Anatomy Unit 10 : Blood
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
formed elements
living blood cells; suspended in plasma
plasma
nonliving fluid matrix. makes up 55% of volume of blood sample. the liquid part of blood made up of 90% water. can dissolve nutrients, salts/electrolytes, respiratory gasses, hormones, plasma proteins, and various wastes and products of cell metabolism.
connective tissue
what type of tissue is blood classified as?
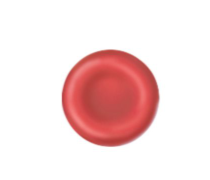
erythrocytes
red blood cells; if a sample of blood is centrifuged, this is the red mass at the bottom of the tube. Functions in oxygen transport. 45% of total volume of blood sample, known as hematocrit. they are anucleate (no nucleus). mature RBCs are literally “bags” of hemoglobin. because they lack mitochondria and make ATP by anaerobic mechanisms, they do not use up any of the oxygen they are transporting, making them very efficient oxygen transporters.
small flexible cells shaped like biconcave disks. because of their thinner centers, they look like miniature donuts when viewed with a microscope. their small size and peculiar shape provide a large surface area relative to their volume, making them ideally suited for gas exchange.
These outnumber white blood cells by about 1000 to 1 and are a major factor contributing to blood viscosity. There are normally about 5 million cells per cubic milometer of blood. When the number of RBC/mm³ increases, blood viscosity increases. The opposite happens when it decreases, causing the blood to thin and flow more rapidly. The more hemoglobin molecules the RBCs contain, the more oxygen they will be able to carry. A single red blood cells contains 250 million hemoglobin molecules.
buffy coat
a thin whitish layer at the junction between the erythrocytes and the plasma. This layer contains the remaining formed elements leukocytes and platelets
leukocytes
white blood cells. far less numerous than red blood cells but they are crucial to body defense against disease. there are 4800 to 10800 white blood cells per millimeter cubed. they account for less than one percent of the total blood volume. the only complete cells in the blood, meaning that they contain nuclei and the usual organelles.
these form a protective movable army that helps defent the body against damage by bacteria, viruses, parasites, and tumor cells. as such, they have some very special characteristics. white blood cells are able to slip into and out of the blood vessels. the circulatory system is simply their means of transportation to areas of the body where services are needed to inflammatory or immune responses.
these can also locate areas of tissue damage and infection in the body by responding to certain chemical that diffuse from the damaged cells. once they have “caught the scent”, the WBCs move through the tissue spaces by ameoboid motion. By following the diffusion gradient, they pinpoint areas of tissue damage and rally round in large numbers to destroy microorganisms and dispose of dead cells.
platelets
cell fragments that help stop bleeding (clotting)
hematocrit
“blood fraction”
leukocytes and platelets
contribute to less than 1% of total volume of blood sample
scarlet red
what is the color of oxygen-rich blood?
dull red
what is the color of oxygen-poor blood?
heavier
blood is ______ than water, mostly because of its formed elements
7.35 - 7.45
typical blood pH range
100.4 degrees F (38 C)
the temperature of blood; always slightly higher than body temperature
plasma proteins
the most abundant solutes in plasma. except for antibodies and protein-based hormones, most of these are made by the liver. these serve a variety of functions. these are NOT taken up by cells to be used as food fuels or metabolic nutrients
albumin
acts as a carrier to shuttle certain molecules through the circulation, is an important blood buffer, and contributes to the osmotic pressure of blood, which acts to keep water in the bloodstream.
clotting proteins
help stem blood loss when blood vessel is injured
antibodies
help protect the body from pathogens
acidosis
when the blood starts to become too acidic; respiratory system and kidneys are used to help restore homeostasis
alkalosis
when blood starts to become too basic ; respiratory system and kidneys are used to help restore homeostasis
hemoglobin
an iron-bearing protein that transports the bulk of the oxygen that is carried in the blood.
anemia
a decrease in the oxygen-carrying ability of the blood is called this. this may be the result of 1) a lower than normal number of RBCs or 2) an abnormal or deficient hemoglobin content in the RBCs.
sickle cell anemia
the type of anemia that causes the most hospital visits. the abnormal hemoglobin formed becomes spiky and sharp when the RBCs unload oxygen molecules or when the oxygen content of the blood is lower than normal, as during vigorous exercise, anxiety, or other stressful situations. the stiff, deformed erythrocytes rupture easily and dam up in small blood vessels. these events interfere with oxygen delivery and cause extreme pain. this is simply caused by a change in just ONE of the amino acids in two of the four polypeptide chains of the hemoglobin molecule.
this occurs chiefly in black people living in the malaria belt of Africa. the same gene that causes sickling makes red blood cells infected by the malaria-causing parasite stick to the capillary walls and then lose potassium. hence, the malaria causing parasite is prevented from multiplying within the red blood cells, and individuals with the sickle cell gene have a better chance of surviving where malaria is prevalent.
