Health Assessment Exam 1
1/124
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
125 Terms
weight loss planned
intentional weight loss
weight loss unplanned
involuntary weight loss of greater than 5% of body weight in 1 month or involuntary weight loss of greater than 10% in 6 months; weight loss of more than 20% indicates severe protein-calorie malnutrition
overnutrition
Too much food energy or excess nutrients to the degree of causing disease or increasing risk of disease; a form of malnutrition
malnutrition
deficiencies, excesses or imbalances in a person's intake of energy and/or nutrients
At risk for undernutrition
alcoholics, behavioral/mental health issues, children, chronic/acutely ill, decreased cognitive function, elderly, illiterate, disabled, low income, traumatic brain injured, substance abusers
nutritional health history
focuses on the clinical, physical and psychosocial factors that may affect a patient's nutritional intake; includes
food preparation, weight, dietary preferences, dietary supplements/vitamins, appetite, food intolerances/allergies, water intake
24 hour diet recall
All foods, beverages and accurate amounts (as possible) consumed within the last 24 hours
Body Mass Index (BMI)
a screening tool that identifies the amount of body fat based on height and weight; first tool to indicate nutritional status
inspection
visual examination of the external surface of the body
inspection, palpation, percussion, auscultation
Order of assessment EXCEPT for the abdomen:
Palpation
an examination technique in which the examiner's hands are used to feel the texture, size, consistency, and location of certain body parts
percussion
tapping on a surface to determine the difference in the density of the underlying structure
Auscultation
listening to sounds within the body (usually with a stethoscope)
light palpation
detects surface characteristics and accustoms the person to being touched; finger pads 1 cm
deep palpation
assesses an organ or mass deeper in a body cavity; using finger pads of dominant hand gently press down 5 cm
tympany
The percussion note one should hear over the abdomen
Dullness on percussion
sign of fluid or solid mass under area being percussed
Resonance (percussion sound)
a low-pitched, hollow sound, usually heard over normal lung tissue
Hyperresonance Percussion Sound
lower-pitched, booming sound found when too much air is present such as in emphysema or pneumothorax
flatness
extremely dull sound produced by very dense tissue such as muscle or bone
bell of stethoscope
cup-shaped endpiece used for soft, low-pitched heart sounds; bruits, murmurs

Diaphragm of stethoscope
flat endpiece of the stethoscope used for hearing relatively high-pitched sounds

General Survey
study of the whole person, covering the general health state and any obvious physical characteristics such as posture dress, behavior, level of consciousness, mobility, distress
Temperature normal range
97.5-99.5 F or 36-37 C
hypothermia
body temperature below 95 F 35 C
fever, pyrexia, hyperthermia
temperature greater than 100 F 37.8 C
oral temperature
should not be used on a patient who cannot follow directions, has decreased mentation, is unable to keep mouth closed or breathes through mouth; standard for adult measurement of temperature
tympanic temperature
taken in the ear; should not be used on patient who is experiencing ear pain, ear drainage or has a large amount of wax
temporal temperature
Measurement of body temperature at the temporal artery on the forehead; usually 0.5 F (0.3 C) lower than oral temp
rectal temperature
temperature taken in the rectum; can stimulate the vagus nerve; contraindicated in rectal surgery, rectal disease, low WBC, blood clotting disorder, neurologic disorders, cardiac disease, diarrhea and hemorrhoids; 0.5 F (0.3 C) higher than oral temp
radial pulse
the pulse felt at the wrist; 60-100bpm expected
apical pulse
pulse taken with a stethoscope and near the apex of the heart
pulse deficit
the apical and the radial pulse rates.
bradycardia
slow heart rate (less than 60 bpm)
Tachycardia
rapid heart rate greater than 100 bpm
pulse volume scale
0 Absent pulse
1+ Weak and thready pulse, difficult to palpate
2+ Normal pulse, able to palpate with normal pressure
3+ Bounding pulse, may be able to see pulsation
Respiratory Rate (RR)
Number of breaths per minute; Adults = 12-20
Tachypnea
Increased breathing rate above 20 bpm
bradypnea
abnormally slow breathing (less than 12 breaths per minute)
depth of respiratory rate
shallow vs deep
rhythm of respiratory rate
regularly spaced or irregularly spaced
respiratory effort
Work of breathing-relaxed easy breaths expected
Dyspnea: labored breathing
Orthopnea: inability to breathe when horizontal
Systolic Blood Pressure (SBP)
The pressure in arteries and other blood vessels when the heart is contracting; the first (top) number recorded.
