Deck 2: Lids & Lacrimal Glands + Cornea & Conjunctiva
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
105 Terms
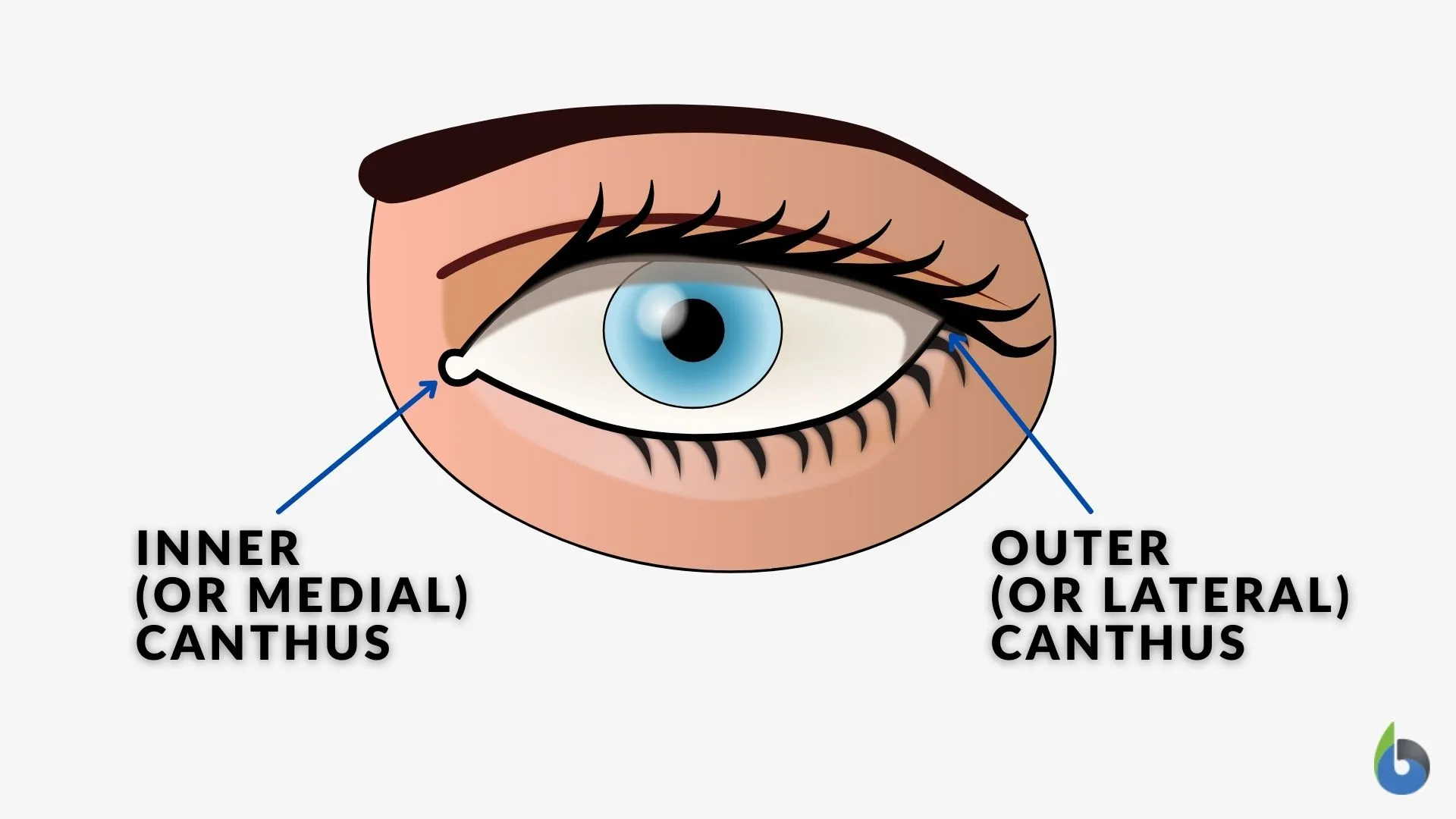
What are the canthi?
points where the upper and lower lids are joined
Describe the contour of the upper eyelid.
it forms a smooth, continuous arch extending from the medial to the lateral canthus
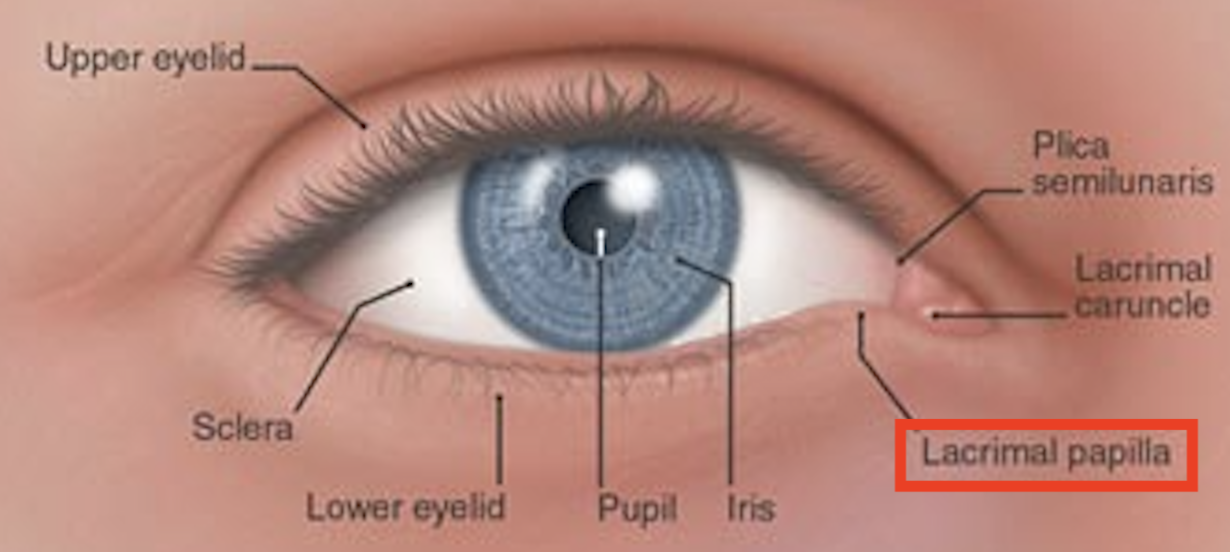
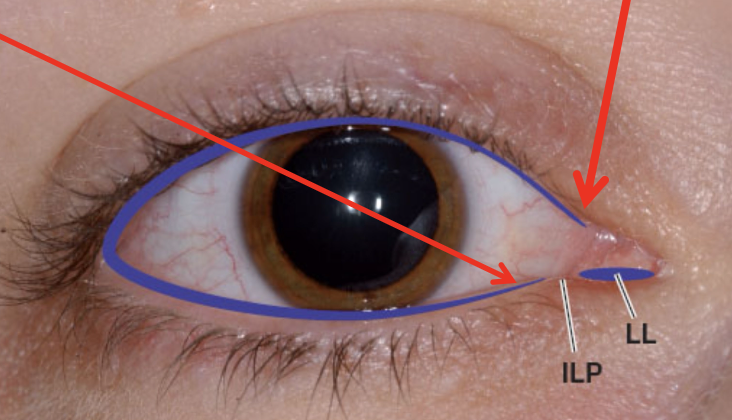
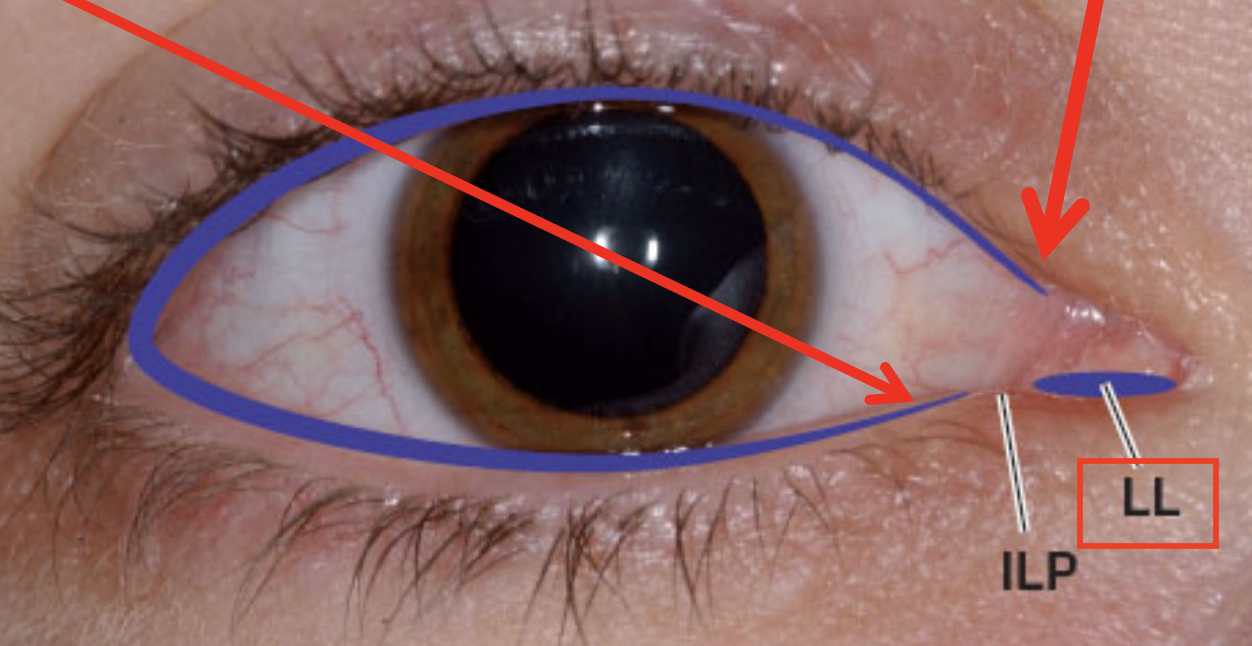
What is the lacrimal papilla?
small elevation near the medial canthus where the lower lid contour peaks
What is located at the top of the lacrimal papilla? What’s this structure’s function?
Inferior Lacrimal Punctum (ILP) — an opening that drains tears into the lacrimal system
Does the superior lacrimal punctum affect the eyelid contour?
No, it’s very small and doesn’t alter the upper lid’s contour
What is the lacrimal lake (LL)?
small reservoir for tears located b/w the inferior lacrimal punctum & medial canthus
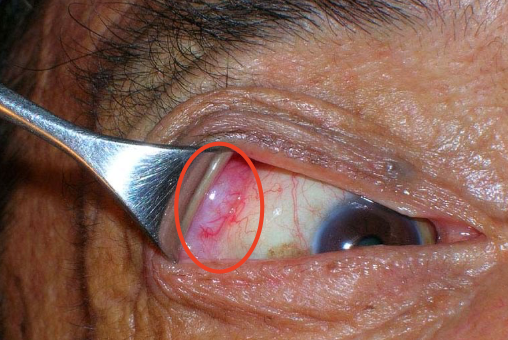
How do the features of the medial and lateral canthi compare?
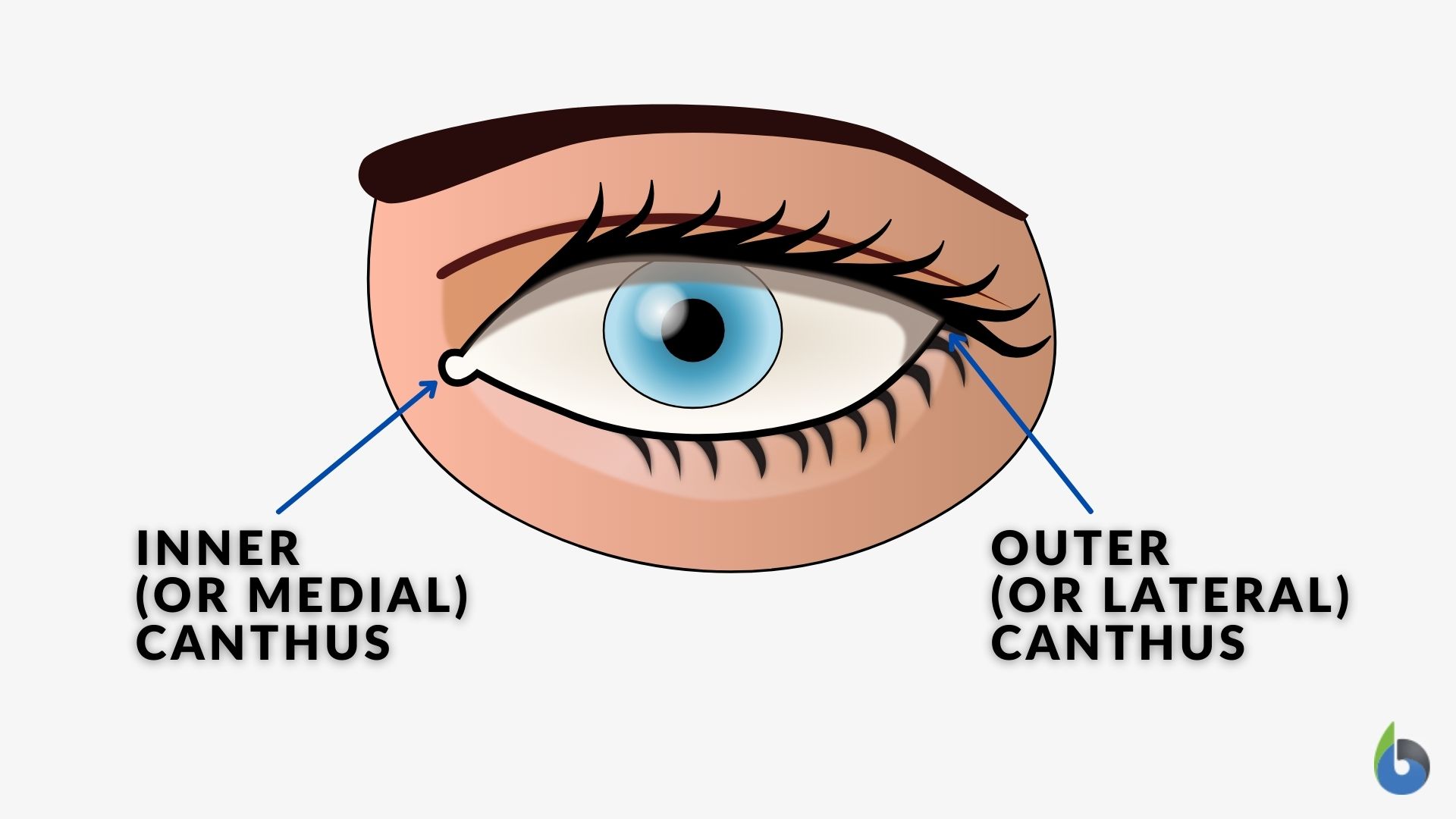
Lateral canthus → featureless
Medial canthus → has a small reddish body (lacrimal caruncle) mounted on the plica semilunaris
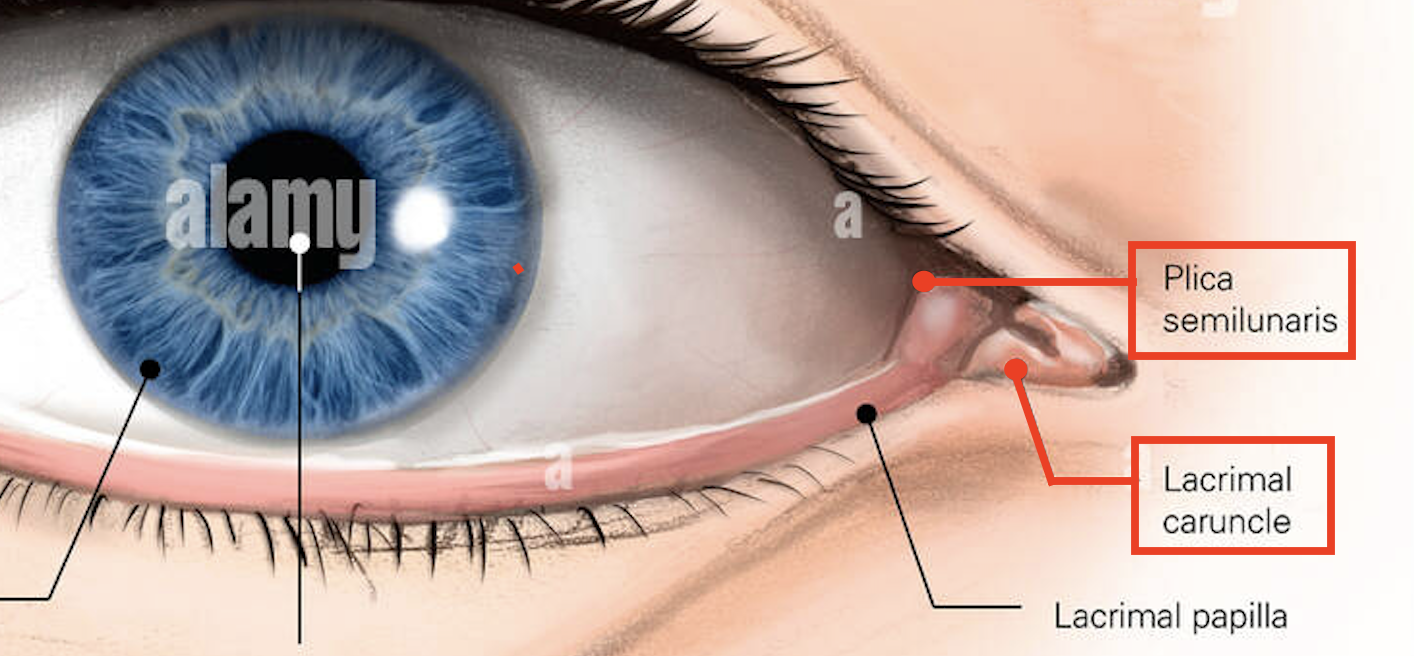
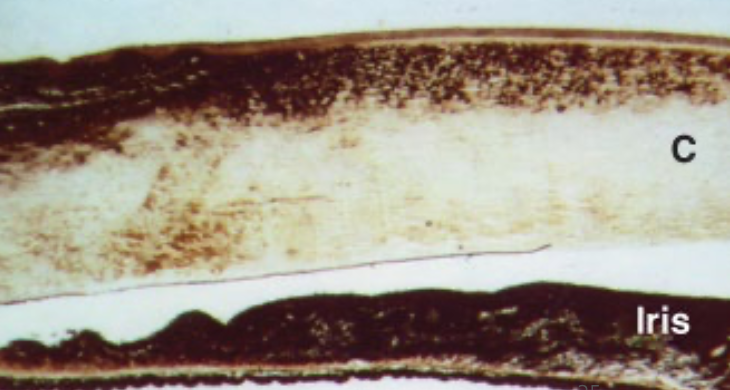
What is the plica semilunaris (P)?
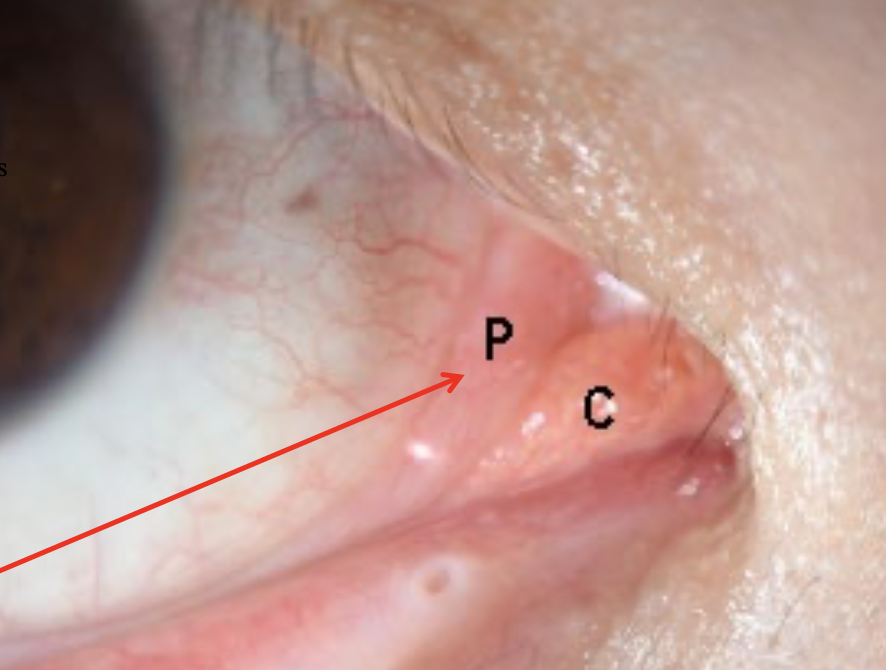
→ a fold of bulbar conjunctiva beside the caruncle (C)
this is a vestigial remnant of the 3rd eyelid
Define Distichiasis.