sickle cells trait (SCT)
those carrying just one sickle cells gene have this. they generally do not display the symptoms but can pass on the sickling gene to their offspring.
polycythemia
an excessive or abnormal increase in the number of erythrocytes. this may result from bone marrow cancer. it may also be a normal physiologic (homeostatic) response to living at high altitudes, where the air is thinner and there is less oxygen available
diapedesis
the process of white blood cells having the ability to slip in and out of the blood vessels
positive chemotaxis
the ability of WBCs to locate areas of tissue damage and infections in the body by responding to certain chemicals that diffuse from damaged cells.
leukocytosis
a total WBC count above 11,000 cells/mm³. this generally indicates that a bacterial or viral infection is stewing in the body.
leukopenia
an abnormally low WBC count, commonly caused by certain drugs, such as cortcosteriods and anticancer agents.
ameboid motion
WBCs move through tissue spaces through this mode of transport
leukemia
literally “white blood”, the bone marrow become cancerous, and huge numbers of WBCs are turned out rapidly
Granulocytes
granule-containing WBCs. They contain lobed nuclei, which are several nuclear areas connected by thin strands of nuclear material. These include neutrophils, basophils, and eosinophils.
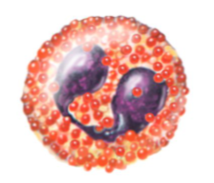
neutrophils
the most numerous of the WBCs. They have a multilobed nucleus and very fine granules that respond to both acidic and basic stains. The cytoplasm stains pink. These are avid phagocytes a sites of acute infection. They are particularly partial to bacteria and fungi, which they kill during a respiratory burst that deluges the phagocytized invaders with a potent brew of oxidizing substances (bleach, hydrogen peroxide, and others).
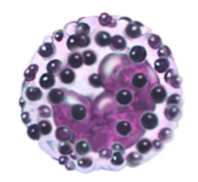
eosinophils
these have a blue-red nucleus that resembles an old-fashioned telephone receiver and sport coarse, lysosome-like, brick-red cytoplasm granules. Their number increases rapidly during infections by parasitic worms (flatworms, tapeworms) ingested in food or entering via the skin. When these encounter a parasitic worm prey, they gather around and release enzymes from their cytoplasmic granules onto the parasite’s surface, digesting it away
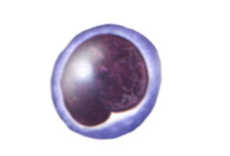
basophils
the rarest of the WBCs, have large histamine-containing (an inflammatory chemical that makes blood vessels leaky and attracts other WBCs to the inflammatory site) granules that stain dark blue.
histamine
an inflammatory chemical that makes blood vessels leaky and attracts other WBCs to the inflammatory site
4-6 million
the occurance of erythrocytes in blood per mm³
4,800-10,800
the occurance of leukocytes in blood per mm³
3,000-7,000 (30-70% of WBCs)
the occurance of neutrophils in blood per mm³
100-400 (1-4% of WBCs)
the occurance of eosinophils in blood per mm³
20-50 (0-1% of WBCs)
the occurance of basophils in blood per mm³
1,500 - 3,000 (20-45% of WBCs)
the occurance of lymphocytes in blood per mm³
100-700 (4-8% of WBCs)
the occurance of monocytes in blood per mm³
150,000 - 400,000
the occurance of platlets in blood per mm³
cell anatomy of erythrocytes
salmon-colored biconcave disks; anucleate; literally, sacs of hemoglobin; most organelles have been ejected
cell anatomy of neutrophils
cytoplasm stains pale pink and contains five granules, which are difficult to see; deep purple nucleus consists of 3-7 lobes connected by thin strands of nucleoplasm

cell anatomy of eosionphils
red coarse cytoplasmic granules; bilobed nucleus stains blue red
cell anatomy of basophils
cytoplasm has few large blue-purple granules; U- or S- shaped nucleus with constrictions, stains dark blue
cell anatomy of lymphocytes
cytoplasm pale blue and appears as thin rim around nucleus; spherical (or slightly indented) dark purple-blue nucleus
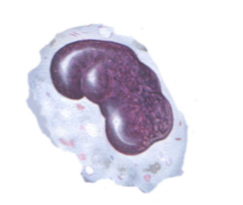
cell anatomy of monocytes
abundant gray-blue cytoplasm; dark blue-purple nucleus often kidney-shaped
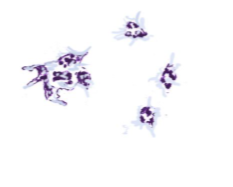
cell anatomy of platelets
essentially irregularly shaped cell fragments; stain deep purple
function of erythrocytes
transport oxygen bound to hemoglobin molecules; also transport small amounts of carbon dioxide
function of neutrophils
active phagocytes; number increases rapidly during short-term or acute infections
function of eosinophils
killl parasitic worms by deluging them with digestive enzymes; play a complex role in allergy attacks
function of basophils
release histamine (vasodilator chemical), at sites of inflammation; contain heparin, an anticoagulant
function of lymphocytes
part of immune system; one group (B) produces antibodies; other group (T) involved in graft rejection, fighting tumors and viruses, via direct cell attack
function of monocytes
active phagocytes that become macrophages in the tissues; long-term “cleanup team”; increase the number of chronic infections such as tuberculosis
function of platelets
needed for normal blood clotting; initiate clotting cascade by clinging to torn area
Never Let Monkeys Eat Bananas
how to remember the order of WBCs in order from most abundant to least
platelets
they are not cells in the strict sense. they are fragments of bizarre multi nucleate cells called megakaryocytes, which pinch off thousands of anucleate platelet pieces that quickly seal themselves off from the surrounding fluids. these appear as darkly staining, irregularly shaped bodies scattered among the other blood cells. they are needed for the clotting process that occurs in plasma when blood vessels are ruptured or broken.
