HTHSCI 2LA2B - Depression
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
Statistics of Depression
- ~10% of Canadians affected by mood disorders
- Suicide in ~15% of individuals with major depressive disorder
- Twice as prevalent in women than men: Men less likely to seek help; Depression often masked by somatic complaints in men
Mood Disorders
- Disorders of emotion
- Including mania and depression
Depressive Disorders
Major Depressive Disorder:
- Characterized by a persistent unpleasant mood
Dysthymia:
- Characterized by chronic mild depressive symptoms
- Less intense symptoms, but last longer
Major Depressive Disorder
- Depressed mood
- Anhedonia (inability to experience pleasure)
- Feelings of worthlessness or excessive guilt
- Decreased concentration
- Psychomotor agitation or retardation, insomnia or hyper insomnia, decreased libido
- Changes in weight or appetite
- Thoughts of death or suicidal ideation
Sub-Classifications of Depression
Specifiers Used with a Diagnosis of Major Depressive Disorder:
- With anxious distress
- With mixed features
- With melancholic features
- With atypical features
- With mood-congruent or incongruent feature
- With catatonia
- With peripartum onset
- With seasonal pattern
Ex. Disruptive mood dysregulation disorder, persistent depressive disorder, premenstrual dysphoric disorder, depressive disorder due to another medical condition, substance/medication-induced depressive disorder, specified and unspecified depressive disorders
Major Depressive Disorder - DSM 5 Criteria for Depression
- Five (or more) symptoms must be present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure
Risk Factors for Depression
- Childhood emotional, physical, and sexual abuses
- Prior episode of depression
- Family history of depressive disorder
- Lack of social support
- Stressful life event
- Current substance abuse
- Economic difficulties
Etiology of Depression
- Multi-Factorial
Dynamic interplay Amongst:
- Genetic predisposition
