HEENT, Neck, Eyes, Ears, Nose, Mouth, Throat: Comprehensive Exam Guide
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
What are the four cardinal techniques of the physical exam?
Inspection, Palpation, Percussion, Auscultation.
What does inspection in a physical exam involve?
Close observation of the patient's appearance, behavior, movement, facial expression, mood, body habitus, skin conditions, eye movements, pharyngeal color, symmetry, abdominal contour, lower extremity edema, and gait.
What is palpation used for in a physical exam?
Tactile pressure to assess skin elevation, depression, warmth, tenderness, lymph nodes, pulses, organ sizes, and crepitus in joints.
How is percussion performed in a physical exam?
Using a striking finger to tap against a pleximeter finger on the chest or abdomen to evoke sound waves indicating resonance or dullness.
What is the purpose of auscultation in a physical exam?
To detect characteristics of heart, lung, and bowel sounds, including location, timing, duration, pitch, and intensity.
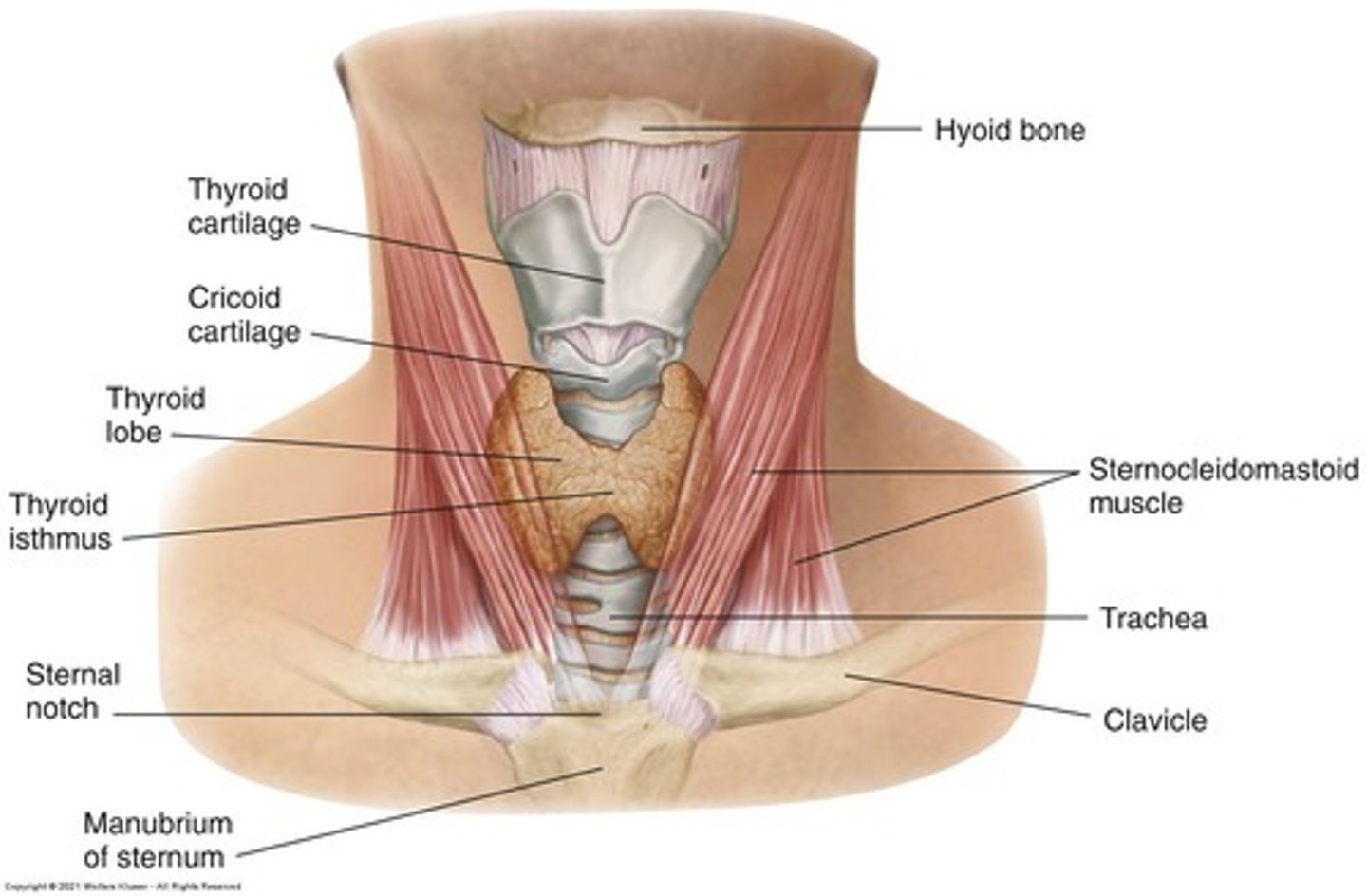
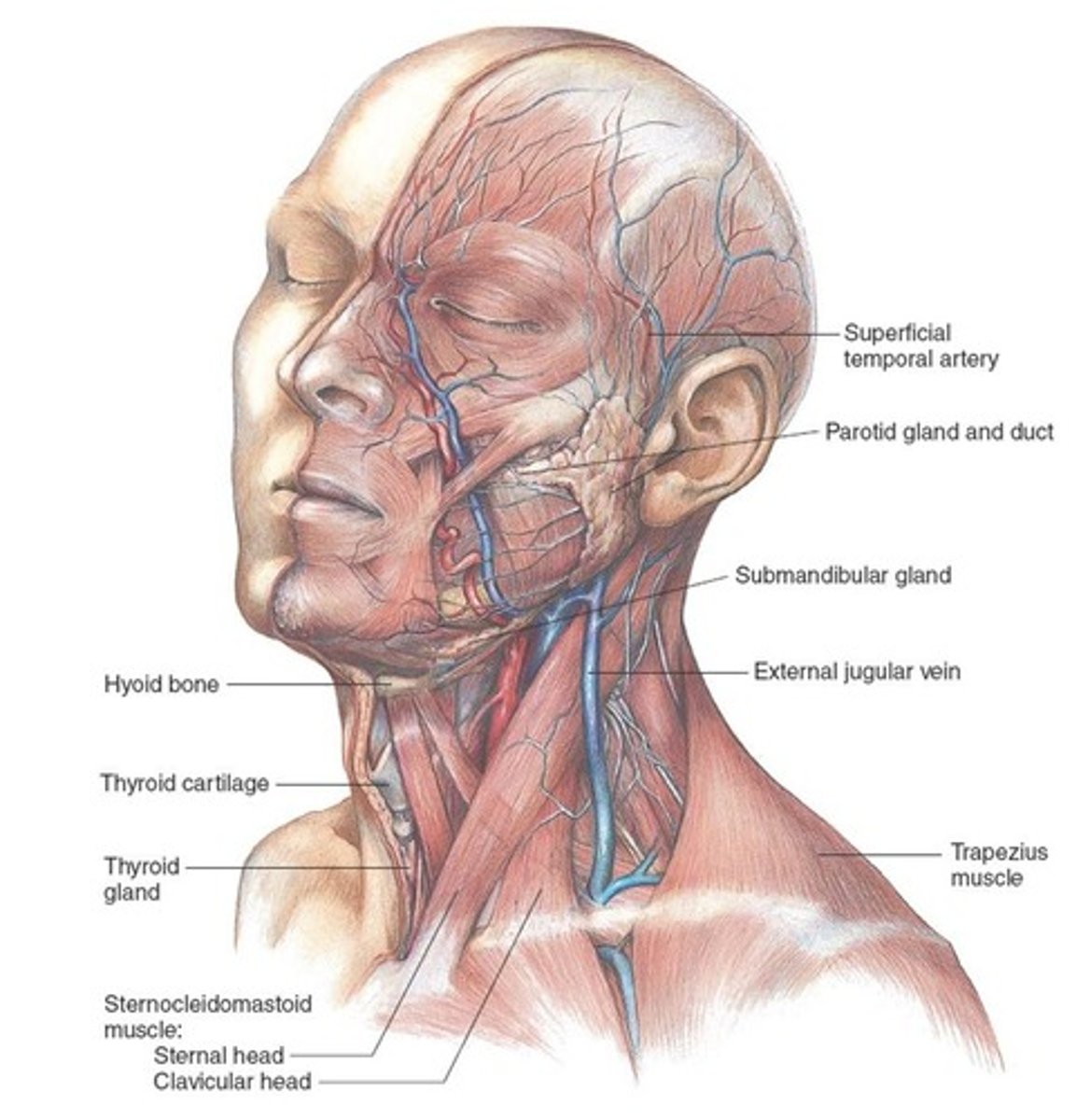
What should be inspected and palpated during a head and neck exam?
Hair, scalp, skull, face, lymph nodes, trachea, and thyroid gland.
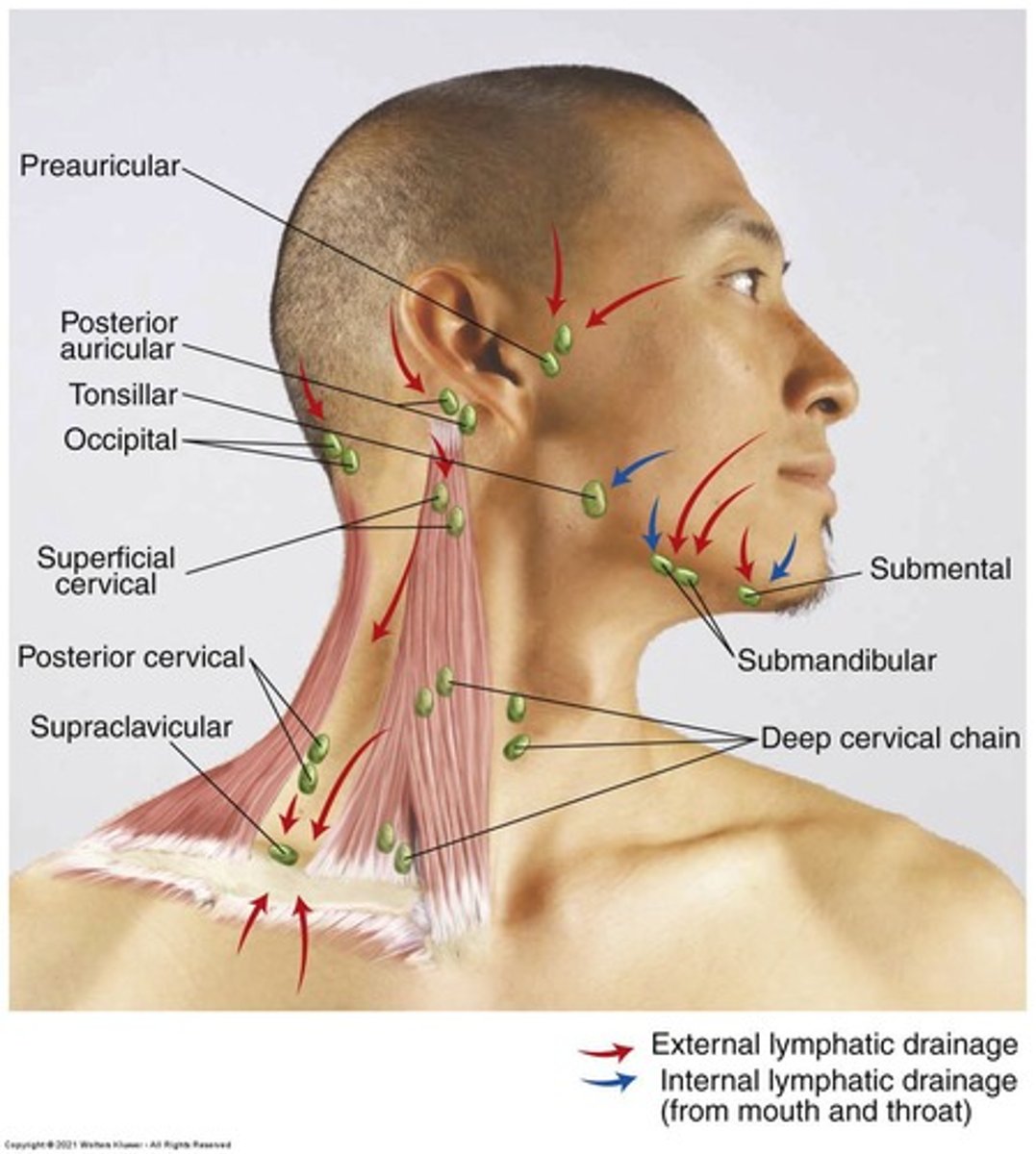
What specific aspects should be noted when inspecting the lymph nodes?