Diastolic Blood Pressure (DBP)
The pressure in arteries and other blood vessels when heart is at rest or between beats; the second (bottom) number recorded.
blood pressure levels in adults
normal: systolic <120, diastolic <80
elevated: systolic 120-129, diastolic <80
hypertension stage 1: systolic 130-139, diastolic 80-89
hypertension stage 2: systolic >140, diastolic >90
hypertensive crisis: systolic >180, diastolic >120
orthostatic vital signs
blood pressure & pulse taken lying, sitting, & standing and documented indicating the corresponding position
subjective data
things a person tells you about that you cannot observe through your senses; symptoms
objective data
information that is seen, heard, felt, or smelled by an observer; signs
Four key principles to inclusive assessment
1. treat every health assessment as an act of humanity
2. health assessments are not about "sameness"
3. examine your own personal biases
4. cultivate a safe environment of care
Cultural Sensitivity
recognizing and respecting the differences between cultures
cultural competency
the enabling of health care providers to deliver services that are respectful of and responsive to the health beliefs, practices, and cultural and linguistic needs of diverse patients
cultural humility
process that requires humility as individuals continually engage in self-reflection and self-critique as lifelong learners and reflective practitioners
Cultural safety
Culturally appropriate health services to disadvantaged groups while stressing dignity and avoiding institutional racism, assimilation (forcing people to adopt a dominant culture), and repressive practices.
Pain
