Comprehensive Guide to Muscular Dystrophies, ADHD, SPD, and Sickle Cell Anemia
1/134
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
135 Terms
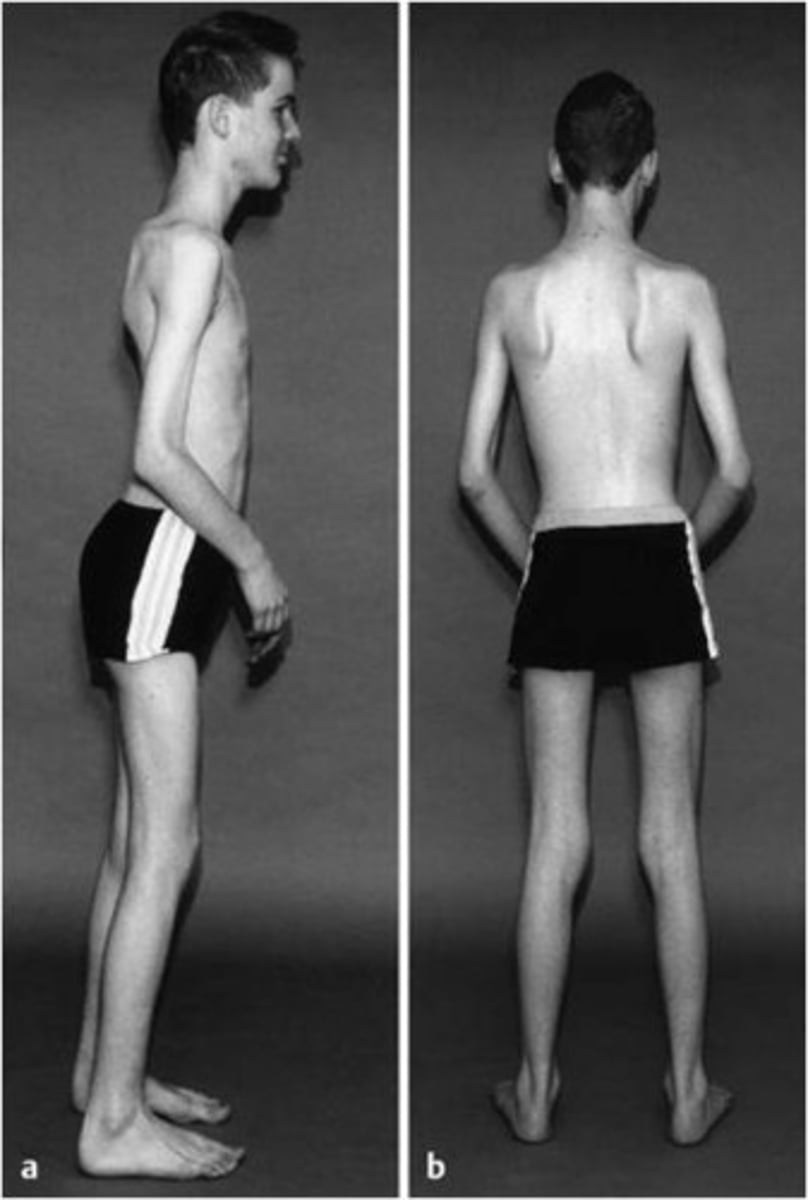
What are the key symptoms of Duchenne Muscular Dystrophy (DMD)?
Symptoms include delayed motor development, proximal weakness, increased fatigue, waddling gait, enlarged calf muscles, frequent falls, inability to run or jump, and the Valley sign.

What is the valley sign?
"valleys" below armpits indicates Duchenne MD

What is the typical progression and life expectancy for Duchenne Muscular Dystrophy?
Progression is proximal to distal, affecting legs before arms, with life expectancy in late teens to early twenties, usually due to heart or breathing problems.
What is the inheritance pattern of DMD?
X-linked recessive
What distinguishes Becker Muscular Dystrophy from Duchenne Muscular Dystrophy?
Becker MD has a slower progression, symptoms typically begin between 6-18 years old (but can be 5-60 years old), and it is caused by a shorter, partially functional dystrophin.
