Looks like no one added any tags here yet for you.
What do humans use for fuel/energy to move?
Adenosine triphosphate (ATP)
Where does ATP come from?
macronutrients in the diet and is broken down into Carbohydrates (CHO), Fats and Proteins (PRO)
what does CHO and PRO as fuel yield?
4kcal per gram
Fats as fuel yield?
9kcal per gram
Fuel Choices for Energy Production - Carbohydrates
absorbed as glucose primarily, also fructose and galactose
Fuel Choices for Energy Production - Fats
absorbed as fatty acids, triglycerides and cholesterol
Fuel Choices for Energy Production - Proteins
absorbed as amino acids plus some small peptides
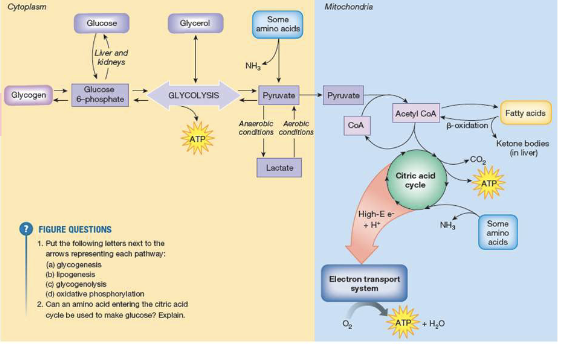
Carbohydrates - Anaerobically
CHO in the form of glucose goes through Glycolysis = 2 ATP and Pyruvic Acid. If initial fuel is glycogen = 3ATP.
Not much energy but very fast
Carbohydrates - Aerobically
Pyruvic acid from anaerobic metabolism enters Kreb’s cycle = 2ATP with leftover Hydrogen ions (H+). H+ enters Electron Transport Chain = 30-32 ATP
Fats - aerobically
Stored energy that is released/produced Aerobically.
Produce greater amount of energy that CHO or Proteins, however it takes longer
Fat breakdown can only continue in the presence of oxoacetic acid that comes from CHO metabolism
Proteins
Vital building ingredient for many cells in our body
Important fuel for Endurance activities (greater than 90)minutes
Proteins go through deamination (removal of an amine group from the amino acid) and transamination (removal of nitrogen) processes
and leave carbon skeletons
Gluconeogenesis is glucose synthesis from these skeletons – your body can now use the protein for energy
Summary for Energy Production
Overview of Muscle Metabolism
Exercise begins with muscle contraction – this requires ATP for energy
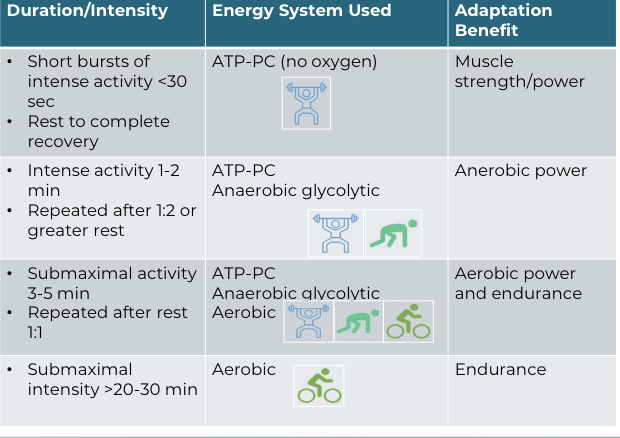
Metabolic Pathways - Phosphagen, or ATP-PC
Short, quick bursts
Fist 30 seconds of intense exercise
Metabolic Pathways - Anaerobic Glycolytic
Moderate intensity or short duration
30-90 sec of exercise
Metabolic Pathways - Aerobic
Predominates after 2 min of exercise
Metabolic Pathways - overview
Aerobic vs Anaerobic Metabolism
Anaerobic metabolism
fast, not efficient
yields only 2 ATP
Aerobic metabolism
slower, more efficient
yields 30-32 ATP
requires adequate O2
Aerobic metabolism
Carbohydrates are converted to ATP through glycolysis/citric acid cycle/ETS pathways (provides 30-32 ATP per glucose)
Fatty acids are processed through a pathway called beta oxidation – the number of ATP produced are determined by the length of the fatty acid
Anaerobic Metabolism
When there is insufficient oxygen, glucose is converted to lactate (referred to as glycolytic metabolism/glycolysis) (provides 2 ATP per
glucose).
