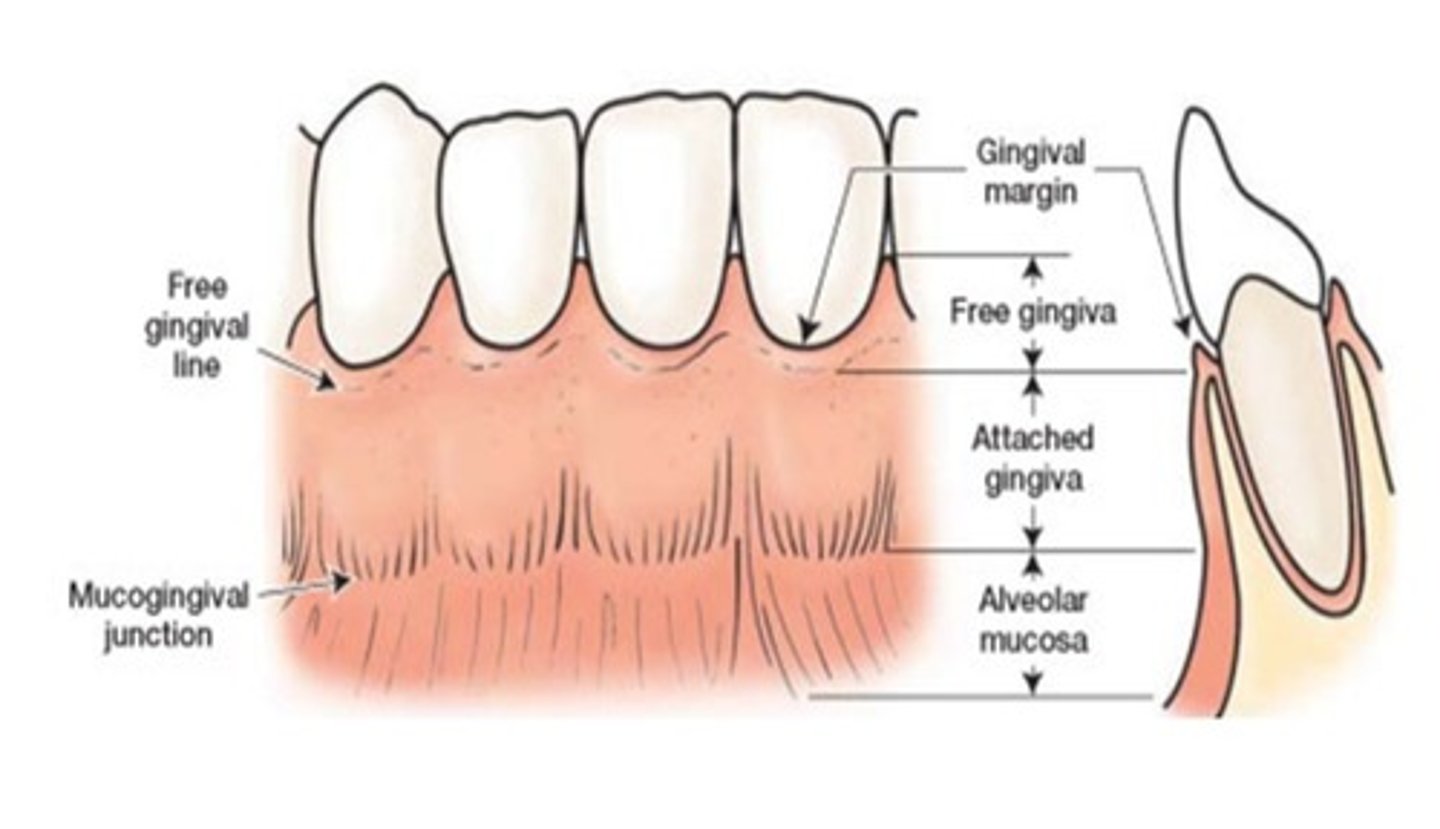
What are the 4 anatomical areas of the Gingiva?
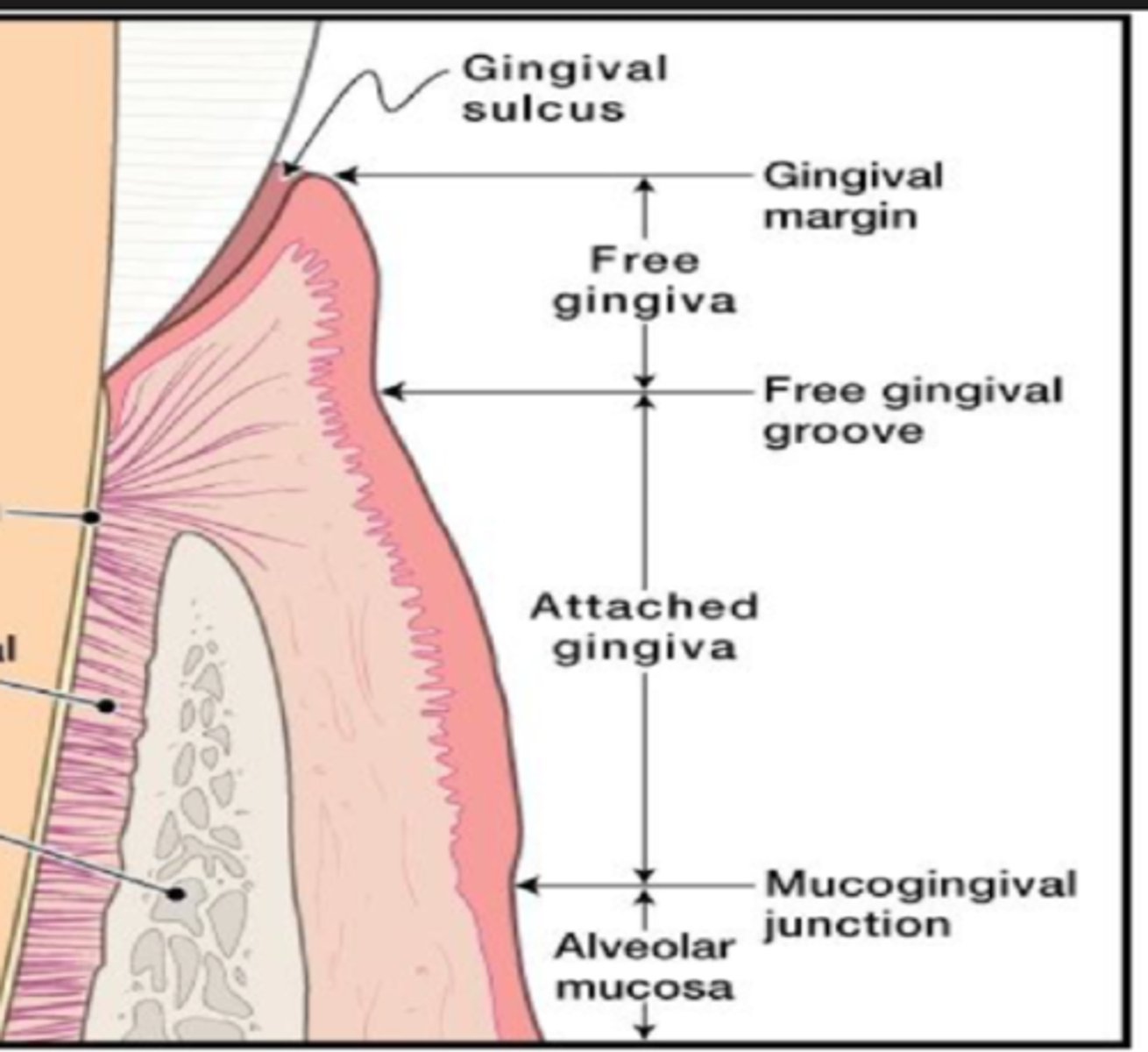
free gingiva, gingival sulcus, interdental gingiva and attached gingiva
*draw a diagram
How does the free gingiva, gingival sulcus, interdental gingiva and attached gingiva protect periodontium from oral environment?
The free, attached, and interdental gingiva acts as a barrier, shielding the periodontium from mechanical and bacterial damage. It can also utilize the saliva and immune system as a form of defense
What are the 2 boundaries of the gingiva?