Multiple rows of lashes
Define Trichiasis.
Ingrowing lashes (e.g., curl inside instead of outside)
Define Madarosis.
Loss of lashes
Define Poliosis.
Whitening of lashes
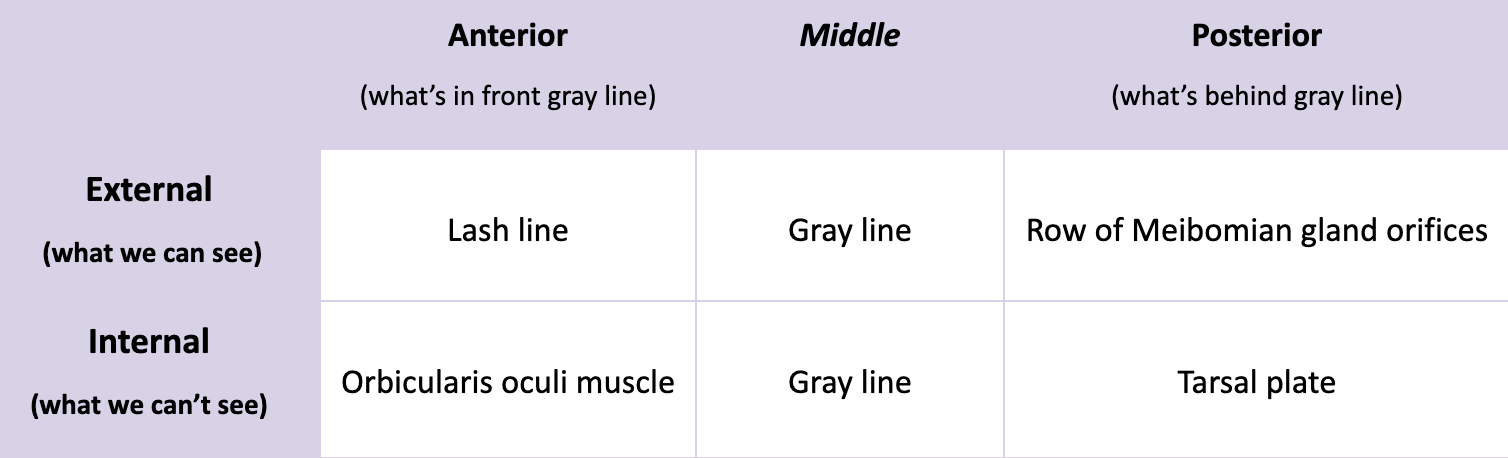
Where is the Gray line located? Mention the internal and external locations.
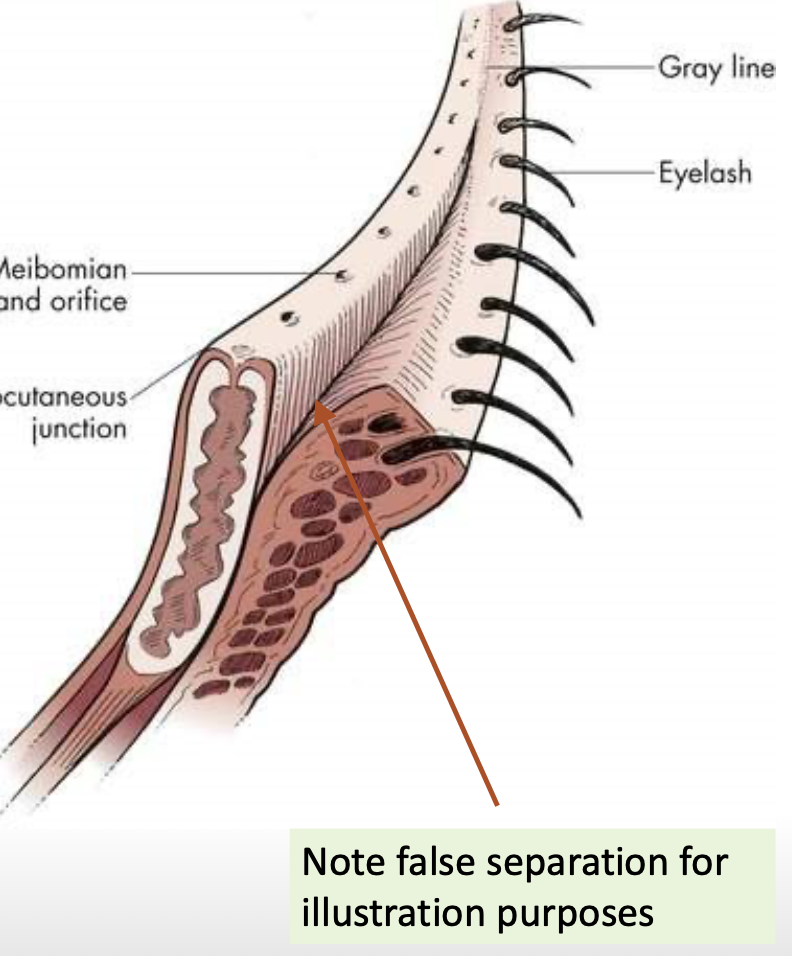
Why is the gray line clinically important?
→ it’s an important surgical landmark b/c it lies along a relatively bloodless plane
During the “split-lid” procedure, the posterior edge of the gray line is split, allowing the eyelid to split into → anterior & posterior lamellae
List the 3 skin layers.
Epidermis
Dermis
Hypodermis
Describe what the skin on eyelids is like.
thin → wrinkle + damage prone
has a keratinized epidermis (made of stratified squamous epithelium)
has a highly attenuated hypodermis
attenuated = weakened (no fat in the eyelid)
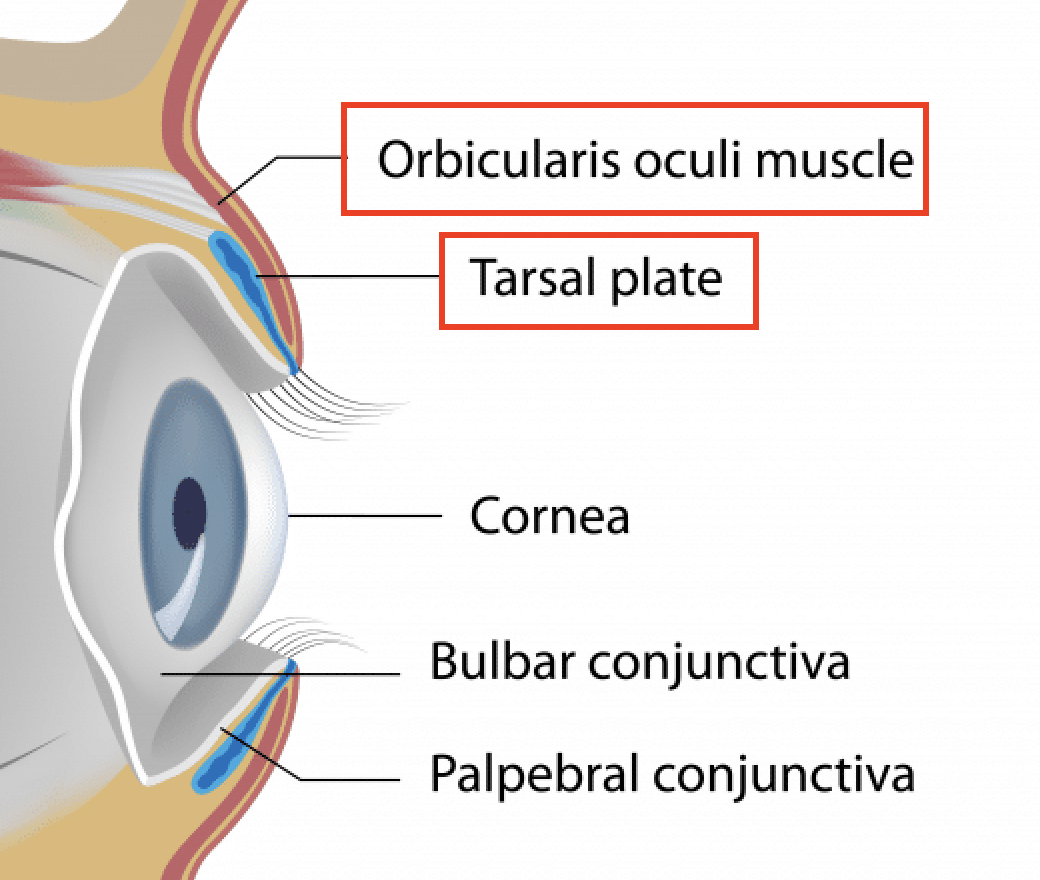
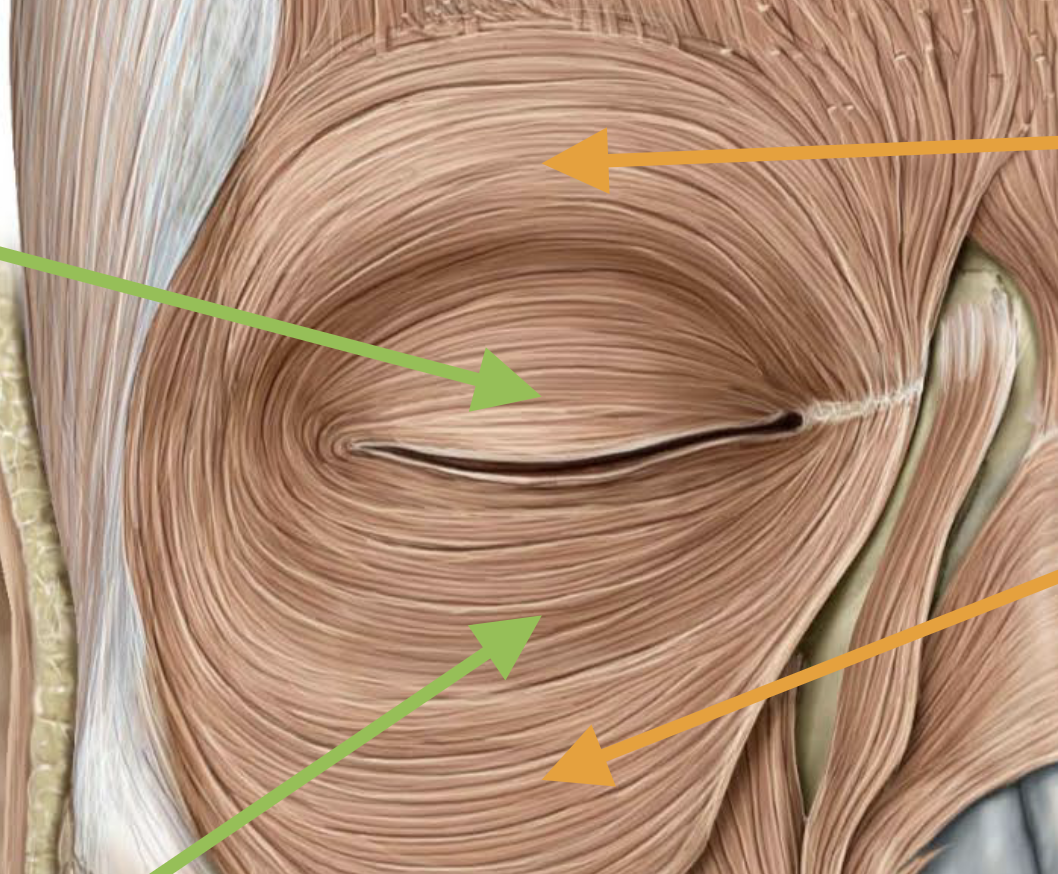
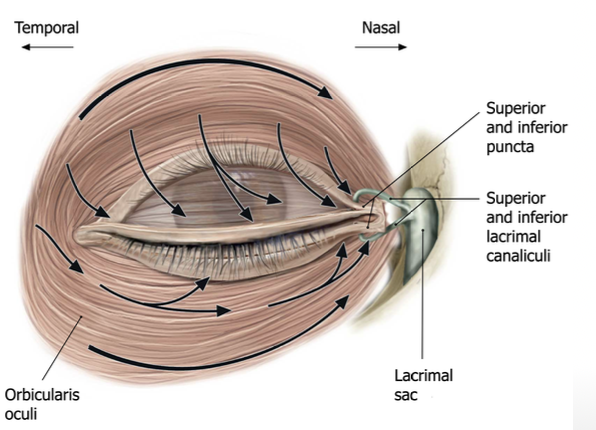
What is the structure of the Orbitus Oculi muscle?
→ Main muscle of the eyelid
Broad and flat skeletal muscle
Encircles the eyelids and orbital rim
Muscle fibers are oriented parallel to the orbital & lid margin → forms a ring around the eye (acts like a sphincter)
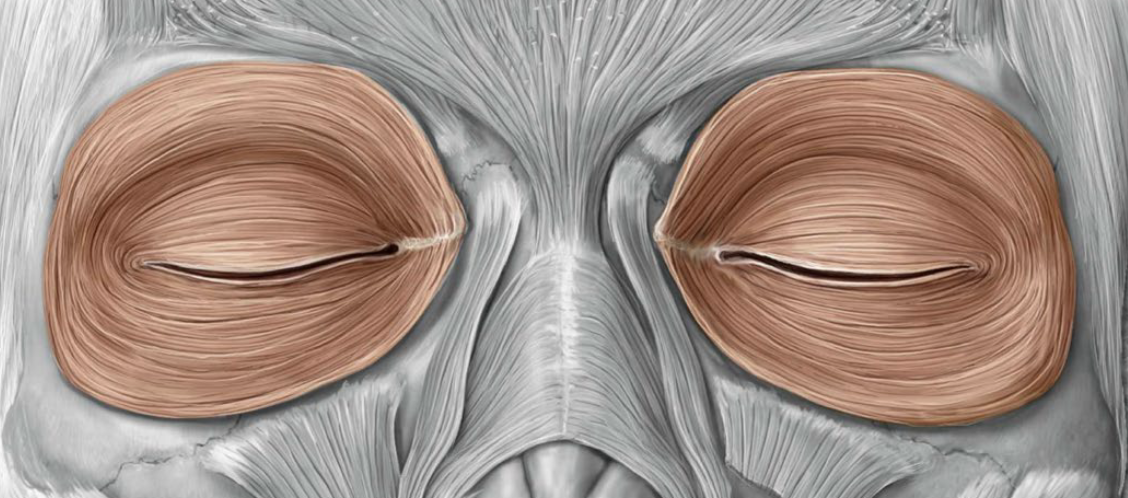
What is the function of the Orbitus Oculi muscle?
→ Acts as a sphincter muscle that constricts to close the eyelid
Voluntary (e.g., winking)
Involuntary reflex (e.g., blinking → protect from light, debris, dryness)
How is the Orbitus Oculi muscle innervated?
→ Supplied by Facial nerve (CN VII)
Specifically the temporal and zygomatic branches
Why is the Orbitus Oculi muscle innervated by 2 branches?
b/c the O. Oculi muscle has 2 distinct portions
Orbital - surrounds the orbital rim → allows “forceful” blinking
Palpebral - lines the inside of the eyelid → allows “gentle” blinking
What are the Tarsal Plates?
→ Thick bands of dense irregular CT that act like the “skeleton” of the eyelid
Span most of the breadth of the upper and lower lids
have Meibomian glands embedded within them
Function: provide form and additional stiffness
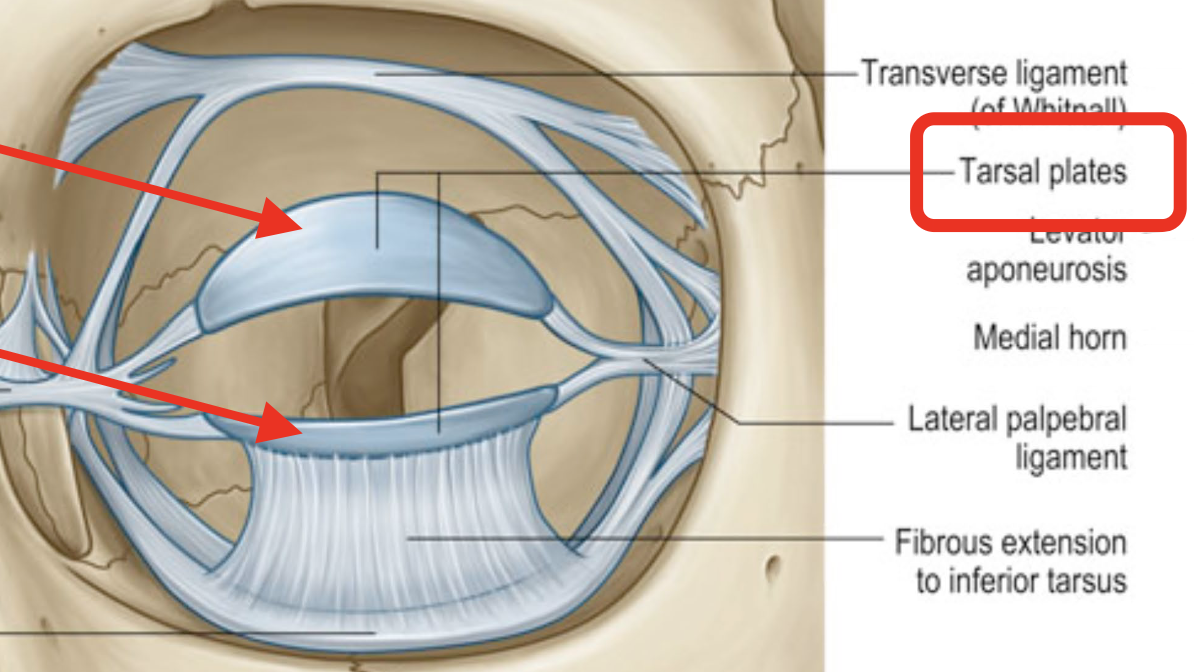
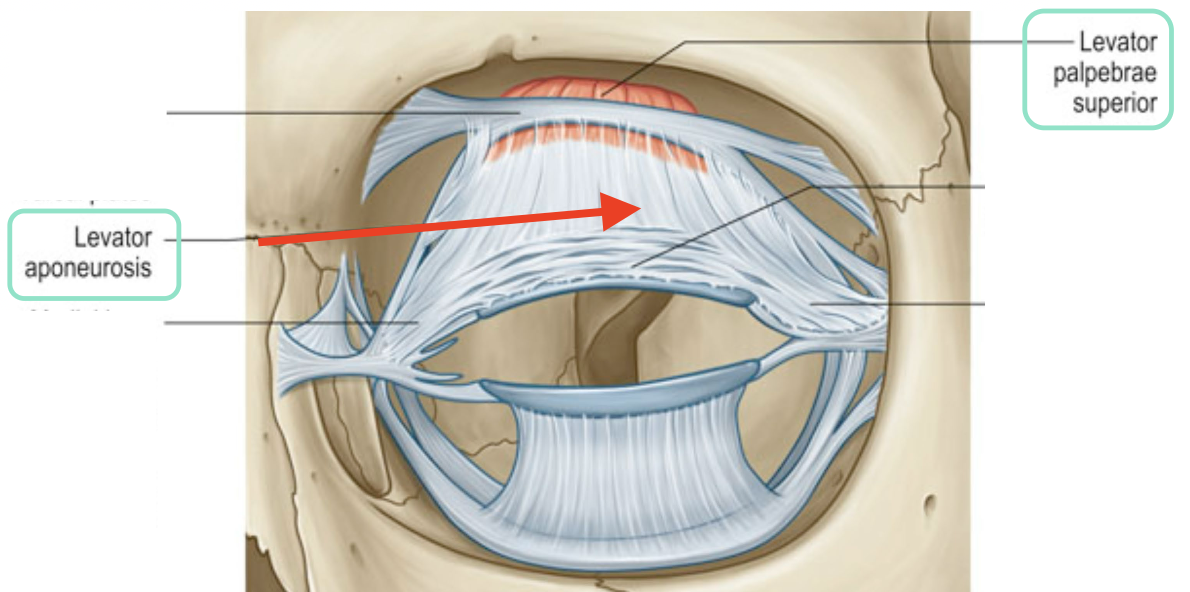
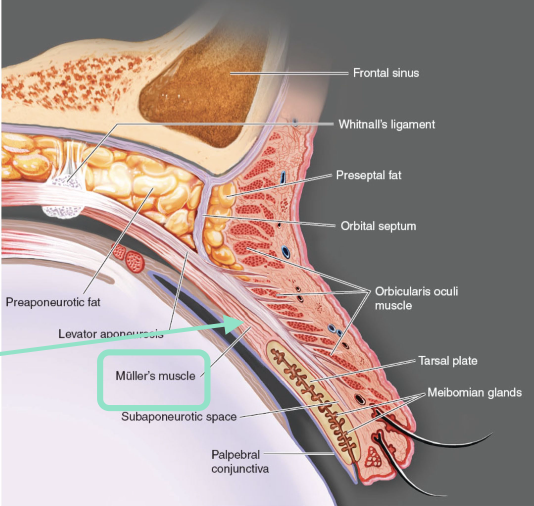
What connects the levator palpebrae superioris muscle to the eyelid at the tarsal plate?