- Environment
- Life history
- Development
- Biological challenges
*Believed that major depressive disorders arise from complex interaction of genes and environmental factors
Genetic Environment Interaction for Depression
Genes & Depression
- Certain variation in genes (polymorphisms) may increase the risk for depression
The serotonin transporter gene is the most studied for depression:
- Because it contains a polymorphism that gives rise to two different alleles long and short
- The short allele slows down the synthesis of the serotonin transporter which is thought to reduce the speed with which serotonin neurons can adapt to changes in their stimulation (leads to a dysregulation of serotonin)
Brain Derived Neurotropic Factor (BDNF) - Genetic Predisposition
- Important role in birth, survival and maturation of brain cells during development
- Important for neuronal cell growth and synaptic changes that occur throughout a person's life
- Activates DNA binding factors that stimulate gene transcription of genes involved in serotonin function (i.e. serotonin transporter, tryptophan hydrolase, serotonin synthesizing enzyme); stimulates expression of the BDNF factor gene
- Believed that BDNF may be the link between stress, neurogenesis, and hippocampal atrophy in depression
- People diagnosed with major depressive disorder have lower levels of BDNF
Alleles val/met Genotype (polymorphism) - BDNF
- Val and met alleles in gene that codes for BDNF
- People with met allele increases a person's vulnerability to depression
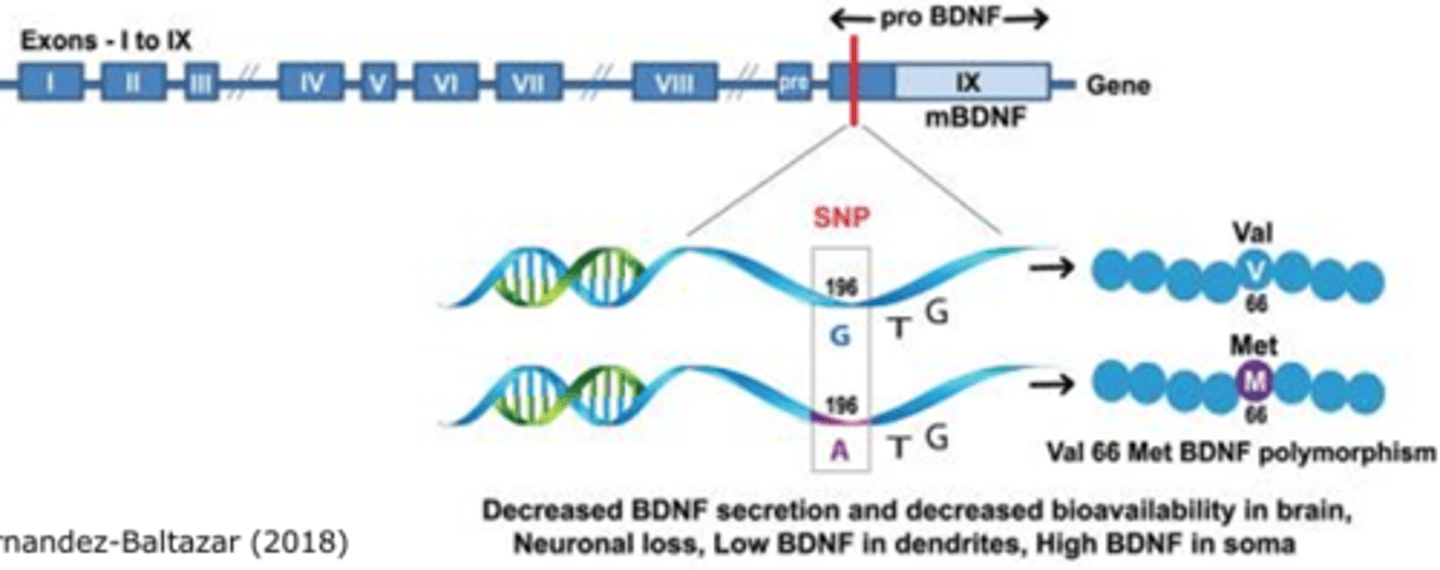
Met Allele
- Found to have relatively small hippocampus at birth, hippocampal hypo activity at rest, hippocampal hyper activation during learning, and relatively poor hippocampus-dependent memory function
- Having this allele increases the vulnerability to depression
Low Levels of BDNF
- The hippocampus and prefrontal cortex of symptomatic depressed patients, and serum studies have shown that serum levels of BDNF are abnormally low in patients with e major depressive disorder