Size, shape, delimitation, mobility, consistency, and tenderness.
What is the significance of symmetry in a head and neck exam?
Asymmetry may indicate underlying pathology and should be carefully noted during inspection.
How should the thyroid gland be examined?
Inspect for size, uniformity, nodularity, and movement while palpating and observing the patient swallow.
What does auscultation over the thyroid gland check for?
The presence of a bruit, which may indicate hyperthyroidism.
What are normal findings for lymph nodes?
They should be small, mobile, discrete, and nontender, often referred to as 'shotty'.
What anatomical regions should be communicated using proper terminology during a head and neck exam?
Frontal, temporal, nasal, oral, auricular, mandibular, and mental regions.
What technique is used to palpate the thyroid gland?
Palpate between the cricoid cartilage and the suprasternal notch while the patient swallows.
What is the recommended position for the patient during a thyroid examination?
The patient should be seated or standing with the neck slightly flexed forward.
What should be observed when the patient swallows during a thyroid exam?
The upward movement of the thyroid gland, noting its contour and symmetry.
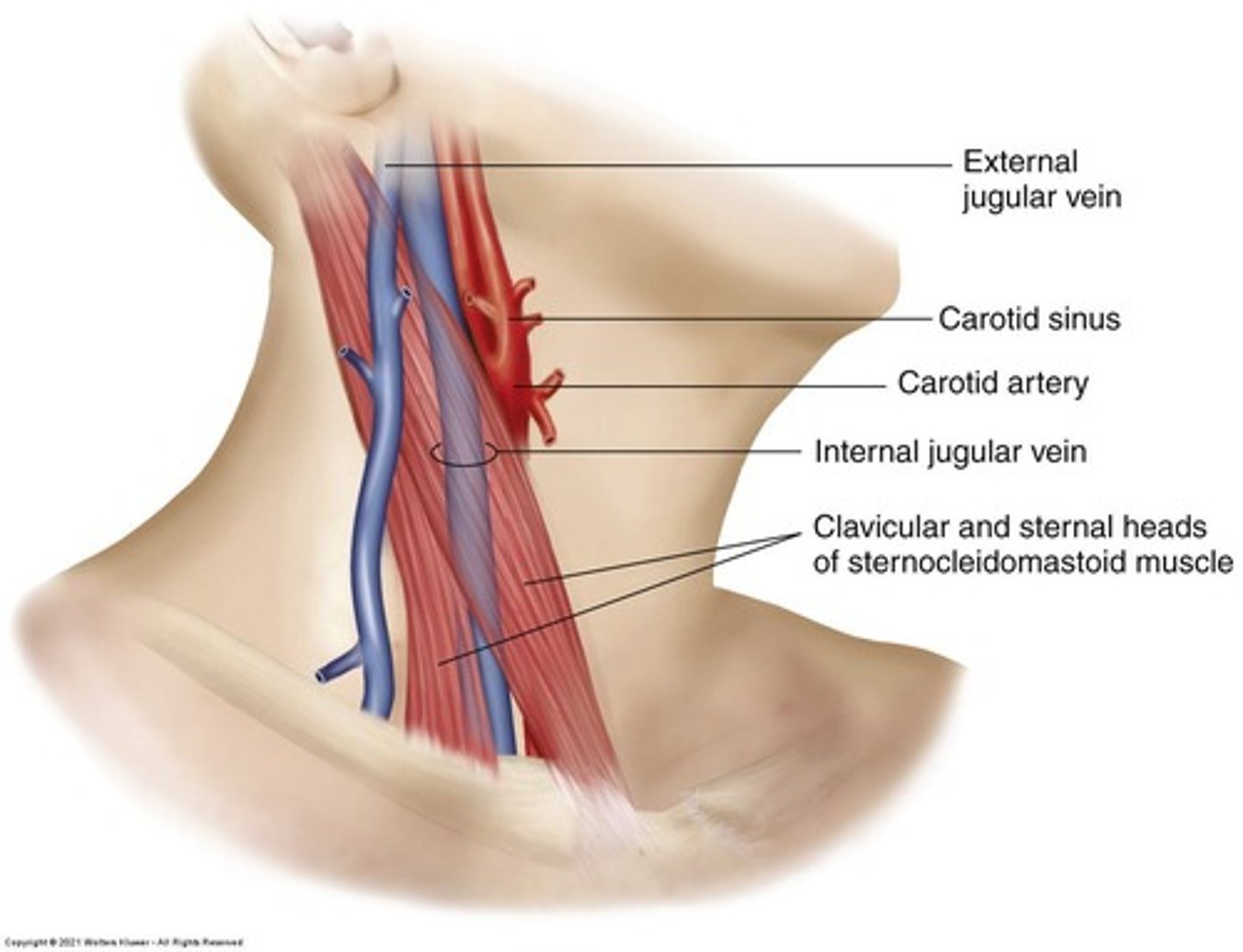
What is the definition of a bruit?