Levator aponeurosis — this is a thin, flat sheet of CT (think of a “wide tendon”) found only in the superior tarsle plate (upper eyelid)
Function: distributes the upper eyelid pull evenly & prevents wobbling
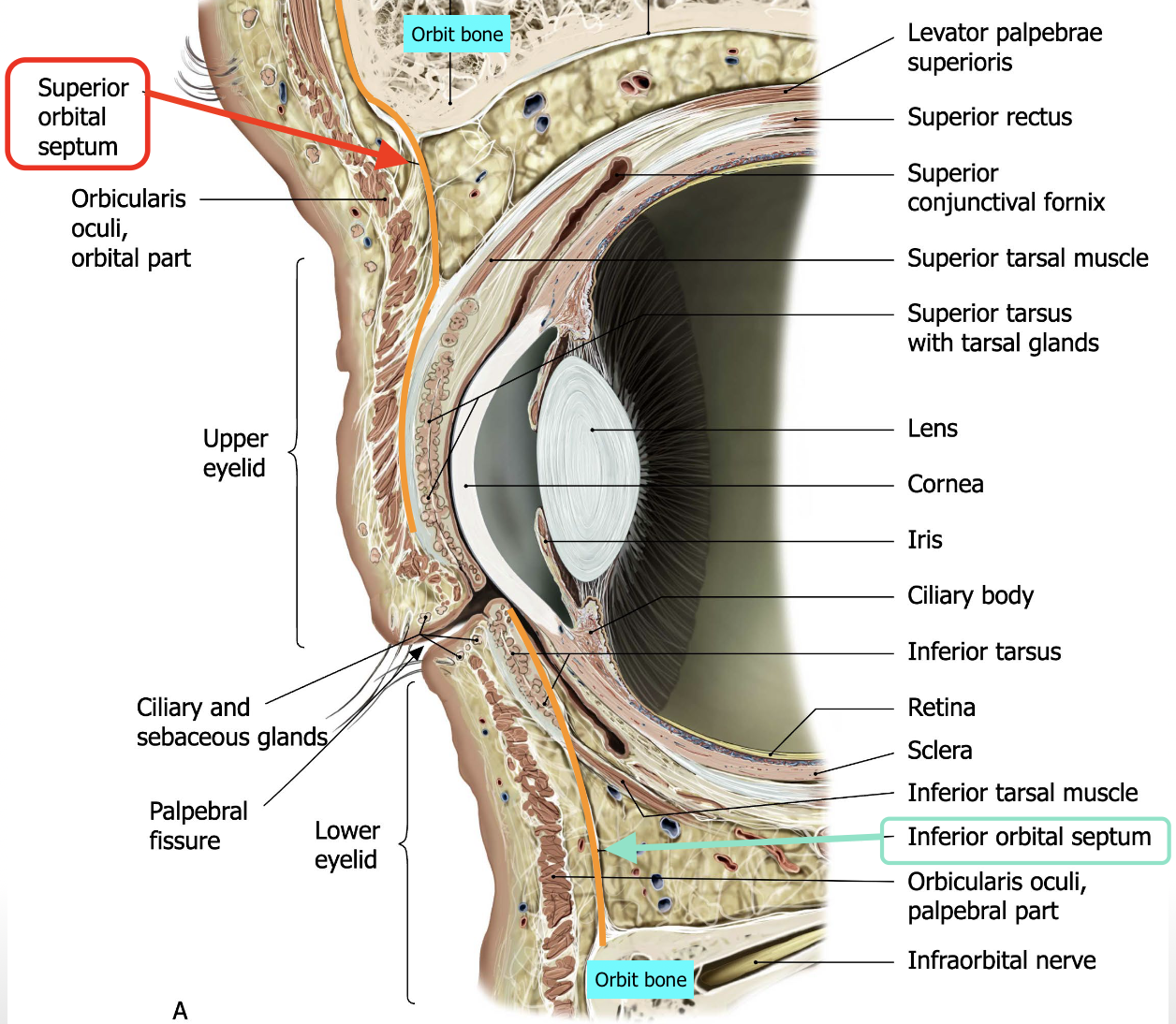
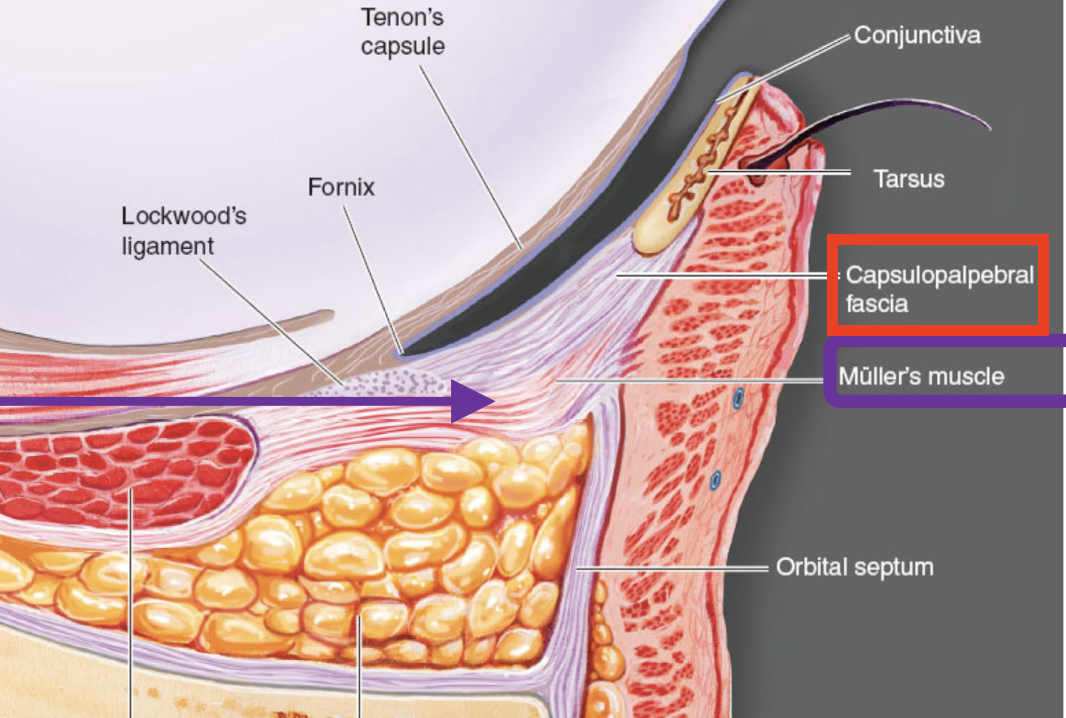
What is the Orbital Septum? Describe it’s structure and function.
→ fibrous membrane that starts at the orbital rim (bone) and extends down to the tarsal plate in each eyelid
this helps separate the eyelid from the orbit & prevents the spread of infection/swelling b/w them
sits behind the orbicularis oculi
- 2 types: Superior orbital septum (upper lid) & Inferior orbital septum (lower lid)
Define pre-septal cellulitis.
Infection in front of the orbital septum

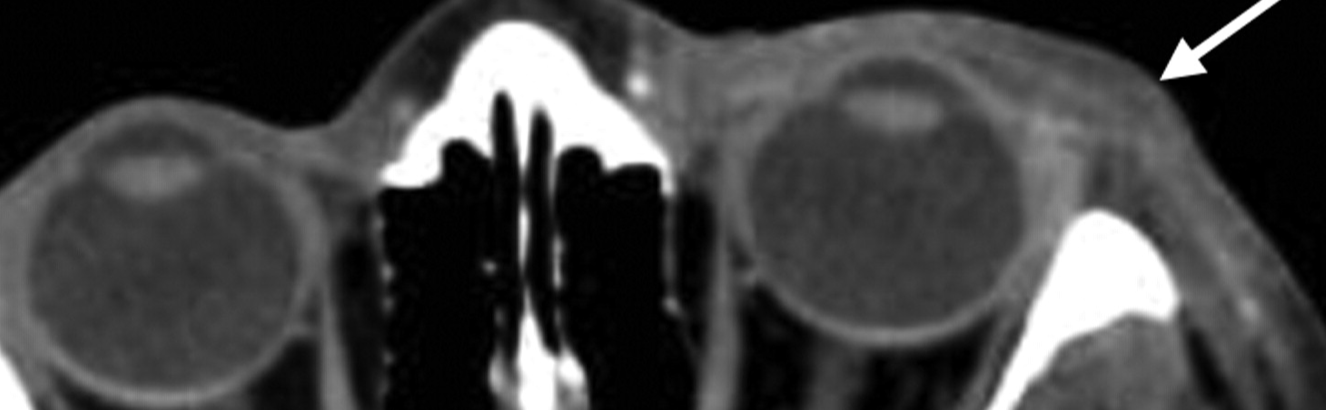
Define Orbital Cellulitis.
infection of the soft issues of the eye socket behind the orbital septum
this is bad b/c the orbit infections lead directly to the brain cavity

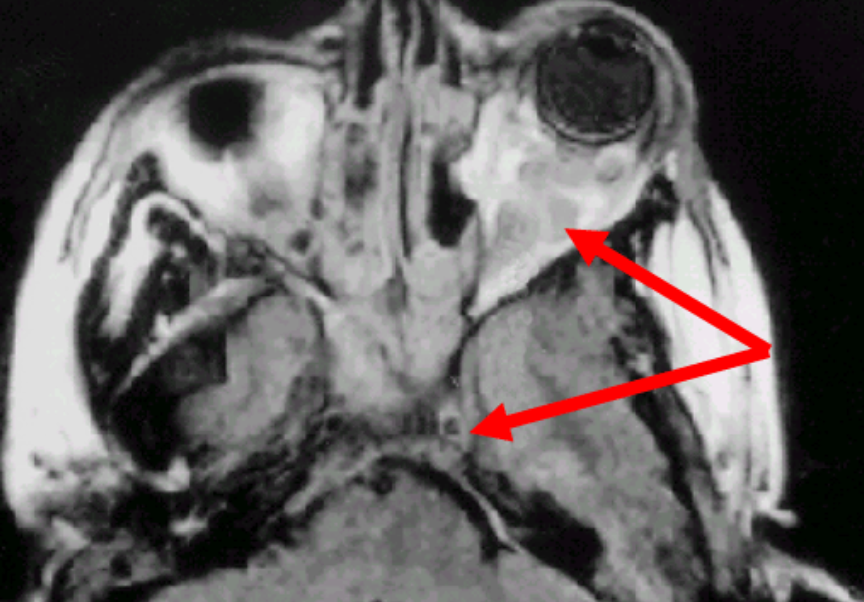
What is Müller’s Muscle?
Smooth muscle that’s innervated by post-ganglionic SNS fibres
aka: “superior/ inferior tarsal muscle”
For the upper lid, describe the Müller’s muscle’s:
origin
insertion
function
Origin: Interior surface of levator aponeurosis
Insertion: superior edge of the tarsal plate
Function: helps raise the upper lid
For the lower lid, describe the Müller’s muscle’s:
function
Function: helps lower the lower lid — “lid retractors”
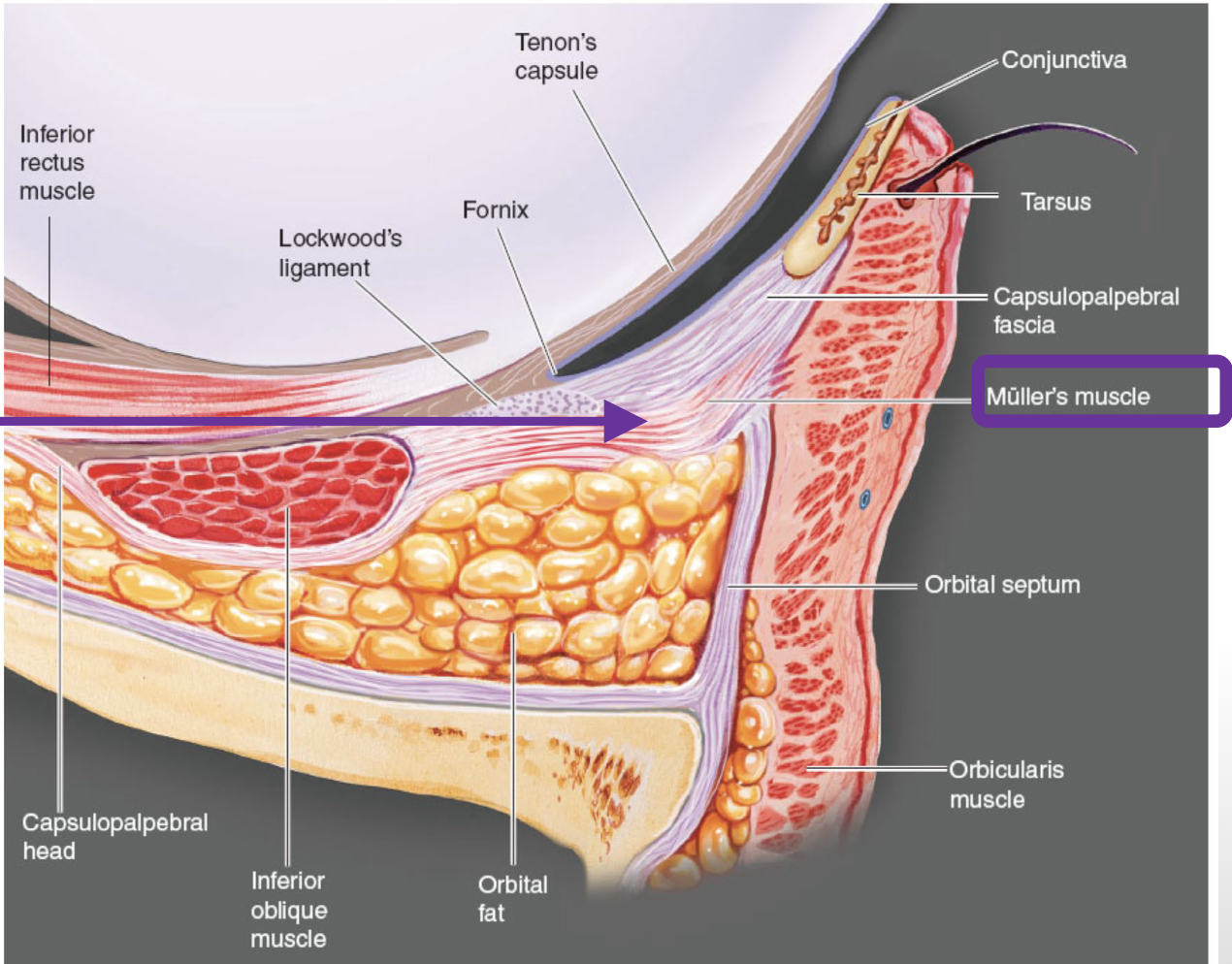
Why does the upper lid have more movement compared to the lower lid?
Lower lid has:
❌ skeletal muscle analogue of the levator palpebrae superioris
❌ aponeurosis
✅ capsulopalpebral fascia (fascial analogue, not a skeletal muscle analogue)
The eyelid has both ______ & __________ glands.
The eyelid has both unicellular & multicellular glands.
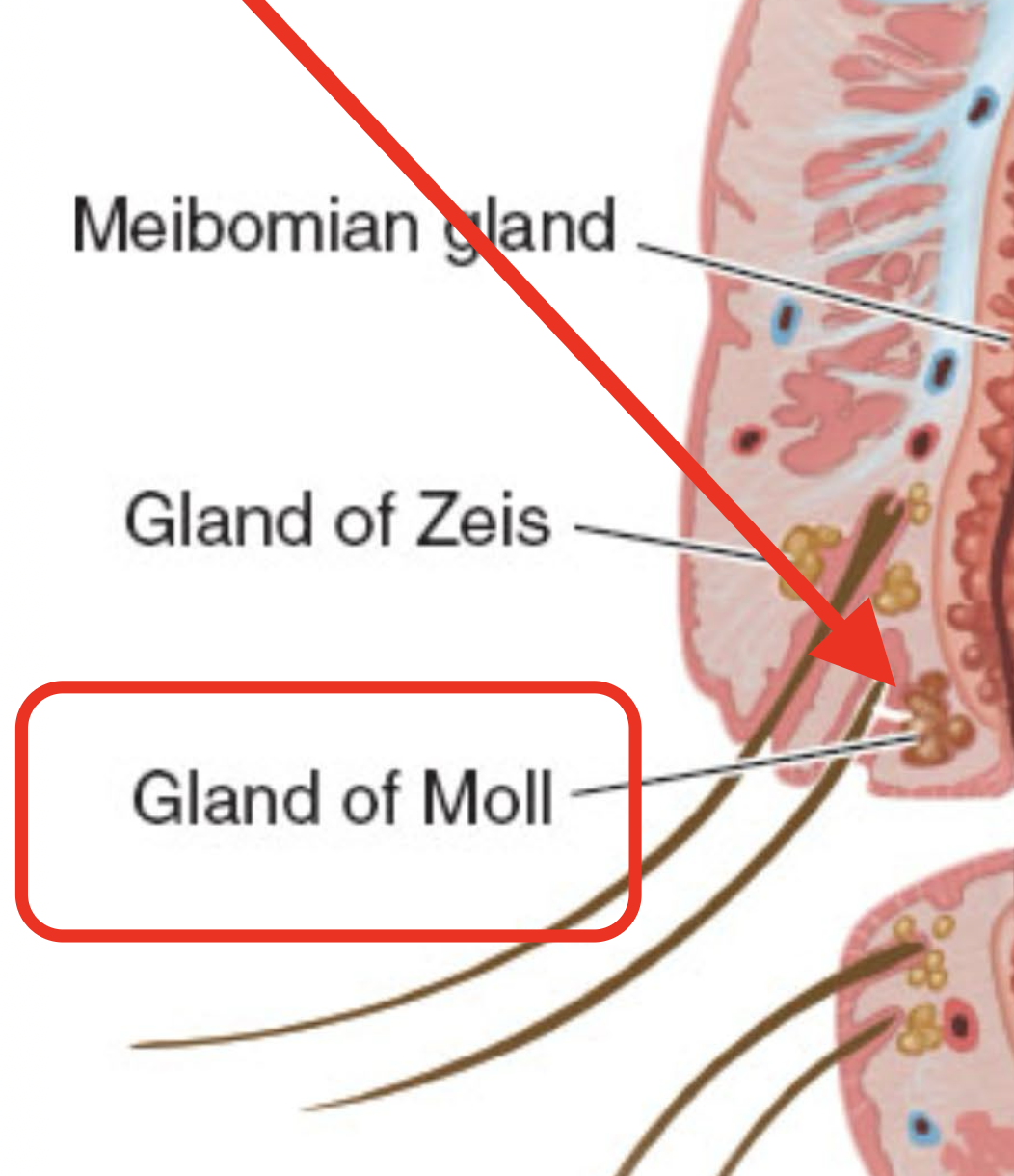
List the most important multicellular glands within the eyelids?
Meibomian glands
Glands of Zeis
Glands of Moll
Glands of Krause
Glands of Wolfring
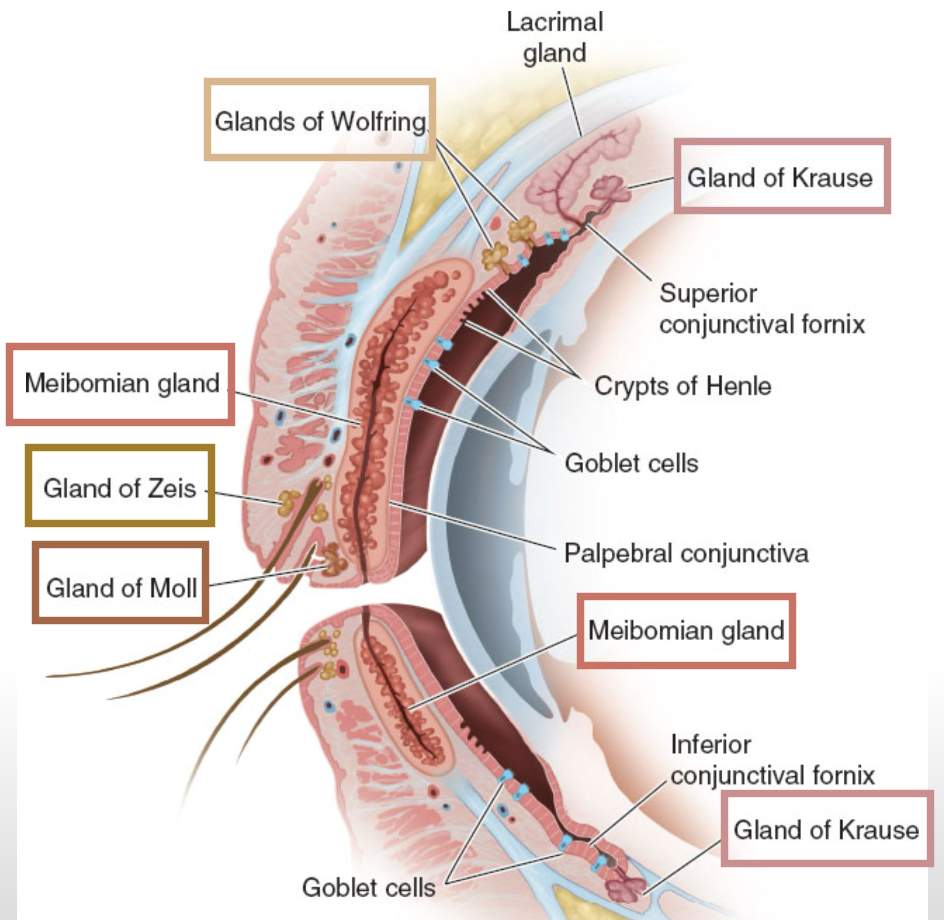
List the characteristics of Meibomian Glands.