When metabolic byproducts accumulate in the muscle, it inhibits glycogen breakdown and has a negative effect on muscle contraction
Substrate Use During Exercise
Lower levels of exercise (< 70% oxygen consumption)
uses 60% fats for energy
uses 40% glucose for energy
Higher levels of exercise (> 70% oxygen consumption)
uses carbohydrates –glucose
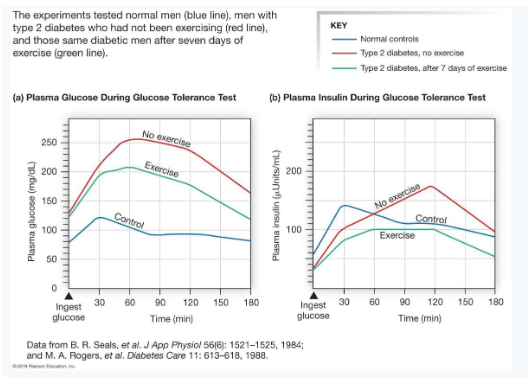
Hormones regulate metabolism during exercise
Insulin secretion is suppressed during exercise.
Muscle does not use insulin for glucose uptake
Muscles use GLUT4 transporters for glucose uptake
Fuel Choices for Energy Systems
What you are doing determines which energy system is being used
The availability of oxygen determines how ATP will be used
VO2 max is the maximum volume of O2 able to be taken in, transported and utilized
Oxygen Consumption
Oxygen consumption is the rate of oxygen used by the body and is used to quantify exercise intensity.
Resting oxygen consumption is approximately 3.5 ml/kg/min.
Maximal oxygen consumption is the amount of oxygen consumed by an individual at maximal exercise, and is used as a measure of cardiorespiratory fitness
VO2max is the product of?
maximal cardiac output and a-vO2 difference
Maximum Oxygen Consumption (VO2 max)
Measure of body’s capacity to use oxygen
Maximum rate of oxygen consumption attainable during physical exertion
Expressed relative to bodyweight
mL/kg per minute
Maximal rate of oxygen consumption equations:
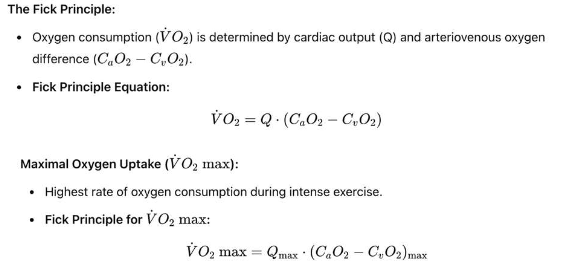
VO2 METs
VO2 can be measured in ml/kg/min (adjusted for differences in body weight), L/min, or METS.
One MET (metabolic equivalent) is the oxygen consumption at rest.
2 METs means that a person is consuming oxygen at twice the resting rate (7 ml/kg/min).
3 METs means that a person is consuming oxygen at three times the resting rate (10.5 ml/kg/min
VO2max is measured using?
open circuit spirometry. The individual performs a graded exercise test to exhaustion with ventilation and expired O2 and CO2 measured.
Estimating V˙O2\dot{V}O_2V˙O2 max using field tests is a practical approach for assessing aerobic fitness without specialized equipment. Some common field tests include:
Cooper Walk/Run Test
Run or walk as far as possible in 12 minutes.
1.5 Mile Run Test
Run 1.5 miles as quickly as possible.
Step Test
Step up and down on a platform for 3 minutes.
Rockport Walk Test
Walk one mile as quickly as possible
Components of Physical Function Related to Human Movement: Definition of Key Terms
• Balance
• Cardiopulmonary endurance
• Coordination
• Flexibility
• Mobility
• Muscle Performance
• Neuromuscular Control
• Postural control, postural stability, and equilibrium
• Stability
What is therapeutic exercise?
