CMPP: Hemolytic Anemia 1
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
95 Terms
Hemolytic anemia
disorders that are characterized by the premature destruction of RBCs
reticulocytosis
one should consider hemolysis in all anemic patients with...
cause of hemolysis
location of hemolysis
hemolytic anemias are characterized by...
Intracorpuscular
hemolytic anemia that is caused by something being wrong with the actual RBC; almost always HEREDITARY!
enzymopathy (G6PD)
hemoglobinopathy (sickle cell, alpha/beta thalassemia)
membranopathy (hereditary spherocytosis)
causes of intracorpuscular hemolytic anemia
hereditary
intracorpuscular hemolytic anemia is almost always...
Extracorpuscular
external force is acting upon the cell, causing hemolysis; ACQUIRED!
mechanical injury
infection
immunologic
medications
stasis
causes of extracorpuscular hemolytic anemia
Intravascular hemolysis
hemolysis within systemic circulation; RBC intracellular contents are released into plasma; excess intracellular components produce specific symptoms
Hemoglobinemia
free hemoglobin is released into the plasma and can cause significant tissue damage; the body works quickly to remove it; causes the plasma to be PINK!
Haptoglobin
removes free hemoglobin from the body
there is only a finite amount of Hp in the body, so it is not freely present in the blood because it is being consumed by the large amount of intravascular hemolysis
why are plasma haptoglobin levels decreased/absent in those with intravascular hemolysis?
renal filtration -- glomerulus filters small alpha-beta globulins
once haptoglobin is overwhelmed, how does Hgb get filtered out?
hemoglobinuria and kidney damage
renal filtration of hemoglobin results in...
after urine is centrifuged, if the supernatant is...
clear = hematuria
red/pink = hemoglobinuria
how can one tell the difference between hematuria and hemoglobinuria
elevated, high (these are byproducts of intravascular hemolysis)
in the lab work for someone going through intravascular hemolysis, unconjugated bili is ______, and LDH is _____
Reticuloendothelial system
extravascular hemolysis; hemolysis is taking place inside macrophages and monocytes; very little hemoglobin escapes into the plasma; Hp would be normal or slightly decreased
jaundice and splenomegaly
in extravascular hemolysis, since heme is broken down within macrophages in the spleen/liver, what symptoms would be more likely to be present?
CBC
reticulocytes
peripheral smear
CMP
unconjugated bili
LDH
haptoglobin
urinanalysis
what tests should be ordered in one with a suspected hemolytic anemia
presence/absence of antigens on the blood cell membrane (e.g. type B blood have B antigens on their surface)
blood type is designated by the...
Direct COOMBS
if hemolysis is supported by initial workup but its cause is unknown, start with...
Direct COOMBS
detects if antibodies (or complement) are bound to the RBC surface antigens; antibodies should NOT be bound to RBC surface, presence indicates the cause of hemolysis
draw blood
add coombs reagent
monitor for agglutination
how to perform a direct coombs test
antibodies/complement are causing hemolysis
if agglutination occurs in a direct coombs test, what does that mean?
effectively rules out autoimmune hemolytic anemia
if agglutination does not occur in a direct coombs test, what does that mean?
G6PD deficiency
what is the most common enzymatic disorder of RBCs?
G6PD deficiency
genetic defect that results in decreased enzyme glucose 6-phosphate dehydrogenase; indirectly allows for premature RBC hemolysis
both!
in G6PD deficiency, is hemolysis extra or intravascular?
X-linked recessive
--> males will be hemizygous (all RBCs affected)
--> females are often heterozygous (1/2 RBCs affected)
in G6PD deficiency, it is an ________ trait. How does this differ how this presents in men vs women?
malaria (thought to provide advantage against malaria infection)
G^PD deficiency is more prevalent in areas that ________ infections are prevalent
G6PD
enzyme found in all normal RBCs that protects them against free radicals; activity of this enzyme diminishes as RBCs age, and low levels of this enzyme makes RBCs more susceptible to oxidation injury and destruction
reticulocytes
what blood cells have the highest G6PD activity?
yes! they make some, just much less than normal
do patients with G6PD have any G6PD?
methemoglobin (Fe3+), insoluble masses, rigid, inflexible, prone to destruction
when exposed to oxidative stress, hemoglobin is oxidized and becomes ________, and this further denatures into _________ that attach to the red cell membrane. This makes the RBCS ______ and ______ and _________________.