→ produce meibum (clear, oily substance) that forms the outermost oily layer of the tear film
Structure: large, elongated sebaceous glands
Location: within the tarsal plates
associated with dry eyes
aka: Tarsal Gland
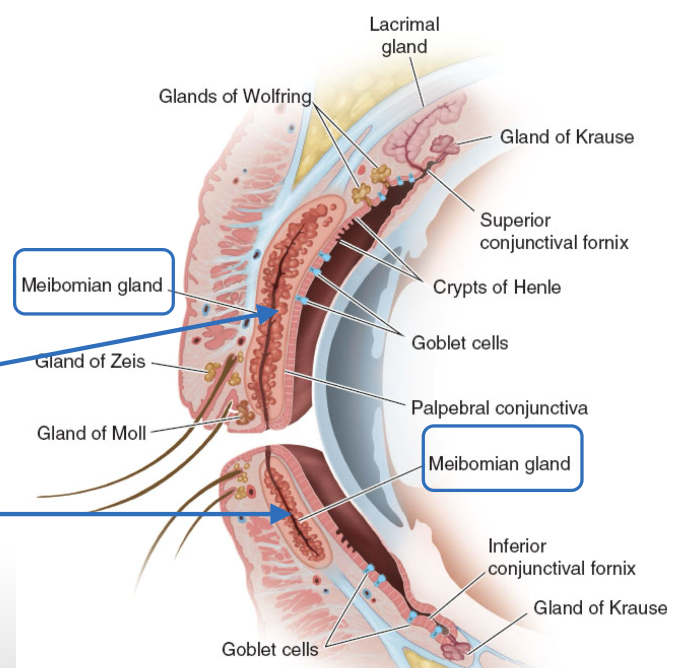
List the characteristics of the Glands of Zeis.
→ secrete an oily secretion that lubricates the eyelashes (upper and lower) as they grow
Structure: almost identical cell structure to meibomian glands
aka: Sebaceous Gland
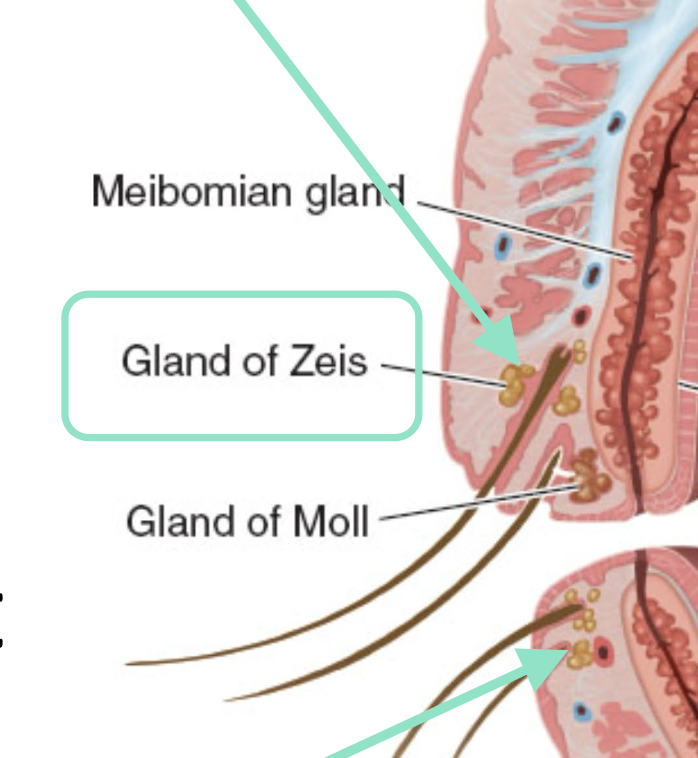
List the characteristics of the Glands of Moll.
→ have apocrine secretion + uncertain function
Structure: Simple tubular glands
aka: Ciliary sweat gland
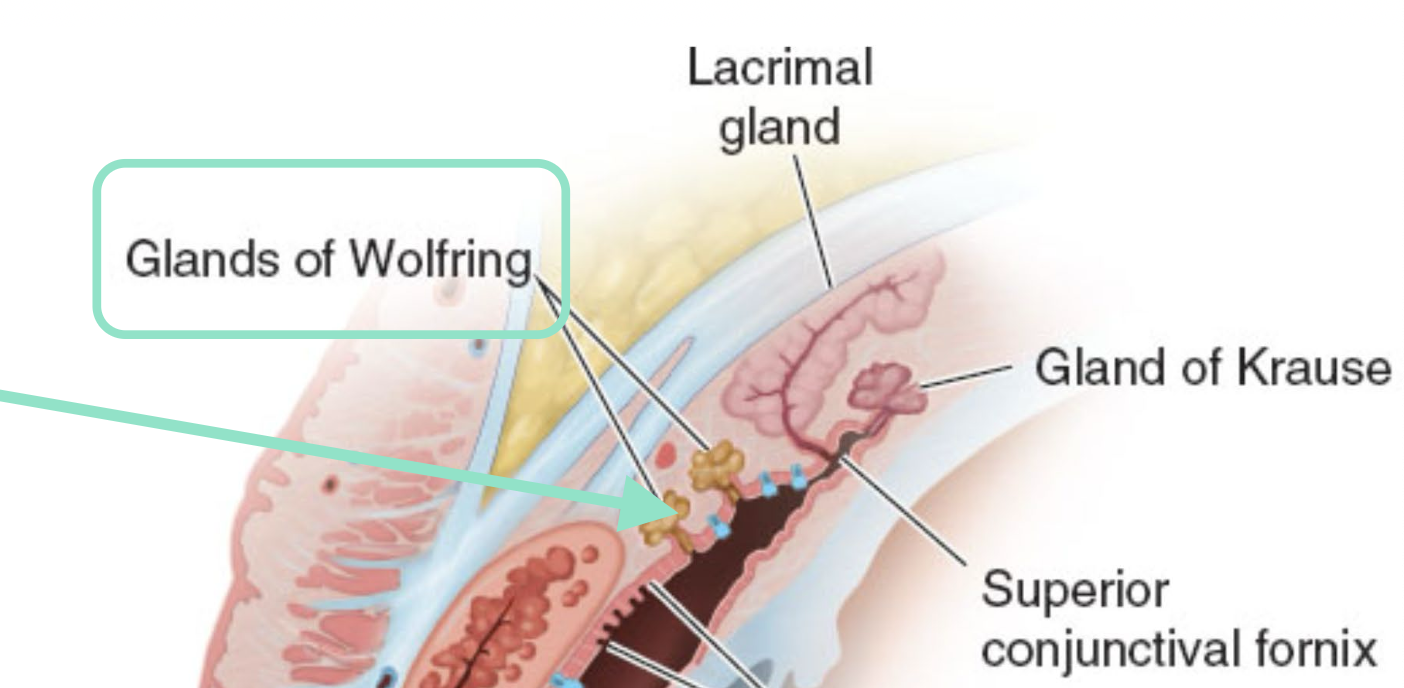
List the characteristics of the Glands of Kraus.
→ Secrete watery fluid that forms the aq layer of the tear film (secretion helps flush out debris or foreign material that may get trapped in the fornix)
Location: deep stroma and subconjunctival CT of the conjunctival fornix
Most are found in the superior fornix
Structure: same histology as the main lacrimal gland
aka: Accessory lacrimal gland
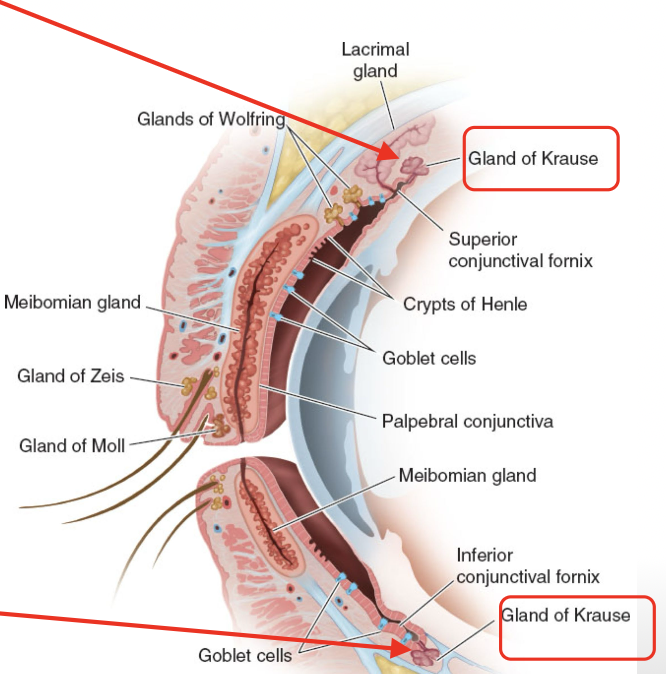
List the characteristics of the Glands of Wolfring.
→ contribute to the aq layer of tear film too
Note: These are the same as Glands of Kraus, they’re just located somewhere else
not as abundant as Glands of Kraus
Location on upper lid: in front of where the Müller’s muscle is inserted, along the superior edge of the tarsal plate
Location on lower lid: along the inferior edge of the tarsal plate
aka: Accessory lacrimal gland
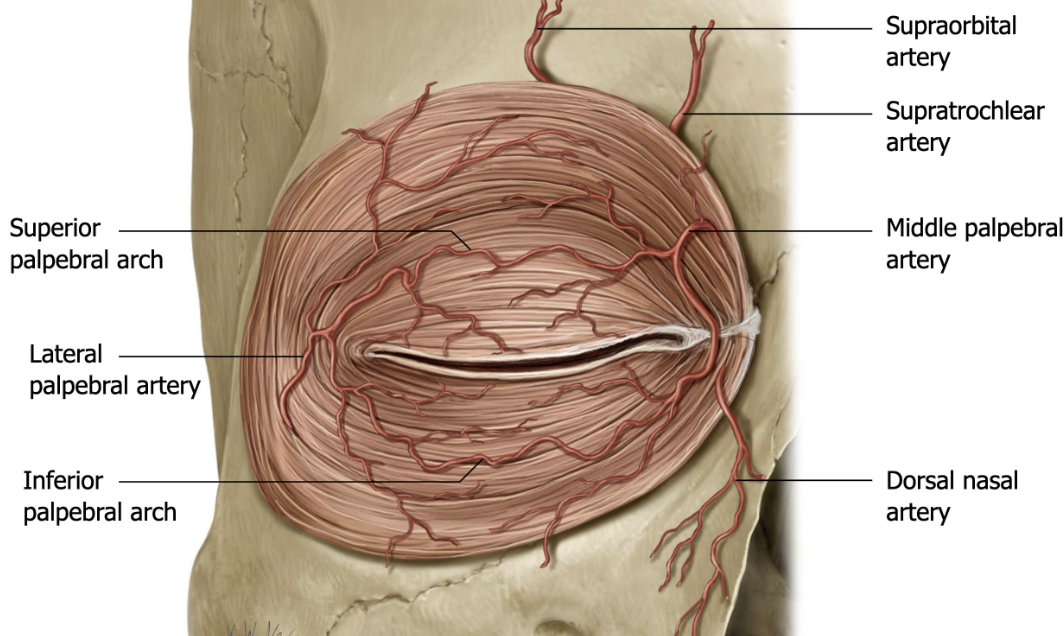
Define arcade.
connective networks of vessels that allow for constant blood flow with movement
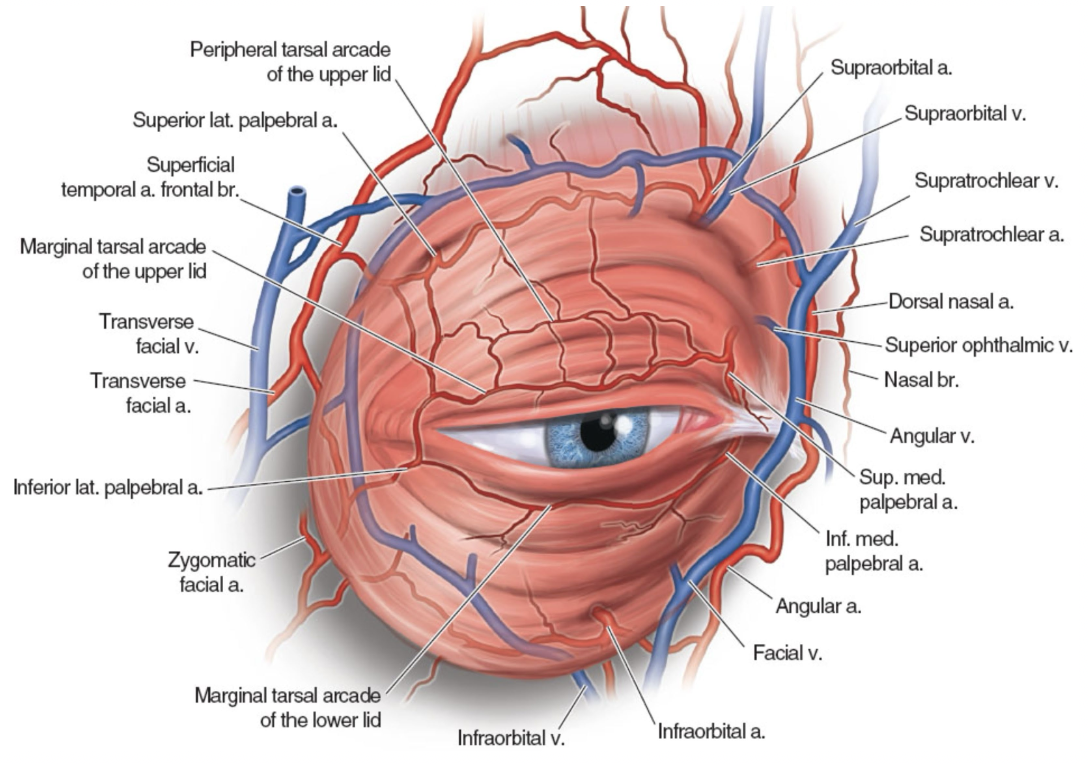
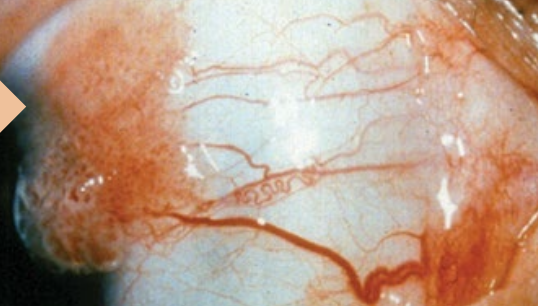
Describe the Arterial Supply of the Eyelids.
eyelids are richly vascularized
Main supply: Vascular arcades formed by the medial & lateral palpebral branches of the ophthalmic artery
Upper lid: 2 arcades
Lower lid: 1 arcade
Additional supply: Branches from the infraorbital, facial, transverse facial, and superficial temporal arteries
Define plexus.
venous version of arcades (connective networks of vessels that allow for constant drainage)
Describe the Vascular Supply of the Eyelids.
Veins form plexi in front of and behind the tarsal plate + near the superior and inferior fornices of the conjunctiva
Major drainage: superior and inferior palpebral vein
What nerves provide sensory innervation to the upper and lower eyelids?
→ ophthalmic (V1) and maxillary (V2) divisions of the Trigeminal nerve (CN V) innervate the eyelids
Upper eyelid: Mainly by the supraorbital branch of the frontal nerve (V1)
Lower eyelid: Mainly by the infraorbital branch of the maxillary nerve (V2)
What is lymph?
→ clear-to-white fluid made of WBC
part of the body’s immune system, helping to drain waste, fats, and bacteria
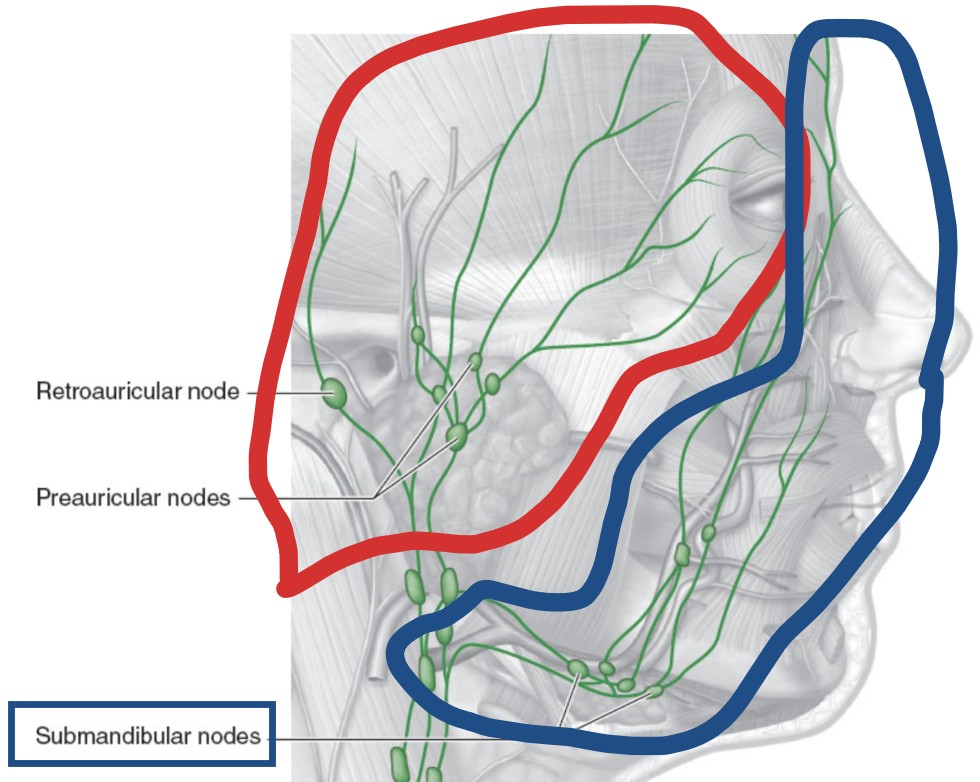
Where do the lymphatics from the lateral portions of the eyelids drain?
Lateral 2/3 of upper lid + lateral 1/3 of lower lid drain into → preauricular (superficial parotid) lymph nodes
pre-auricular = ear
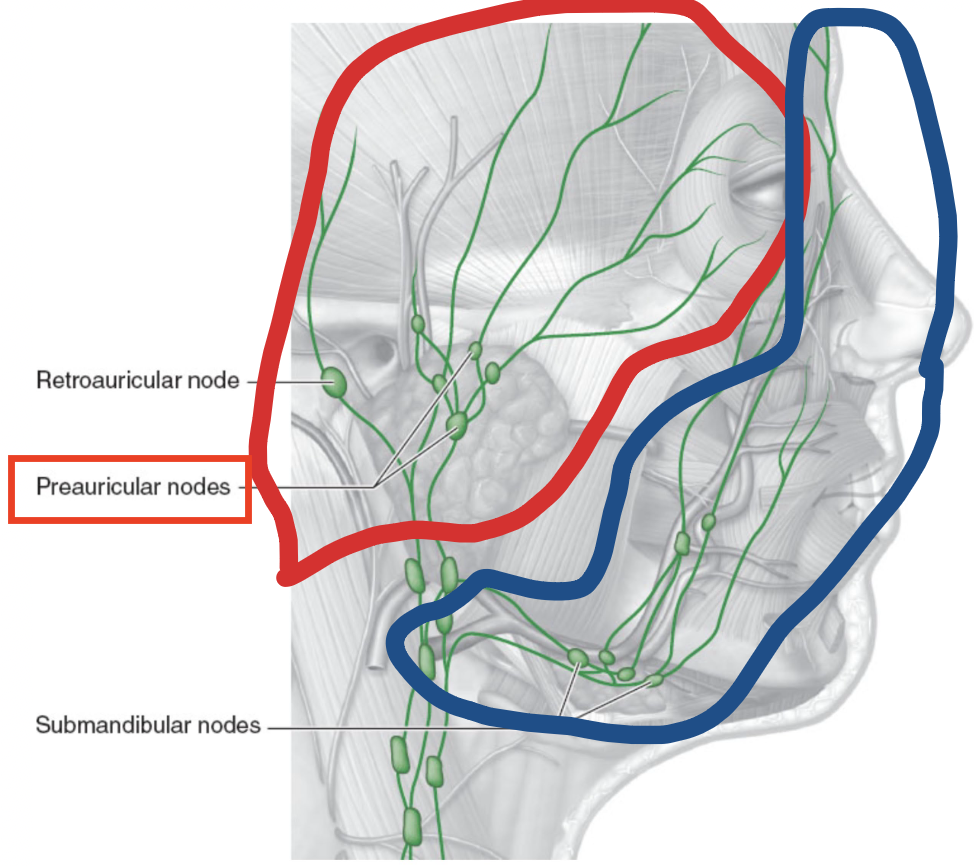
Where do the lymphatics from the medial portions of the eyelids drain?