Hippocampus & Depression
- Significant to depression because it is believed to modulate the cognitive aspects of depression such as memory impairments and feelings of hopelessness, guilt, doom, and suicidality
Neurobiological Theory
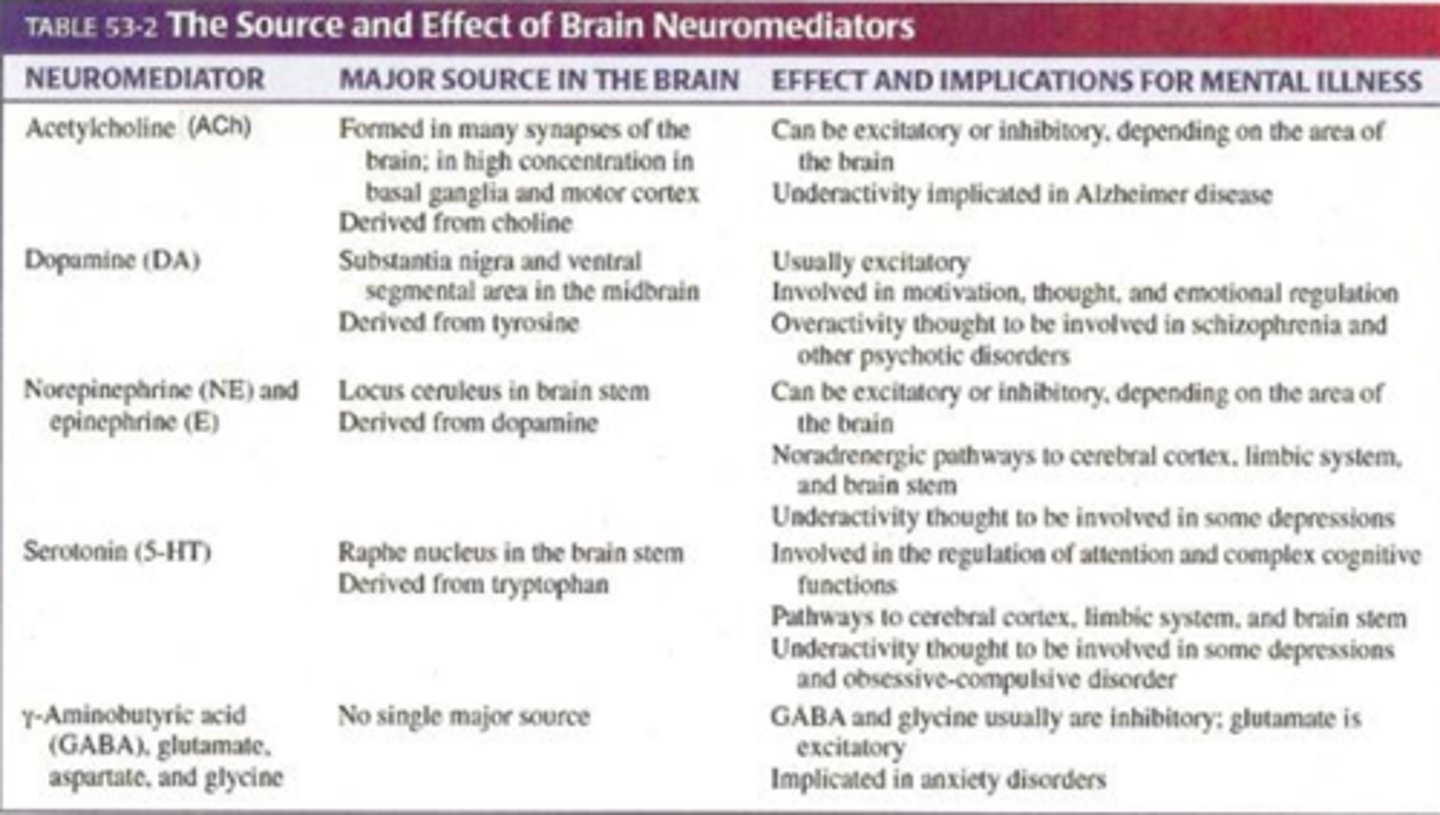
Neurobiological Theory Explanation
- Suggests that major depression is caused by a deficiency or dysregulation in the central nervous system concentration of neurotransmitters
- Norepinephrine and serotonin under-activity is thought to be involved in the development of depression
Neurotransmission
- How nerve cells communicate with one another
- Synapse: Nerve cells communicate by electrochemical signals which cross the point at which two neurons meets
- Neurotransmitters: Released from the axonal terminal of one neuron (presynaptic), the neurotransmitter then crosses the synapse and binds to receptors of the postsynaptic cells and causes an excitatory or inhibitory action
- Cortex: New part of the brain, filters and orders the outside world for us (allows us to see, touch, hear, and speak); plans, thoughts, and ideas originate in this layer
- Receptor Sites: Receive nerve signals and allow for an effect to form through forming electrical signals through ions in post synaptic neurons
Steps of Neurotransmission
1. The synthesis of a transmitter substance
2. The storage and release of the transmitter
3. Binding of the transmitter to receptors on the postsynaptic membrane
4. Removal of the transmitter from the synaptic cleft
Neurotransmitter Synthesis & Release - Synaptic Transmission
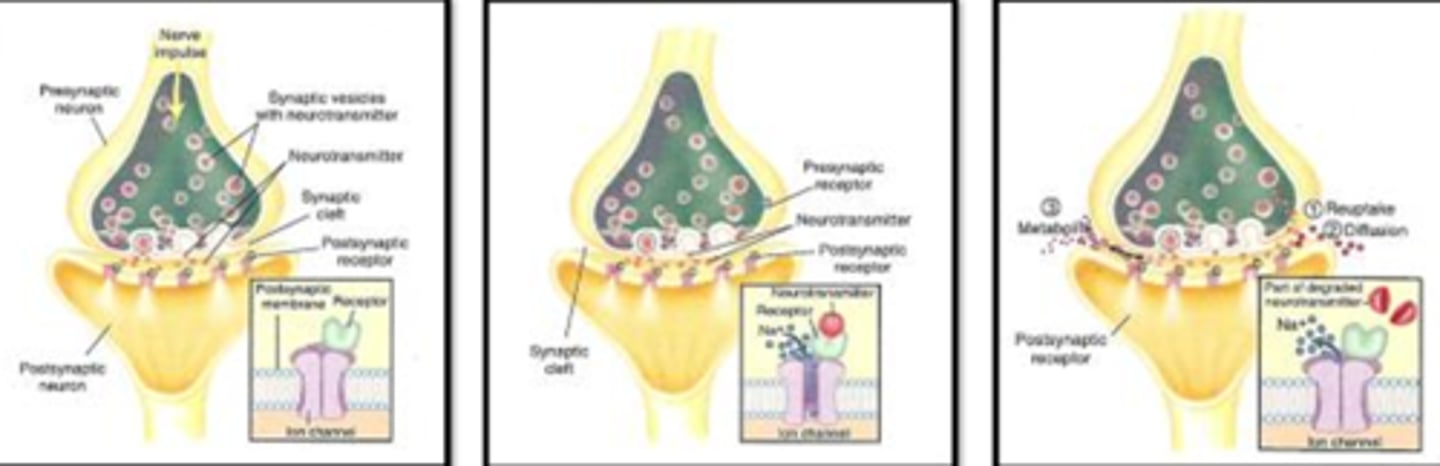
Step #1 - Synthesis & Release
- Neurotransmitters are synthesized in the presynaptic neuron, and then stored in synaptic vesicles
- Communication between the 2 neurons begins with a nerve impulse that stimulates the presynaptic neuron, followed by movement of the synaptic vesicle to the cell membrane and release of the neurotransmitter into the synaptic cleft