Gingival margin - coronal
Alveolar mucosa - apical
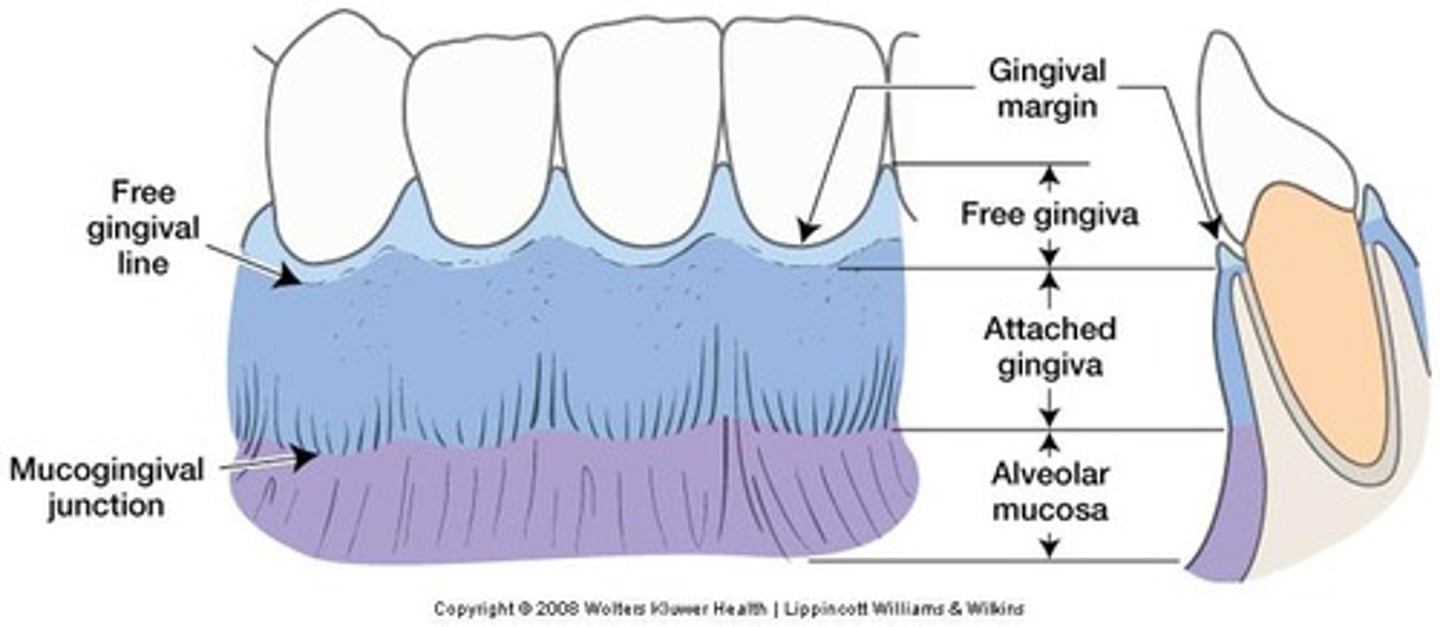
What is the free gingival groove?
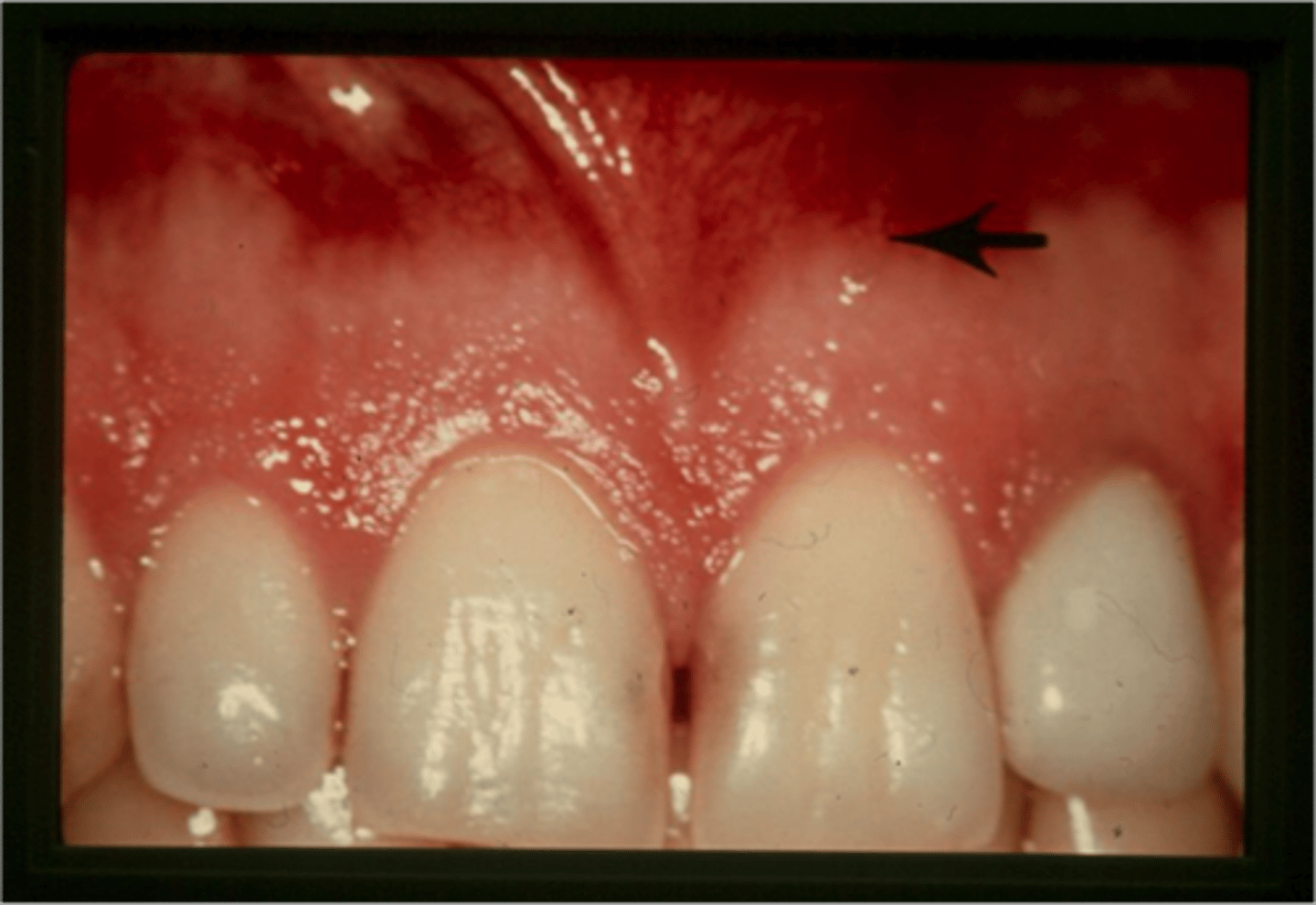
shallow linear depression that separates the free and attached gingiva (can be hard to see with the naked eye)
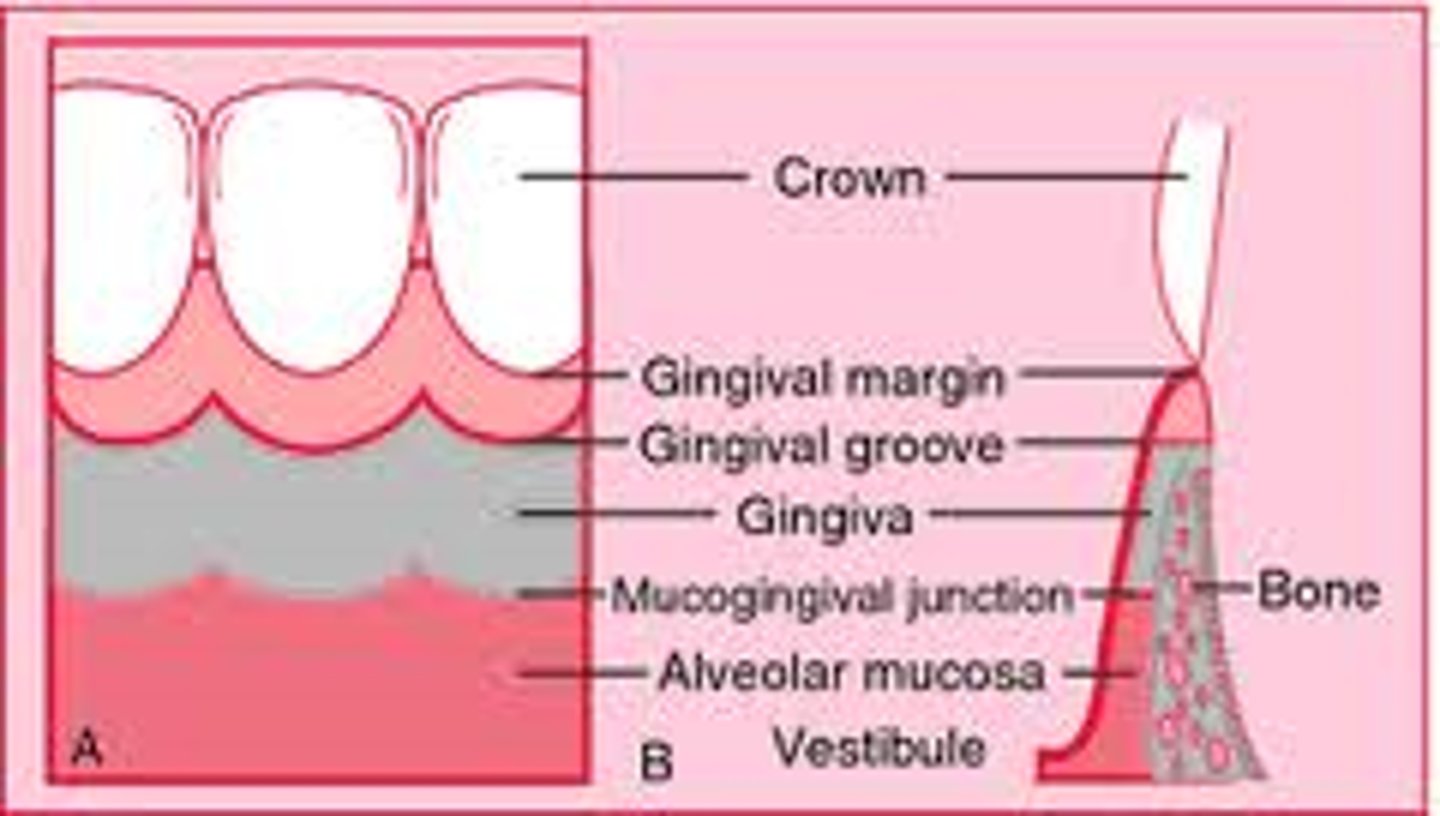
What is the mucogingival junction?