Medial 1/3 of upper lid + medial 2/3 of lower lid follow the facial vein to drain into → submandibular lymph nodes
submandibular = directly under chin
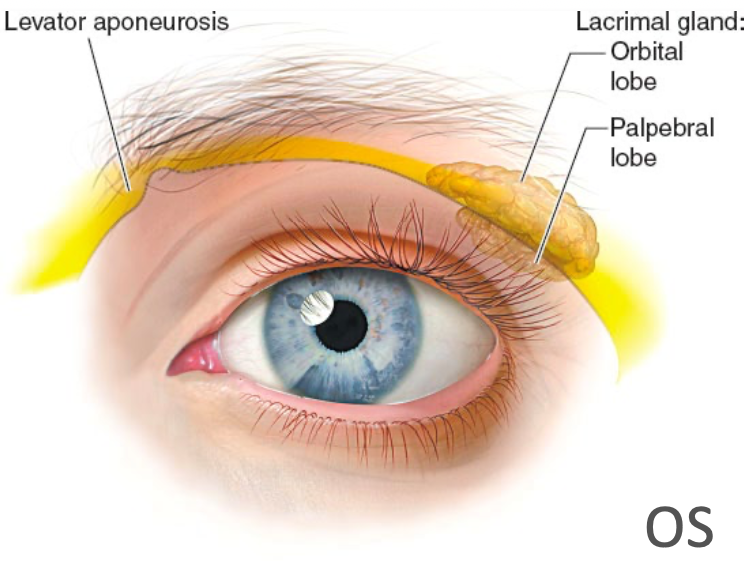
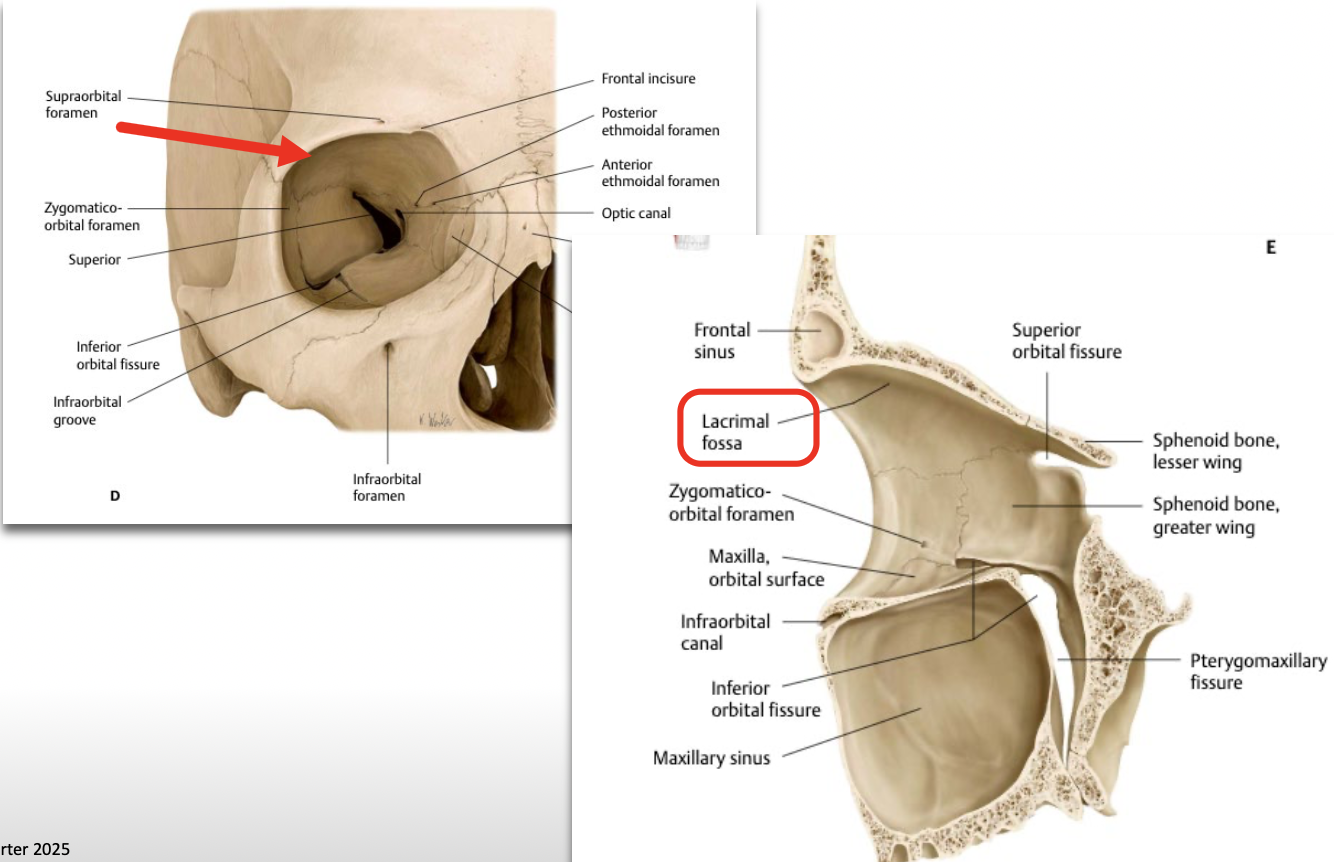
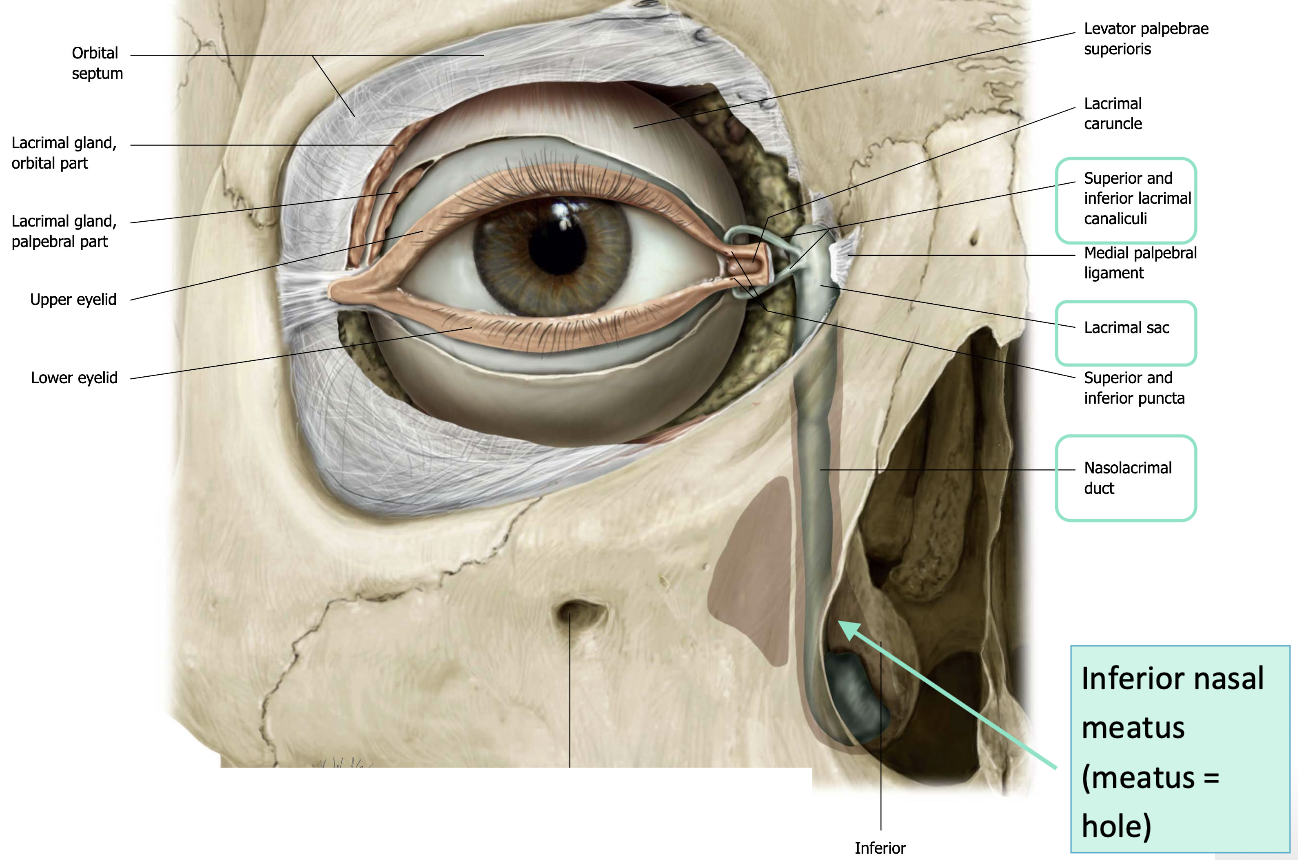
Where is the lacrimal gland located?
behind the lateral aspect of the superior orbital rim
What does the lacrimal system include, and what are its main components?
→ production & drainage of tears
Tear production: Main + accessory lacrimal glands
Main - makes 90% of tears
Accessory (Krause & Wolfring) - makes 10% of tears
Tear drainage: via the paired lacrimal canaliculi, lacrimal sac & nasolacrimal duct which convey tears into the nasal cavity
Outline the characteristics of the Lacrimal Gland.
→ Almond-shaped (~2 cm) gland that’s the 1er producer of the aq layer of the tear film
when produced in excess, the overflowing fluid → tears
watery fluid secretion w/ an electrolyte content similar to plasma
fluid moistens & lubricates the surfaces of the conjunctiva and cornea + provides nutrients & dissolved O2 to the cornea
Location: lies in the fossa for the lacrimal gland in the superolateral part of each orbit
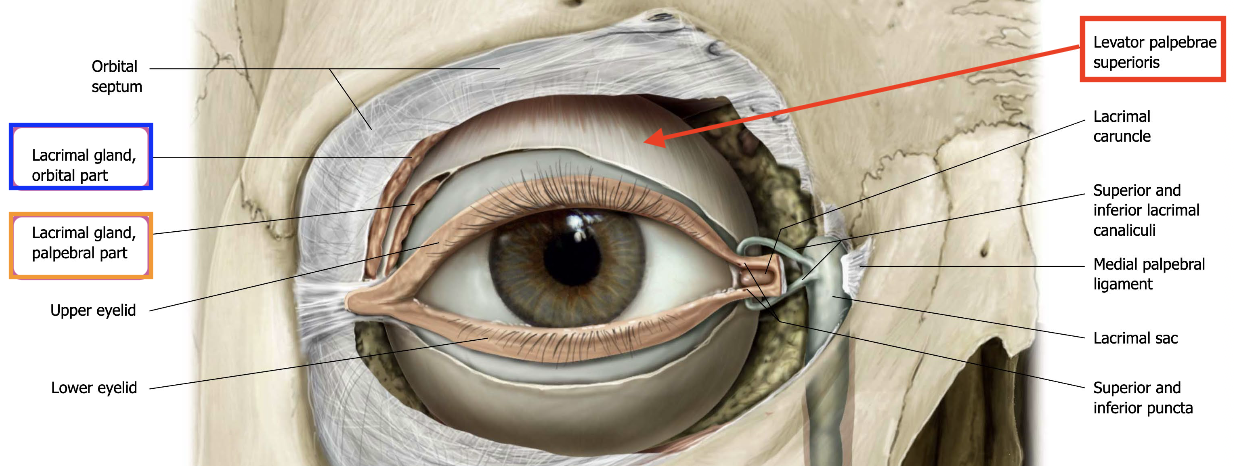
What is the lacrimal gland divided into?
Divided into → Superior orbital & Inferior palpebral lobe
by the lateral expansion of the levator aponeurosis as it spreads into the eyelid from the orbit
aponeurosis cuts right through the middle of these lobes
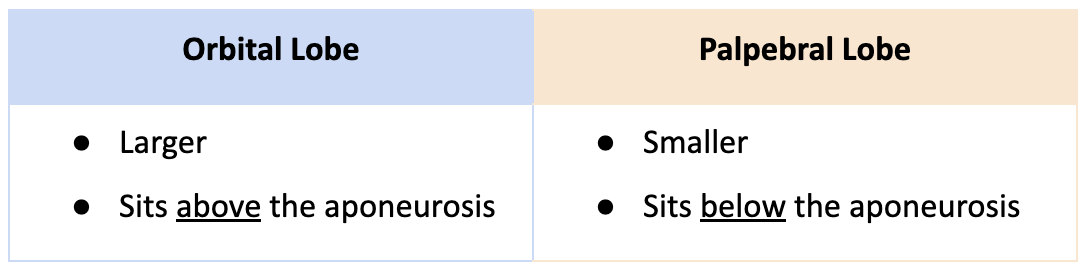
Compare the Superior orbital & Inferior palpebral lobes.
How can the inferior palpebral lobe of the lacrimal gland be easily visualized?
by pulling the upper lid superiorly and laterally
What happens if the lacrimal gland expands due to a tumor?
it can compress the orbital contents

Where do the secretory ducts of the lacrimal gland drain?
12 secretory ducts from the lacrimal gland drain into → superior fornix (fornix of conjunctival sac)
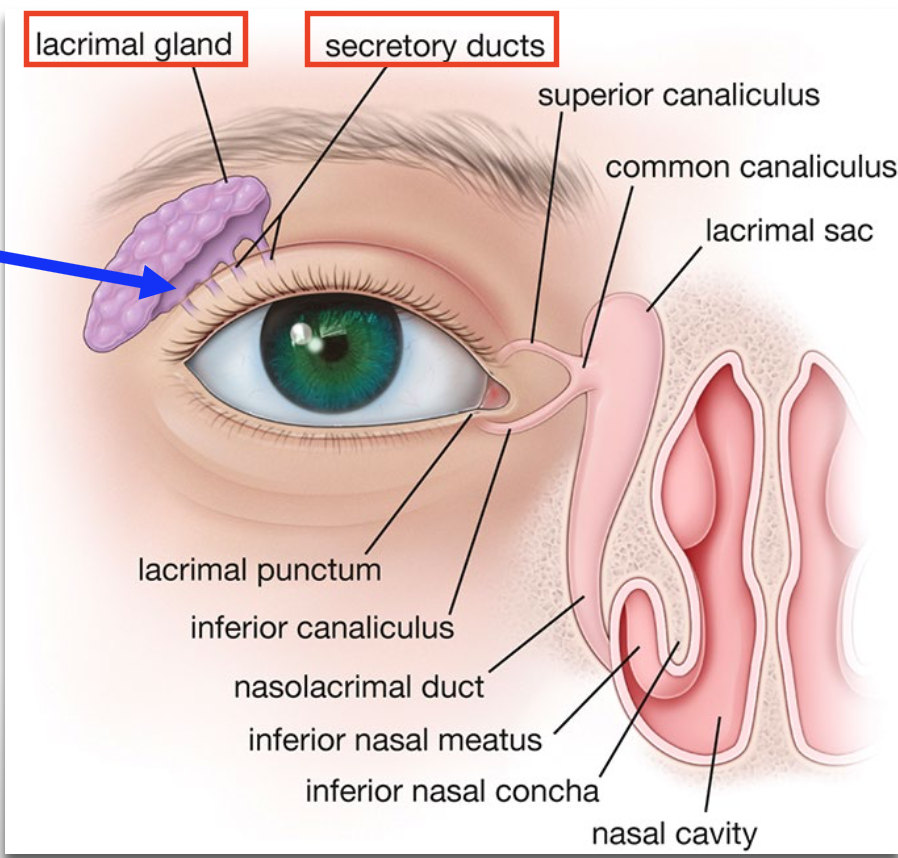
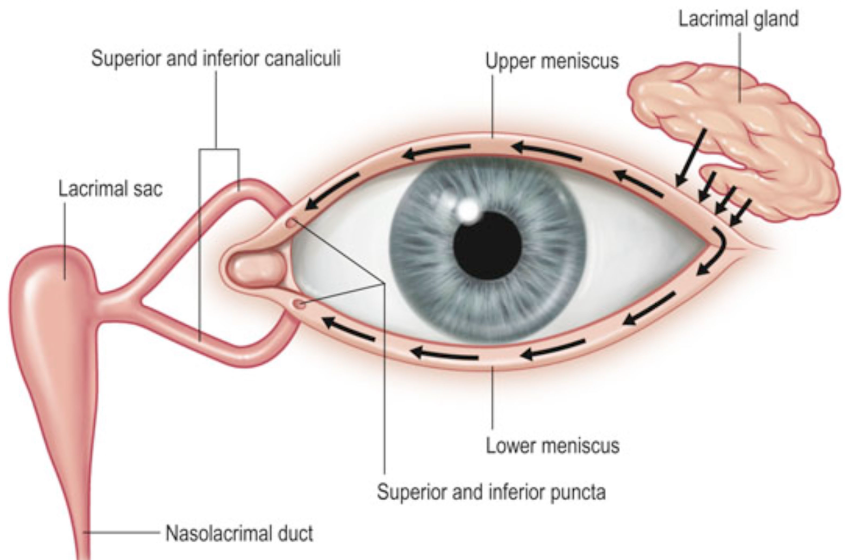
Trace the pathway of lacrimal fluid drainage and explain how blinking assists in this process.
Blinking (temporal → nasal) pushes tears across the eye toward the drainage openings
1) Tears accumulate in lacrimal lake
2) Reach the Inferior lacrimal punctum (ILP)
3) Drain from ILP into superior & inferior lacrimal canaliculi
4) Canaliculi carry fluid into lacrimal sac, where the orbicularis oculi pulls fluid into the sac
5) From the sac, fluid drains into inferior nasal meatus (hole) of nasal cavity via the nasolacrimal duct
6) Fluid flows posteriorly, across the floor of the nasal cavity to the nasopharynx (back of nose/throat)
7) Fluid is eventually swallowed after cleansing conjunctival sac
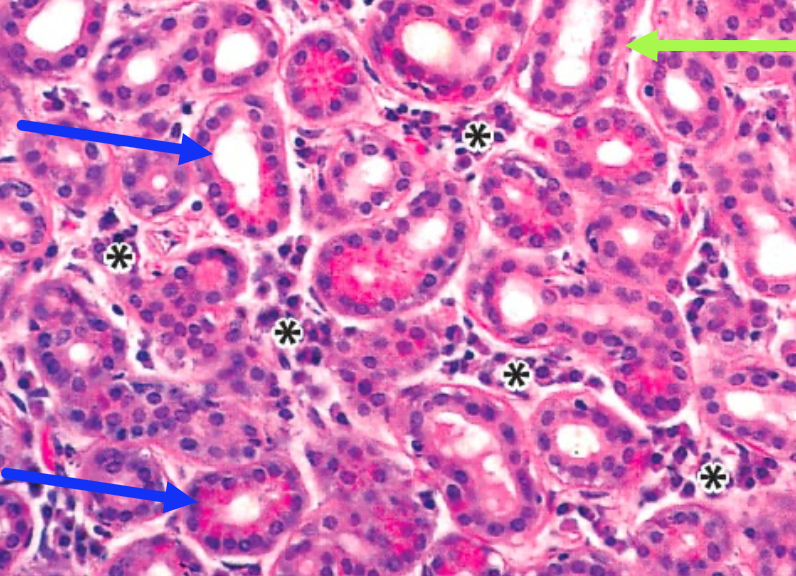
Describe the histology of the Lacrimal Gland.