hematopoiesis
blood cell formation, occurs in red bone marrow, or myeloid tissue. each type of blood cell is produced in different numbers in response to changing body needs and different stimuli. after they mature, they are discharged into the blood vessels surrounding the area. on average, red bone marrow turns out an ounce of blood contain 100 billion new cells each day.
myeloid tissue/ red bone marrow
in adults, this tissue is found chiefly in the flat bones of the skull and pelvis, the ribs, sternum, and proximal ephphyses of the humerous and femur.
hemocytoblast
all of the formed elements arise from this common type of stem cell. this resides in the red bone marrow. this forms two types of descendants: the lymphoid stem cell (produces lymphocytes) and the myeloid stem cell (produces all other formed elements)
erythropoietin
the rate of erythrocyte production is controlled by this hormone.
hemostasis
stoppage of bleeding
vascular spasms, platlet plug formation, and coagulation/blood clotting
the three major phases of hemostasis
vascular spasms
the immediate response to blood vessel injury is vasoconstriction, which causes that blood vessel to go into spasms. the spasms narrow the blood vessel at that point, decreasing blood loss until clotting can occur.
platelet plug formation
platelets are repelled by an intact endothelium, but when it is broken so that the underlying collagen fibers are exposed, the platelets become “sticky” and cling to the damaged site. achored platelets releases chemicals that enhance the vascular spasms and attract more platelets to the site. as more and more platelets pile up, a small mass forms.
coagulation
at the same time, the injured tissues are releasing tissue factor. this combination interacts with other blood protein clotting factors and calcium ions to form an activator that leads to the formation of thrombin, an enzyme. Thrombin then joins soluable fibrinogen proteins into long, hairlike molecules of insoluable fibrin. Fibrin forms a meshwork that traps the RBCs and forms the basis of a clot. within the hour, the clot begins to retract, squeezing serum from the mass and pulling the ruptured edges of the blood vessel closer together.
tissue factor
injured tissues release this. it interacts with PF3, a phospholipid that coats the surfaces of the platelets
3-6 minutes
how long blood normally takes to clot
thrombus
a clot that develops and persists in an unbroken blood vessel. if it is large enough, it may prevent blood from flowing to the cells beyond the blockage.
embolus
if a thrombus breaks away from the vessel wall and floats freely in the bloodstream it becomes this. it is usually no problem unless or until it lodges in a blood vessel too narrow for it to pass through.
thrombocytopenia
results from an insufficient number of circulating platelets. even normal movements cause spontaneous bleeding from small blood vessels. this is evidenced by many small purplish blotches called petechiae on the skin. it can arise from a condition that suppresses the bone marrow, such as bone marrow cancer, radiation, or certain drugs.
hemophilia
this term applies to several different hereditary bleeding disorders that result from a lack of any of the factors needed for clotting, commonly called “bleeder’s disease”, these have similar isgns and symptoms that begin in early life. even minor tissue trauma results in prolonged bleeding and can be life-threatening. repeated bleeding into joints causes them to become disabled and painful. when a bleeding episode occurs, hemophiliacs are given a transfusion of fresh plasma or injections of the purified clotting factor they lack.
anitgen
a substance that the body recognizes as a foreign; it stimulates the immune system to release antibodies or use other means to mount a defense against it. most of these are foreign proteins, such as those that are part of viruses or bacteria that have managed to invade the body. although each of us tolerates our own self-antigens, one person’s RBC proteins will be recognized as foreign if transfused into another person with different RBC antigens
antibodies
the “recognizers”. present in plasma in the plasma that attach to the RBCs bearing surface antigens different from those on the patient’s RBCs.
agglutination
binding of the antibodies causes the foreign RBCs to clump. this leads to the clogging of small blood vessels throughout the body. during the next few hours, the foreign RBCs are lysed, and their hemoglobin is released into the bloodstream.