Step #2 - Receptor Binding
- Once released from the presynaptic neuron, the neurotransmitter moves across the synaptic cleft and binds to receptors on the postsynaptic neuron
- The action of a neurotransmitter is determined by the type of receptor (excitatory or inhibitory) to which it binds
- Binding of a neurotransmitter to a receptor with an excitatory function often results in the opening of an ion channel (i.e. sodium)
- Many presynaptic neurons also have receptors to which a neurotransmitter binds
- The presynaptic receptor function in a negative feedback manner to inhibit further release of the neurotransmitter
Step #3 - Neurotransmitter Removal
- Precise control of synaptic function relied on the rapid removal of the neurotransmitter from the receptor site
A Released Neurotransmitter:
- Be taken back up into the neuron in a process called reuptake
- Diffuse out of the synaptic cleft
- Be broken down by enzymes into inactive substances or metabolites
Neurotransmitters
- Typically stored in the vesicles in the presynaptic axonal terminal and released by the process of exocytosis
Biogenic Amine Hypothesis
Serotonin & Norepinephrine:
- Decreased levels
- Due either to decreased presynaptic release or decreased postsynaptic sensitivity, is the underlying pathologic process in depression
Dopamine:
- Decreased in depression
- Increased in mania
- Frequency of depression is higher in patients with Parkinson's disease which is caused by lower rates of dopamine production in the substantia nigra
*Healthy individuals without a personal or family history of major depressive disorder tend to not show any mood changes, while persons who have been successfully treated with serotonin-reuptake inhibitors will relapse into depression
*Lowering serotonin factors doe not induce depression in all people
Prefrontal Cortex - Neurophysiology of Symptoms
Prefrontal Cortex:
- Reduced volume and activity