Compound tubuloacinar gland — made up of many acini arranged into lobules (empty spaces) with large lumen that are separated by an interstitial fibrovascular matrix (loose CT)
acini are lined by columnar secretory cells and partially surrounded on their basal surface by a discontinuous ring of myoepithelial cells
myoepithelial cells help release tears
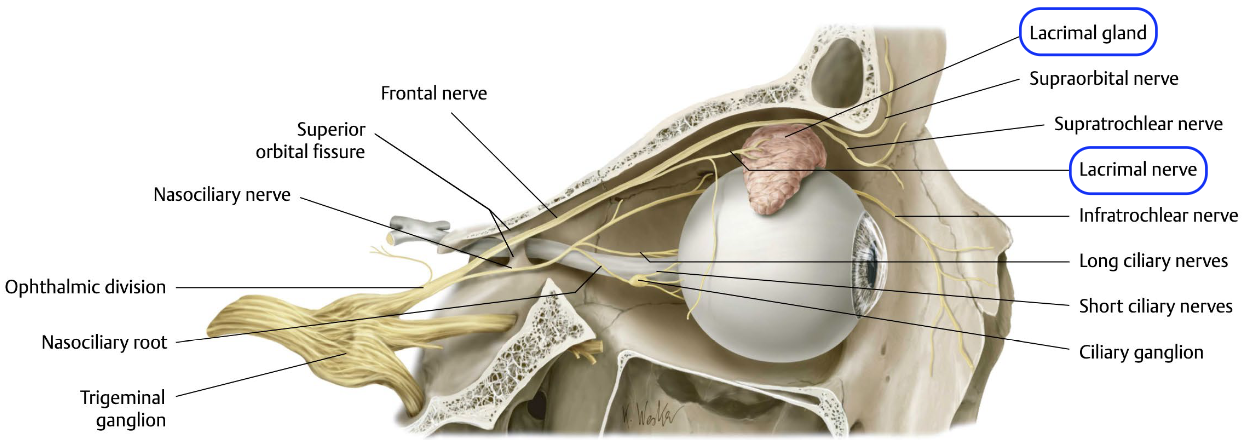
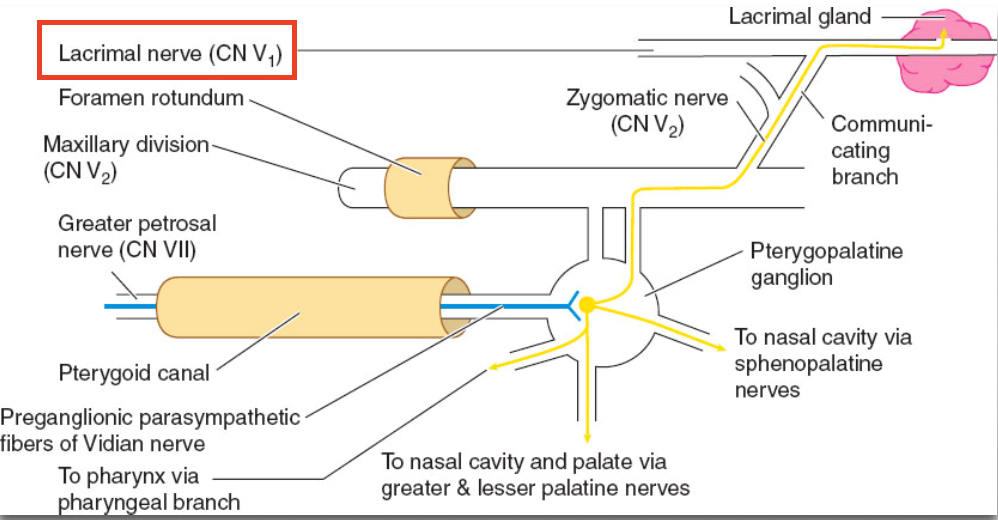
How is the lacrimal gland innervated?
Lacrimal nerve (a branch of the ophthalmic division of CN5 – V1) carries PNS, SNS & sensory fibres to the gland
Sensory fibers - come directly from CN5
Autonomic (PNS, SNS) fibers - join the lacrimal nerve after it branches from the main trunk of the ophthalmic division (V1)
What is the arterial supply to the lacrimal gland?
receives blood supply from the lacrimal artery (a branch of the ophthalmic artery)
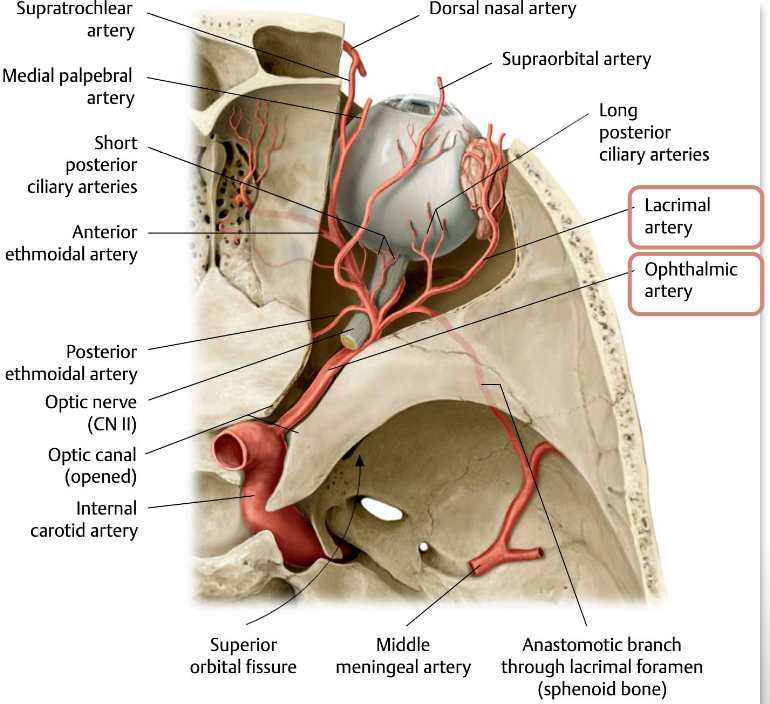
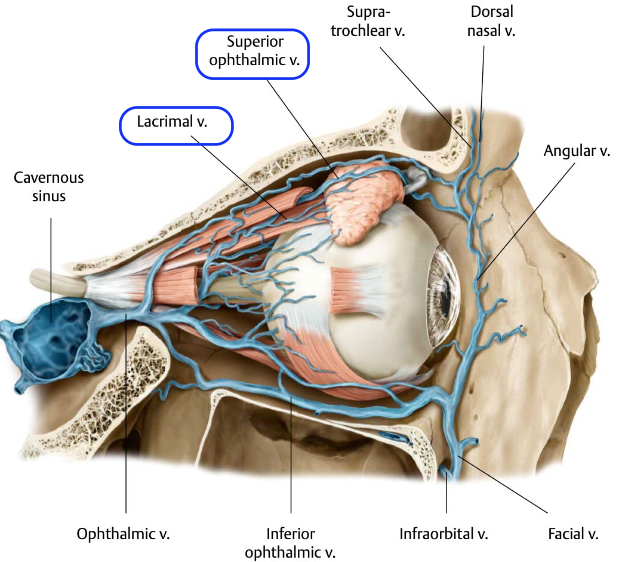
What is the venous drainage from the lacrimal gland?
drains blood via the lacrimal vein, which joins the superior ophthalmic vein
What are the key dimensions and properties of the cornea?
Corneal size
Corneal shape
Central thickness
Limbal thickness
Central radius of curvature
Average surface power
Size: Nearly adult size at birth
Shape: Slightly wider (11.7 mm) than tall (10.6 mm) → not a perfect circle
Central thickness: ~0.52 mm (520 µm)
Thinner corneas (common in African ancestry) ↑ glaucoma risk
Limbal thickness: ~0.67 mm
Central radius of curvature: 7.6–7.7 mm
Average surface power: Anterior: +49 D; Posterior: –6 D; Net: +43 D
Define Microcornea.
Abnormally small corneas → ranges from 7-10 mm
Define Megalocornea.
Abnormally large corneas → >12mm in neonate & >13 mm in adult

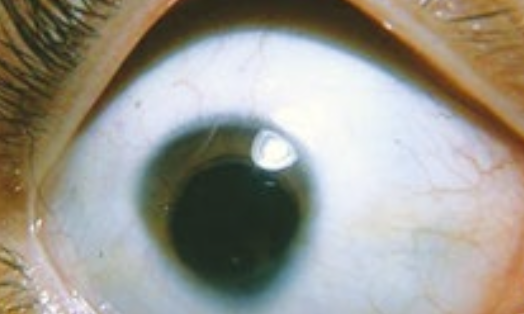
→ radius of curvature (7.6-7.7) differs b/w the vertical and horizontal meridians
difference b/w these curvatures = amount of astigmatism
cornea is steeper (shorter radius) vertically than horizontally — “with-the-rule” astigmatism
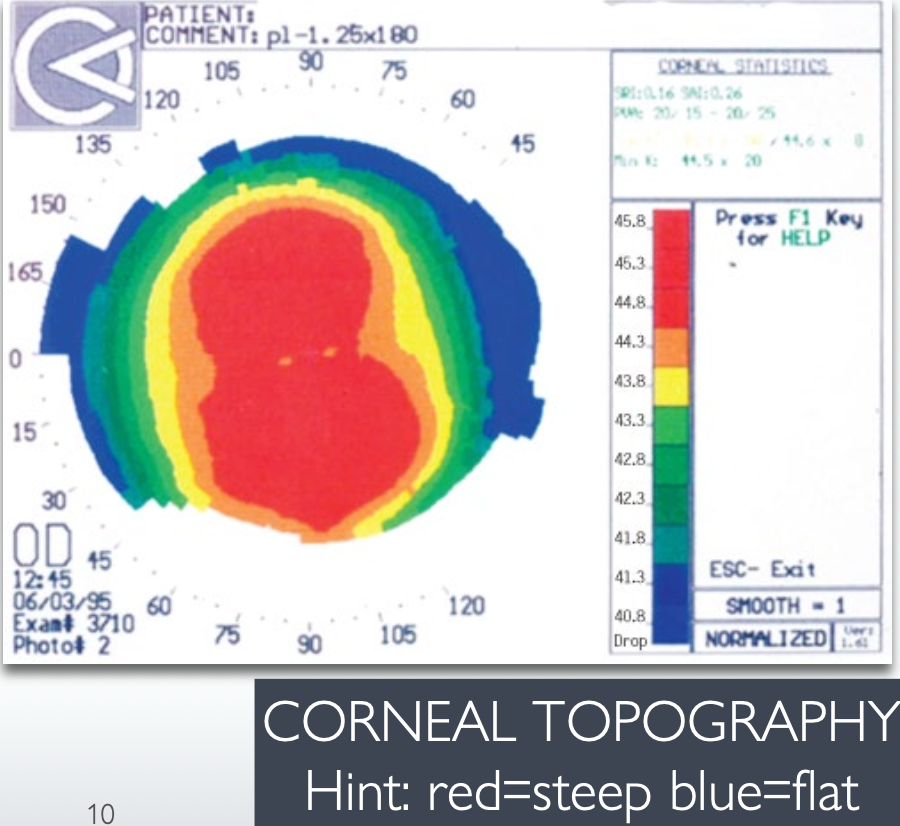
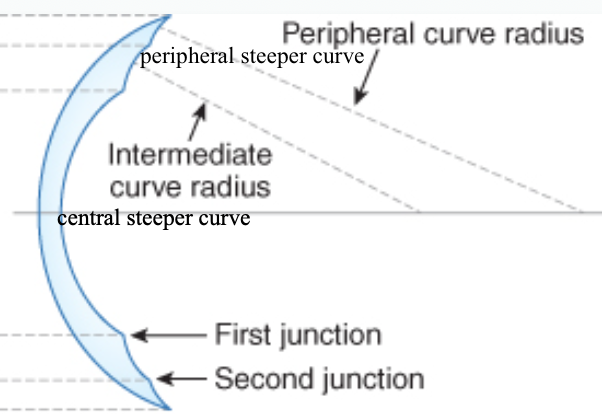
What does it mean that the cornea is aspherical?
→ means corneal curvature changes from center to periphery (not a perfect sphere)
steeper centrally (red zone) and flatter peripherally (blue zone)
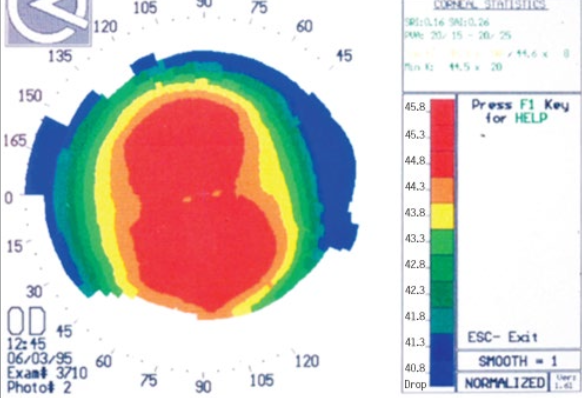
Contact lens are designed with progressively flatter curvatures, starting from the central (base) curve to the peripheral curves at the edges
How does an aspherical cornea affect contact lens design?
to match the corneal shape, contacts lens gradually flatten from the center to the edge
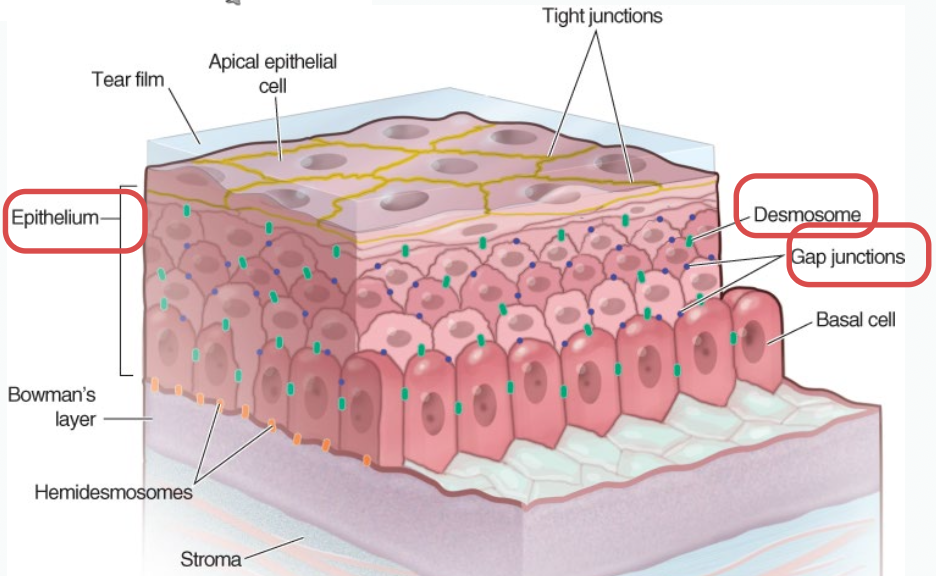
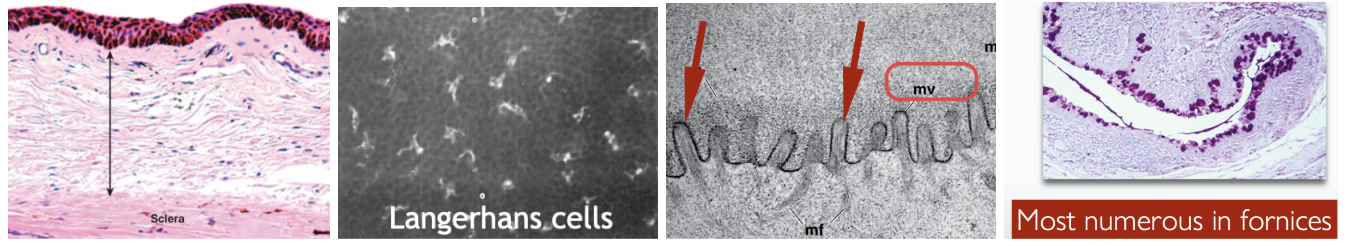
What are the characteristics of the Corneal Epithelium?
→ Non-keratinized, stratified squamous epithelium
Central cornea is made up of 5-7 layers:
Surface squamous cells: 2–3 layers
Wing cells: 2–3 layers
Basal cells: 1 layer, columnar
Peripheral cornea - has Langerhan cells (not in central cornea or else we can’t see)
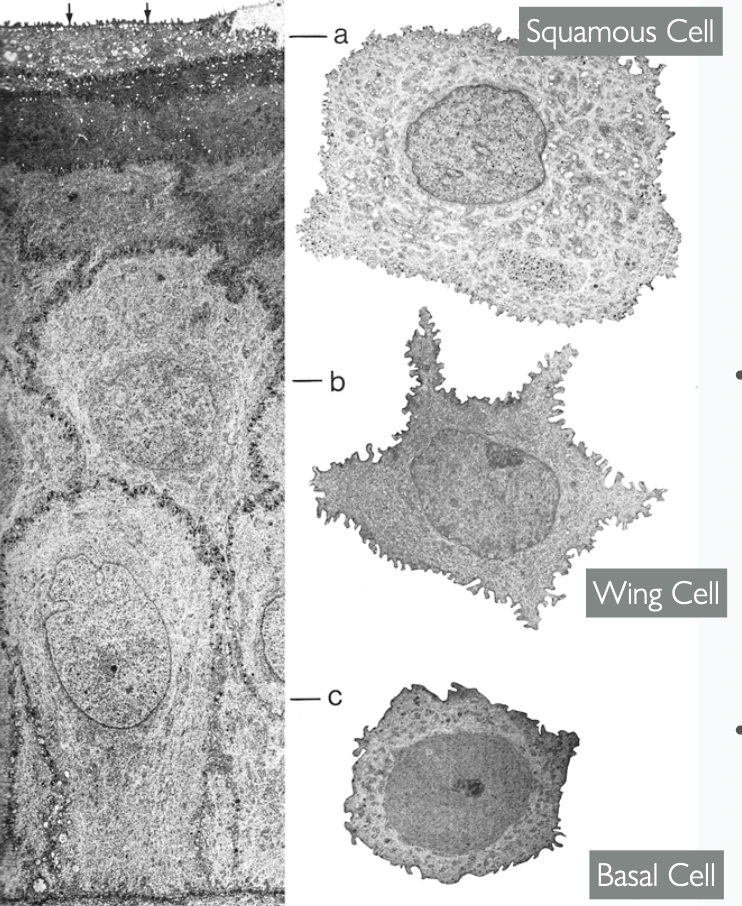
How are Wing cells are attached to eachother?
How do these junctions change as the Wing cells mature into surface squamous cells?
→ attached via desmosomes & gap junctions
Wing cells move toward the surface → flatten → surface squamous cells
Surface squamous cells develop tight junctions (TJ) b/w them
TJs act as a permeability barrier for the corneal epithelium
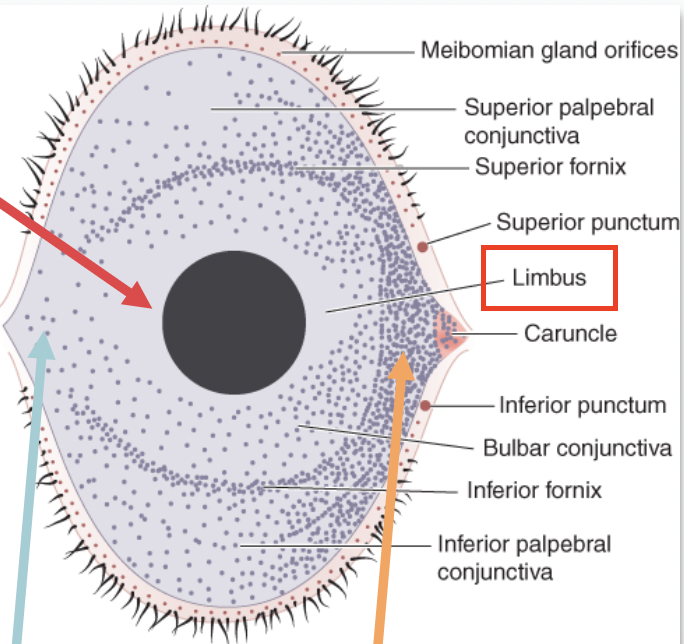
Where are stem cells for the corneal epithelium located?
Limbus — from here, stem cells migrate to the rest of the cornea
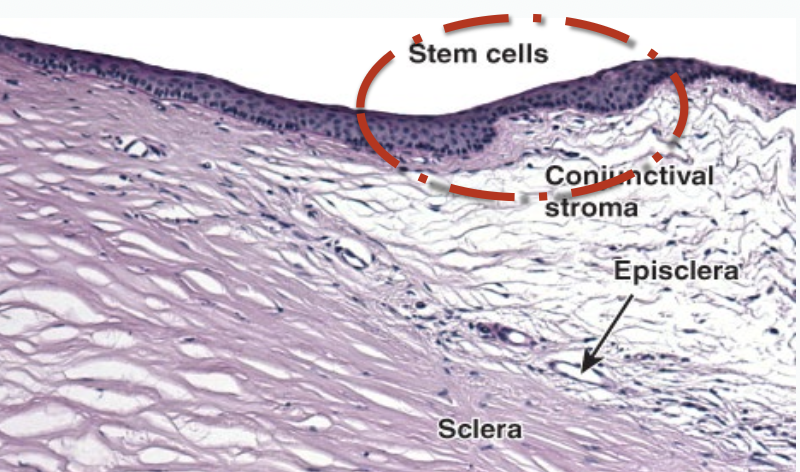
What is the most common site for corneal epithelial malignancies? Why?