clinically visible boundary where the pink attached gingiva meets the red, shiny alveolar mucosa
Define free gingiva. Where is it attached?
the unattached portion of the gingiva that surrounds the tooth in the region of the CEJ (Cementoenamel Junction)
It is attached by the junctional epithelium at the base of the sulcus
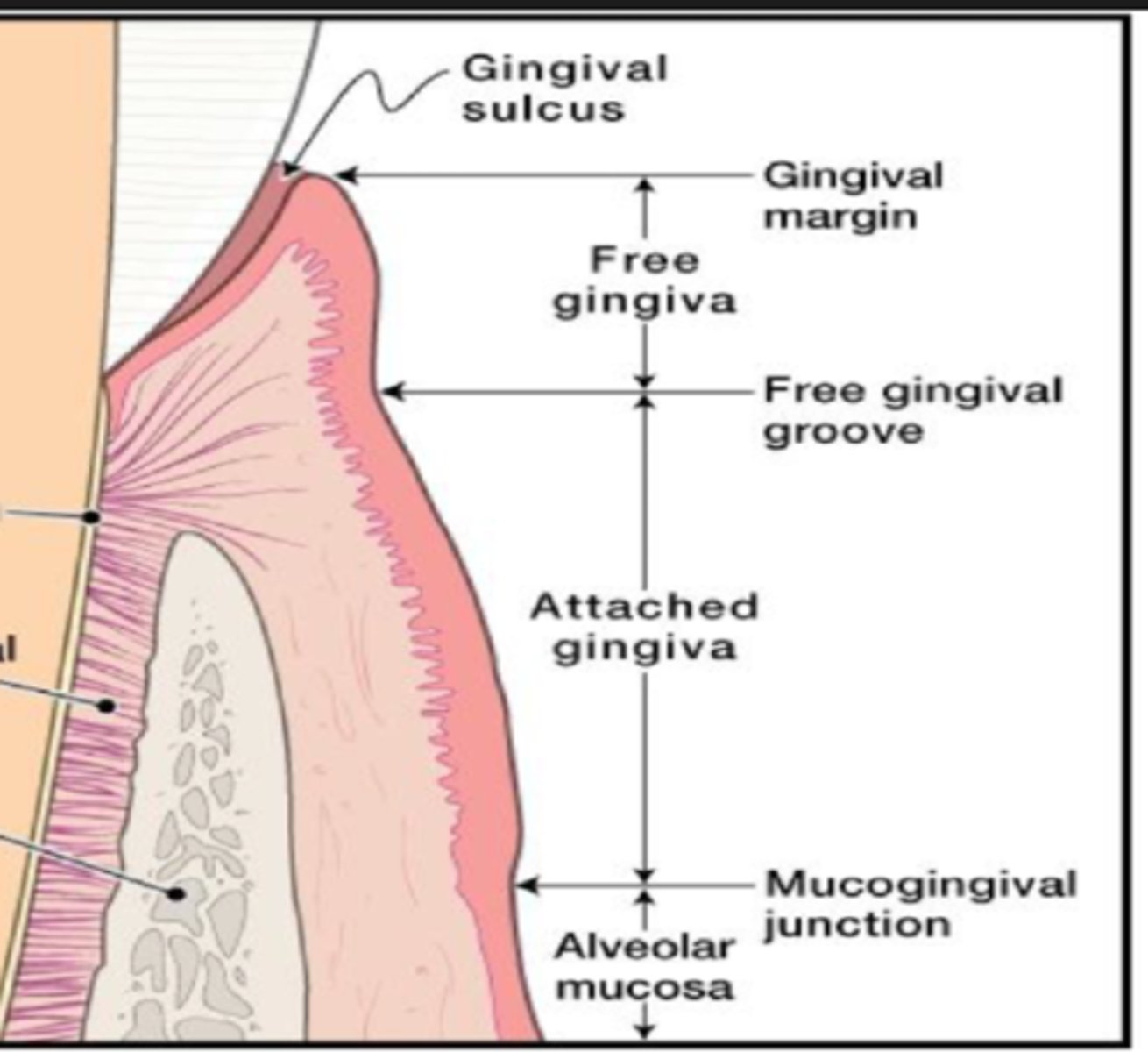
The unattached gingiva creates a space between the gingiva and the tooth which is called?
gingival sulcus.
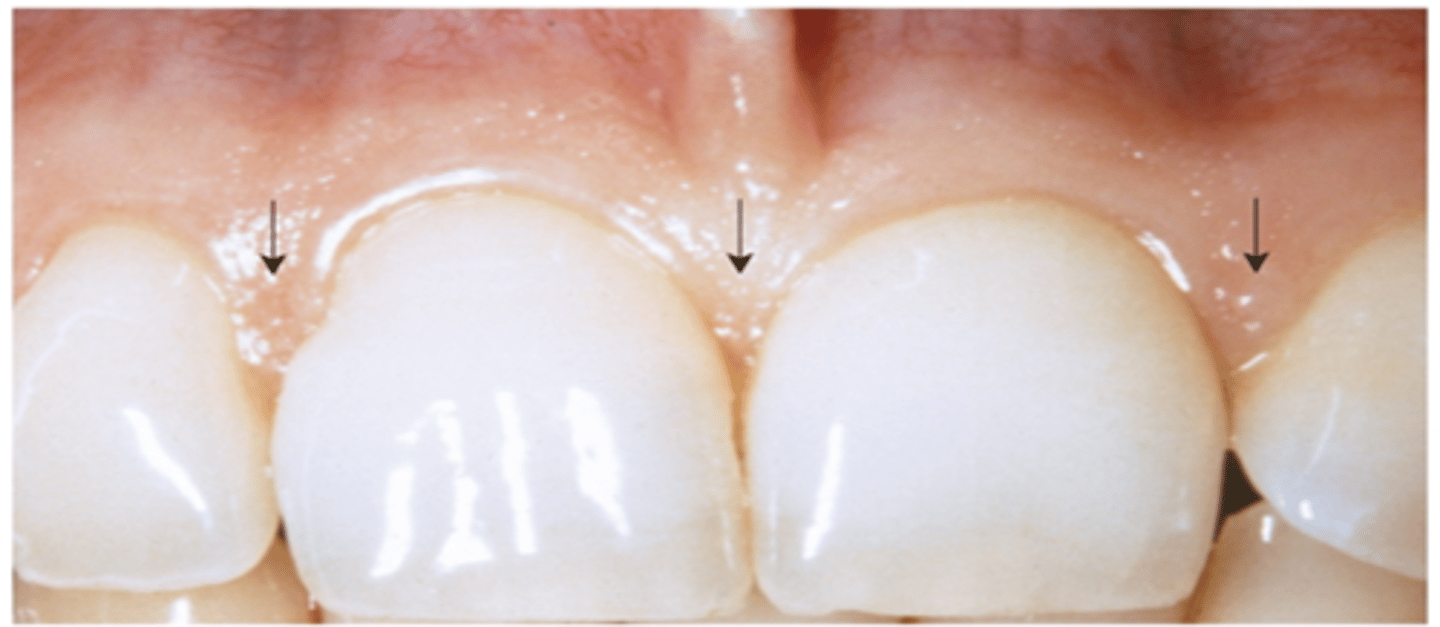
What is the free gingival margin?