A sound similar to a cardiac murmur but not of cardiac origin, often described as a blowing sound.
What conditions may cause a bruit to be heard over the thyroid gland?
Hyperthyroidism from Graves disease or toxic multinodular goiter.
What is the technique for palpating lymph nodes?
Use the pads of the index and middle fingers in a rotary motion to assess the lymph nodes.
What should be done to ensure proper examination of the trachea?
Inspect and palpate for deviation and breath sounds.
What is the significance of using tangential lighting during a thyroid examination?
It helps to identify the contours of the thyroid gland more clearly.
What should be documented when describing lymph node size?
Document in two dimensions with maximal length and width (e.g., 1 cm x 1 cm).
What does supraclavicular lymphadenopathy (LAD) indicate?
Increased cancer risk.
What does the presence of hard or fixed lymph nodes suggest?
Malignancy.
What does generalized lymphadenopathy indicate?
Systemic illness.
What does tracheal deviation signify?
Mass effect.
What condition is indicated by a goiter?
Thyroid pathology.
How should head and neck exam findings be recorded?
Example: 'NC/AT. Trachea midline. No LAD. Thyroid not enlarged.'
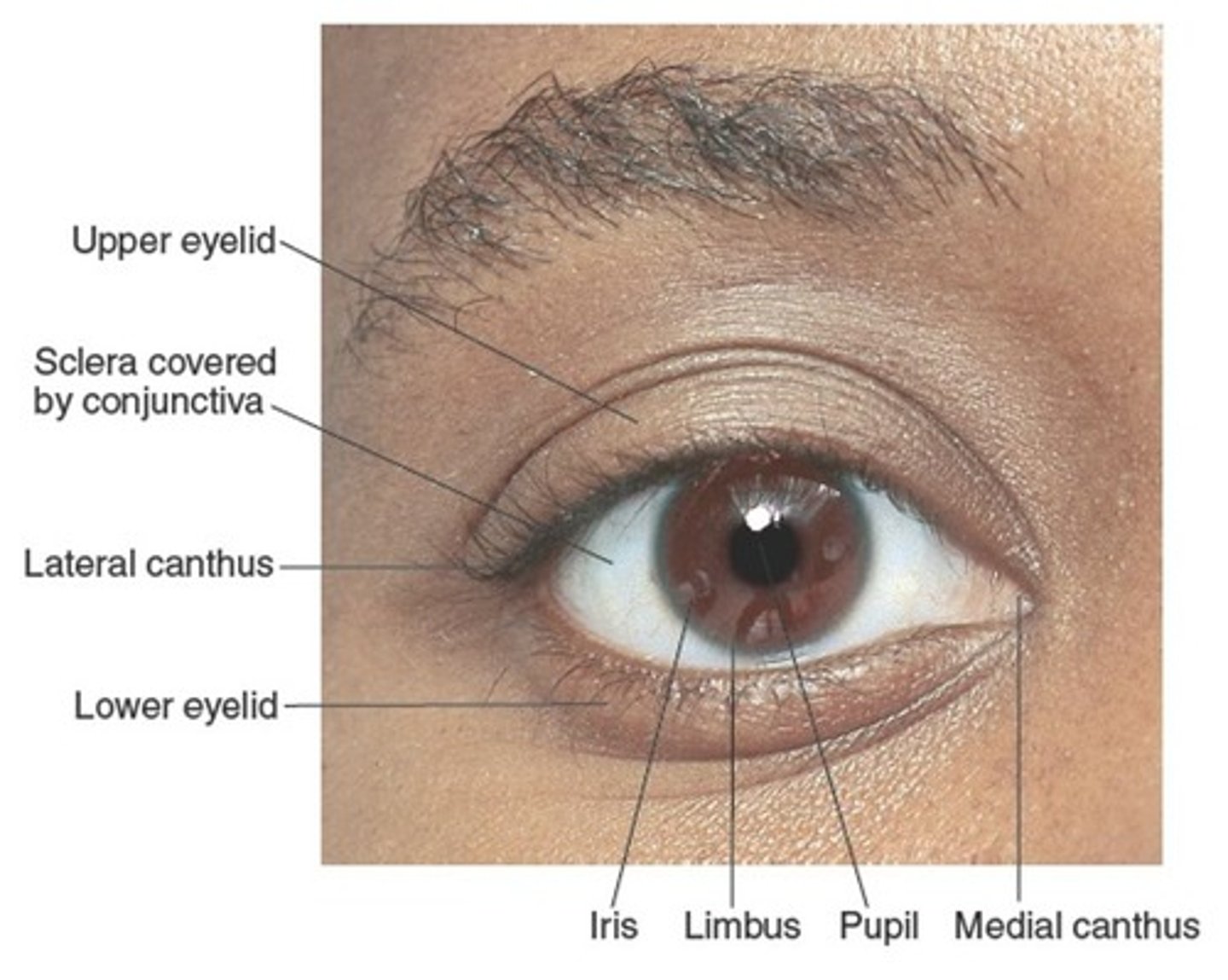
What does OD and OS stand for in eye examinations?
OD = right eye, OS = left eye.
What are key components of the review of systems (ROS) for eye exams?
Vision changes, pain, diplopia, discharge, trauma.
What should be inspected during a physical exam of the eyes?