- Part of the cerebral cortex which covers the outermost part of the brain which is the most evolved portion of our brain
- Contains the centers for elaboration of thought, voluntary motor and sensory functions, speech, and memory patterns and has extensive connections with deeper parts of the brain
PET Scan:
- Variable brain tissue uptake of an infused radioactive substance
- Drugs can be infused to study neurotransmitter receptor activity or concentration in the brain
MRI:
- Helps to diagnose structural abnormalities of the brain and can distinguish between grey and white matter
Gray Matter:
- Contains neuronal cell bodies, dendrites, unmyelinated axons, axon terminals, and neuroglia
Prefrontal Cortex
- Reduced and less active because of a decrease in the neurotransmission of serotonin and norepinephrine, and alterations in the neurotransmission of dopamine in this area
- Decrease in BDNF in the prefrontal cortex; leads to a decrease in neuronal volume because pathways are not being used, so density of these pathways decreases and there is a pruning of these pathways
Frontal & Temporal Lobes - Neurophysiology of Symptoms
*Decreased functioning
Frontal Lobe:
- Integrates and interprets somatic or bodily, visual, and auditory information that is critical for recognition of the familiar, as well as appropriate interpretation of and response to social contexts (emotion and language)
Temporal Lobe:
- Responsible for the modulation and fine-tuning of emotion appropriate to the level of intensity
- Responsible for planning, problem solving, intellectual insight, judgement, and expression of emotion
- Limbic system located here and regulates emotional behaviour
Amygdala - Neurophysiology of Symptoms
- Increased blood flow and oxygen consumption during depression
- Abnormal neurodevelopment
- Located deep in the medial temporal lobe in the primitive part of our brain
- Receives neuronal signals from the temporal and occipital lobes of the cortex and communicates with the hypothalamus and other parts of the limbic system