What are the common symptoms of Becker Muscular Dystrophy?
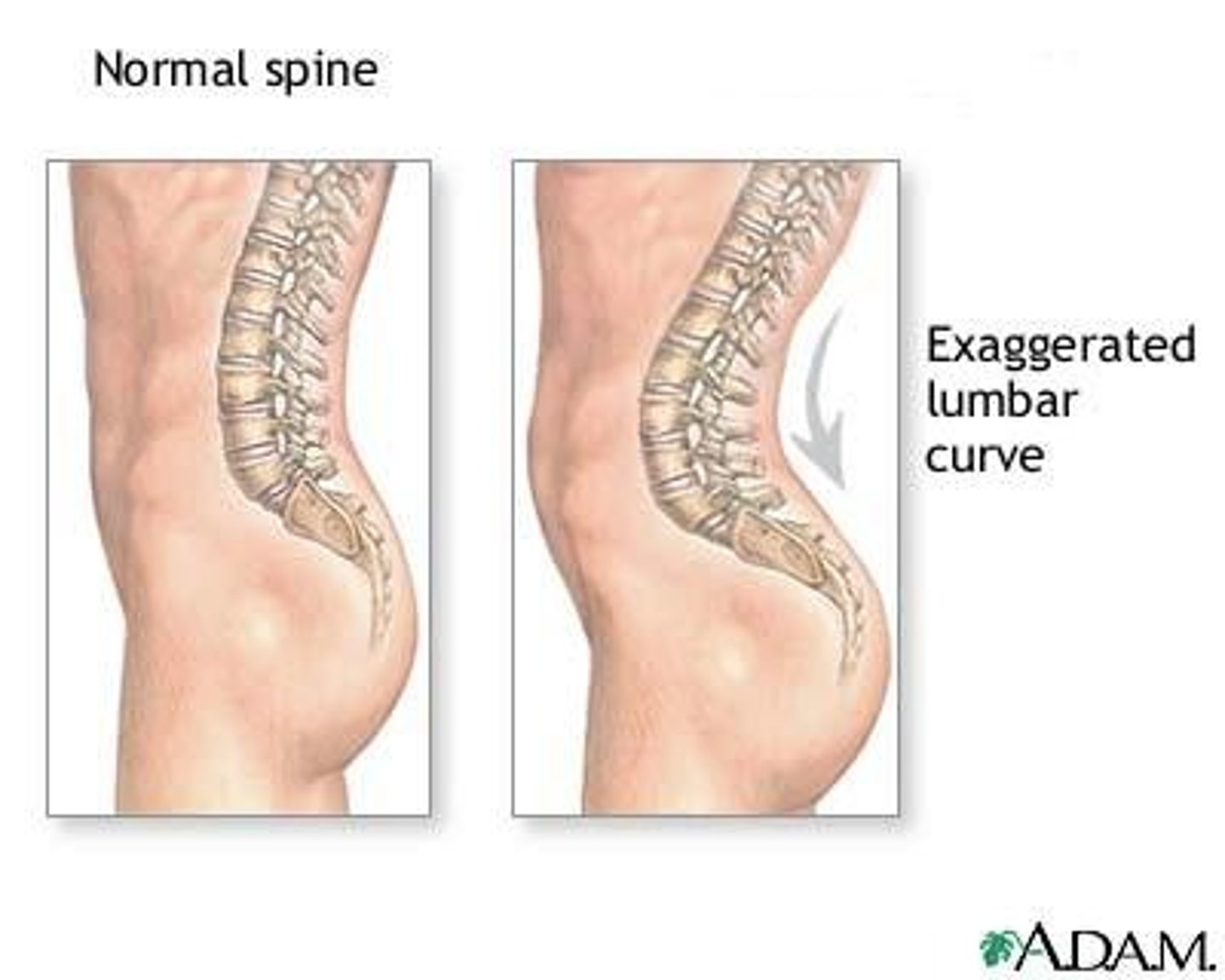
Symptoms include delayed ambulation, difficulty climbing stairs, walking on toes, cramps, fatigue, and lumbar lordosis.