The systematic performance or execution of planned physical movements of activities intended to enable the patient or client to:
1. Remediate or prevent impairments of body structures or functions
2. Enhance activities or participation
3. Prevent or reduce health-related risk factors
4. Optimize overall health status, fitness or sense of well-being
Management Model
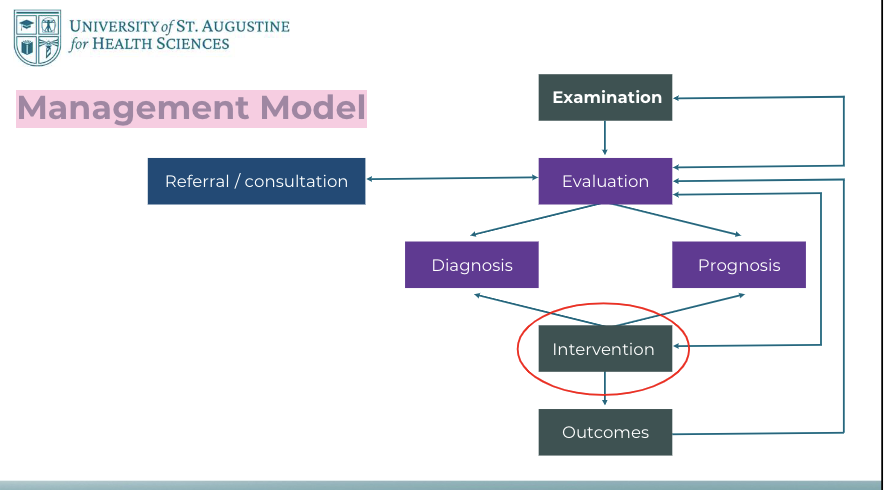
Therapeutic Exercise Interventions
• Aerobic capacity/endurance conditioning or reconditioning
• Flexibility exercises
• Strength, power, and endurance training
• Balance training
• Neuromotor development training
• Gait and locomotion training
• Relaxation
• Posture training
• Graded motor imagery
Role of Physical Therapists
Simply addressing impairments does not guarantee improvements in performance or quality of life
Importance of Task-Specific Exercises
To enhance a patient’s performance in activities and participation in life roles, as well as to improve health-related quality of life, interventions should include exercises that are specific to the tasks the patient aims to perform
How do we prescribe therapeutic exercise?
ICF Framework FITT-VP Considering contextual factors
Using principles of science (physiology and biomechanics)
Using best evidence from research
ICF framework
1. Patient’s goals → participation restrictions
2. Activity limitations
3. Body structure/function impairments
4. Contextual factors → Environmental and Personal, Barriers and Facilitators
ICF Definitions
Health Condition- the disorder or disease state
Participation Restrictions - the inability of the individual to engage in expected life situations (e.g. work, social role, play, chores, recreation)
Activity Limitations - the inability to perform certain tasks, functions that lead to participation restrictions (e.g., cannot sit at a desk; cannot hold a tennis racket; cannot ascend a flight of stairs at home)
Body Structures and Functions - anatomic and physiologic (including psychological) impairments that limit function
Contextual Factors - Environmental and Personal Factors (e.g., physical, social, and attitudinal) influencing a person’s life
Activity Limitation and Participation Restriction
Correlation Between Body Function and Activity Limitations:
Decreased isometric strength in lower extremities correlates with difficulties in stooping and kneeling.
Reduced peak power in lower extremities is linked to slower walking speeds and challenges moving from sitting to standing.
Variability in Impact of Impairments:
Not all impairments consistently lead to activity limitations.
Increased joint space narrowing in osteoarthritis patients did not consistently correlate with increased activity limitations in a 2-year study.
Critical Threshold of Impairments:
Severity and complexity of impairments must reach a critical, person-specific level to significantly impact functioning.
ICF Construct Relevance:
Findings support the ICF framework, highlighting that environmental and personal factors interact with all aspects of functioning and disability
Individual responses to health conditions are unique and influenced by various factors
Purpose of Exercise Training
The purpose of performing regular exercise is to achieve a positive adaptation in physical function. Each exercise we prescribe is linked to a specific goal
Principles of Exercise Training
Exercise Training Principles
Components of an exercise prescription
Examples of training adaptation
Exercise Training Principles
Overload
Specificity/ Specific Adaptation to Imposed Demands (SAID)
Reversibility
Individual differences
Overload
the stress to the body during an exercise challenge must be greater that the stress encountered in daily activities; this applies to both aerobic and resistance exercise
SAID (Specific Adaptations to Imposed Demands):
A framework of specificity is a necessary foundation on which exercise programs should be built.
the adaptive effects of training are specific to the mode of exercise used in training; if the client’s goal is to be able to climb stairs, then the training should involve ascending and descending stairs
Specificity of Training - adaptive effects of training are highly specific to the training method employed (strength v power v endurance)
Reversibility Principle; “Use it or lose it”
adaptive changes that occur in response to aerobic or resistance exercise training are lost if the individual stops performing the exercise program
If activities can be incorporated into routine functional activities, then the adaptations can be maintained
Individual differences responses differ between individuals because of
age, genetic differences, initial fitness level, etc
Components of an exercise prescription
Intensity: How hard a person is working
Volume: What is the total amount of exercise?