Lids, conjunctiva, sclera, pupils, fundus.
What is the normal color of the optic disc during a fundoscopic exam?
Yellow/orange.
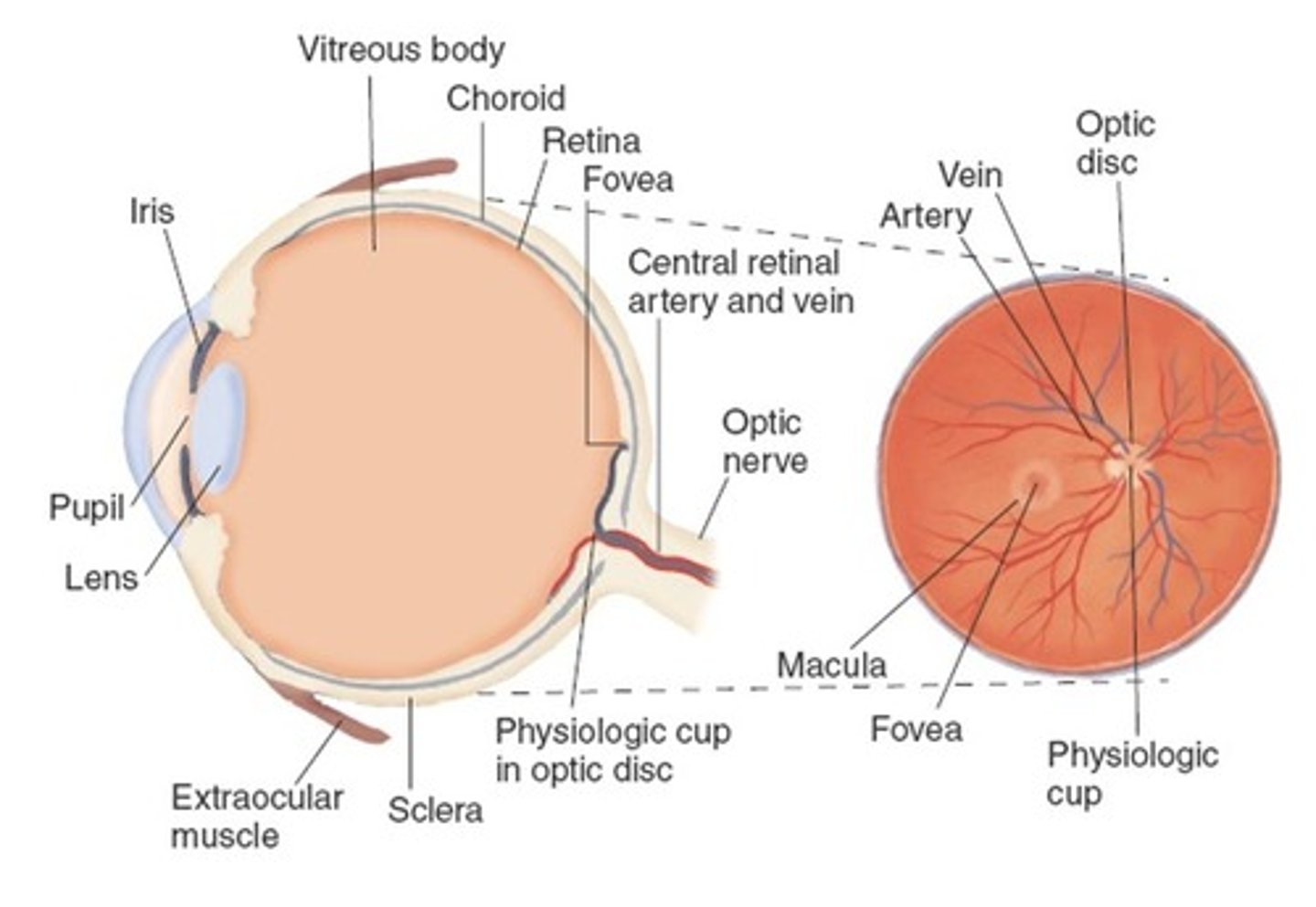
Where is the fovea located in relation to the optic disc?
Lateral to the disc.
What is the significance of the macula?
It is the region where the visual image arrives after passing through the cornea and lens.
What are the characteristics of a normal optic disc?
Color yellowish orange to creamy pink, tiny disc vessels, sharp margins.
What does flashing lights indicate in an eye exam?
Retinal detachment.
What does itching or redness suggest in an eye exam?
Conjunctivitis.
What cranial nerve is associated with visual field defects?
Cranial Nerve II (optic nerve).
What are the normal characteristics of pupils?
Equal in size, round, reactive to light and accommodation.
What is Adie's pupil?
A dilated pupil with slow reaction.
What does CN III palsy present as?
A blown pupil and ptosis.
What are the symptoms of Horner's syndrome?
Miosis, ptosis, and anhidrosis.