is whatever the experiencing person says it is, existing whenever he/she says it does; should be accepted as such and respected
acute pain
short-term, self-limiting, often predictable trajectory; stops after injury heals
chronic pain
Enduring pain that does not decrease over time; may occur in muscles, joints, and the lower back, and may be caused by enlarged blood vessels or degenerating or cancerous tissue. Other significant factors are social and psychological.
intractable pain
severe pain that is extremely resistant to relief measures
intermittent pain
Pain that comes and goes at intervals
phantom limb pain
pain in a limb (or extremity) that has been amputated
radiating pain
starts at the origin but extends to other locations
referred pain
pain that is felt in a location other than where the pain originates
Quality of Pain Descriptors
stabbing, burning, itching, tingling, cramping, aching, dull, tender, shooting, sharp, pressure, crushing, throbbing, etc.
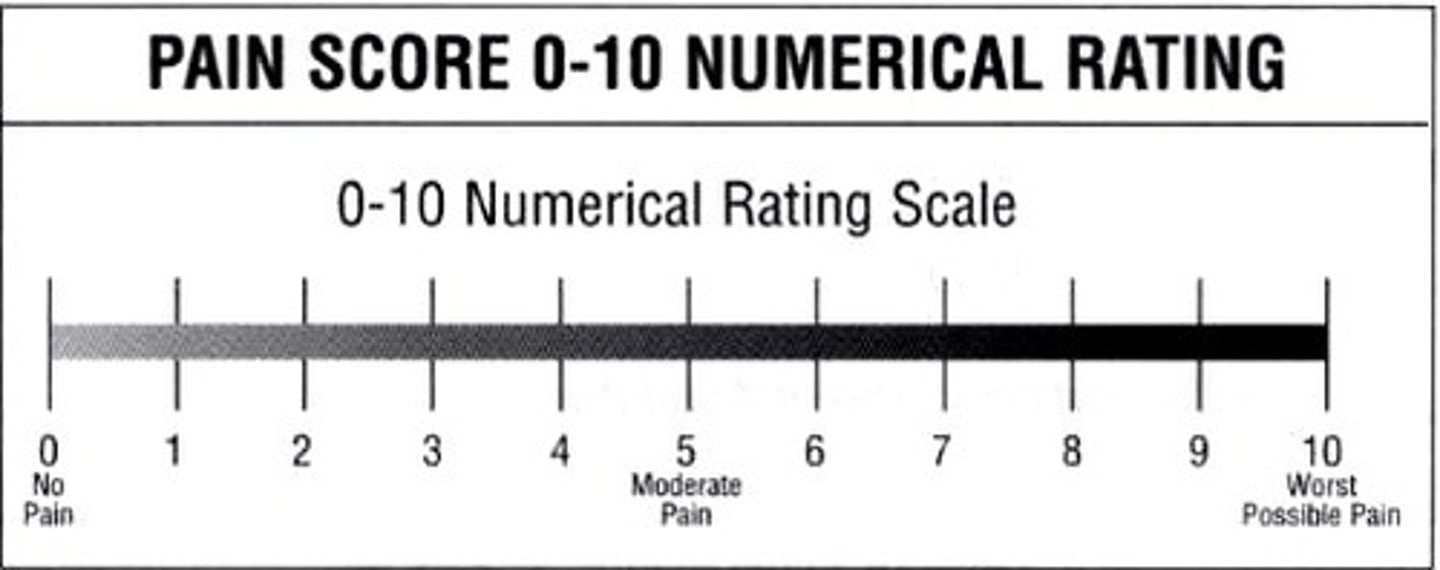
numeric rating scale
patient chooses level of pain for each site 0-10; most adults, but not old
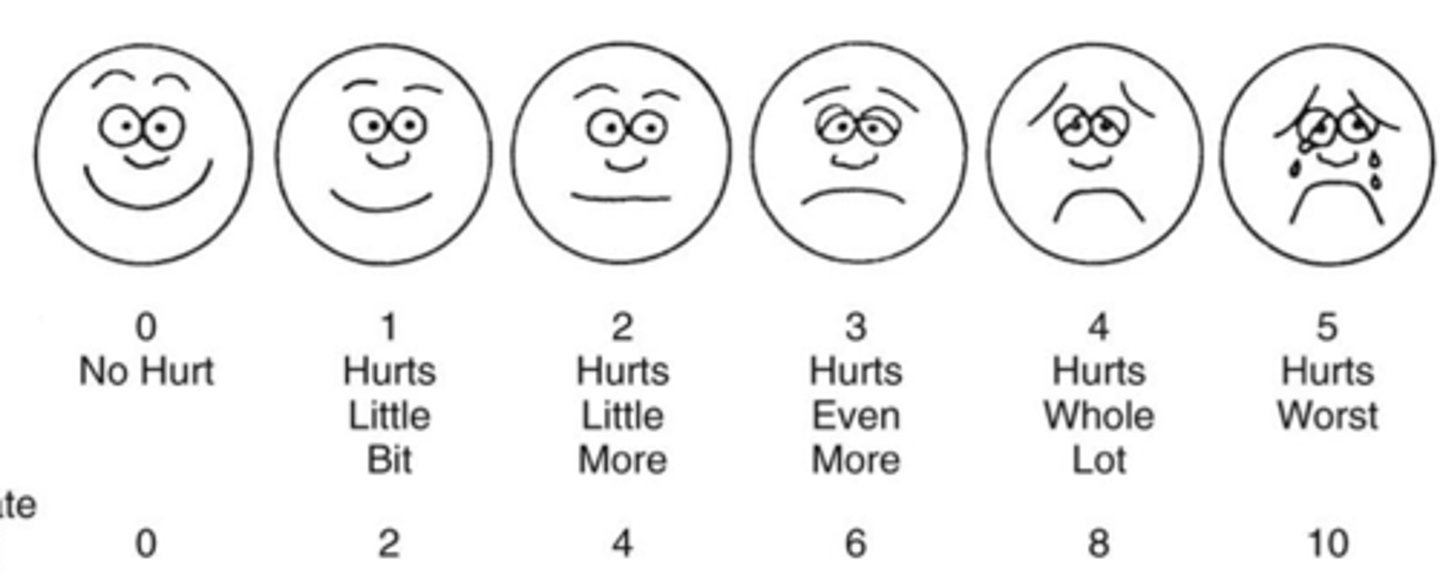
Wong-Baker FACES scale
a pain assessment tool that asks patients (often children) to select one of several faces indicating expressions that convey a range from no pain through the worst pain
PAINAD scale
assessment tool for pain used with dementia patients; assesses 5 common behaviors: breathing, vocalization, facial expression, body language, and consolability. A score of 4 or above indicates a need for pain management.
documentation of pain
Level of pain, description of pain, action taken, response to interventions
OPQRST (pain assessment)
Onset, Provocation, Quality, Region/Radiation, Severity, Timing.