Frequency: Number of session per day or week
Time: Duration of a bout of exercise in a session
Can be described as sets and repetitions
Includes the rest interval between sets or between exercises
Type: what is the mode of exercise?
Progression: how is the exercise prescription advanced?
Duration: total time frame of the training program
Intensity
how hard a person is working
For example, an aerobic exercise prescription could be based on HR response, a resistance exercise prescription could be based on % of 1RM
Submaximal vs. maximal loading – what is the goal and why?
Time
How long is the individual working during a bout of exercise?
Can be a set of amount of time, i.e. run for 20 minutes
Time can also be measured in sets and repetitions
Repetitions – number of times a particular movement is repeated. The number of muscle contractions performed to move the limb through a motion against a specific load.
Sets – a predetermined number of repetitions grouped together. After each set, there is a brief interval of rest
Volume
a measure of the overall stress of the exercise prescription
Volume = Frequency x Sets x Reps x Intensity
Example: According to ACSM, all healthy adults aged 18 – 65 should participate in 30 minutes of moderate-intensity aerobic activity, five days a week
Volume = 150 minutes/week of moderate intensity aerobic exercise
Volume should also consider the other physical stress (other exercises and non-exercise
physical activity)
Progression
The component of PROGRESSION refers to increasing the dosage of exercise over time
As the individual adapts, one or more components of FITT-VP can be increased as tolerated
Any component of FITT can also be reduced at any time if exercise is not tolerated
PROGRESSION must follow assessment and re-evaluation!
How do we prescribe therapeutic exercise?
FITT-VP
The classic exercise prescription has four components, which can be abbreviated by the acronym FITT
ACSM’s Guidelines for Exercise Testing and Prescription extends this with two additional components: FITT-VP
FITT-VP is a useful memory aid; however, it may be more effective to change order in the actual exercise Rx process to begin with Type
Biological Factors
Age, sex and race
Height/weight relationship
Congenital disorders (skeletal deformities, neuromuscular/cardiopulmonary disorders or anomalies)
Family History of disease; genetic predisposition
Behavioral/Psychological/Lifestyle Factors
• Sedentary lifestyle
• Poor nutrition
• Use of tobacco, alcohol or other drugs
• Low level of motivation
• Inadequate coping skills
• Difficulty dealing with change
• Negative affect
Physical Environment Characteristics
Architecture barriers in the home, community and workplace
Ergonomic characteristics of the home, work or school environments
Socioeconomic Factors
Economic status
Level of education
Access to healthcare
Family or social support
SODH
• Economic Stability
• Education Access and Quality
• Healthcare Access and Quality:
• Neighborhood and Built Environment
• Social and Community Context
Selecting and Advancing Interventions
Initial Exercise Prescription
Dosage: FITT-VP
Tolerance: ability of the patient to successfully manage a given input or load based on their current level of abilities, impairments, and overall health.
Progression of Exercise
1. Continuous Assessment and Adaptation
2. Thoughtful Manipulation of Exercise Variables
Fatigue
Fatigue is defined as the inability to maintain force production for a given task
Muscle (local) fatigue – diminished response of muscle to repeated stimulus
Cardiorespiratory fatigue – systemic diminished response to prolonged physical activity related to the body’s ability to use oxygen efficiently
Factors that influence fatigue: health status, diet, lifestyle (sedentary/active)
Types of Fatigue
Motor Performance Fatigue
Quantifiable decrease in the maximal voluntary force production capacity of the neuromuscular system
Influenced by both neural and muscular factors
Perceived Motor Fatigue
The subjective experience of fatigue that emerges during a motor task, often described as a sensation of tiredness, weariness, lack of energy, or exhaustion
Mechanisms of Fatigue
• Overview of Central vs. Peripheral Fatigue
• Role of the Neuromuscular System
Peripheral Fatigue
Decline in muscle's ability to generate force
Causes:
Metabolic changes in muscle fibers
• Accumulation of byproducts (ROS, phosphates, calcium, lactate, ADP, magnesium)
Reduced glycogen
Effects:
Impaired muscle function
Slower muscle contraction
Key Byproducts:
Lactate, hydrogen ions, creatine, inorganic phosphate
H+ and Pi impair muscle function
Lactic acid not a cause of fatigue!
Central Fatigue
involves CNS influences on neuromuscular strength.
Influenced by physiological, psychological, and motivational factors
Stress and sleep deprivation can be factors
Affects cognitive functions and physical performance through higher brain structures.