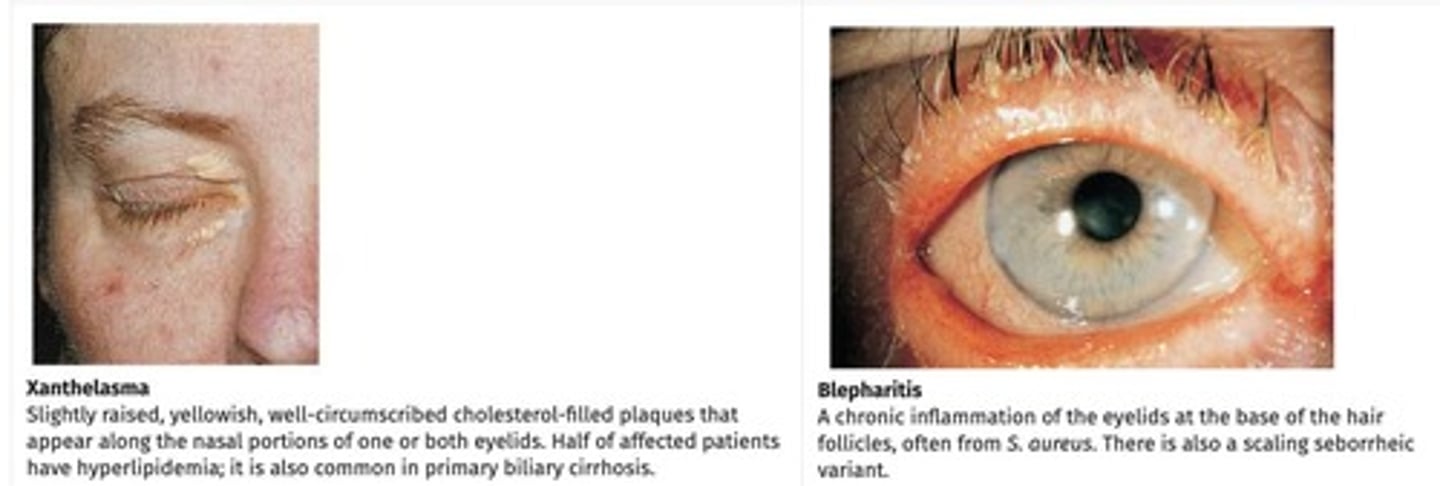
What are common eyelid disorders?
Ptosis, entropion, ectropion, exophthalmos, blepharitis, hordeolum, chalazion, xanthelasma.
What are some common eye conditions?
Conjunctivitis, subconjunctival hemorrhage, hyphema, iritis, glaucoma, episcleritis, corneal injury.
What is a pinguecula?
A benign, yellow corneal opacity.
What is a pterygium?
A triangular encroachment on the cornea.
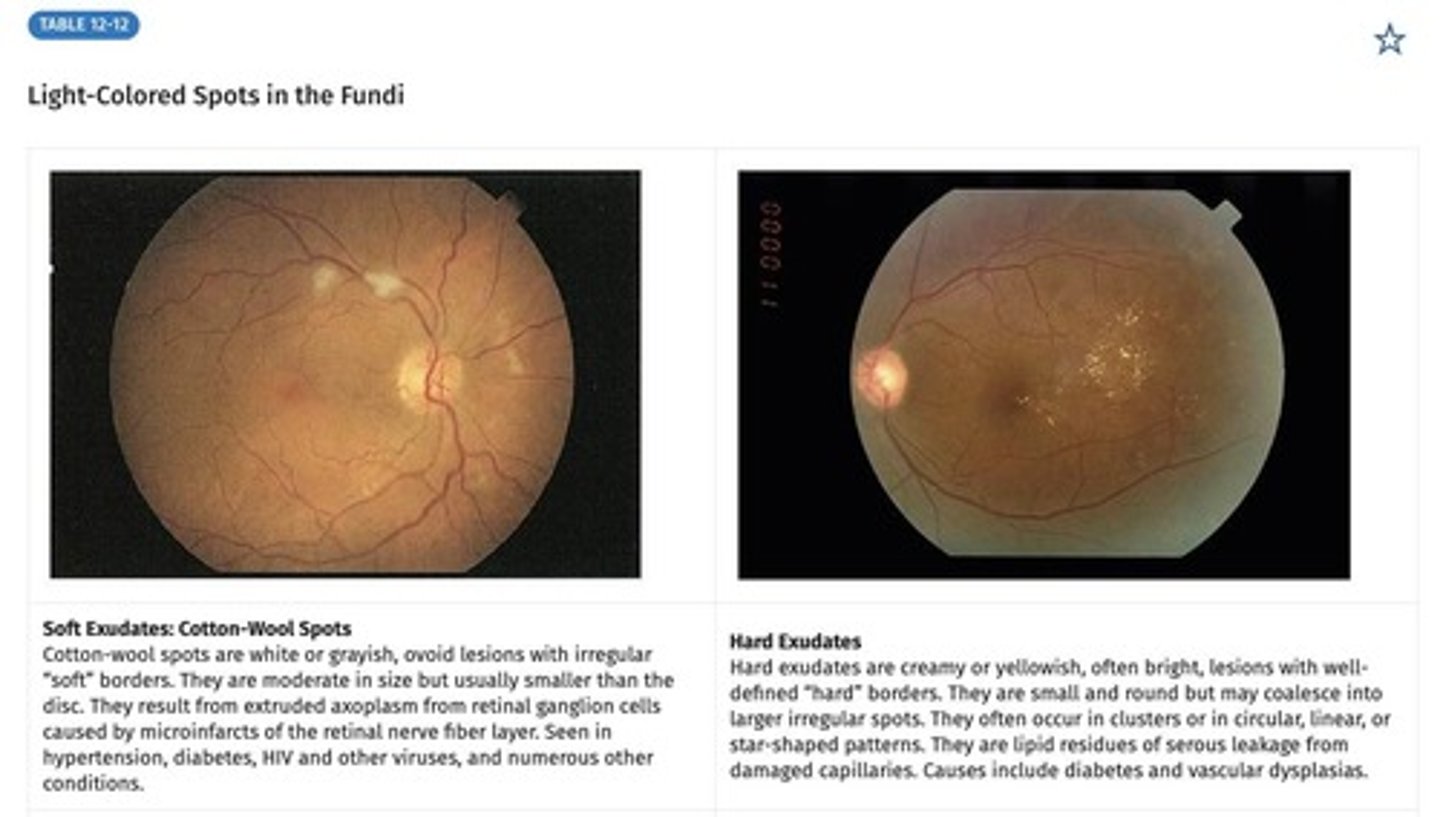
What are some fundoscopic abnormalities?