OLDCARTS (pain)
Onset
Location
Duration
Character
Aggravating factors
Relieving factors
Timing
Severity
active listening
Pay close attention to the patient's report and non-verbal cues; maintain good eye contact and express a willingness to listen.
active observing
Concentrate on what you hear and see during the interview.
broad opening questions
Will allow the patient to report more spontaneous information and tell you their story. An example is, "What can I do for you today?"
clarification
Obtain clarification if the patient does not clearly express the problem or issue and you are confused about what the patient is saying to you
confrontation
Give the patient honest and respectful feedback about what you see or hear that is inconsistent with what the patient is telling you.
empathy
Identify, understand, share and accept the patient's feelings.
respect
Be respectful of what the patient is saying and feeling.
exploring
Encourage the patient to give you more details. An example is, "Tell me more about the pain in your back."
facilitation
Use simple verbal statements or words to encourage the patient to continue to tell the story. Statements like "uh huh", "And then?"
focusing
Ask specific questions to collect and clarify data that he patient may not be stating during the interview.
Reflecting/Stating the observed
Repeat the patient's words specifically to encourage elaboration of the patient's self-report; this encourages more discussion. An example of reflection is Patient: "I cannot believe that I did not go for my mammogram and now I may have breast cancer." Nurse: "You sound upset. Are you angry that you did not go for your mammogram?"
transitional statements
Use transitional statements to help redirect the interview to another significant area. An example of a transitional statement is, "Now, I would like to discuss your family history."
Silence
Planned absence of verbal remarks allows the patient and the nurse to think over or feel what is being discussed.
Summarizing
State a brief summary at the end of the interview; this allows for clarification and accurate data of the patient's history or problem.
Leading the patient
Do not lead the patient; patients tell you what they want you to hear and may not always be truthful in their self-report.
Asking too many questions
only ask one question at a time for clarity and to disallow misunderstanding
not allowing enough response time
give the patient enough time to think through the answer
using medical jargon
use simple terms so the patient can understand you
assuming what the patient is saying
Never assume what the patient is saying; this leads to misinterpretations
using cliches
Cliches (e.g. "you will feel better in the morning") show disregard for the patient's feelings. This is giving false reassurance.
Offering false reassurance
Never tell the patient that everything will be fine when it may not be.
Specifically asking "why" questions
A patient may feel offended and feel like you are criticizing; a subtle approach is usually more comfortable
changing the subject inappropriately
Sometimes nurses change the subject abruptly when the interview is uncomfortable; this is not helpful for the patient.
Giving opinions
Do not give your own opinions. If the patient asks, "What should I do?" help clarify the options, and provide information about the choices the patient has and refer the patient to talk with his or her healthcare provider.
Stereotyping
be objective during the assessment; every patient is unique and should be respected regardless of race, religion, gender, sexual preference or age.
using patronizing language
Patronizing language communicates superiority or disapproval. Statements such as, "You know better than that," are patronizing and offensive to the client. Condescending approaches, such as, "You should have used the call button before you got up. You're lucky you didn't hurt yourself," do not communicate respect for the client.
Language interpretation
Explain the right to have a language interpreter. Speak directly to the patient and not at the interpreter. Ask simple and clear questions; provide time for the patient to ask questions. Avoid using family members for interpretation.
open-ended questions
allows the patient to express thoughts and encourage verbalization; this type of question allows the nurse to explore the focused topic more broadly. Start with open-ended questions and then use closed questions.
close-ended questions
used to clarify and focus on specific problems; can usually be answered with one word or "Yes" "No"
Three phases of the interview
1. Introduction
2. Working phase - gather data w/ open-ended questions, then closed questions
3. Closing - gives the patient one last chance to share concerns or express himself or herself
Also briefly summarize what you learned during the interview
comprehensive health history
looks at the whole patient and reviews all body systems; this health history takes time
focused or problem-based history
focuses specifically on an acute problem or symptom that the patient is experiencing