Limbus!
b/c it’s the regions with the most epithelial cells
How do corneal epithelial stem cells divide and migrate?
1) Stem cells in the limbus produce transient amplifying cells
2) These move in a vorticeal pattern into the basal layer
Vorticeal - move inward towards the centre in a swirl pattern
3) Some basal cells may further divide
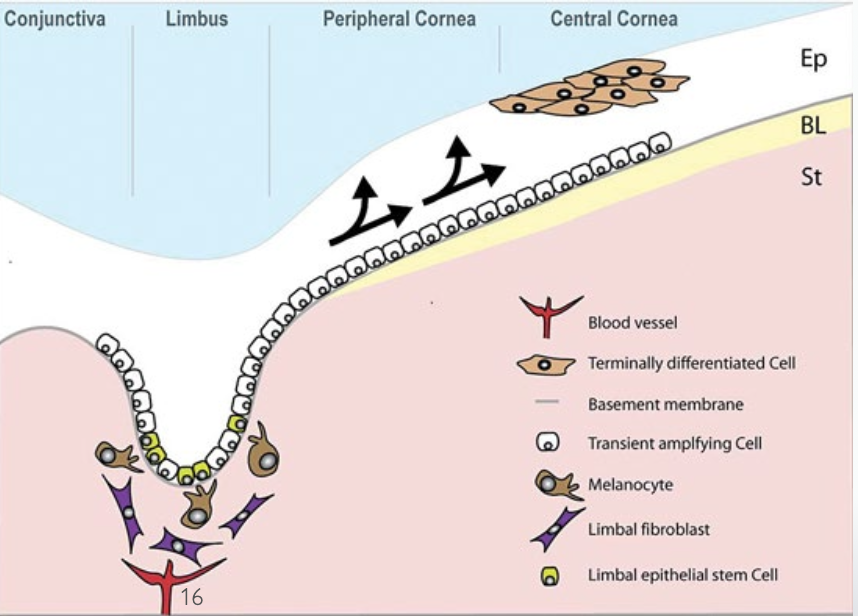
Why do limbal stem cells move in a Vorticeal pattern?
b/c it helps evenly distribute new cells across the corneal surface and maintain a smooth epithelium
How often does the complete epithelium turn over?
7-10 days
Vortical keratopathy is a condition where the corneal epithelium develops pigmented or deposit lines in a swirl (vortex) pattern. Which conditions can cause vortical (swirl) pigmented deposits in the cornea?
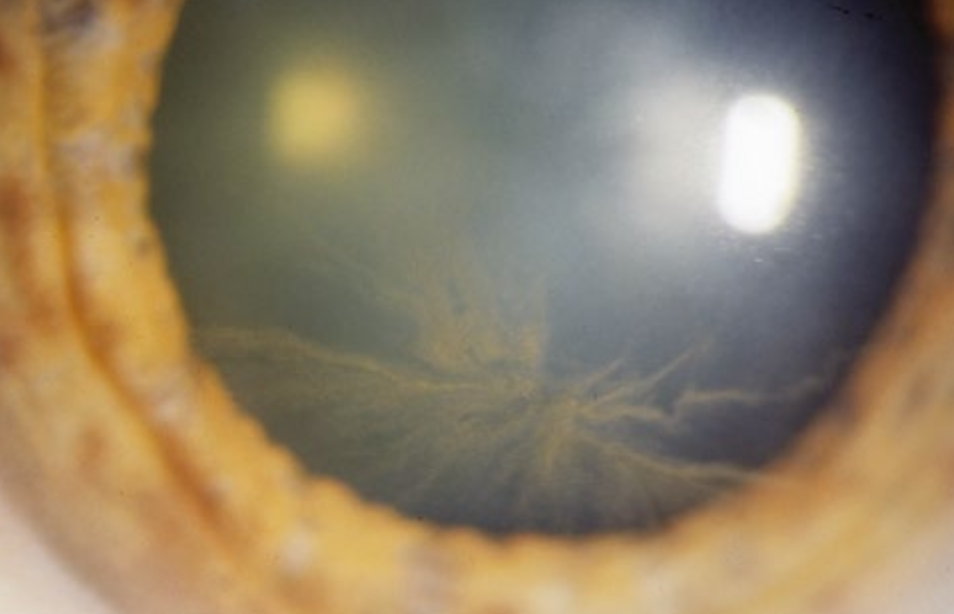
Metabolic diseases: Fabry’s disease
Medications: Amiodarone
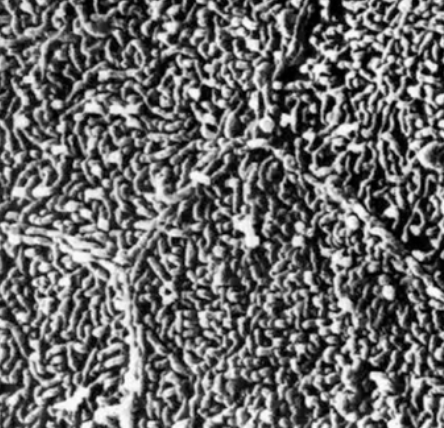
What do corneal surface cells develop to hold the tear film?
Microplicae — holds tears to the tear film on a micron level and prevent tears from just falling straight down
List the characteristics of the Tear Film 💧.
Thickness: 3 μm
Protective functions: Lubricant & antimicrobial
Vision Function: 1st optical surface of the eye (the 1st thing light travels through)
Index of refraction: 1.336
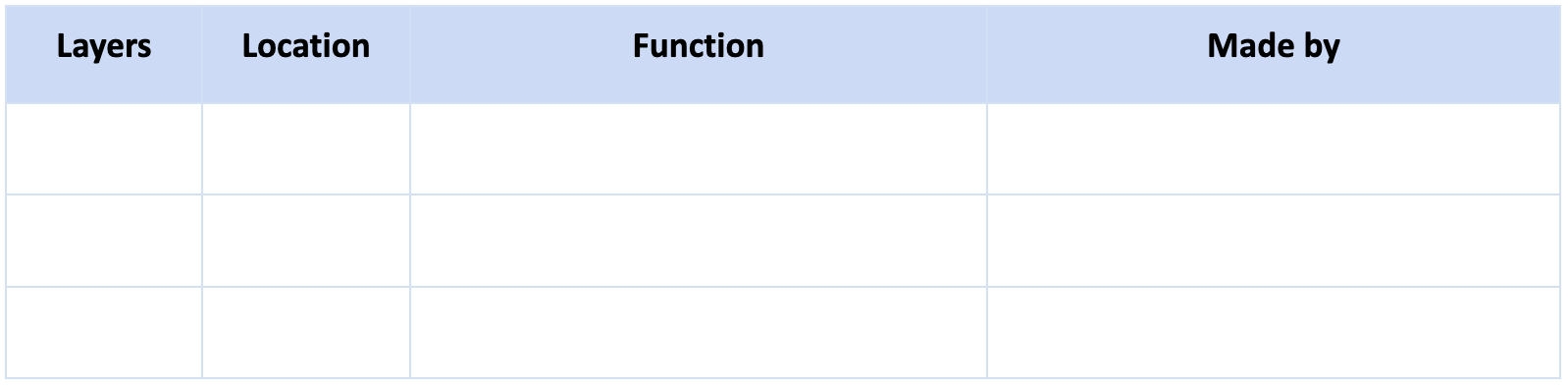
List the 3 layers of the tear film. Fill out this table.
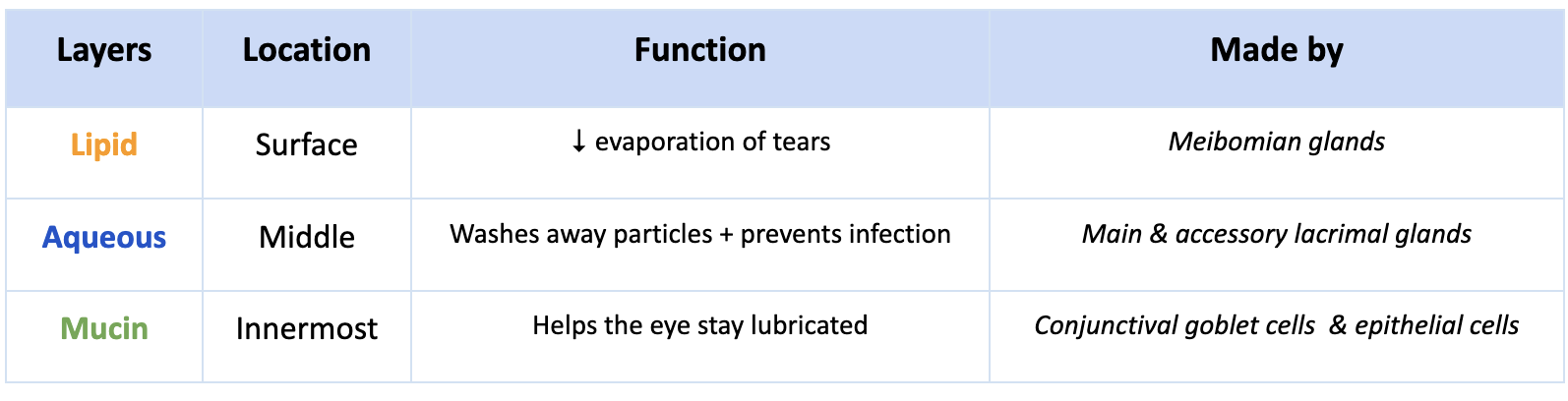
What is the largest cranial nerve? What are its divisions?
Trigeminal nerve (CN V)
3 divisions (“tri”)
Ophthalmic (V1)
Maxillary (V2)
Mandibular (V3)
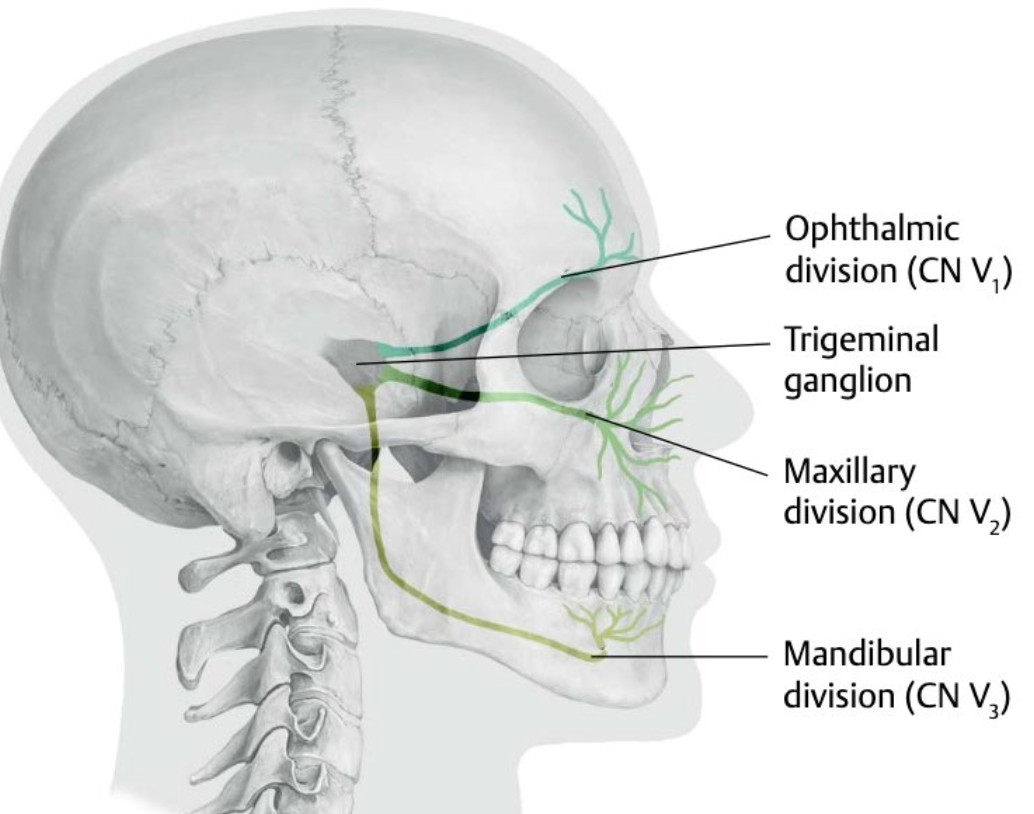
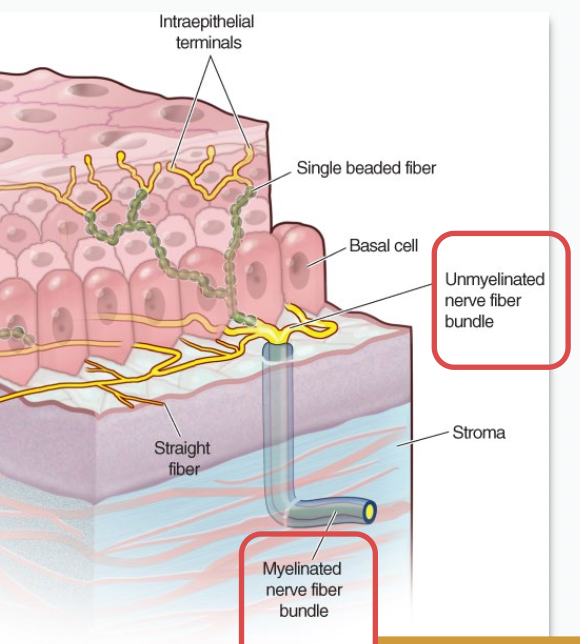
Describe the sensory innervation of the cornea.
Corneal sensory nerves originate from the ophthalmic division (CN V1) of trigeminal nerve
Travel in the nasociliary nerve and its long ciliary nerve branches
Branches into nerve fibers that penetrate the cornea
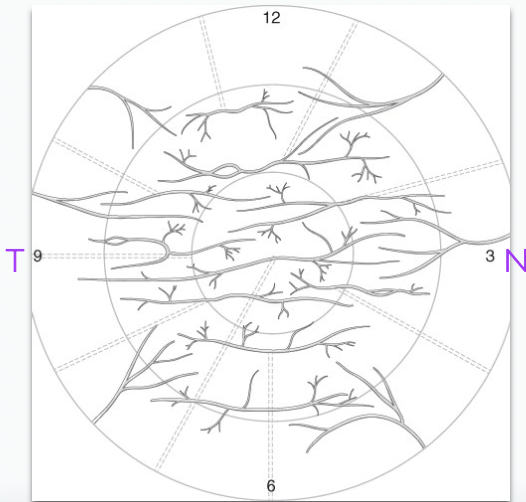
How is corneal innervation distributed?
→ Most nerves enter from the nasal & temporal limbus
Weakest innervation: Superior & inferior cornea
Strongest innervation: Medial (nasal) & lateral (temporal) cornea
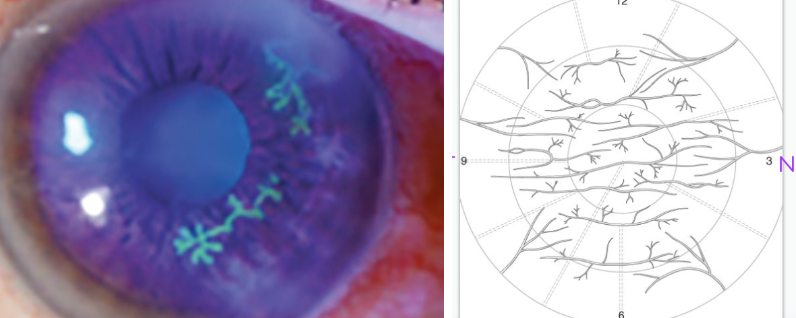
Which viruses can cause dendriform corneal lesions, and what is their pattern?
Neurotropic viruses - Herpes Simplex Virus (HSV)
form a branching (tree-like) pattern, visible with staining
branching b/c corneal nerves themselves have a branching innervation
Why are corneal nerve fibers difficult to see clinically?
Corneal nerve fibers entering from limbus demyelinate when they pass through the Bowman’s layer → hard to see
Outline the location and composition of the Bowman’s layer.
Location:
found directly under the corneal epithelium
it’s not the basement membrane
layer ends about 1 mm before the limbal junction with the sclera
Composition:
Acellular (has no cells)
densely packed Type 1 & 3 collagen fibers with smaller diameters than in the stroma
What happens to the Bowman’s layer if cut perpendicularly vs if completely removed? What does this mean?
Cut perpendicular → scars
Completely removed → no scarring
Bowman’s layer is very resilient (due to dense collagen packing)!
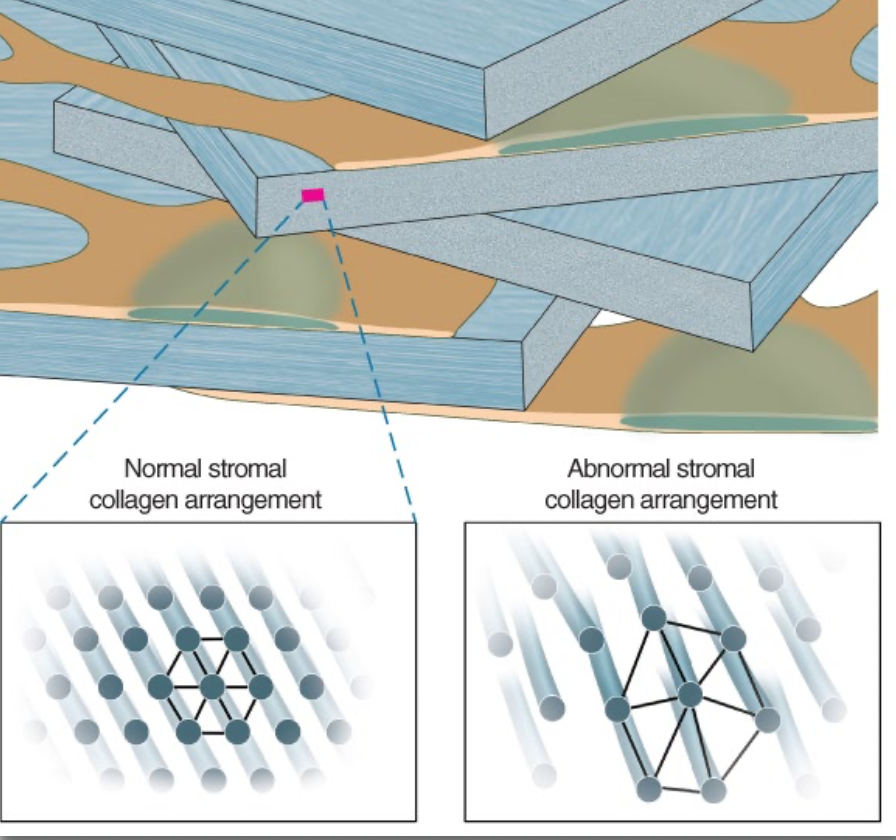
Outline the composition, cells & function of the Stroma.
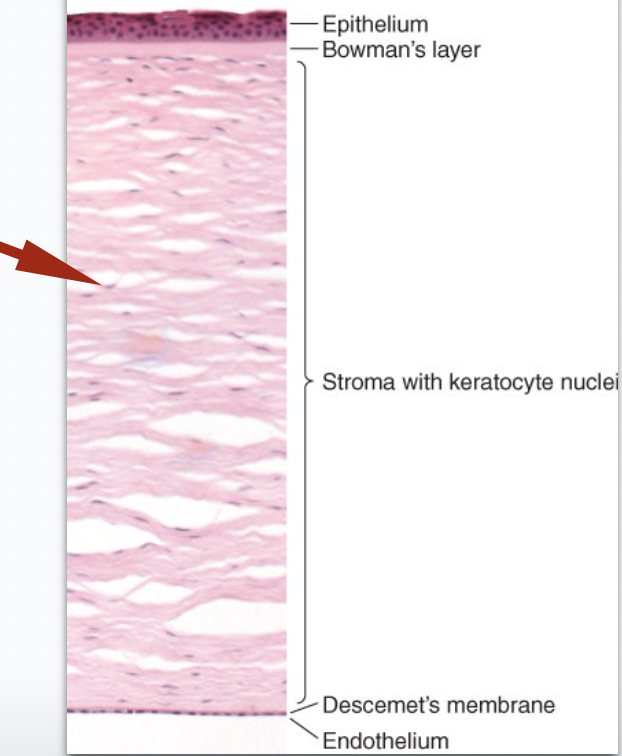
Composition
Dense regular CT
each CT layer = lamellae
Each lamella has:
Parallel arrangement of T1 collagen fibers
Uniform spacing b/w fibers → maintained by proteoglycans & GAGs
# of lamellae ↓ with age due to slow stromal turnover
Cells:
Keratocytes (specialized fibroblast-like cells) are found b/w the lamellae layers and are connected by gap junctions
Function: Maintenance & repair
What % of corneal thickness comes from the stroma?