Heinz bodies
round denatured hemoglobin inclusions that are bound to cell membrane; sign that RBC was exposed to oxidation
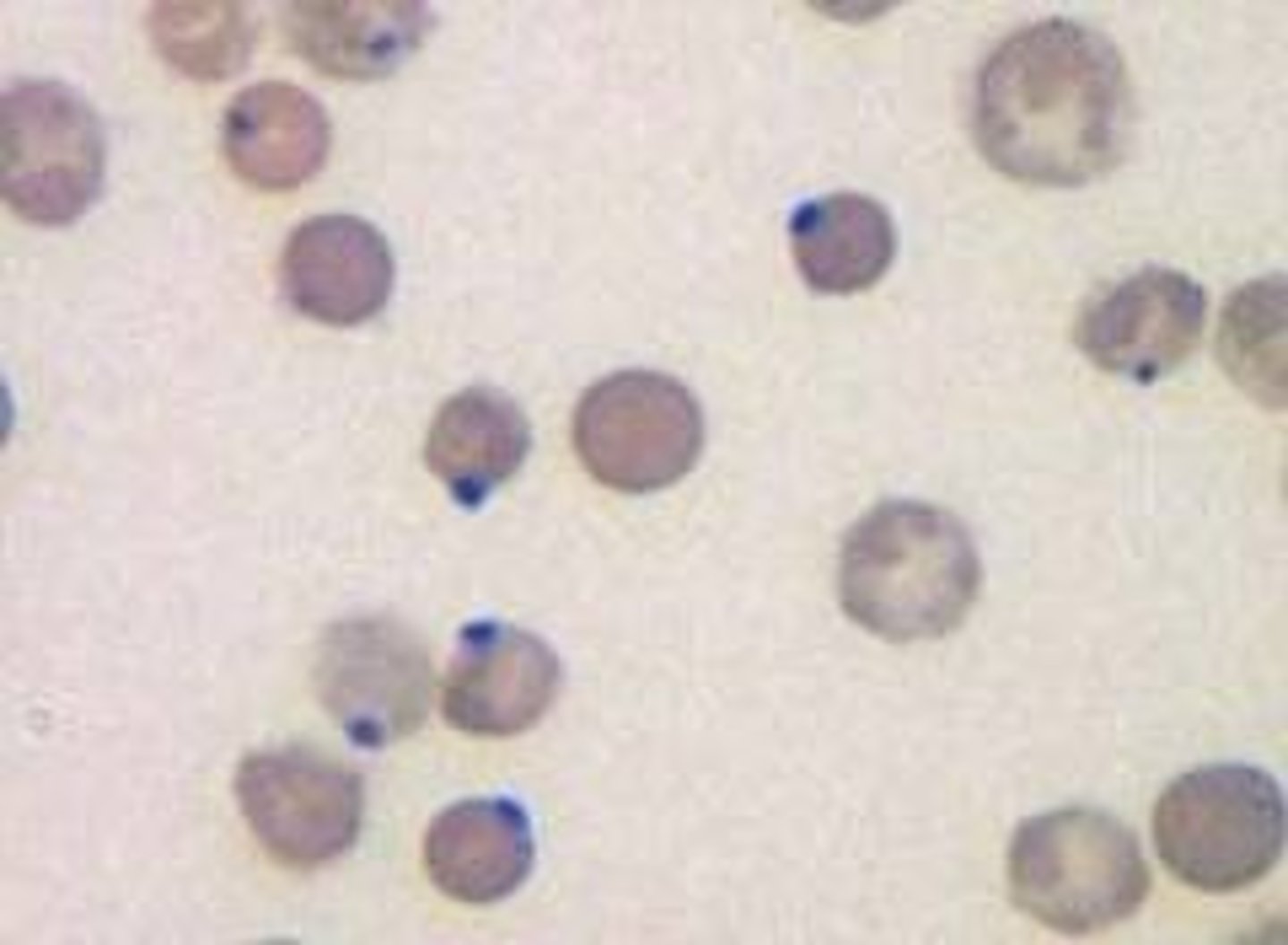
Bite cells
macrophages recognize that Heinz bodies are abnormal, so they "bite" the denatured Hb out of the cell; results in RBCs with semicircular portions removed
infection
medications
food exposure
chemical exposure
what causes oxidative stress?