What is the life expectancy for individuals with Becker Muscular Dystrophy?
Life expectancy extends into middle and late adulthood.
What is the inheritance pattern of Becker MD?
X-linked recessive
What are the key characteristics of Limb-Girdle Muscular Dystrophy?
Positive Gower sign, waddling gait, enlarged calves, severe lordosis, and proximal muscle weakness. Progression not always symmetrical.

What is a positive Gower sign?
Has to use hands to "walk up" thighs when going from sitting to standing
Indicates limb-girlde MD
What is the inheritance pattern of Limb-Girdle MD?
It includes various subtypes, typically caused by recessive genes. Affects both genders equally.
What is the life expectancy for those with Limb-Girdle Muscular Dystrophy?
early thirties to a normal lifespan
Symptoms of Myotonic Muscular Dystrophy
Slow progression of weakness starting in the face, lower legs, forearms, hands, and neck.
Muscles lock, followed by delayed relaxation.
Many organs affected, especially the heart
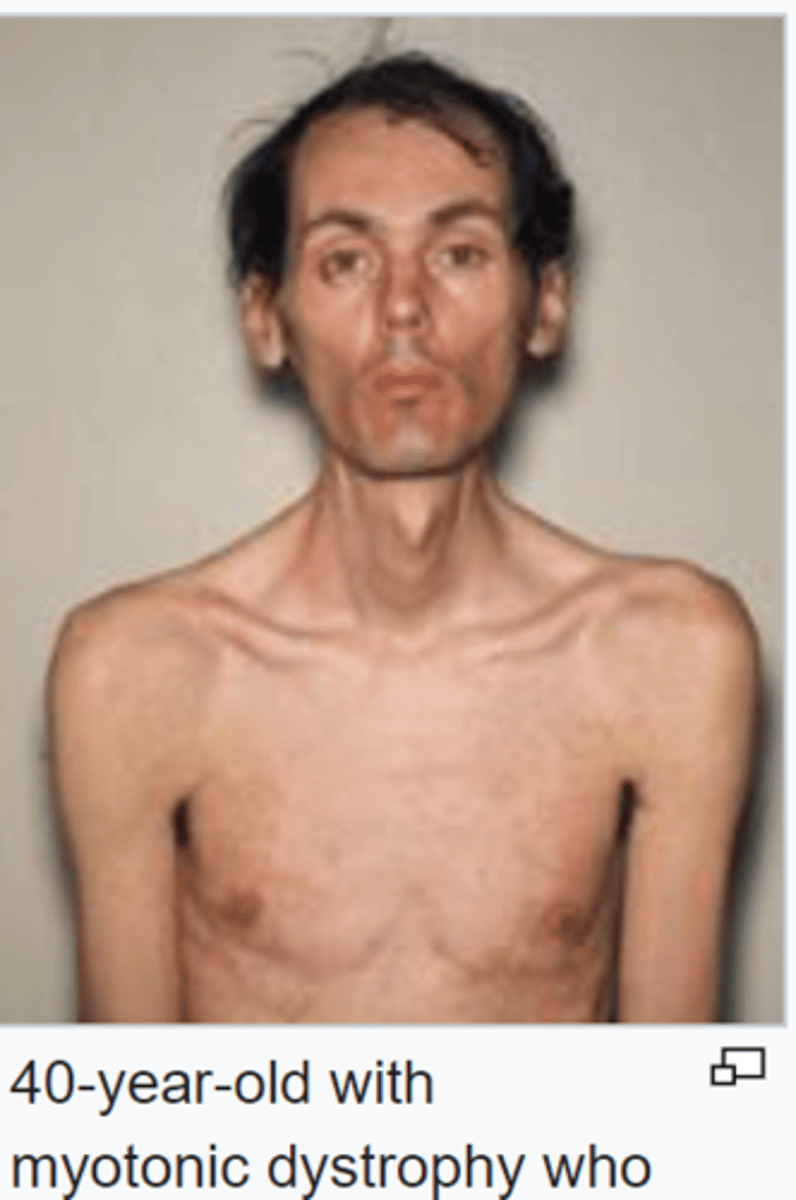
When is the onset of symptoms for Myotonic MD?
teens or adulthood.