Hemorrhages, exudates, microaneurysms, drusen, papilledema, detachment, neovascularization.
What are the normal functions of the nose?
Warms air, humidifies air, and partially filters air.
What are the key components of the ROS for ear and nose complaints?
Ear: hearing loss, vertigo, pain, discharge, tinnitus; Nose: rhinorrhea, congestion, sinus pressure, epistaxis.
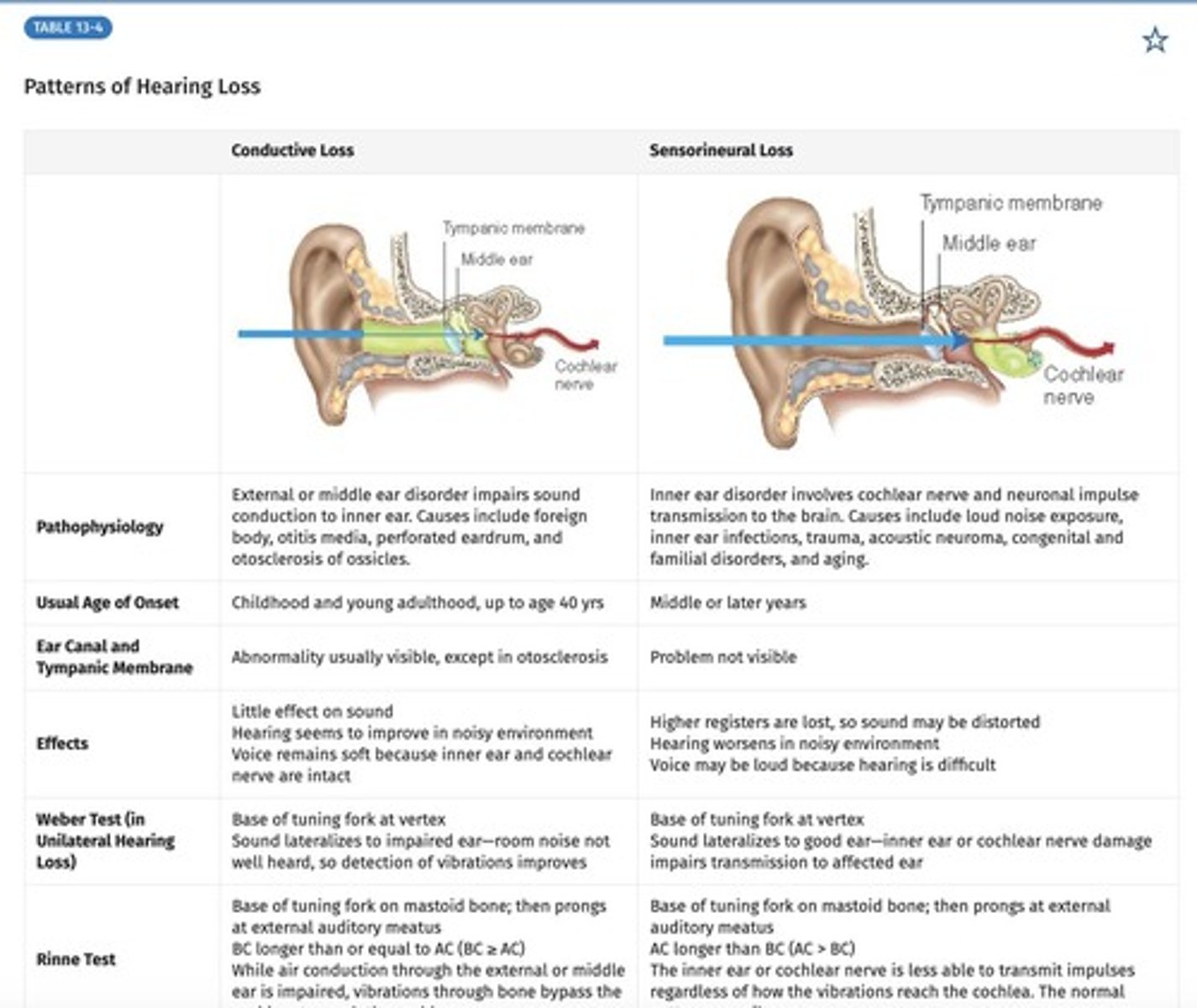
What is the difference between conductive and sensorineural hearing loss?
Conductive: problem with external/middle ear; Sensorineural: problem with inner ear or CN VIII.
What are the common physical signs of allergic rhinitis?
Allergic 'salute', nasal crease, and allergic 'shinners'.
What are potential complications of allergic rhinitis?
Avascular polyps may originate in the ethmoid sinuses and extend into the nasal airway.
What are the first-line treatments for allergic rhinitis?
Antihistamines (oral vs topical), decongestants (systemic or topical), and nasal corticosteroid sprays.
What medications can cause rhinitis?
Cocaine abuse, anticholinergic medications, overuse of oxymetazoline nasal spray, reserpine, beta blockers, hydralazine, oral contraceptives, ACE inhibitors, and PDE-5 inhibitors.
What is the treatment for drug-induced rhinitis?
Change medications.
How does pregnancy affect nasal mucosa?
Elevated hormone levels lead to a nasal mucosal response; estrogen receptors are present in the nasal mucosa.
What is the treatment for nasal congestion during pregnancy?
Saline nasal spray.
What characterizes vasomotor rhinitis in the elderly?
Imbalance of autonomic nervous system activity, chronic dry nasal mucosa, and clear rhinorrhea.
What treatments are available for vasomotor rhinitis?
Saline nasal spray, corticosteroid nasal spray, azelastine nasal spray, and ipratropium nasal spray.
What are the symptoms of viral rhinitis?