thin, rounded edge where free gingiva meets the tooth. It follows a scalloped and curved contours of the underlying CEJ

The attached gingiva is tightly bound to: (2)
1. underlying cementum on the cervical-third of the root
2. Periosteum of alveolar bone
The attached gingiva is the widest at...? Why?
incisor and molar regions
b/c there is more mechanical stress at those teeth regions
The attached gingiva is the narrowest at...?
premolar regions
Pigmented attached gingiva may be due to:
1. increased production of melanin from melanocytes
2. health issues

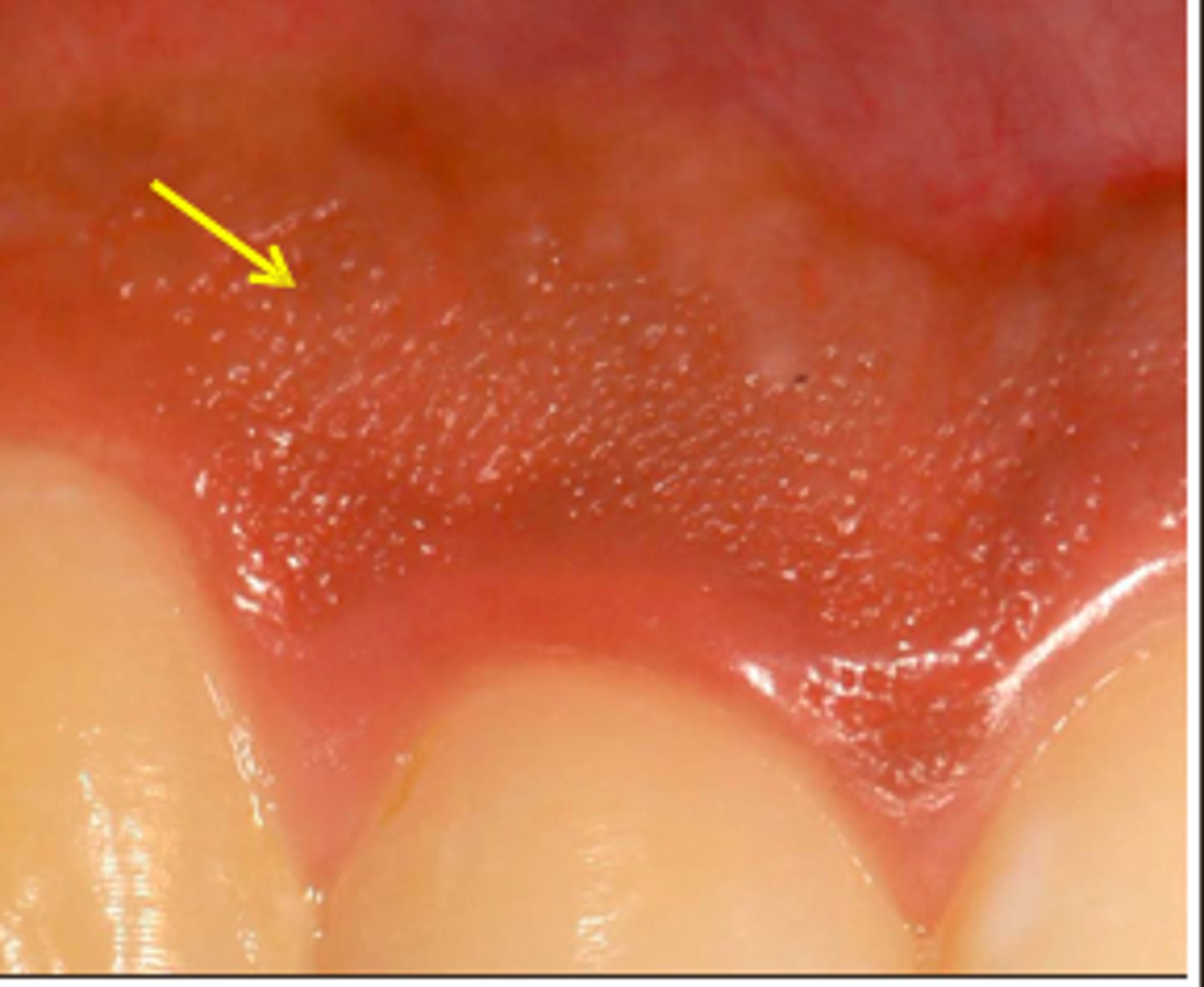
What causes the stippled texture of the attached gingiva/interdental gingiva?
Rete ridges - it increased surface area to anchor the oral epithelium to the deeper connective tissues
-locking the layers together allowing tissue to withstand more mechanical force
What prevents the free gingiva from being pulled apically from the tooth when tension is applied to the alveolar mucosa?
Attached gingiva
What are the 3 structures of the interdental gingiva?
1. facial papilla
2. lingual papilla
3. interdental col
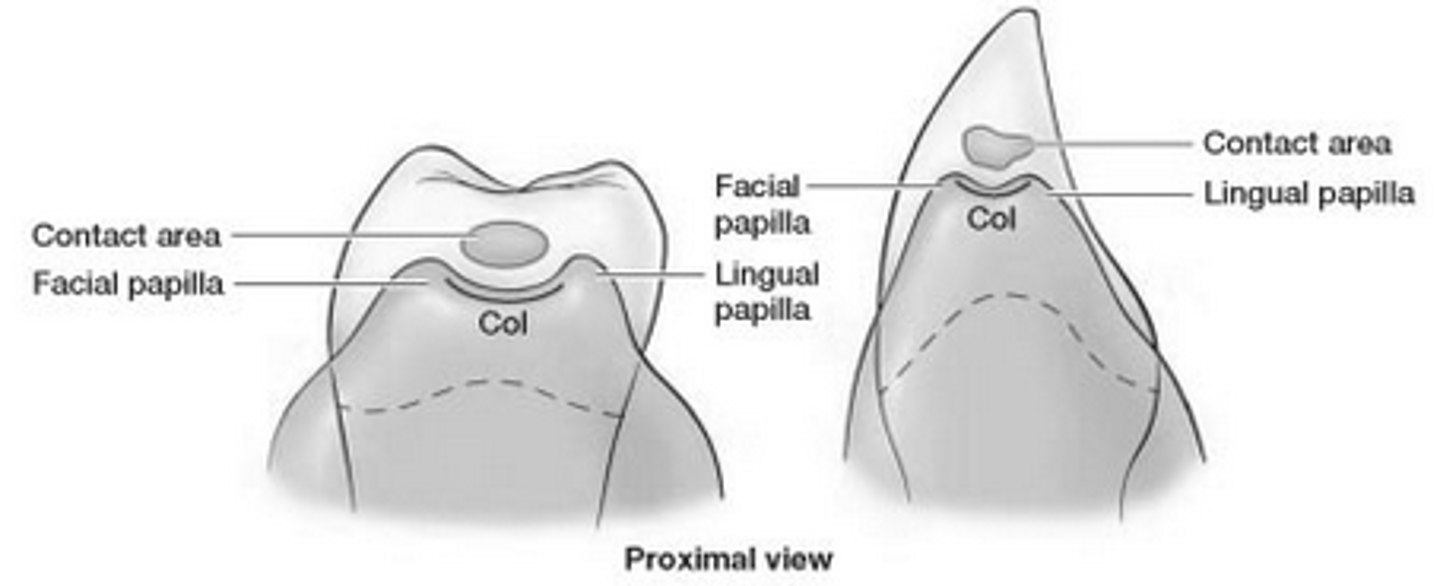
What is the function of the interdental gingiva?
prevents food from becoming packed between the teeth during mastication
When is the interdental col not present?
Interdental col is not present if there is large space between 2 teeth or if there is notable gingival recession
the gingival sulcus is filled with?
gingival crevicular fluid (GCF) that is secreted by near by connective tissue (lamina propria)
- contains inflammatory cells
- increased production when there is inflammation at the gums
- healthy sulcus do not have much GCF
What is the measurement for a clinically healthy gingival sulcus?
