Tolerance and transplantation
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
Immunogen or tolerogen: (factors the favor immune vs tolerance response) [physical form, route of injection, dose of antigen]
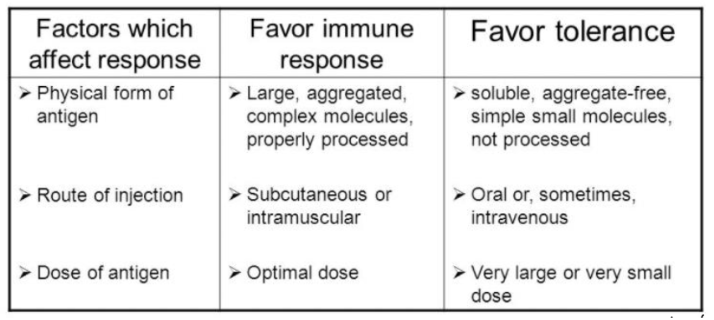
Tolerance is favored when: (2 reasons)
Lack of adjuvant
Long term persistence of antigen
Low level of costimulation
Central tolerance
deletion of lymphocytes with receptors that recognize self Ag before they mature during lymphocyte development: B cells bone marrow(bone marrow) ; T cells (thymic selection (affinity model, use of mTEC)
Issues with tolerance:
Leaky tolerance
reasons : not all self-Ag are expressed in central lymphoid organs, weakly reactive cells, genetic defects impact apoptosis
Peripheral Tolerance
Deletion, anergy, or induction of regulatory function in T cells recognizing self Ag
Treg cells [what are the molecules on the cell surface and]
Highly specific to an antigen
Molecules CD25+, CTLA-4 [it is present in most but higly active] (co-inhibitory molecule → decrease in proinflammatory molecules), IL-2R, FoxP3
How to get Treg
(central) Natural Treg = In the thymic selection →
(peripheral) Induced Th = cytokines like TGF-B and IL-2 switch helper into T reg cells
Function of Treg: (inhibitory cytokines & bystander suppression)
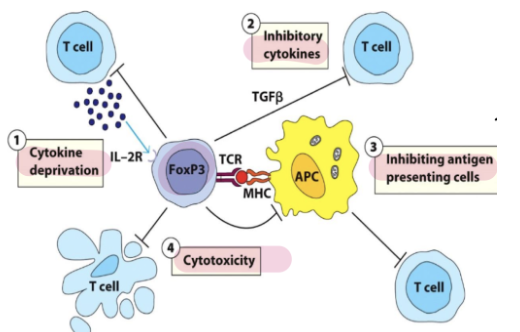
Treg interacts with APC’s Ag-MHCII complex it can down regulate other helper t cells on the APC surface
Cytolysis: Perforin, granzyme, FasL
B regulatory cells [what do they secrete]
Secrete IL-10, IL-35, TGf-
Turn on Treg
Engagement w/ Th17 cells can downregulate their function
Myeloid derived suppressor cells
Immature group of myeloid cells (granulocytes and monocytes)
They are producing inhibitory cytokines
In the case of cancers it shows down antitumor t cells —> poor prognosis
Methods of Tolerance for specific sites in the bidy {3 reasons}
Antigen sequestration
Lack of lymphatic drainage (anterior and lens of eye)
Ags are isolated from interaction w/ immune cells
Restricted immune entry : blood brain barrier (stromal cells line blood vessels)
Limited immune cells present
Few immune cells (cornea)
Immune tolerance in pregnancy [3 exmaples]
Palceneta = immunological barrier
Separate blood systems
T reg
Syncytium = fused placental cells so no immune cells or maternal blood can enter
Syncytium
fused placental cells so no immune cells or maternal blood can enter
Types of Transplantation:
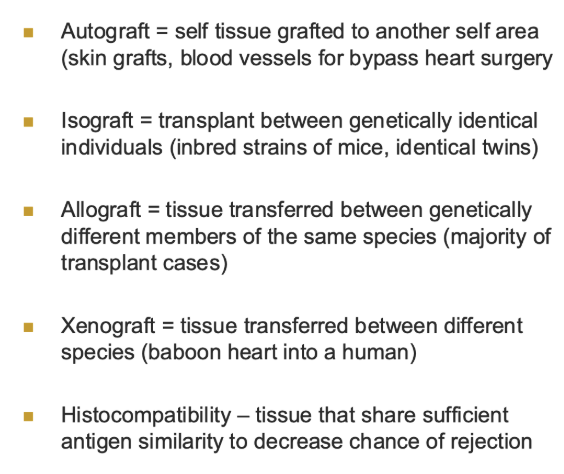
Xenotransplantation:
Testes and kidney survived in humans from chimpanzee
Matching in transplantation:
Blood group Ag difference = most intense graft rejections
MHC compatibility (parents and siblings are first choice
Cross matching = blood test → circulating Abs especially to HLA
Anti rejection drugs
allow organ transplants between completely mismatched people