What is the life expectancy for individuals with Myotonic Muscular Dystrophy?
into late adulthood.
Inheritance of Myotonic MD
Autosomal dominant
Key features of Facioscapulohumeral Muscular Dystrophy
Weakness in facial, shoulder, and upper arm muscles.
Hard to close eyes
Asymmetrical smile
Drooping of the corners of the mouth
Can't whistle or pucker
Atrophy
Winged scapula
Beevor sign
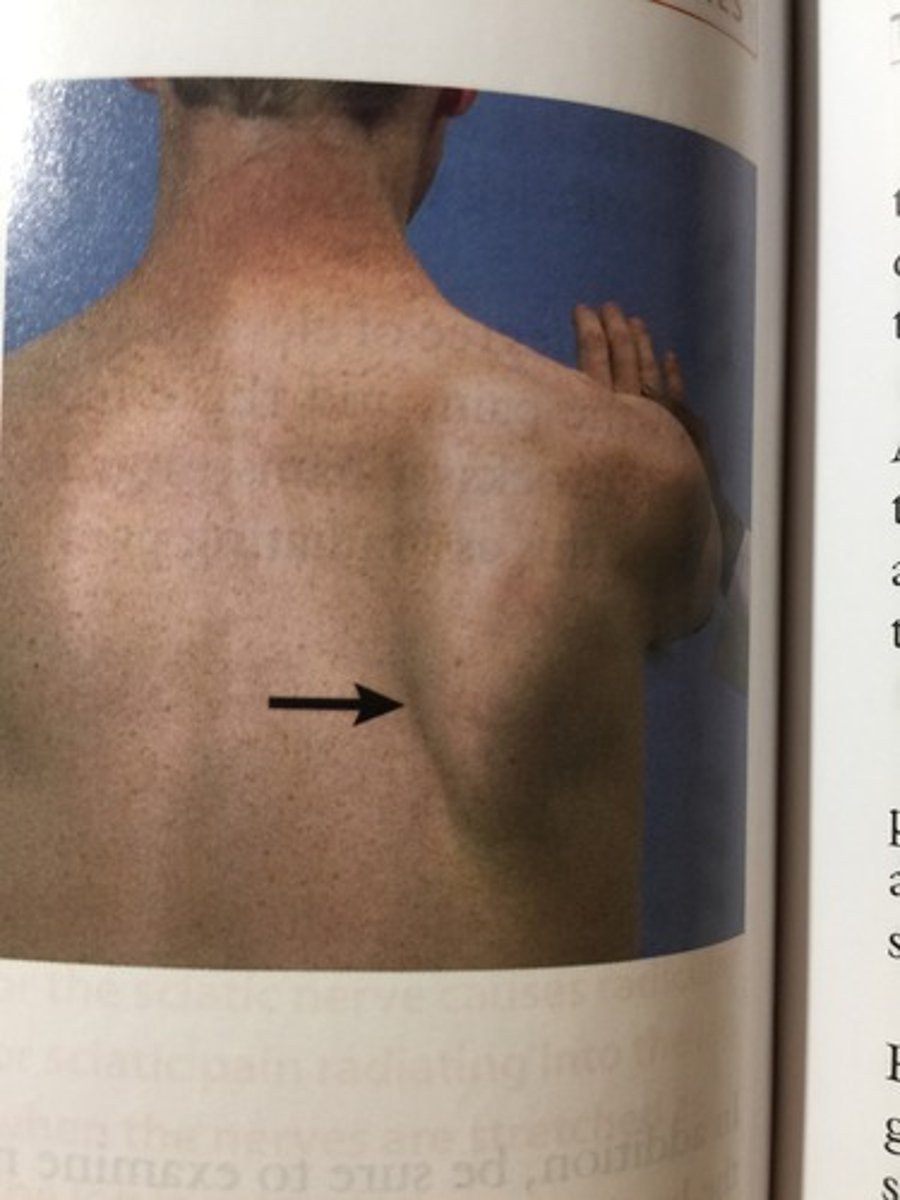
What is the Beevor sign?