Develops slowly in submaximal exercise
Other Fatigue Factors
Perception of Effort: Mental fatigue increases the perception of effort during exercise, making tasks feel more demanding and impairing endurance performance.
Stress and Sleep Deprivation: These factors significantly affect performance by altering neural activation patterns, slowing cognitive processes, and increasing subjective fatigue.
Motivation: Mental fatigue can decrease intrinsic motivation, which negatively affects performance, especially in tasks perceived as mentally demanding.
Cognitive Demands of Exercise: The cognitive load, including the need for sustained concentration and decision-making, is significantly impacted by mental fatigue, particularly in tasks that require both physical and cognitive effort.
Behavioral Changes: Mental fatigue leads to behavioral changes such as decreased self-selected pace and power output, which are influenced by changes in mental state rather than just physiological fatigue
Training can reduce fatigue
Physiologic Adaptation Through Specific Training:
Types of Training to Improve Mitochondrial Capacity:
Threshold Work -> increases buffering capacity.
High-Intensity Interval Training (HIIT) ->boosts mitochondrial efficiency and capacity, improving energy utilization and metabolite processing.
Long Duration Low-Intensity Training ->Increases mitochondrial density, enhancing overall endurance and fatigue resistance
Recovery Factors
1. Peripheral Fatigue
2. Central Fatigue
3. Tissue Damage
4. Cognitive Fatigue
5. Psychological Factors
Recovery
Central Fatigue Recovery:
Endurance Exercise: Recovers quickly within minutes.
Resistance Exercise: Recovers quickly but may take longer based on exercise extent and duration.
Peripheral Fatigue Recovery:
Endurance Exercise: Begins within 3-5 minutes; complete recovery takes longer but is generally faster
Resistance Exercise: Slower recovery due to muscle damage; can take days for full recovery.
Effect of Duration:
Short-Duration Exercise: Central fatigue resolves in minutes; peripheral fatigue begins recovery within minutes.
Long-Duration Exercise: Central fatigue takes longer due to prolonged neural involvement; peripheral fatigue recovery is delayed, taking hours or days for full recovery
Fitness- Fatigue Model
Implications for Training:
Short-Term Overreaching: High-intensity/volume phases followed by recovery can boost performance due to lasting fitness effects.
Overtraining Risks: Insufficient recovery leads to fatigue buildup, negating fitness benefits and risking overtraining syndrome.
Practical Application: Balance intensity, volume, and frequency to optimize gains while managing fatigue.
Plan workouts, recovery periods, and training cycles strategically to maximize performance.
Balance Between Overload and Recovery
Overreaching:
An accumulation of training and/or non-training stress.
Results in a short-term decrement in performance capacity.
May include physiological and psychological signs of maladaptation.
Recovery and restoration of performance capacity typically take several days to weeks.
Overtraining:
Also an accumulation of training and/or non-training stress.
Leads to a long-term decrement in performance capacity.
Might manifest with physiological and psychological symptoms of maladaptation.
Recovery process is more prolonged, taking several weeks to months
Overtraining Syndrome (OTS)
Physiological Symptoms
Persistent fatigue and tiredness
Increased susceptibility to infections
Changes in resting heart rate
Insomnia or changes in sleep patterns
Weight loss and appetite changes
Chronic muscle soreness or pain
Overuse injuries
Psychological Symptoms
Mood disturbances
Lack of motivation
Anxiety
Decreased concentration and focus
Performance Symptoms
Decreased performance
Inability to complete workouts
Prolonged recovery times
Altered heart rate response to exercise
Important Exercise Prescription Variables
Rest Interval
The time between sets or bouts of exercise.
Also the time in between exercises within a session.
Recovery
Time between exercises session
How does the individual feel and perform on the next session?
Frequency
The number or days per week an exercise session is repeated.
Duration
The total number of weeks or months an exercise program is carried out.
Capacity
defined as what a person can do in a standardized controlled environment.
An individual’s ability to execute a task or an action.
Highest probable level of functioning of a person in each domain at a given moment.
An individual’s ability to execute a task under ideal and controlled conditions, without the influence of environmental variables that might affect performance in daily life.
Assessed in a standardized environment
What an individual can do in a standardized, controlled
environment
Performance
describes what an individual actually does in
their daily environment.
Captures the actual activities a person engages in within
their typical daily life.
Takes into account both the physical and social
environment and personal factors like motivation.
Can include use of assistive devices
What an individual does do in their daily environment
Performance should never exceed Capacity!