Mild to moderate congestion and clear rhinorrhea.
What bacteria are commonly associated with bacterial rhinitis?
Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.
What is the treatment for bacterial rhinitis?
Amoxicillin, Augmentin, or doxycycline for 5-7 days; second-line options include Augmentin, levofloxacin, and moxifloxacin.
What is acute bacterial rhinosinusitis (ABRS)?
Typically presents after a viral infection or failure to resolve after viral symptoms.
What environmental factors can contribute to rhinitis?
Dusty workplaces, toxic fumes, and irritants from hobbies or nearby factories.
What is atrophic rhinitis and who is it commonly seen in?
Usually occurs in the elderly, characterized by anatomical deformities of the nasal septum and turbinates, leading to a dry nose.
What are treatment options for atrophic rhinitis?
Premarin cream and corticosteroid nasal spray.
What are nasal polyps and how do they appear?
They are glistening, gray or white, mucoid masses in the nasal cavities and are most common with allergic rhinitis.
What is the treatment for nasal polyps?
They can be reduced with steroids or excised if they are persistently symptomatic.
What are septal defects and what can cause them?
Septal defects or perforations can be due to piercings, cocaine use, foreign bodies, rheumatologic diseases, or head and neck tumors.
What criteria indicate that a nasal bone X-ray is not needed?
Tenderness and swelling isolated to the bony bridge, the patient can breathe through each naris, the nose is straight, and no septal hematoma is present.
What is the common treatment for anterior epistaxis?
Local pressure for 10 minutes, identifying instigators, and possible use of oxymetazoline nasal spray.
What should be considered in adolescent males with nasal obstruction and bleeding?
Juvenile nasopharyngeal angiofibroma.
What characterizes acute sinusitis?
Symptoms include purulence, dental/facial pain, unilateral sinus tenderness, and usually follows an upper respiratory infection.
What is chronic sinusitis and its common treatment?
It lasts more than 12 weeks and may require surgery for symptomatic mucoceles.
What are the common symptoms of chronic sinus obstruction?
Chronic obstruction, congestion (pain/pressure), mucopurulent nasal drainage, and hyposmia.
What damage is typically seen in the sinus mucosa of chronic sinusitis patients?
The mucosa is typically damaged, thickened, and cilia are spotty throughout.
What is a primary treatment for chronic sinus issues related to tobacco use?
Stop tobacco use.
What pharmacological treatments are used for chronic sinusitis?
Antibiotics (Amoxicillin, Augmentin, Doxycycline, Levofloxacin), Oxymetazoline nasal spray (for 3-4 days only), Antihistamines, and Corticosteroid nasal spray.
What is barosinusitis?
A condition characterized by negative air pressure in one or more sinus cavities, which can occur acutely with rapid changes in ambient pressure or chronically with obstruction of the maxillary sinus ostia.
What are the consequences of disrupted aeration in the paranasal sinuses?
Painful symptoms may arise if aeration is disrupted, often due to nasal disorders like edema.
Which sinuses are particularly susceptible to trauma?
Frontal, Ethmoid, and Maxillary sinuses.
What are the characteristics of benign tumors in the nasal cavity?
Benign tumors include inverted papilloma (most common in the lateral nose wall) and squamous papilloma.
What is the prevalence of juvenile nasal angiofibroma?
It occurs in teenage males and represents 0.5% of head and neck cancers.
What are common symptoms of malignancies in the nasal cavity?
Nasal obstruction, congestion, proptosis, visual changes, diplopia, facial pain or numbness, and bleeding.
What is the Mallampati Score used for?
To assess airway and visualization of the soft palate.
What percentage of children aged 5 to 19 years have untreated dental caries?
19%.
What is the prevalence of dental caries among adults aged 20 to 64 years?
91%.
What risk factors are associated with periodontal disease?
Low income, male sex at birth, smoking, diabetes, and poor oral hygiene.
What is the recommended frequency for dental exams?
Annual dental exams, or every 6 months if covered by insurance.
What are the main causes of oropharyngeal cancer?
Alcohol and tobacco use cause 75% of cases.
What is the significance of HPV in oropharyngeal cancer?
HPV is associated with 70% of tonsillar, base of tongue, and oropharynx cancers.
What should be included in the ROS for oral/throat complaints?
Pain, dysphagia, odynophagia, hoarseness, lesions, and bleeding.
What are the common risk factors for oral diseases?
Age over 45, smoking, and alcohol use.
What is the most common type of oral cancer?
Squamous cell carcinoma (SCC), which occurs 90% of the time.
What is geographic tongue?
A recurrent inflammatory disorder affecting the dorsum of the tongue, characterized by local loss of filiform papillae leading to red patches with white, polycyclic borders.

What symptoms might patients with geographic tongue experience?
Patients are usually asymptomatic or may experience mild symptoms, oral discomfort, burning, and sensitivity to some foods.
What characterizes Black Hairy Tongue?
Elongated filiform papillae and yellowish to brown discoloration of the tongue surface, associated with smoking, antibiotic use, dehydration, Candida infection, and poor oral hygiene.
What is Angular Cheilitis?
Softening to fissuring of the skin at the angles of the mouth, often affecting people with no teeth or ill-fitting dentures, leading to potential secondary Candida infection.
What is Actinic Cheilitis?
A precancerous condition resulting from excessive sunlight exposure, primarily affecting the lower lip, characterized by scaly, thickened, and slightly everted skin.
What triggers HSV-1 (oral herpes)?
Recurrent episodes triggered by sun, stress, or illness, presenting with tingling, burning, vesicles, and potentially lymphadenopathy.
What is Angioedema?
Localized subcutaneous or submucosal swelling caused by fluid leakage, usually benign but can be life-threatening if it involves the larynx or develops into anaphylaxis.