navel moves towards the head upon flexing the neck, indicating selective weakness of the lower abdominal muscles
Indicates Facioscapulohumeral MD

Onset of Facioscapulohumeral Muscular Dystrophy
variable onset (7-20 yrs old)
Inheritance of Facioscapulohumeral MD
autosomal dominant
What is the life expectancy for individuals with Facioscapulohumeral Muscular Dystrophy?
Life expectancy is normal.
What are the symptoms of Emery-Dreifuss Muscular Dystrophy?
Symptoms include contractures before muscle weakness, toe walking, increased falls, and elbow contractures at a 90-degree angle.
What is the progression and life expectancy for Emery-Dreifuss Muscular Dystrophy?
Progression is symmetrical, and life expectancy can be normal if cardiac issues are addressed.
What is the common genetic cause of all types of Muscular Dystrophy?
All types of Muscular Dystrophy are caused by genetic mutations.
What common symptoms are shared by all types of Muscular Dystrophy?
Common symptoms include decreased strength, muscle cramping, and decreased gross motor skills.
What is Spinal Muscular Atrophy (SMA) and how does it relate to MD?
SMA is a progressive motor neuron disease characterized by generalized muscle weakness, often mistaken for MD.
What is Myasthenia Gravis and how does it relate to MD?
Myasthenia Gravis causes weakness and rapid fatigue of voluntary muscles due to a breakdown in communication between nerves and muscles, mimicking MD.
What is Pompe Disease and how does it relate to MD?
Pompe Disease is an inherited disorder caused by glycogen buildup in cells, which can mimic MD symptoms.
What is Charcot-Marie-Tooth (CMT) disease and how does it relate to MD?
CMT is a hereditary, slowly-progressing disease of the peripheral nerves that can be mistaken for MD.
What diagnostic tests are used to diagnose Muscular Dystrophy?
Hematology (tests for elevated CK levels), electromyography (measures electrical activity of muscle), and muscle biopsy (determines type of MD).
What are the medical and surgical management options for Muscular Dystrophy?
Management may include physical therapy, medications to manage symptoms, and surgical interventions to address complications.
What is the primary goal of treatment for muscular dystrophy?
Maintenance of independence for as long as possible.
What respiratory maintenance strategies are important for MD patients?
Suctioning, cough assist, or antibiotics may be needed due to high risk of infection/pneumonia.
Why is skin integrity important in MD management?
Reduced mobility can lead to skin infections or damage, decreasing joint mobility, requiring routine inspections.
What pain management strategies are recommended for MD patients?
Regular joint stretching to reduce tightness, cramping, and spasms.
How does nutrition play a role in managing muscular dystrophy?
It helps with skin integrity and obesity control; may require diet modifications or feeding tubes for patients with dysphagia.
What is the focus of occupational and physical therapy (OT/PT) services for MD patients?
To prevent or slow loss of strength, range of motion, and function, and to determine necessary equipment for assistance.
What are some medication interventions for muscular dystrophy?
Corticosteroids, immunosuppressants, anticonvulsants, antibiotics, OTC analgesics, and experimental drugs like Spinraza and Emflaza.
What surgical management options are available for MD patients?
Contracture release, scoliosis repair, cardiac stability, respiratory assist, spinal stabilization, pacemakers, tracheostomies, and feeding tubes.
How does muscular dystrophy impact occupational performance?
Increased dependence in ADLs/IADLs, requiring adaptive equipment and home modifications.
What educational considerations are there for children with muscular dystrophy?
Most do not have cognitive impairment but may experience increased absences due to illness and fatigue.
How does muscular dystrophy affect work and play for individuals?
Fatigue and physical limitations may require modifications to activities.
What social participation challenges do individuals with muscular dystrophy face?
Fear, anxiety, anger, frustration, depression, and suicidal ideation can affect the individual and their family.