Stress
• Broad response to any demand disrupting homeostasis.
• Can include emotional, psychological, or physical triggers
Physical Stress
• Force applied to biological tissue.
• Can be external (e.g., GRF during running) or internal (e.g., muscle tension generated to produce movement).
• Can lead to positive or negative adaptations
Exercise
• Planned, structured, and repetitive physical activity.
• Aims to improve physical fitness and overall health
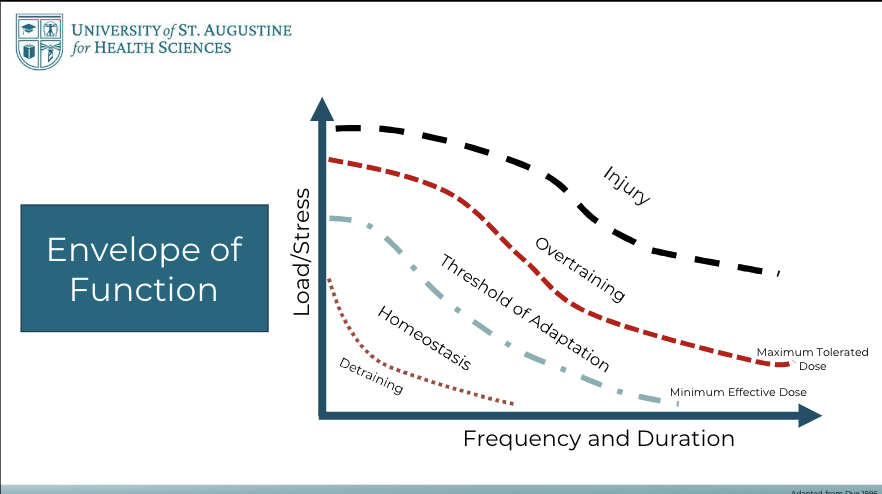
Physical Stress Theory
Physical stress levels that are lower than the maintenance range result in decreased tolerance of tissues to subsequent stresses (e.g., atrophy).
Physical stress levels that are in the maintenance range result in no apparent tissue change
Physical stress levels that exceed the maintenance range (i.e., overload) result in increased tolerance of tissues to subsequent stresses (e.g., hypertrophy).
Excessively high levels of physical stress result in tissue injury.
Extreme deviations from the maintenance stress range that exceed the adaptive capacity of tissues result in tissue death
Wolff's Law
Bones adapt to the loads they are subjected to; increased stress strengthens them, while reduced stress weakens them.
Bone Remodeling: Involves resorption of old bone and formation of new bone to adapt to mechanical stress.
Load-Specific Changes: Bone density and structure change according to the type and amount of stress applied
Davis’s Law
Soft tissues adapt to the demands placed on them, lengthening under tension and shortening in the absence of it.
Scar Tissue Formation: The law also plays a role in how scar tissues align along lines of stress, which is crucial for post-surgical or injury recovery.
Functional Adaptation: The adaptations are functional responses to the specific types and patterns of stress encountered, helping to improve efficiency and performance of the tissues under repeated stresses
Envelope of Function
Examples of Training Adaptations
Possible Physiological Adaptations to Exercise Training:
Aerobic Exercise:
Increased aerobic capacity, there is an increase in VO2max that occurs because of central adaptations (increase cardiac output) and peripheral adaptations (increased number and size of muscle mitochondria).
Resistance Exercise:
Skeletal muscle – increased mass (hypertrophy)
Neural system – increase in motor unit recruitment, rate of firing and synchronizing of firing of muscles
Metabolic system – increase in ATP storage and myoglobin storage
Body composition – increase in lean body mass, decrease in body fat
Connective tissue – increase in strength of tendons, ligaments and connective tissue in muscle, increase in bone mineral density
How does physical stress relate to capacity and performance?
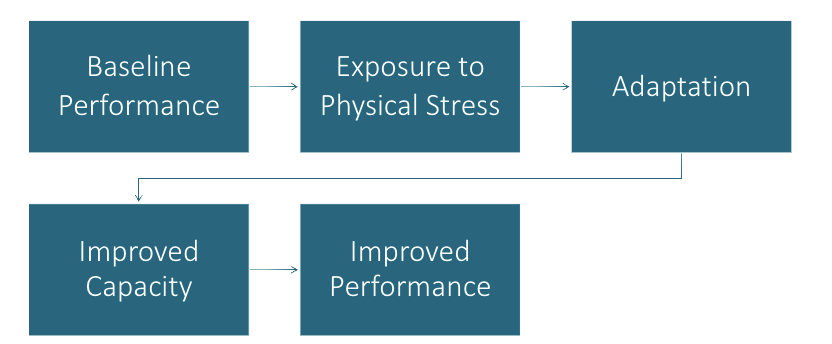
Progressive Overload
For an exercise program to be effective, continual and gradual increase in training stress is required; As the individual adapts, performance increases
Becomes capable of producing greater force, power, or endurance
Training stress needs to adjust to match new level of performance
Not just about increasing Volume or Load!