- Helps a person relate to the surrounding environmental and pattern appropriate behaviour
- Important in emotional function and regulation, the modulation of affective responses in social settings, as well as sexual arousal, aggression, and fear responses
- Important in emotional memory, and are believed to mediate the anhedonia (decreased drive and regard for pleasurable activities), anxiety, and reduced motivation symptoms of depression
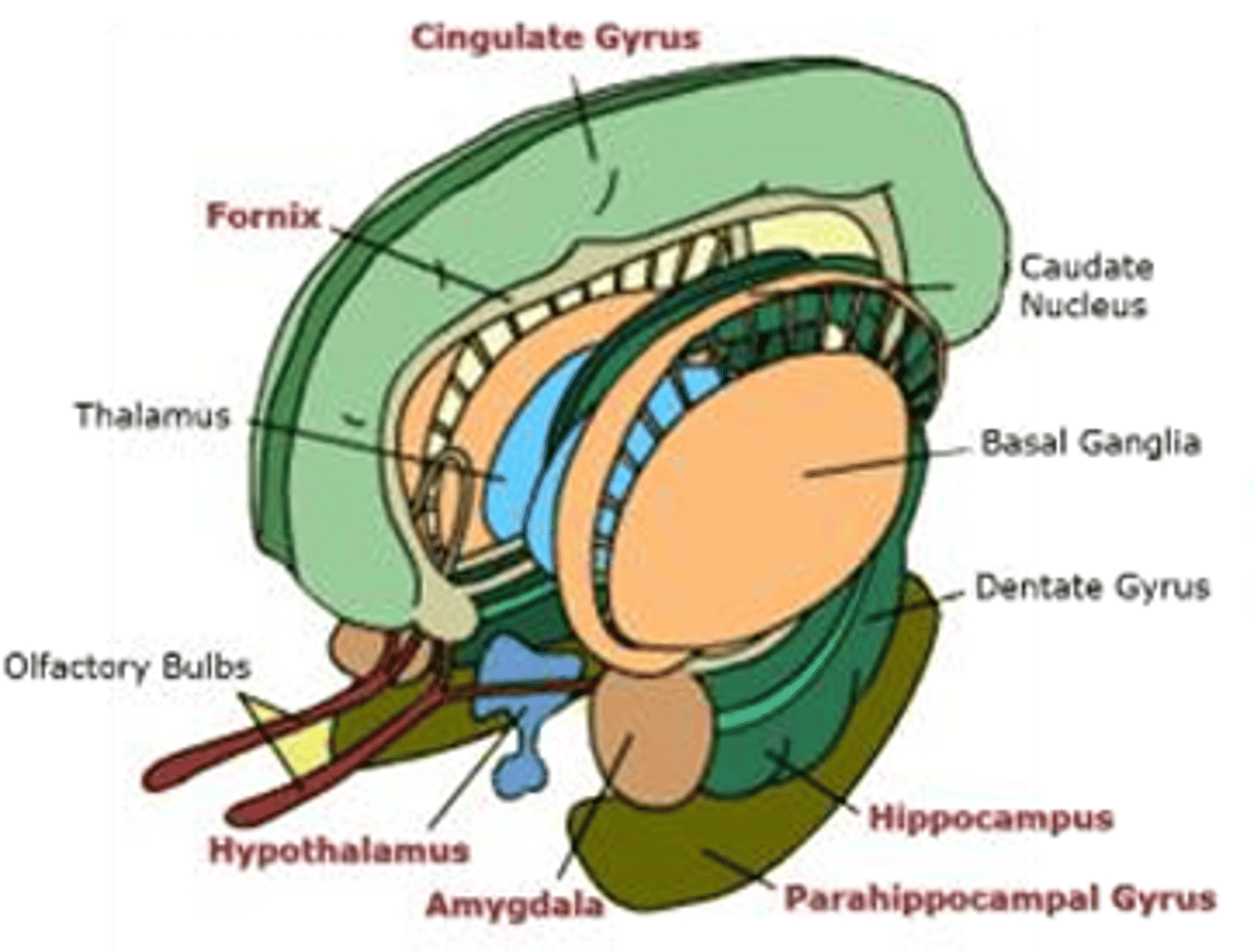
Limbic System - Neurophysiology of Symptoms
- Limbic system and Basal Ganglia are involved in the development of mood disorders and regulates our emotional behaviour
- Includes the hippocampus, parahippocampal gyrus, cingulate gyrus, amygdala, and a bridge like structure called the fornix which connects the hippocampus with the hypothalamus
- The neurocortex and hippocampus are thought to mediate cognitive aspects of depression, such as memory impairments and feelings of worthlessness, hopelessness, guilt, doom, and suicidality
- Changes in the hypothalamus are believed to be responsible for the neurovegetative symptoms of depression (i.e. too much or too little sleep, appetite and energy, loss of interest in sex and pleasurable activities)
- Dysregulation of serotonin, norepinephrine, and dopamine results in abnormality of connectivity within the limbic system and may also explain symptoms of emotional liability, irritability, and suicidality
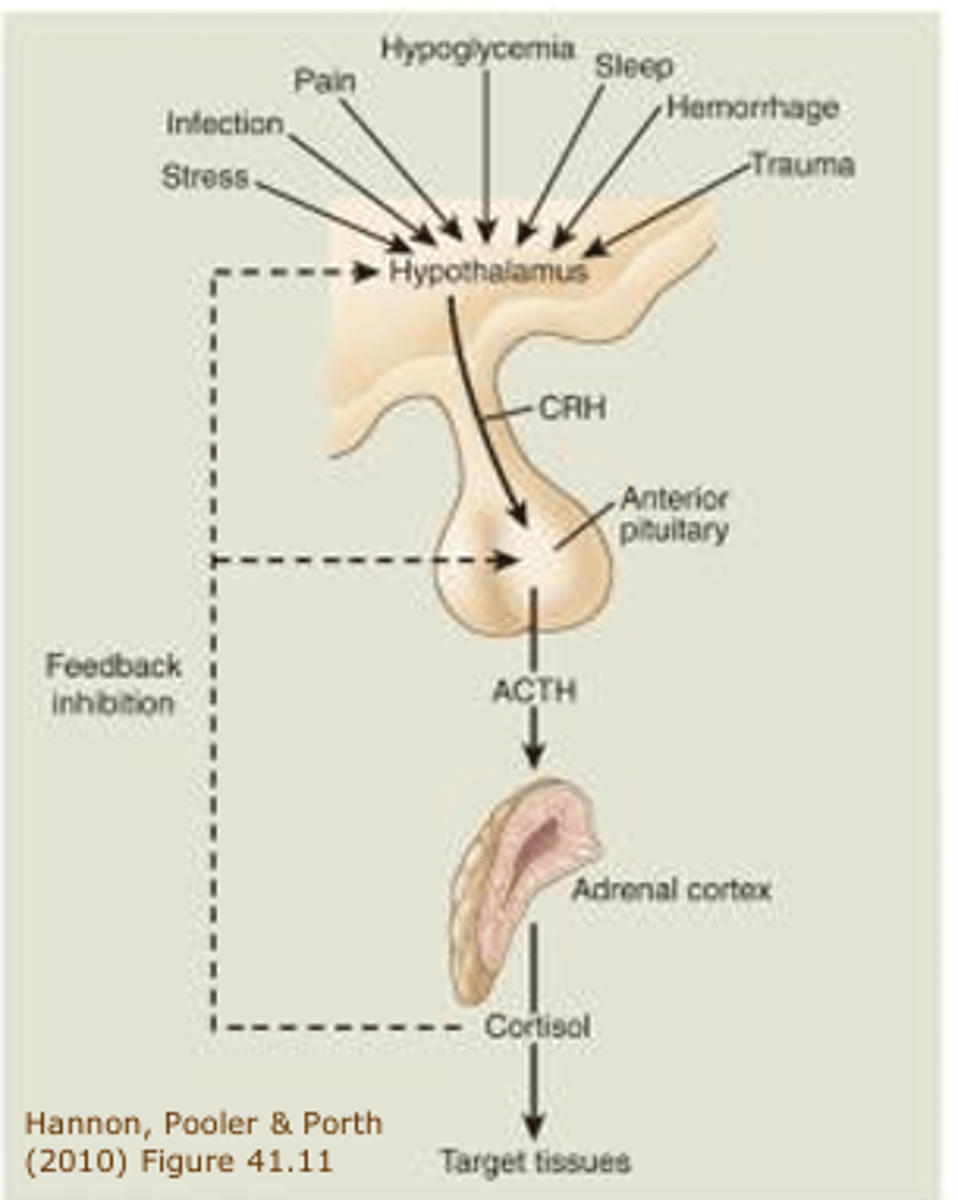
Hypothalamic-Pituitary-Adrenal Axis (HPA) - Neuroendocrine System
People with depression have increased levels of: - CRF
- Cortisol: Disturbances in the function of the HPA axis in depression cause cortisol levels to spike erratically throughout the day
With childhood stress:
- Chronic disinhibition of HPA axis
- Exaggerated stress response as adults
Major Depressive Disorder:
- Stress activated the amygdala and norepinephrine systems causing symptoms of increased vigilance and fear, and people had an exaggerated stress response and increased levels of CRF and norepinephrine in the plasma
Hypothalamic-Pituitary-Adrenal Axis (HPA)
Pathway Changes that Lead to Depression
Changes in pathways that influence the activity of neurotransmitters:
- Thyroid function (depressed patients with decreased thyroid function are given thyroid replacement therapy in order to reverse this process and speed up their ability to metabolize and respond to treatment with antidepressant medication)
- Sleep-wake cycle (normal sleep cycle is often reversed in depressed individuals where the person reaches deep sleep earlier in the cycle; melatonin may be used for treatment)
- Circadian Rhythms (regular cycles of sleep and waking and body functions such as temp regulation and hormone secretion based on changes in the 24 hr light-dark solar day; patients with depression have circadian abnormalities of mood, sleep, temp, and neuroendocrine secretion; treatment sedative medication may be used and patients are taught sleep hygiene techniques)
- Cytokine dysregulation (dysregulation of cytokines can result in adverse effects and may manifest as symptoms of major depression and related disorders)
Depression & Dysregulation of Cytokines
- Depression is common in infectious and autoimmune diseases
- Exposure to cytokines induces depressive symptoms and cytokine secretion is increased in major depression
- Antidepressants have anti-inflammatory effects and have been used to treat chronic pain
Depression & Serotonin
- Decreases in the availability and action of serotonin at the nerve synapse may be manifested as increased subjective experiences of pain and complaints of physical symptoms of which may be indicative of a depressive illness
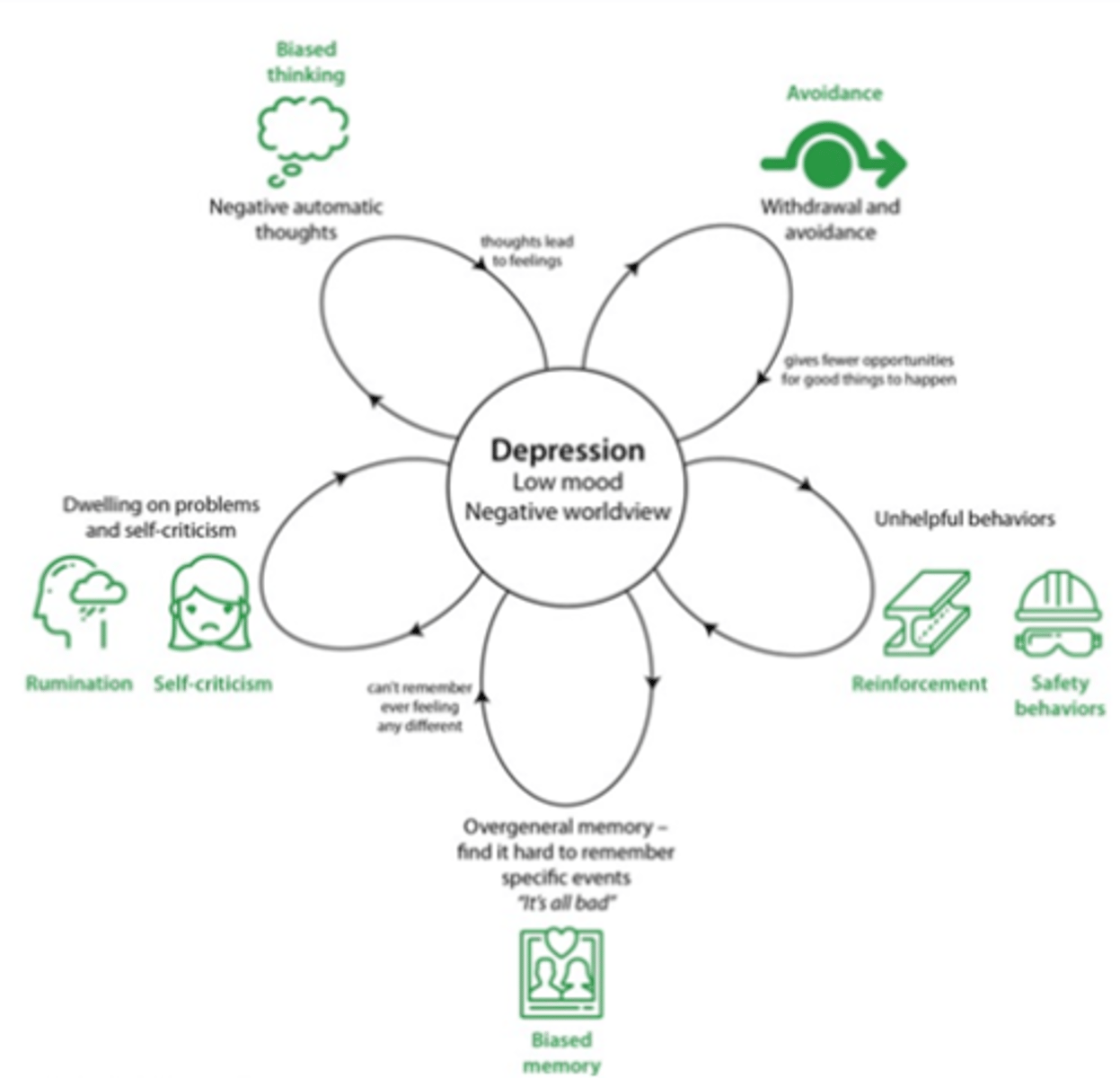
Environmental - Theories of Causation for Depression
- Psychodynamic factors (negative beliefs)
- Behavioural factors (decrease in pleasurable activities)
- Developmental factors (parenting)