What characterizes Attention Deficit Hyperactivity Disorder (ADHD)?
Persistent and maladaptive symptoms of inattention, hyperactivity, and impulsivity.
What is the gender prevalence of ADHD?
Boys are 4 times more likely to have ADHD.
At what age does ADHD typically onset?
ADHD typically has an onset at 7 years old.
What are the three hallmark clinical presentations of ADHD according to the DSM-V?
Combined (both attention and hyperactive-impulsive symptoms), predominately inattentive, and predominately hyperactive-impulsive.
Why is it important for ADHD diagnosis to show symptoms in multiple contexts?
Symptoms in one setting may indicate a problem with the setting, while symptoms in all settings suggest the issue is with the child.
How are ADHD severity ratings differentiated?
Mild: a few symptoms beyond diagnosis with minor impairment; Moderate: many symptoms with moderate impairment; Severe: many symptoms with high impairment.
What are some brain differences found in people with ADHD?
Specific brain differences have been identified, though the notes do not specify what they are.
What are the characteristics of the PFC in individuals with ADHD?
Lower dopamine levels, irregular fronto-cortical and fronto-subcortical systems, responsible for cognition and motivation, and reduced gray matter.
What is the prevalence of ADHD in children and adults?
Affects 7-11% of children and 4-5% of adults.
What percentage of children with ADHD typically outgrow the condition by adulthood?
Half of the children with ADHD.
What are some examples of inattentive symptoms of ADHD?
Trouble paying attention to details, making careless errors, not listening, getting distracted, losing things, and difficulty with boring tasks.
What are some examples of hyperactive-impulsive symptoms of ADHD?
Fidgeting, wandering, running around, difficulty being quiet, talking a lot, interrupting, and struggling to take turns.
What are the three steps to diagnosing ADHD?
1. Conduct an ADHD assessment for children aged 4-18 with academic or behavior problems. 2. Check if DSM-5 criteria are met through observations, interviews, and rating scales. 3. Screen for comorbid conditions.
What is the BASC-32 scale used for?
It tests for ADHD, anxiety, and mood disorders and makes students eligible for special education.
What is developmental coordination disorder (DCD)?
Also known as dyspraxia, it involves clumsiness, delays in sitting or walking, and difficulty with tasks like jumping or tying shoelaces.
What does DAMP stand for and its connection to ADHD?
DAMP stands for Deficits in Attention, Motor control, and Perception, often seen in individuals with ADHD.
What conditions are commonly comorbid with ADHD?
Substance abuse, PTSD, OCD, and bipolar disorder.
How does ADHD presentation change as individuals age?
Overactivity becomes more inward, with restlessness and difficulty sleeping; impulsivity subsides, but attention and disorganization symptoms continue.
What main factor predicts how a child with ADHD will perform in school and work as an adult?
IQ.
What type of treatment is most effective for ADHD?
Multimodal intervention.
What are some medications used to treat ADHD symptoms?
Long-lasting stimulant medications like Methylphenidate (Ritalin) and Dextro-amphetamine (Adderall), as well as nonstimulants like Atomoxetine and Guanfacine.
What are nonpharmacological interventions available for ADHD?
CBAT, CBT, meta-cognitive therapy, mindfulness, and coaching.
What is CBAT and its target age group?
Child-focused behavioral activation therapy for children aged 7-10, involving parent-training and direct work with the child.
What is the purpose of CBT in treating ADHD?
To change the patient's thinking and teach organizational, problem-solving, and planning skills.
What is the role of mindfulness in ADHD treatment?
To bring awareness to the present moment and reduce automatic or impulsive responses.
Why is parent education and training important for children with ADHD?
It helps parents understand and support their child's needs and manage challenging behaviors.
How can occupational therapists (OTs) support classroom interventions for children with ADHD?
By facilitating reasonable accommodations through a 504 plan or providing extensive support via an individualized education plan (IEP).
What are the three main categories of support an Occupational Therapist (OT) can provide?
Behavioral programs, instructional strategies, and environmental strategies.