Manipulate training variables to match stimulus to goals
Physical Activity
Any bodily movement produced by the contraction of skeletal muscles that results in a substantial increase over resting energy expenditure
Exercise
Planned and structured physical activity designed to improve or maintain physical fitness
Physiological Responses During Exercise
Ventilatory Responses
Cardiovascular Responses
Cardiac output
Muscle blood flow
Blood pressure
Metabolic Response
Exercise Induced Ventilation Responses
Muscle and joint mechanoreceptors and
proprioceptors send afferent sensory signals to
the motor cortex. The descending pathways
from the motor cortex to the respiratory
control center in the medulla increase
ventilations early in exercise. A Feed forward
mechanism.
Chemoreceptors in the aorta and carotid
arteries monitor PO2, PCO2 and pH and
influence ventilation rate
Blood Flow Distribution
This is a very important concept.
The shunting of blood to areas of need is how the body supplies blood to the exercising muscles.
Notice the 5x increase in cardiac output
Blood Pressure Changes During Exercise
This is a very important concept.
Understanding the expected BP changes during exercise gives you insight into your patient’s tolerance and safety during exercise
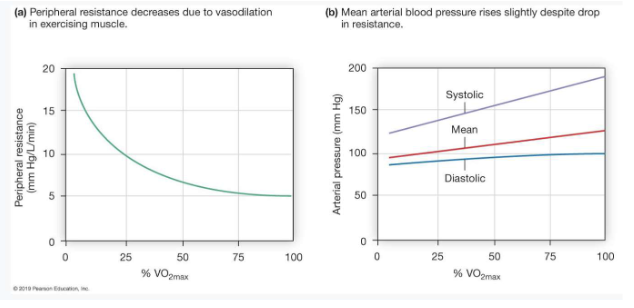
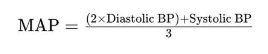
Mean Arterial Pressure (MAP)
Mean Arterial Pressure (MAP) can be defined using the formula
During Exercise: The increase in cardiac output and changes in vascular resistance during exercise lead to an increase in MAP.
Diastolic BP (DBP): The pressure in the arteries when the heart is resting between beats. This phase is longer and thus has a
greater influence on the average pressure over the cardiac cycle.
Systolic BP (SBP): The pressure in the arteries when the heart beats and pumps blood
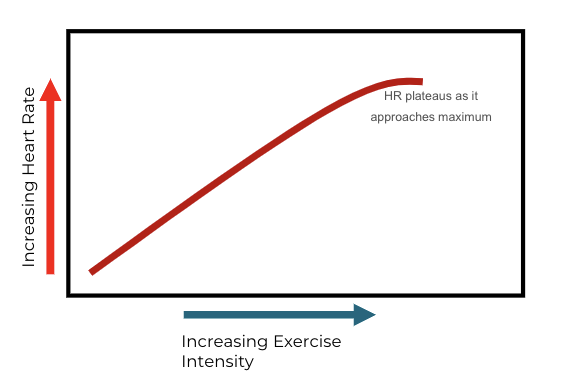
Heart Rate Changes During Exercise
HR should increase progressively and linearly with the intensity of exercise
This rise reflects the body's need to deliver more oxygen to working
muscles and to remove carbon dioxide and other metabolic byproducts
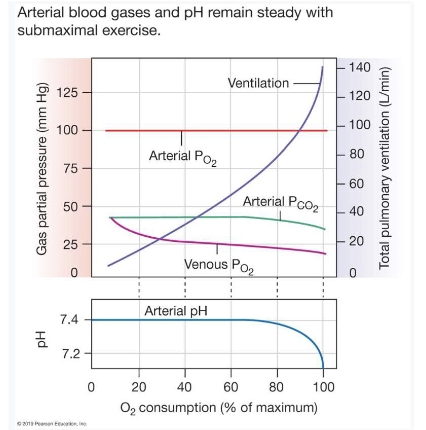
Blood Gases & Exercise
Note arterial PO2 remains steady during submaximal exercise. This is a normal exercise response If you are using a pulse oximeter on your .patient and observed decreasing oxygen levels – the exercise level is not being tolerated by your patient and should be stopped
Exercise Influences on Blood Glucose & Insulin Levels
Exercise has a positive effect on plasma glucose and insulin levels. It is important to educate your patients as to the role of exercise to improve and/or maintain appropriate plasma glucose levels especially with diabetic patients.