Luminex bead-based screening assays
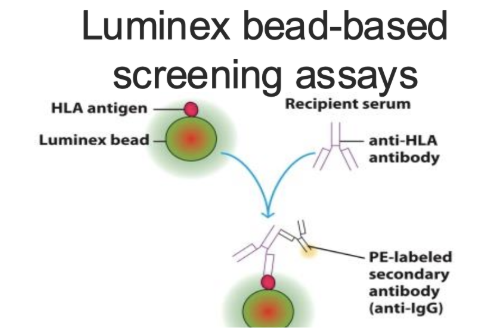
unique HLA antigen on each bead, then detect fluorescent marker for what specific bead it is
MHC/HLA compatibility
Siblings have a 25%
chance of MHC identity
Parent-to-child grafts
have a 50% MHC match(they get one allele from each parent)
Certain organs have higher rate os success: [and then certain combos]
Cornea transplant are successful bc they are immune privileged
Certain combinations of organs increase the odds of success
Heart and lung
Kidney and pancreas
Rejection first and second set (why. isthis faster):
First set = 12-14 days memory of the anti-graft response is generated
Second set rejection = occurs much faster due to memory from prior graft → necrosis
Hyperacute
rejection by preexisting antibodies
Occurs before grafted tissue revascularizes
Preexisting antibodies bind to graft cells and activate complement and ADCC
Acute rejection (what are the two stages)
mediated by T cell response ; 7-10 days [the T cells have not seen the antigen in this T cell before]
Sensitization stage
APC present Ag
T cells activate and proliferate
T cell expansion and Memory t Cells are created
Effector stage:
Immune cells into graft tissue
Inflammatory cytokines and cell-damaging chemicals
Antibody production
Do memory T cell still require APCs to activate
Yes but they dont require a storng costimulatory signal or as much antigen
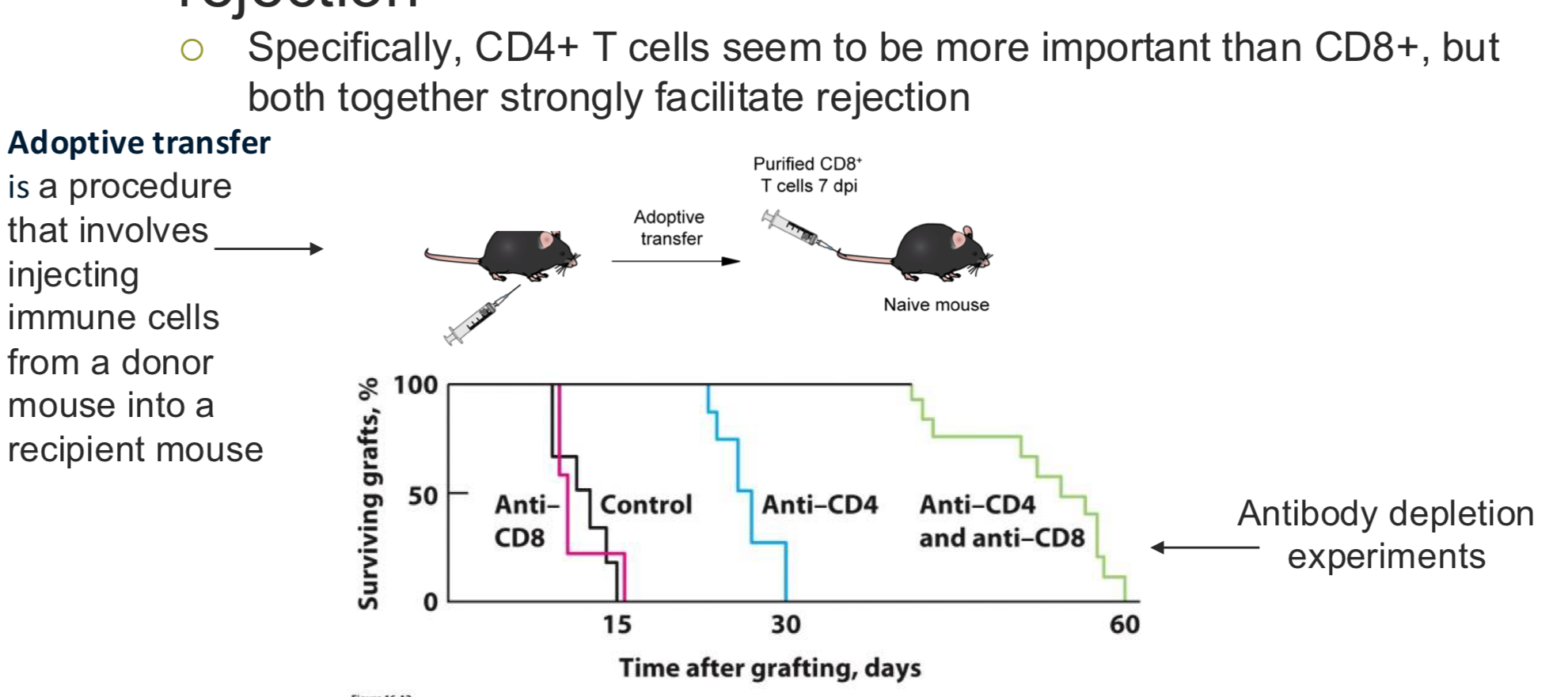
Adoptive transfer and t cell neutralization experiments (what is the experiment)
t cells mediate graft rejection = CD 4 more important than 8 but 8 is important too
Adoptive transfer: take T cells from one mice and give it to another increasing the number of t cells and see how this would cause a response to the graft
Antibody depletion experiment : add antibodies that target the helper cells and deplete the t cellsChronic rejection: with phagocytosis, degranulation
Chronic rejection:
Months-years later
Antirejection med not effective
Humoral and cell-mediated response
Graft versus host disease (GVHD)
Immune cells donate organ expand and attack recipient
General immunosuppressive therapy - irradiation {what could it treat}
Irradiation of lymphoid regions to eliminate lymphocytes; wipe out recipient immune cells and add new immune cells → used to treat graft vs host disease and cancer
General immunosuppressive therapies
Specific immunosuppressive therapies [blocking T cell function]
mABs
Basiliximab: mAB to cd 25
Cd 25 is a subunit to IL-2r
Rituximab: mAb to CD20 on B cells
• mAb binding leads to cell death
Belatacept
soluble CTLA-4 protein → T cell anergy, used in kidney transplantation
Problems w/ immunosuppression
Drug toxicity
Increased infections
Increased endogenous viral infections (dormant infections) Bk polyomavirus → target graft