1-3 mm deep
at 4mm, the sulcus is considered a gingival pocket and it is a early sign of gum disease
Define Periodontal Ligament (PDL)
Periodontal ligament is composed of dense fibrous connective tissue that serves to connect the tooth to the alveolar process (tooth socket). It's main role is to support the tooth in the socket by absorbing mechanical loads placed on the tooth during mastication etc.
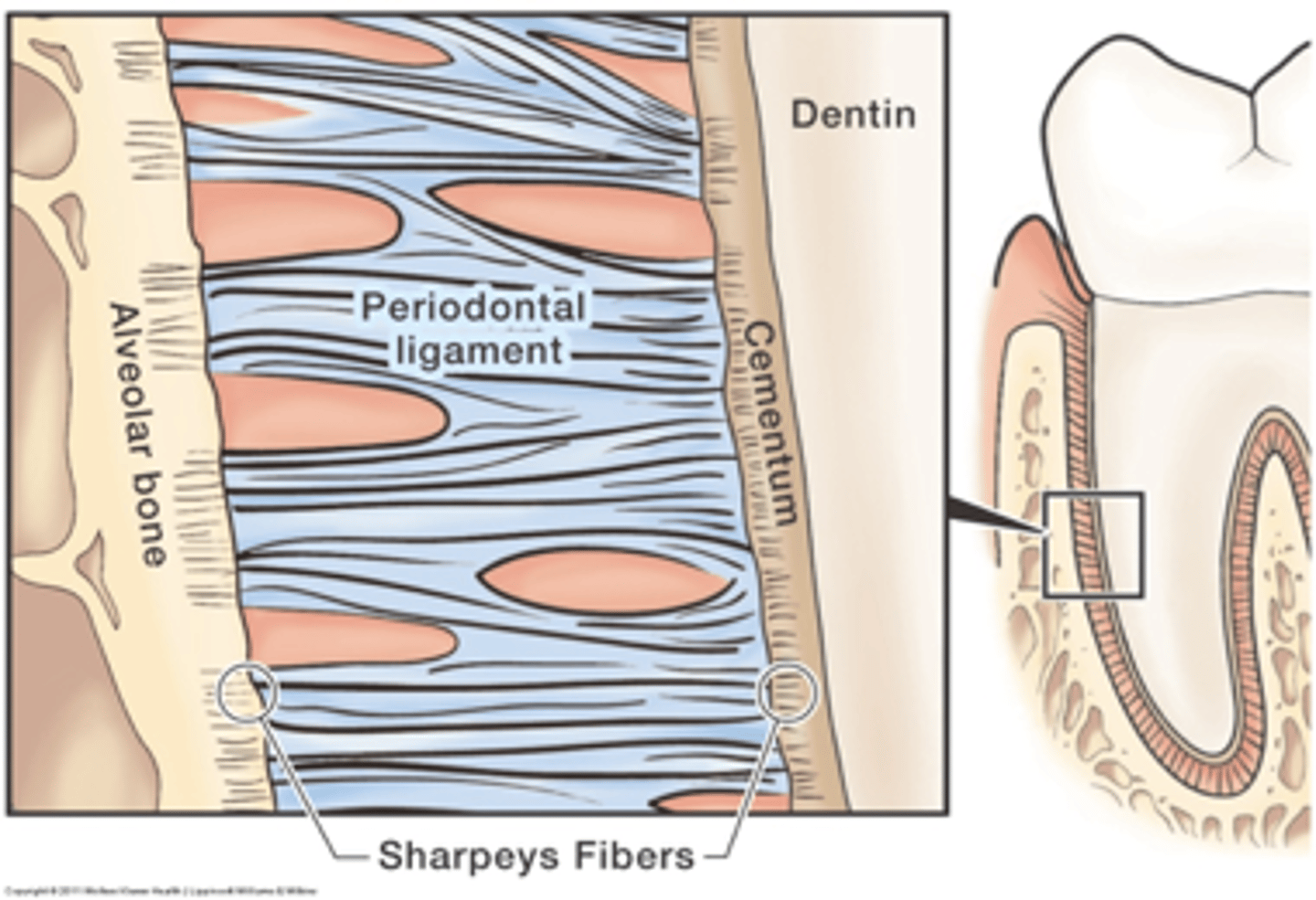
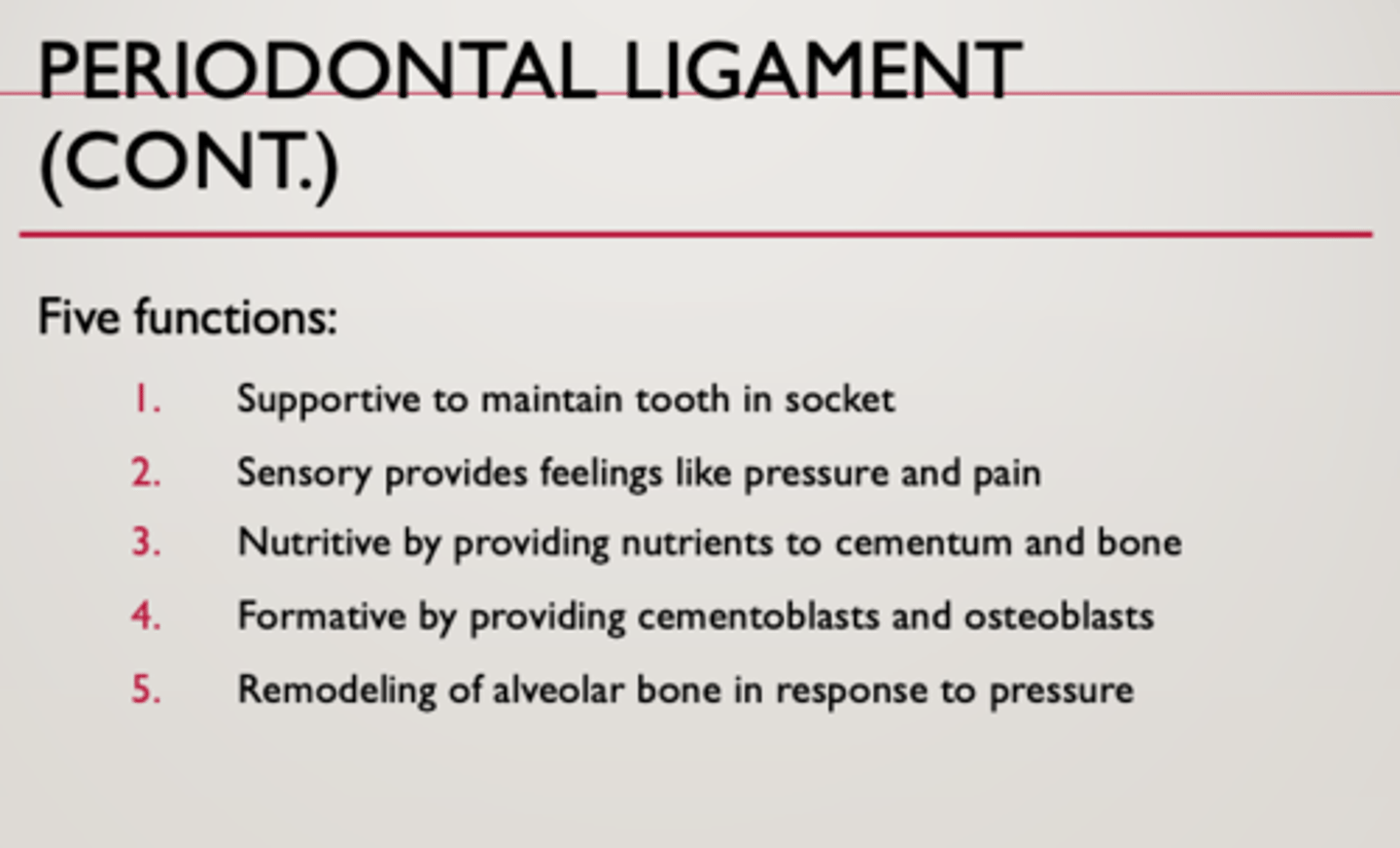
What are the 5 functions of the Periodontal Ligament?
1. Support - suspents and maintains tooth in socket, cushions forces
2. Sensory - has nerve endings that relay sensory information
3. Nutritive - has blood vessels that provide oxygen and nutrients to the periodontium
4. Formative - build and maintain (via cementoblasts) the cementum and may aid in periodontal regeneration
5. Remodelling - can remodel alveolar bone in response to pressure (via osteoblasts and osteoclasts)
What is the cementum?