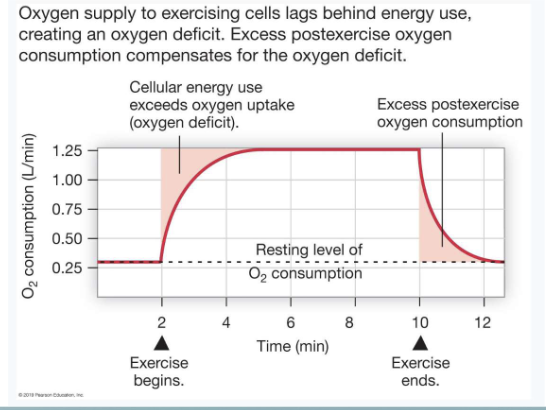
O2 Consumption & Exercise
When exercise begins there is a need for energy that is greater that what the body can produce using oxygen. This creates an oxygen deficit which is made up with additional sources of energy that do not require oxygen (phosphocreatine, and anaerobic glycolysis)
Oxygen delivery increases and there is a leveling where energy and oxygen needs are matching, referred to as “steady state”.
At the conclusion of exercise, oxygen consumption does not immediately return to resting levels but stays elevated for a period of time
Autonomic Nervous System
Enhance Cardiorespiratory Function:
Increases cardiac output and blood pressure.
Regulates blood flow and volume.
Decreases airway resistance.
Vascular Control:
Vasoconstriction redirects blood to active muscles.
Releases hormones to maintain fluid balance.
Energy Mobilization:
Increases lipolysis and glycogenolysis.
Mobilizes fatty acids and glucose.
Thermal Regulation:
Controls blood flow and sweat glands for temperature regulation.
Promotes heat loss through skin vasodilation and sweat.
Hemostatic Responses:
Increases blood clotting ability during physical stress.
Balances clot formation and breakdown.
Sympathetic and Parasympathetic Activity:
SNS activation enhances exercise capacity.
PSNS withdrawal initially raises heart rate
Autonomic Nervous System During Exercise
Sympathetic Nervous System Activation:
Triggers "fight or flight" response during exercise.
Increases heart rate and cardiac output.
Redirects blood to active muscles.
Promotes glycogen and fat breakdown for energy.
Increases respiratory rate for better oxygen uptake.
Parasympathetic Nervous System Functions:
Dominates "rest and digest" activities.
Modulates heart rate at lower exercise intensities.
Facilitates quick post-exercise recovery.
Dynamic Balance Between Systems:
Sympathetic dominance increases with exercise intensity.
Parasympathetic activity aids in recovery post-exercise.
Adaptation and Efficiency:
Regular exercise improves autonomic response
Trained individuals have higher parasympathetic tone and a responsive sympathetic system for better performance and recovery
Changes in response to training stimulus over time
Neurological, physical, and biochemical changes
Improved Performance
Same amount of work can be done at a lower
physiological cost
Significant changes observed in 10-12 weeks
Adaptation depends on the organism's ability to change in response to a training stimulus
Training Stimulus Threshold
Individual with low fitness level has more potential to improve
Individual with higher initial fitness level will require greater intensity stimulus to improve
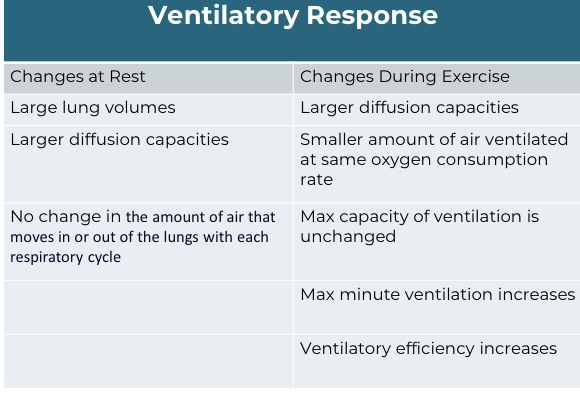
Physiological Adaptations to Exercise - ventilatory response