infection
what is considered the most likely cause of hemolysis in G6PD-deficient individuals
fluoroquinolones
methylene blue
nalidixic acid
nitrofurantoin, nifuratel, nitrofurzone
phenazopyridine
primaquine and tafenoquine
rasburicase and pegloticase
sulfonylureas
what medications are indicated in precipitating hemolysis in G6PD deficient patients?
fava beans
henna compounds
naphthalene (mothballs, lavatory deodorant)
RUSH (isobutylene nitrate, amyl nitrate) -- sexual enhancement drug
what foods are indicated in precipitating hemolysis in G6PD deficient patients?
Favism
subset of G6PD deficiency that occurs following ingestion of fresh fava beans; occurs mostly in children; can cause acute intravascular hemolysis; not all patients with G6PD deficiency will have this
acute intravascular hemolysis
favism causes...
hemolyze, hemoglobin, reticulocytosis
after an oxidative stressor, G6PD deficiency cells _______ but cells with sufficient G6PD survive. This leads to a rapid drop in _________, and the body responds by producing new RBCs (____________).
8 days
acute hemolytic process lasts approx...
jaundice/icterus
pallor
dark urine
hyperbillirubinemia
abdomen/back pain
what is a common presentation of a G6PD deficiency pt within 24 hours of exposure to oxidative stressor?
abrupt drop in Hb
increased reticulocyte count
Bite cells/Heinz bodies on peripheral smear
what is seen in labs for those with G6PD deficiency?
education -- avoid foods, meds, chemicals known to cause oxidative stress
prophylactic folic acid supplement
treatment of G6PD deficiency
hydration, but not too much
blood transfusion if hemodynamically unstable
splenectomy is typically ineffective
how to treat acute anemia in G6PD deficiency
Hereditary spherocytosis
what is the most common cause of hemolytic anemia due to a red cell membrane defect?
Hereditary spherocytosis
autosomal dominant genetic defect that affects the proteins involved in the cytoskeleton and cell membrane of the RBC; results in spherocytosis and hemolysis
cytoskeleton and membrane of the RBCs
in HS, there is a mutation within the...
Cytoskeleton
the microscopic network of proteins inside living cells which gives it its shape and flexibility
flexible
Normal RBCs are ________ and are able to travel through capillaries and splenic sinusoids.
swell, shrink
Normal RBCs can change their shape in response to the tonicity of its environment. They _______ in response to a hypotonic environment, and _______ in response to a hypertonic environment.
Band 3
Ankyrin
Spectrin
HS results from gene mutations that code for...
weak
in HS, genetic mutations cause defects in the RBC membrane that causes it to become...
blebs to form on RBC surface
K+/H2O exit the cell
Cells become dehydrated
RBC changes shape (spherocyte)
a weak RBC membrane can cause...
Spherocyte
round RBC (NOT biconcave); no central pallor; decreased surface area and flexibility
RBC gets stuck in splenic sinusoids, and macrophages identify and phagocytize the spherocytes
what happens when extravascular hemolysis occurs in those with hereditary spherocytosis?
this process occurs because RBCs are less likely to survive in unfriendly environments -- spontaneously lyse/hemolyze
--> acidic stressors, oxidative stressors, metabolically unfavorable conditions
what happens when intravascular hemolysis occurs in those with hereditary spherocytosis?
repeated hemolysis gets rid of nutrients needed to produce effective RBCs
--> iron, folate, and B12 deficiencies
why does hereditary spherocytosis lead to nutritional deficiencies?
anemia can worsen as volume expansion occurs throughout pregnancy
why does hereditary spherocytosis become more complicated during pregnancy?
parvovirus B19
in hereditary spherocytosis, aplastic crisis can occur with infections. it is very common with what pathogens?
splenic pooling of RBCs and increased hemolysis
--> EBV, Hepatitis, cirrhosis
in one with hereditary spherocytosis, conditions that cause splenomegaly can cause...
splenomegaly (VERY COMMON)
jaundice
hyperbilirubinemia
hemoglobinuria
hemogloinemia
cholelithiasis
what are some common symptoms of hereditary spherocytosis?