Thin yellow layer of hard mineralized tissue that covers the surface of the root and overlies dentin.
- it is 55% organic, 45% inorganic material
- It is softer than dentin and enamel.

Why does the cementum make orthodontic treatment possible?
The cementum is resistant to resorption (break down of bone).
Which part of the cementum is acellular? cellular?
Acellular poetion: upper 2/3rds of root
Cellular portion: lower 1/3rd of the root
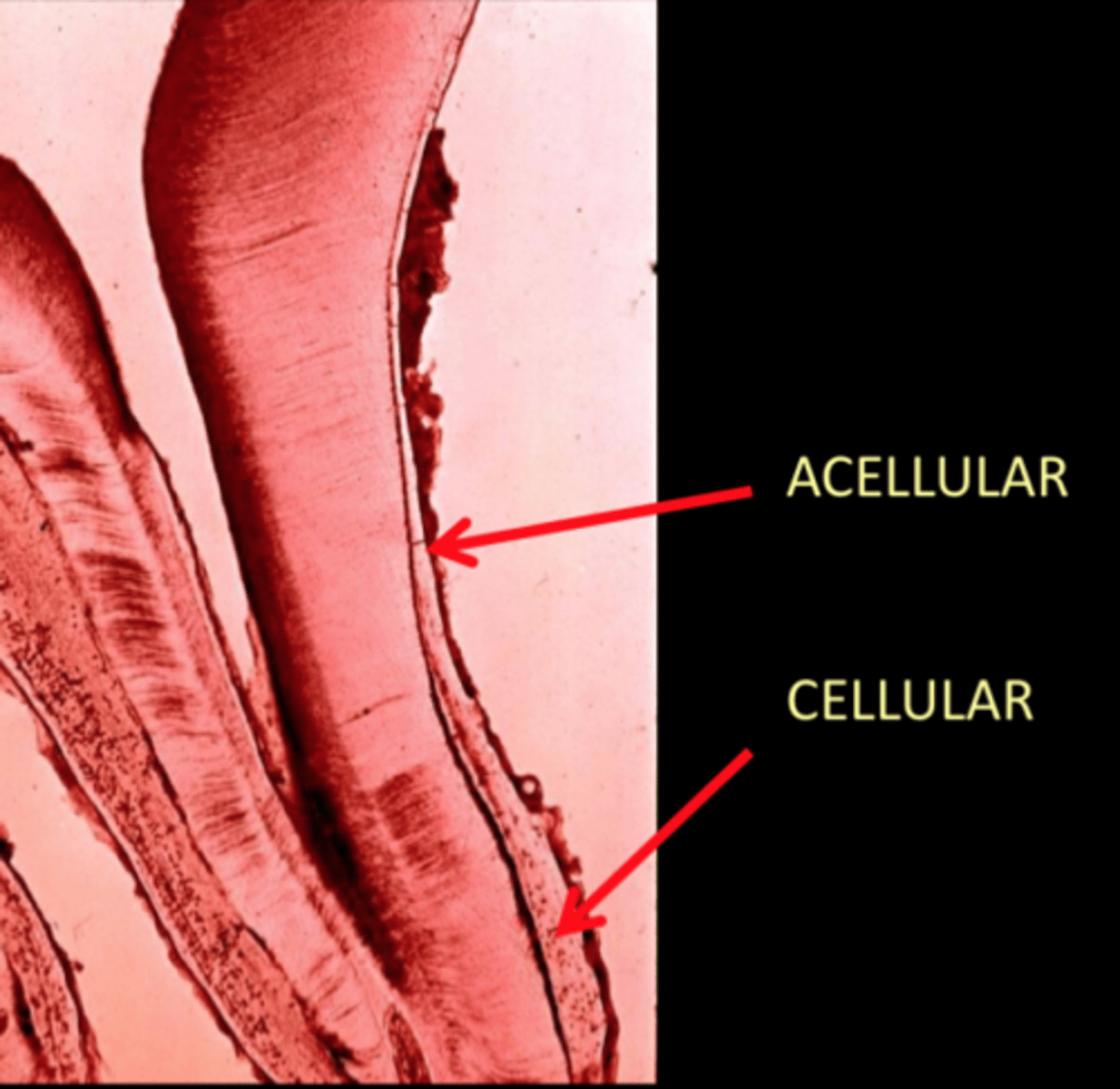
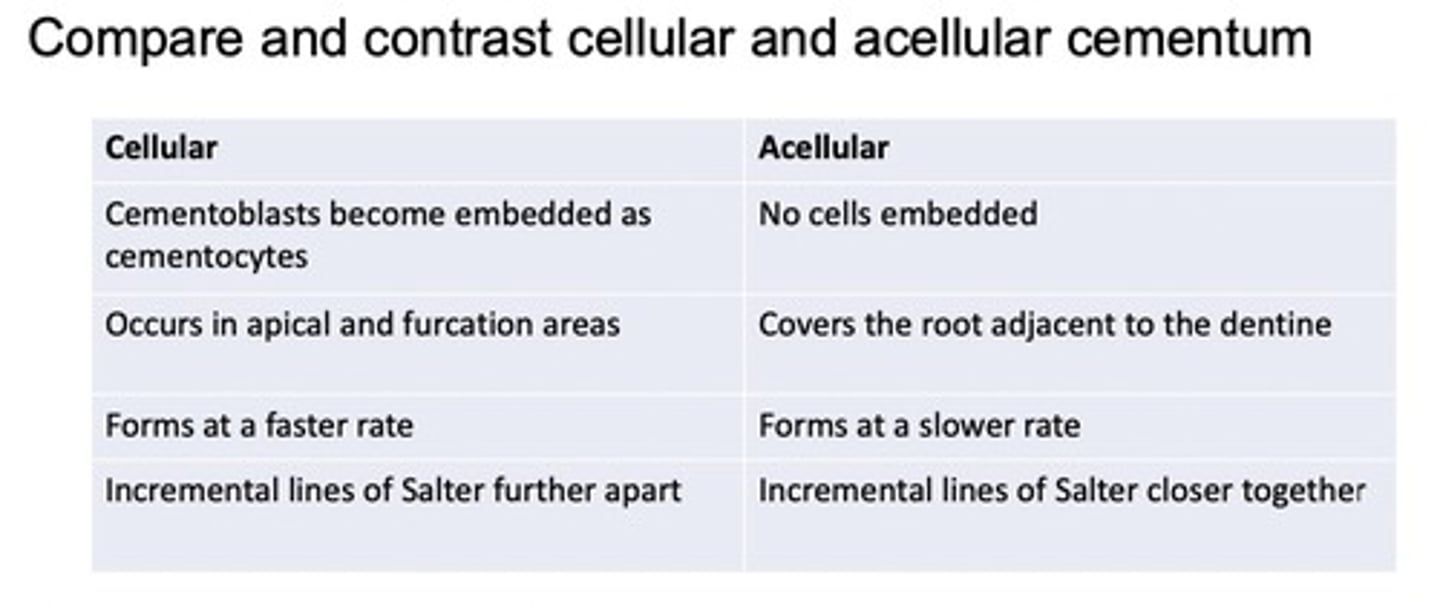
Compare and contrast the acellular and cellular cementum
Acellular:
- forms before teeth are in occlusion
- no cells
- covers 2/3rd of root
- plays important role in tooth support
Cellular:
- forms after the teeth have reached occlusion
- composed of cementocytes
- covers apical third of root
- compensates for active eruption and normal tooth wear by continuous deposition of cementum (cementum thicker as we age)
cementum is relatively permeable to
- extrinsic dyes
- organic substances
- inorganic ions
- bacteria
Cementum receives nutrients from
periodontal ligament {PDL)
