Nutrition
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
Optimal Nutritional Status
Sufficient nutrients for daily needs and increased demands; supports long, active life.
At-Risk Groups (Undernutrition)
Infants, children, pregnant women, immigrants, low income, hospitalized, aging adults.
Overnutrition Causes
Excess calories, fat, sodium; exceeds metabolic needs.
Overnutrition Complications
Obesity, heart disease, diabetes, hypertension, stroke, gallbladder disease, sleep apnea, cancer, osteoarthritis.
Infant Nutrition (0–2 yrs)
Breastfeed 1st year, avoid cow’s milk <1 yr, provide adequate fat/calories.
Picky Teen Nutrition Advice
Healthy, protein-rich snacks; avoid fad diets; educate on nutrition.
Social Media Impact
Promotes unrealistic body ideals; increases obesity risk; affects body image.
Metabolic Syndrome Factors
3 of 5: high BP, high glucose, high triglycerides, large waist, low HDL.
Dysphagia
Swallowing difficulty; leads to malnutrition/dehydration/aspiration risk.
Older Adult Nutrition Factors
Poor health, dysphagia, isolation, limited income, mobility issues, polypharmacy.
Physiologic Changes in Older Adults
Poor dentition, reduced taste/smell, decreased GI absorption, muscle loss, fat gain.
Socioeconomic Challenges for Older Adults
Low income, limited support, difficulty shopping/cooking.
Immigrant Nutrition Challenges
Limited reserves, unfamiliar foods, adapting to U.S. diet.
Mini-Nutritional Assessment (MNA)
Quick tool for older adults in long-term care/community settings.
Poor Nutrition Effects
Slower wound healing, higher fall risk, longer hospital stays, pressure injuries.
Most significant lab for Nutrition
Albumin; low = protein-calorie malnutrition.
Food Frequency Questionnaire
Tracks food intake frequency; better than 24-hr recall for patterns.
Food Diaries
3-day record; useful for erratic eating; must record immediately.
Choose My Plate / USDA Guidelines
Visual and practical guidance for healthy diet and chronic disease prevention.
Usual Weight
Detect unintentional loss/gain; baseline for BMI.
Changes in Appetite/Taste/Swallowing
May indicate illness, medication effects, or malnutrition.
Chronic Illness Risk
Diabetes, pancreatitis, malabsorption, cancer, kidney disease.
Medication Impact
Can affect absorption; supplements/herbals may be harmful.
Parental Interventions
Small portions, healthy snacks, repeated exposure, avoid pressure.
Adolescent Weight Perception
Assess perception to prevent eating disorders; ensure nutrient intake.
Low Albumin
Indicates poor protein intake/malnutrition; affects healing and immunity.
Anthropometric Measures
Weight, height, BMI, waist-hip ratio, skinfold, arm span.
BMI
Height + weight; >30 = obesity, >40 = morbid obesity.
Malnutrition Severity
Current ÷ usual weight ×100; 85–95% = mild, 75–84% = moderate, <75% = severe.
Significant Weight Loss
5% 1 month, >7.5% 3 months, >10% 6 months.
Waist-to-Hip Ratio
Fat distribution; >1 men, >0.8 women = higher disease risk.