90%
How does the Maurice’s Theory explain the Optical Transparency in the cornea?
→ T1 collagen are neatly spaced → destructive interference → ❌ light scattering
changing stromal spacing (e.g., edema) → ❌ destructive interference → light scatters → opaque cornea
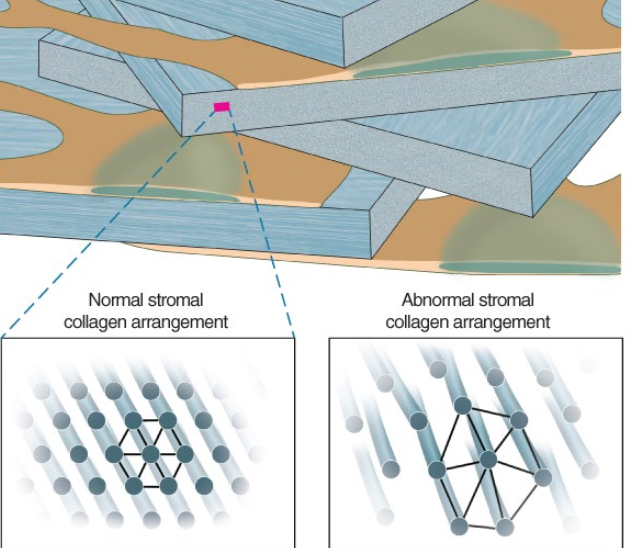
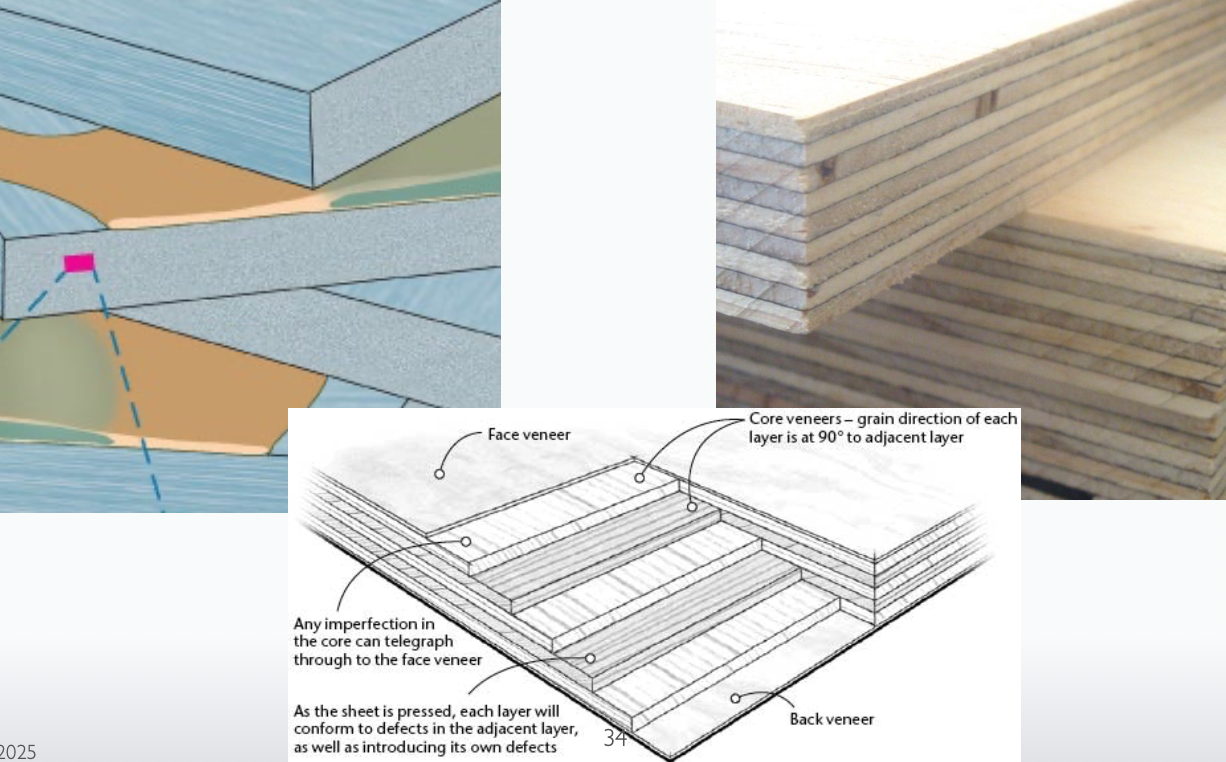
How are stromal lamellae arranged?
oriented 90° apart, like plywood → strength
Is the corneal stroma a uniform matrix?
No!
→ varying conc of diff proteoglycans
Anterior stroma - has ↑ [Keratocytes] & [plasma proteins]
Posterior stroma (near Descemet’s membrane) - more structurally durable
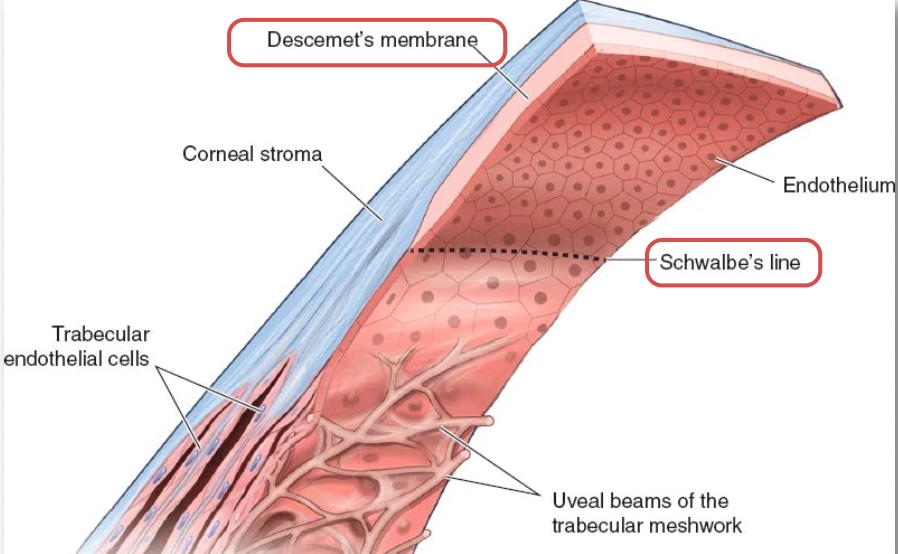
What is the Descemet’s membrane?
→ TRUE basement membrane of the corneal epithelium
it’s peripheral edge = Schwalbe’s line
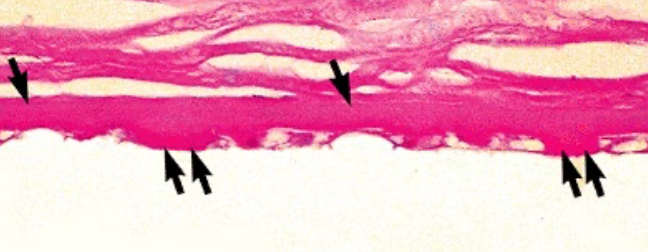
How does Descemet’s membrane change with age?
Thickens uniformly with age
Hassal-Henle bodies may develop (small nodules) in DM edges → normal
similar nodules called “Glutta” may develop in central cornea → pathological
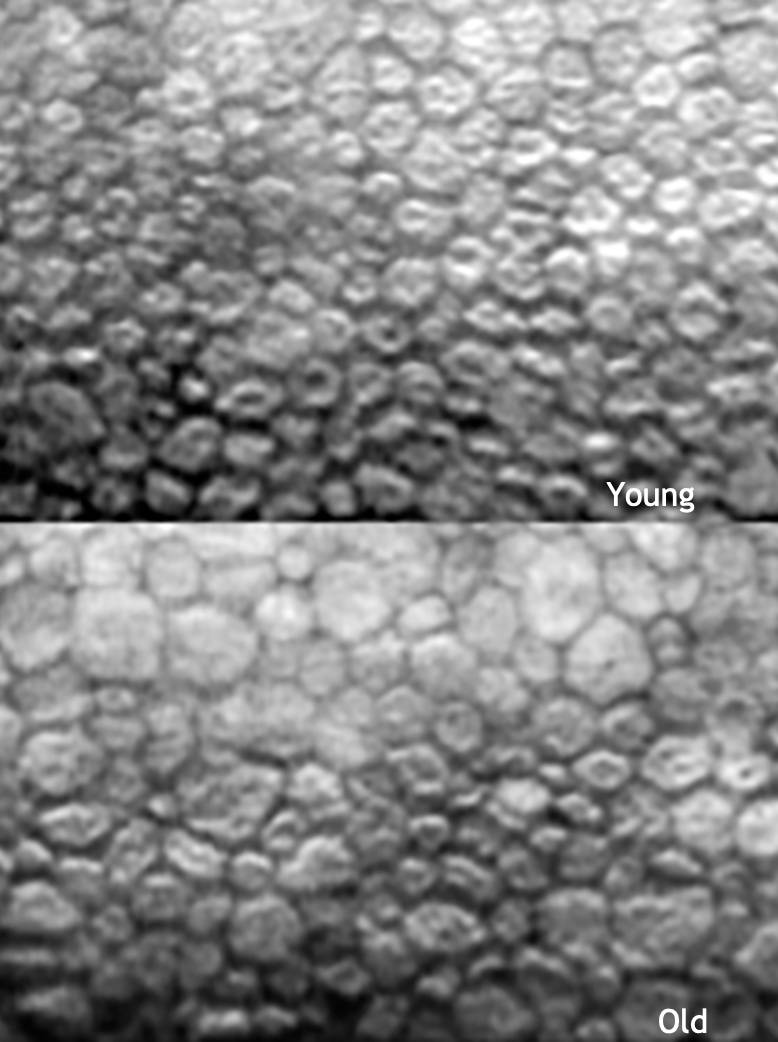
Describe how the cells change with age in the Corneal Endothelium.
👦🏼 Young — Simple, cuboidal epithelial cells
Aging → lose epi cells which aren’t replaced (3,000–3,500 cells/mm² → below 500–700 cells/mm²)
👴🏼 Old — remaining cells become thin and squamous to cover DM
What is the Arlt’s Triangle?
triangular area on the corneal endothelium where particulate matter from the aq humor tends to deposit
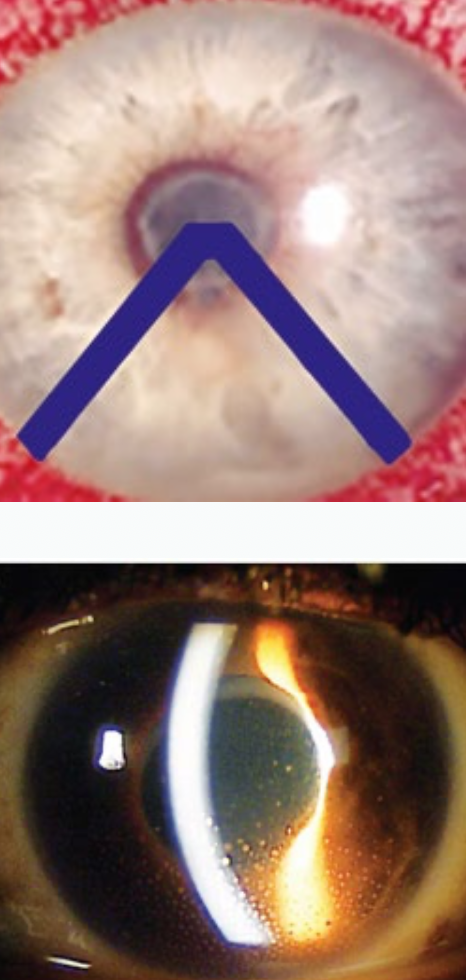
What is the mechanism behind the Arlt’s triangle?
Aq humor moves in a convection current — warm near the iris, cool near the cornea
Aq rises posteriorly (near iris) → falls along the cornea → forms a triangular deposition zone (Arlt’s △)
What are normal and abnormal findings regarding the Arlt’s triangle △?
Deposits within Arlt’s △ → normal
Deposits outside Arlt’s △ → pathological
There are 3 landmarks at the lid margins. What are they?
External – 2 rows of lashes
Middle – grey line
Innermost– 1 row of openings representing the Meibomian gland orifices (holes)
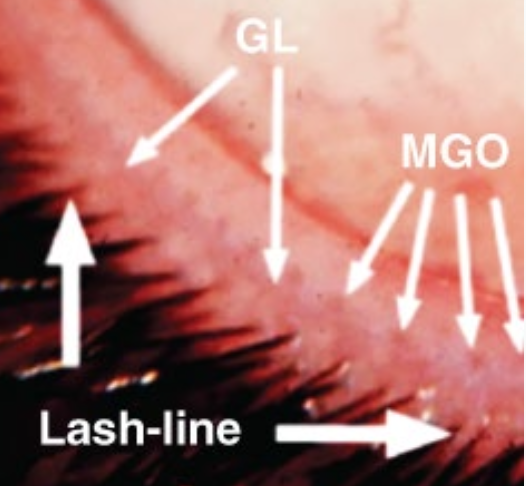
Where is the mucocutaneous junction?
posterior to the MGOs
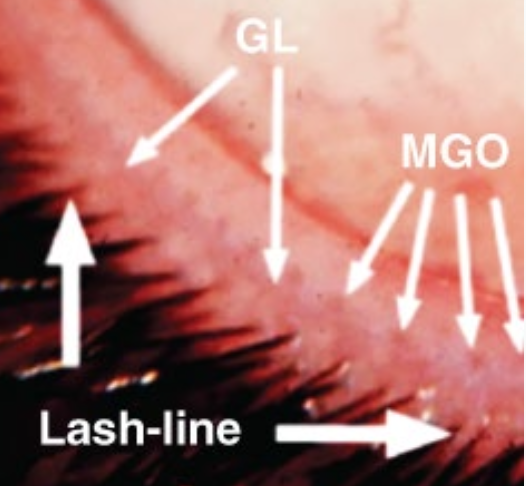
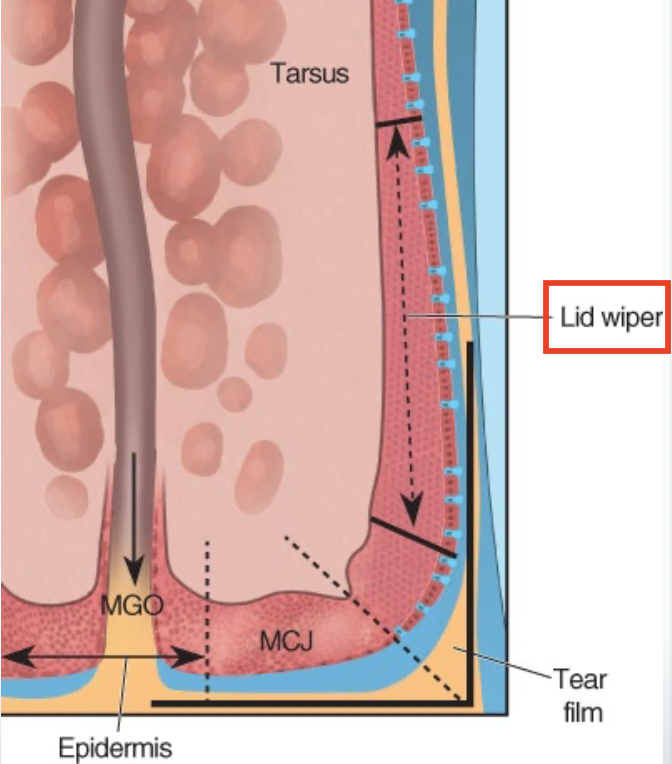
What is the Lid Wiper region of the conjunctiva?
→ portion of the conjunctiva just posterior to the mucocutaneous junctions (where the skin meets the conjunctiva).
has a thickened epithelium
forms a narrow strip that actually contacts and wipes across the cornea during each blink
What’s the function of the Lid Wiper?
Acts like a “windshield wiper”
Removes old tears, debris & cells
Smooths and spreads a new thin tear film over the cornea
Helps maintain a smooth optical surface for clear vision
What is Lid Wiper Syndrome? What does it lead to?
→ Caused by chronic mechanical irritation (from blinking over contact lens edges)
Leads to:
Dry eye symptoms
Discomfort, burning, or foreign body sensation
Poor tear film distribution (tear layer not spread evenly)
List the characteristics of the Conjunctival Epithelium.
Stratified cuboidal to stratified squamous
continuous with the corneal epithelium at the limbus
has lots of Langerhan’s cells + goblet cells
has microvilli on the surface to → hold the glycocalyx & tear film in place + ↑ SA secretion
Are the goblet cells uniform in density in the Conjunctical epithelium?
No!
↓ goblet cells near the limbus & lid margin
↑ density as you move away from limbus and lid margin
↑ nasally (esp fornices b/c they help sweep the gunk out)
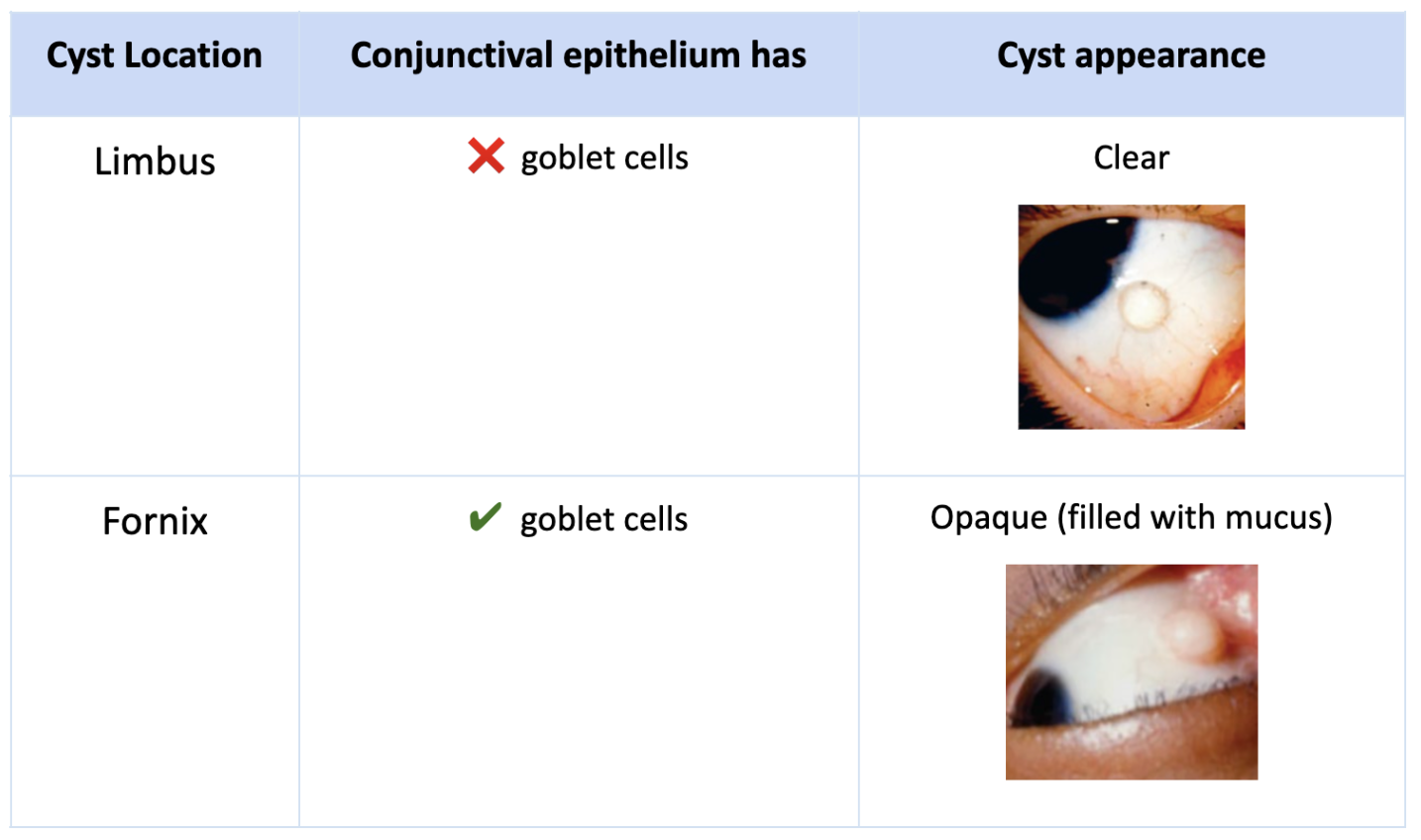
What are Epithelial inclusion cysts? Give examples on how it’s location affects the types of cysts formed.
→ cysts formed from the overlying epithelium reflecting the cell types found in that region