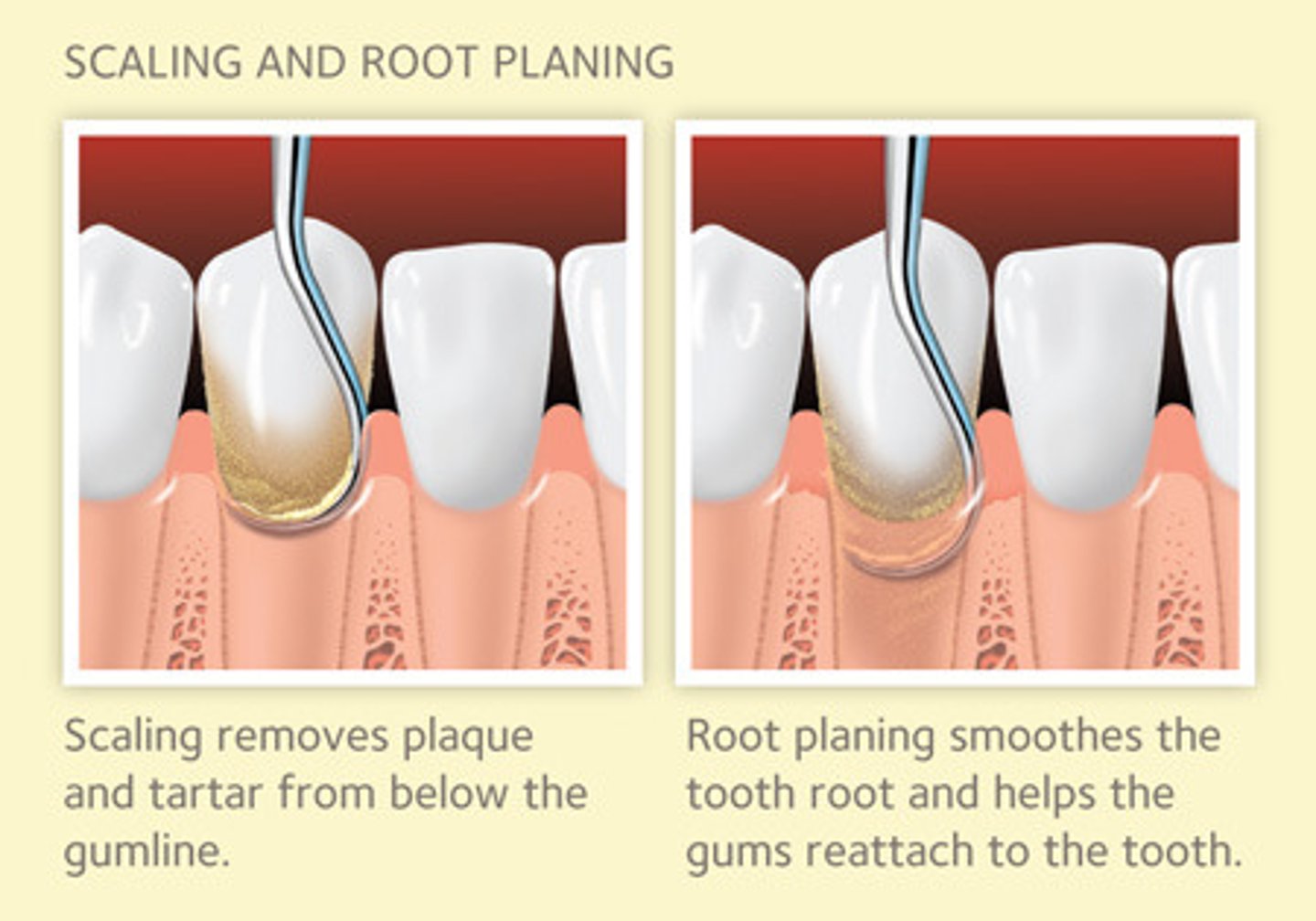
What is root planing?
Removal of the cementum on the exposed root surface
What are the 3 main functions of the cementum?
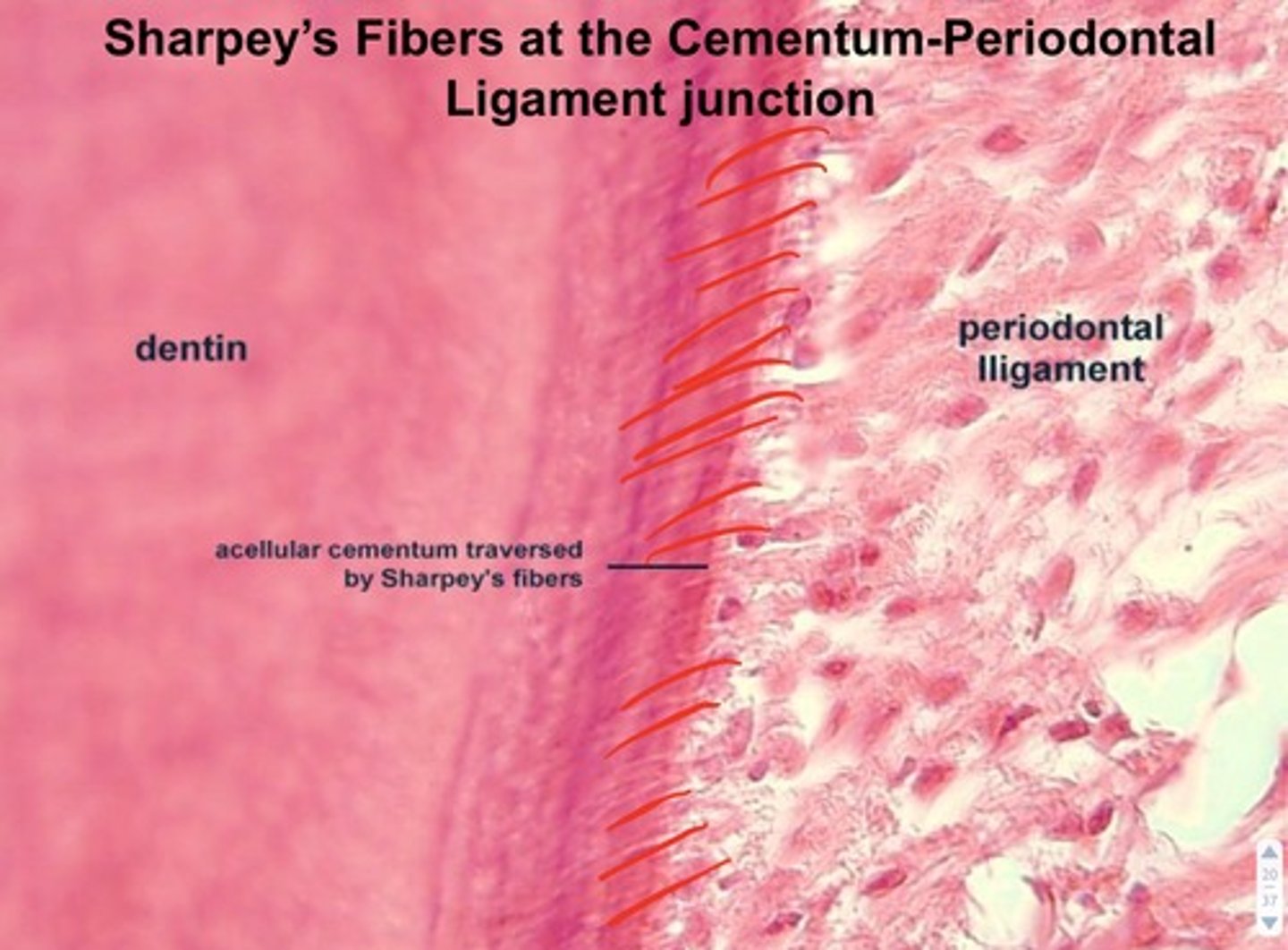
1. Attachment site for the periodontal ligament collagen fibres (terminal endings known as Sharpeys Fibers)
2. Protects underlying dentin and seals the ends of open dentinal tubules (pores in the dentin)
3. Compensates for tooth wear at occlusal or incisal surfaces due to attrition (reduced str b/c of sustained pressure)
What are Sharpeys fibers?
terminal collagen fibres from the periodontal ligament that attaches the PDl to the cementum.
What is the alveolar bone/alveolar process?
the portion of the upper (maxillary) or lower (mandibular) bones that surrounds the roots of the teeth
What are the characteristics of the alveolar process?
1. Mineralized connective tissue (60% inorganic, 25% organic, 15% water)
2. Existence is dependent on presence of teeth
3. Forms bony sockets that support and protect roots of teeth.
When does the alveolar process begin to resorb?