What are some examples of behavioral programs used by OTs?
Contingency management approaches, daily report cards, token economies, positive reinforcement, time out, and planned ignoring.
What instructional strategies can OTs train children in?
Study skills, note-taking, self-regulation, and social skills.
What are some environmental strategies an OT might use in a classroom?
Seating the child close to the teacher, reducing noise and clutter, and utilizing peer tutoring.
How can ADHD symptoms interfere with a child's performance in ADLs?
Symptoms can make it hard for children to start tasks, plan routines, and complete tasks on time.
What challenges do children with ADHD face in IADLs?
They struggle to keep their house clean, do laundry, pay bills on time, meal prep, and care for pets.
How does ADHD affect health management for children?
Children may have difficulty refilling medications and consistently meeting with clinicians.
What sleep-related challenges do individuals with ADHD face?
Many struggle to get enough sleep or follow a bedtime routine, leading to fatigue that exacerbates symptoms.
How does ADHD impact educational performance?
It is associated with poor school performance, low grades, and a higher likelihood of dropping out.
What employment challenges do individuals with ADHD face?
They have a greater risk of low socioeconomic status and lower rates of professional employment.
How does ADHD affect social participation and play?
Children may experience less enjoyment from social play, struggle to wait their turn, become overstimulated, and be easily irritable.
What are the eight components of our sensory system?
Visual, auditory, tactile, olfactory, gustatory, vestibular, proprioception, and interoception.
What is the function of the vestibular system?
It detects linear, angular, and circular movement of the body and the pull of gravity, aiding in balance and spatial perception.
What characterizes vestibular dysfunction?
It can manifest as a need to move excessively or a fear of movement, known as gravitational insecurity.
What is proprioception and where is it located?
Proprioception is located in mechanosensory neurons in muscles, joints, and tendons, allowing awareness of body position and motion.
What does interoception refer to?
Interoception is the awareness of the body's physiological state, interpreting signals from internal organs.
What is an adaptive response in sensory integration?
An adaptive response is the ability to learn from the environment and react in a way that helps overcome challenges.
How does sensory integrative dysfunction relate to sensory processing disorder?
Sensory integrative dysfunction is the old term for sensory processing disorder (SPD).
What factors might cause sensory processing disorder (SPD)?
Various factors, including genetic, environmental, and neurological influences, may contribute to SPD.
What are some possible factors contributing to Sensory Processing Disorder (SPD)?
Maternal stress, high adrenaline and cortisol, postnatal abuse, abnormal white matter, low birth weight, prematurity, maternal illness, maternal medication use, single parenthood, low socioeconomic status (SES), maternal alcohol use, smoking, and paternal illicit drug use.
How common are SPD symptoms in the general population?
1 in 20 people have SPD symptoms, which can be as high as 2 in 10 children.
In which populations is SPD more commonly found?
SPD is more common in gifted children and those with ADHD, ASD, and Fragile X syndrome.
What characterizes sensory overresponsivity?
An intense or prolonged reaction to stimuli due to sympathetic nervous system activation, leading to behaviors such as aggression, avoidance, or shutdown.
What is sensory underresponsivity?
Challenges in the CNS's feed-forward mechanism, resulting in a lack of detection of incoming sensory information, often seen in 'easy babies' who are hypo-aroused.
What is sensory craving in children?
A constant desire for more sensory input, leading to impulsive and unsafe behavior, with two subtypes: the 'more and more' group and the self-regulating group.
What are postural disorders in sensory-based motor disorders?
Difficulty maintaining good posture, both while still and during movement.
What is dyspraxia?
A condition characterized by difficulty with motor planning, leading to clumsiness and maladaptive responses during novel tasks.
What is sensory discrimination?
The difficulty in distinguishing between similar stimuli, such as visual differences (ovals vs circles) or auditory differences ('b' vs 'd').
Why is the diagnosis of SPD considered controversial?
SPD is not recognized as an official disorder in the DSM-5.
Do individuals outgrow SPD?
No, individuals do not outgrow SPD, but they may develop compensatory strategies as they age.