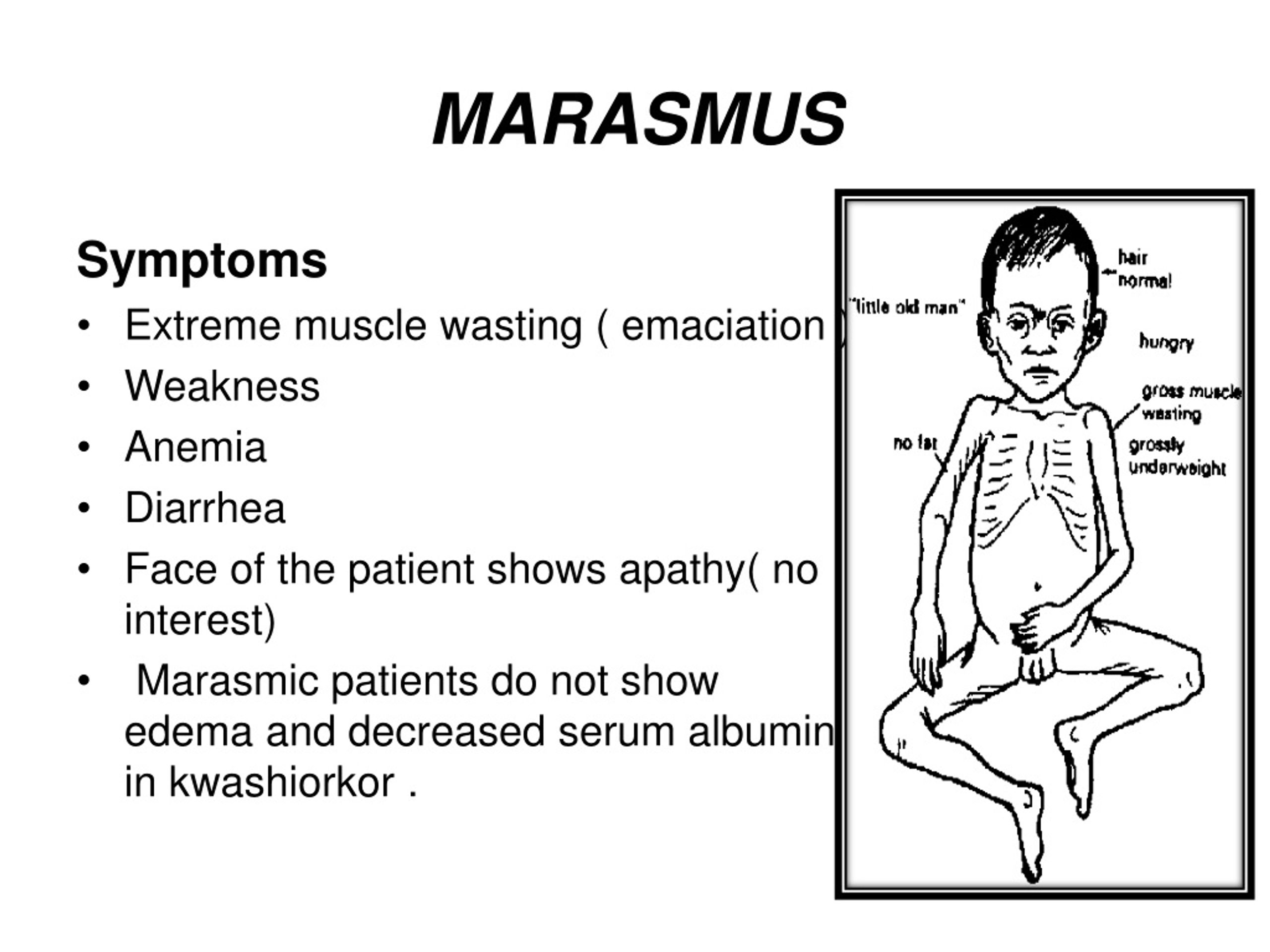
Marasmus
Protein-calorie starvation; decreased anthropometrics.
Scorbutic Gums
Vitamin C deficiency; bleeding/swollen gums.
Rickets
Vitamin D + calcium deficiency; soft bones, delayed growth.
Magenta Tongue
Riboflavin (B2) deficiency; may mimic iron/B-complex deficiencies.
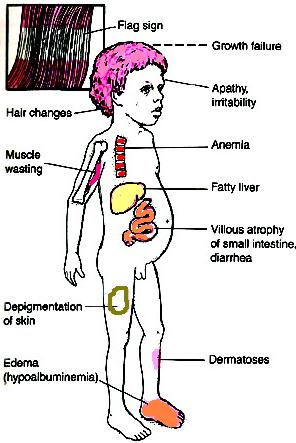
Kwashiorkor
High-calorie, low-protein diet; may appear obese; edema common.
Height + Weight for BMI
Both needed to calculate BMI and assess nutritional status.