1. when teeth are extracted
2. when teeth do not erupt
** can also occur due to periodontal disease
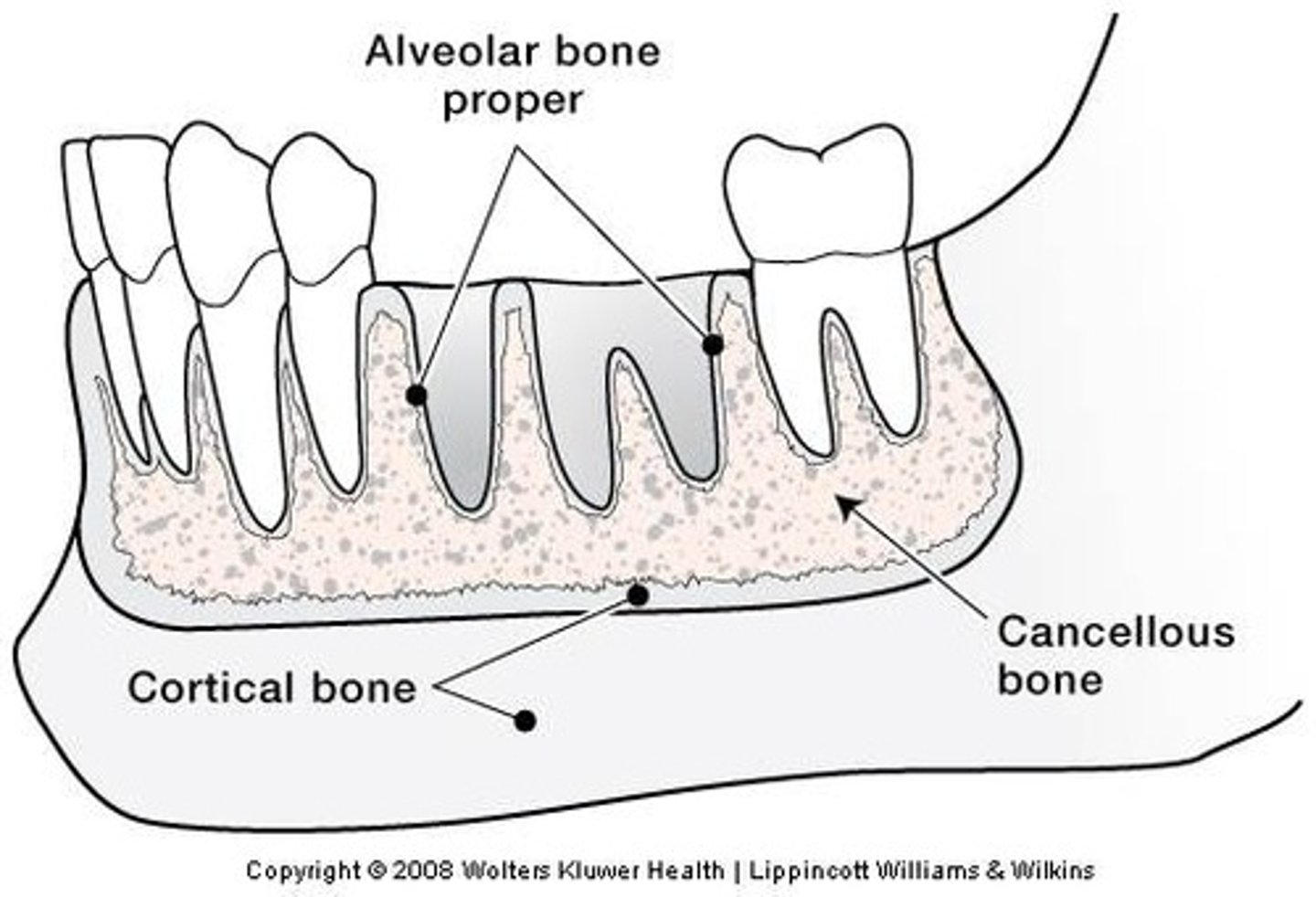
What are the 3 layers of the alveolar process?
1. alveolar bone proper
2. cortical bone
3. cancellous bone
What is another name for the alveolar bone proper?
Cribriform plate - because of its perforated nature so it resembles the cribriform plate also found in the ethmoid bone in the skull.
The thin layer of bone lining the tooth socket surrounding the root of the tooth is called?
Alveolar Bone Proper
What is found at the alveolar bone proper?
1. Alveolus (bone socket that houses the tooth
2. Alveolar Foramina -> for nerves
3. Sharpeys Fibres -> anchoring collagen fibres
When teeth are extracted, what do you see directly ?
Alveolar bone proper
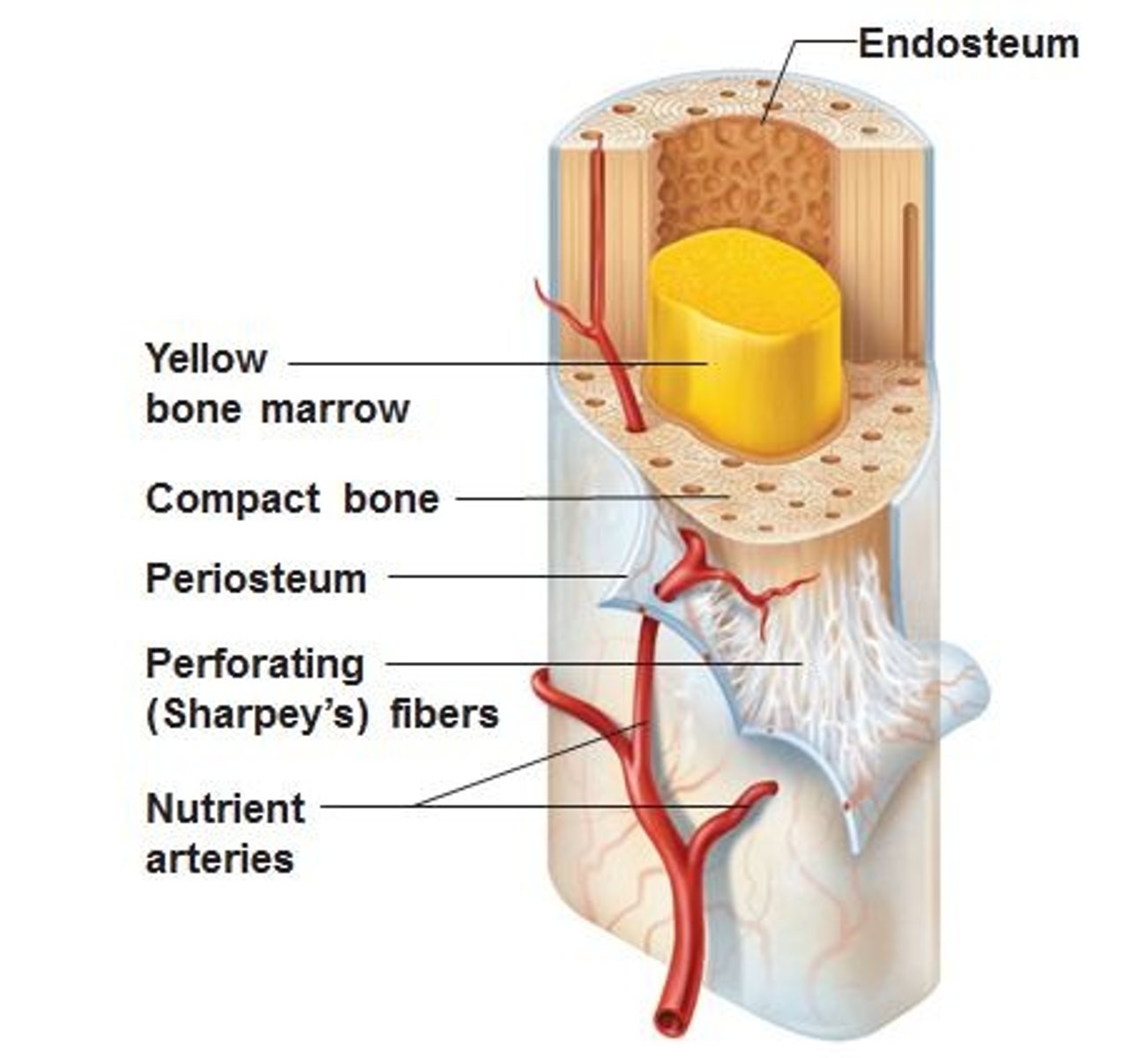
What is the cortical bone/cortical plate?
Layer of compact bone that forms the hard outer wall of the mandible and maxilla on the facial(buccal) and lingual aspects . It surrounds the alveolar bone proper and helps support the socket.
Where is the buccal cortical bone thinner/thicker?
- thinner at the incisor, canine and premolar region
- thicker at the molar regions
What is the alveolar crest?
the most coronal portion of alveolar bone found between teeth
What is cancellous bone? Where is it found?
Cancellous bone (spongy bone) fills the interior portion of the alveolar process (lattice-like appearance). It is found mostly in the interproximal areas (between teeth).
There is a higher proportion in the maxilla than in the mandible.
What is the Periosteum?
Layer of connective tissue covering outer surface of bone.