Gallstones are PIGMENTED and radiopaque -- can be seen on XR
--> unconjugated bili from hemolysis combines with calcium
what is unique about the cholelithiasis that occurs in hereditary spherocytosis?
microcytic anemia
elevated MCHC (hyperchromic)
Elevated RDW
Pseudohyperkalemia
what are some unique lab values associated with hereditary spherocytosis?
there is membrane loss and red cell dehydration, so, since that membrane is lost, more cell is taken up by Hgb due to a smaller size
why is MCHC elevated in those with hereditary spherocytosis?
varied cells are being affected with bulging
why is RDW elevated in hereditary spherocytosis?
K+ leaking out of a faulty membrane
why is pseudohyperkalemia seen with hereditary spherocytosis?
round cells without central pallor
hyper chromic cells
--> these results alone are NOT diagnostic for hereditary spherocytosis
what is seen on peripheral smear in those with hereditary spherocytosis?
NEGATIVE, since antibodies are not responsible for the hemolysis
what are the direct coombs results in one with hereditary spherocytosis?
Eosin-5'-maleimide (EMA) binding test
confirmatory test of choice for hereditary spherocytosis; dye (EMA) binds RBC membrane proteins; flow cytometry is used to measure labeled RBCs
decreased -- as they lack the mabrane proteins/membrane isn't as strong
EMA labeled RBC levels will be ______ in patients with HS
Osmotic fragility test
test RBC ability to respond to tonicity; adds patient RBC to hypotonic solution and sees how it tolerates it; relatively low sensitivity/specificity
expand and swell, burst
in the osmotic fragility test, normal RBCS ______________, spherocytes will _____.
folic acid -- prophylactic supplementation due to increased use (hemolysis)
blood transfusion -- based on severity
EPO -- corrects anemia (but not cell shape)
splenectomy -- reserved for SEVERE cases, effective in improving anemia/hemolysis
treatment for hereditary spherocytosis
children, but discontinued as bone marrow picks up
EPO supplementation is primarily used in what age group?
age 6
a splenectomy to treat HS is delayed until a child is older than...
PCV20
H flu type B
Meningitis A/B
Flu
COVID
what vaccinations should be given prior to a splenectomy?
if gallstones are present
when would a cholecystectomy be performed in one with HS?
Paroxysmal nocturnal hemoglobinuria
acquired chronic hemolytic anemia; mutation (PIG-A) results in a defect of myeloid stem cells; defect leads to recurrent episodes of hemolysis that occurs mainly at night; occurs in 3rd-4th decade of life; associated with aplastic anemia, iron deficient anemia, myeloid leukemia/myelodysplasia
PIG-A, myeloid stem cells
Paroxysmal nocturnal hemoglobinuria results from a mutation in what gene that affects what types of stem cells?
hemolysis and concentration of urine is happening anyway (usually happens at night), so buildup is more noticeable in the morning
why does Paroxysmal nocturnal hemoglobinuria mainly occur at night?
PIG-A gene
gene essential for production anchor proteins (CD55/CD59) in the RBC membrane
deterring complement activation
CD55/CD59 are responsible for...
fatigue, dyspnea, hemoglobinuria
abdominal/muscular pain
thrombosis or peripheral AND ABDOMINAL/CEREBRAL VEINS
presentation of paroxysmal nocturnal hemoglobinuria
normocytic, normochromic, pancytopenia with reticulocytosis
also contains products indicative of hemolysis (LDH, absent haptoglobin, elevated unconjugated bili)
what are the findings on labs for one paroxysmal nocturnal hemoglobinuria
flow cytometry
what test is needed for diagnosis of paroxysmal nocturnal hemoglobinuria
RBCs lack CD55/CD59 anchored proteins
what does flow cytometry show in one with paroxysmal nocturnal hemoglobinuria
C5 complement inhibitors
treatment for paroxysmal nocturnal hemoglobinuria
eculizumab (Soliris)
ravulizumab (Ultomiris)
C5 complement inhibitor agents
anticoagulants if thrombosis is present
what should be given in conjunction to those with PNH on C5 complement inhibitors
N. meningitidis
treatment of PNH using C5 complement inhibitors increases the risk of what condition?
Meningococcal vaccines (both MenA/B)
Antibiotic prophylaxis (Pen V)
patients on C5 complement inhibitors should receive what to help decrease their risk of N. meningitidis