- Family distress
- Social factors
Psychodynamic Factors
- Involve distorted negative beliefs and thoughts about the self, the environmental, and the future that can induce and perpetuate depressive symptoms
Behavioural Factors
- Involve a severe reduction in rewarding activities or an increase in unpleasant events in one's life that result in depression and further restriction of activity, decreasing the likelihood of experiencing pleasurable activities and intensity a mood disturbance
Developmental Factors
- Involve loss of a parent or lack of emotional adequate parenting that may delay or prohibit the realization of appropriate developmental milestones
Family Distress
- Involves a disruption in family dynamics involving maladaptive circular patterns in family interactions that contribute to the onset of depression in family members
Social Factors
- Adverse or traumatic life events especially that involve the loss of an important human relationship or role in life that is followed by a depression
Antidepressant Drugs - Treatment
- SSRIs
- MAOIs
- TCAs
- Novel or Dual antidepressant drugs
*Clinical antidepressant effects occur only after chronic administration of days to weeks
*These drugs normalize levels of serotonin, dopamine, and norepinephrine in the brain and thus their neurotransmission at the synapse
*Antidepressants also increase levels of BDNF and affect synaptic plasticity by increasing the activity of neurotransmitters in the synapse and nerve cell volume
*Antidepressant response takes days to weeks because it requires sufficient time for the levels of BDNF to gradually rise and exert synaptic and nerve cell sprouting
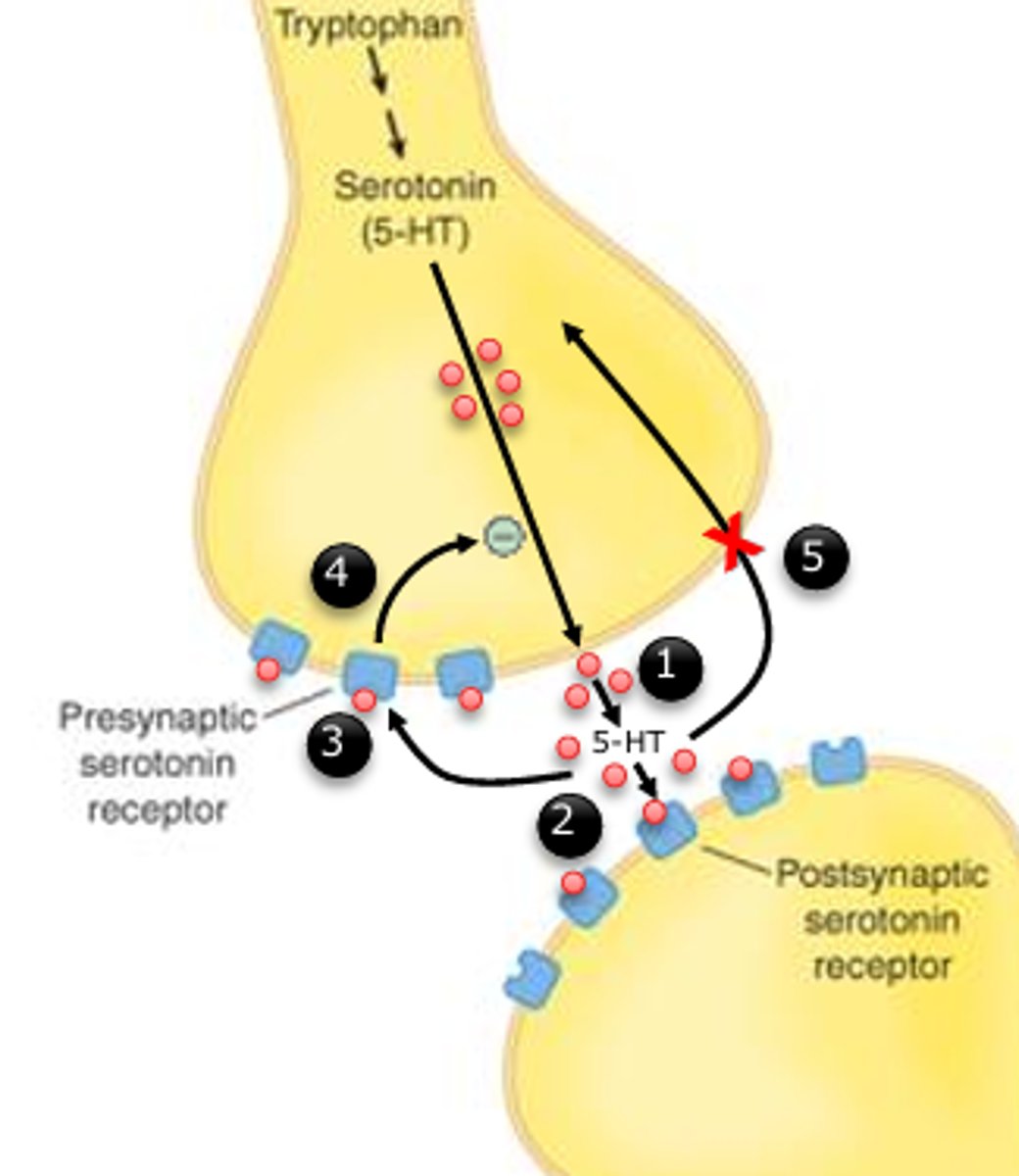
Selective Serotonin Reuptake Inhibitors (SSRIs)
1. 5-HT is released
2. 5-HT binds to its postsynaptic receptor
3. 5-HT binds to its presynaptic receptor 3
4. Step 3 results in less5-HT being released 4
5. If sertotonin uptake is blocked, more 5-HT will be available in the synaptic space
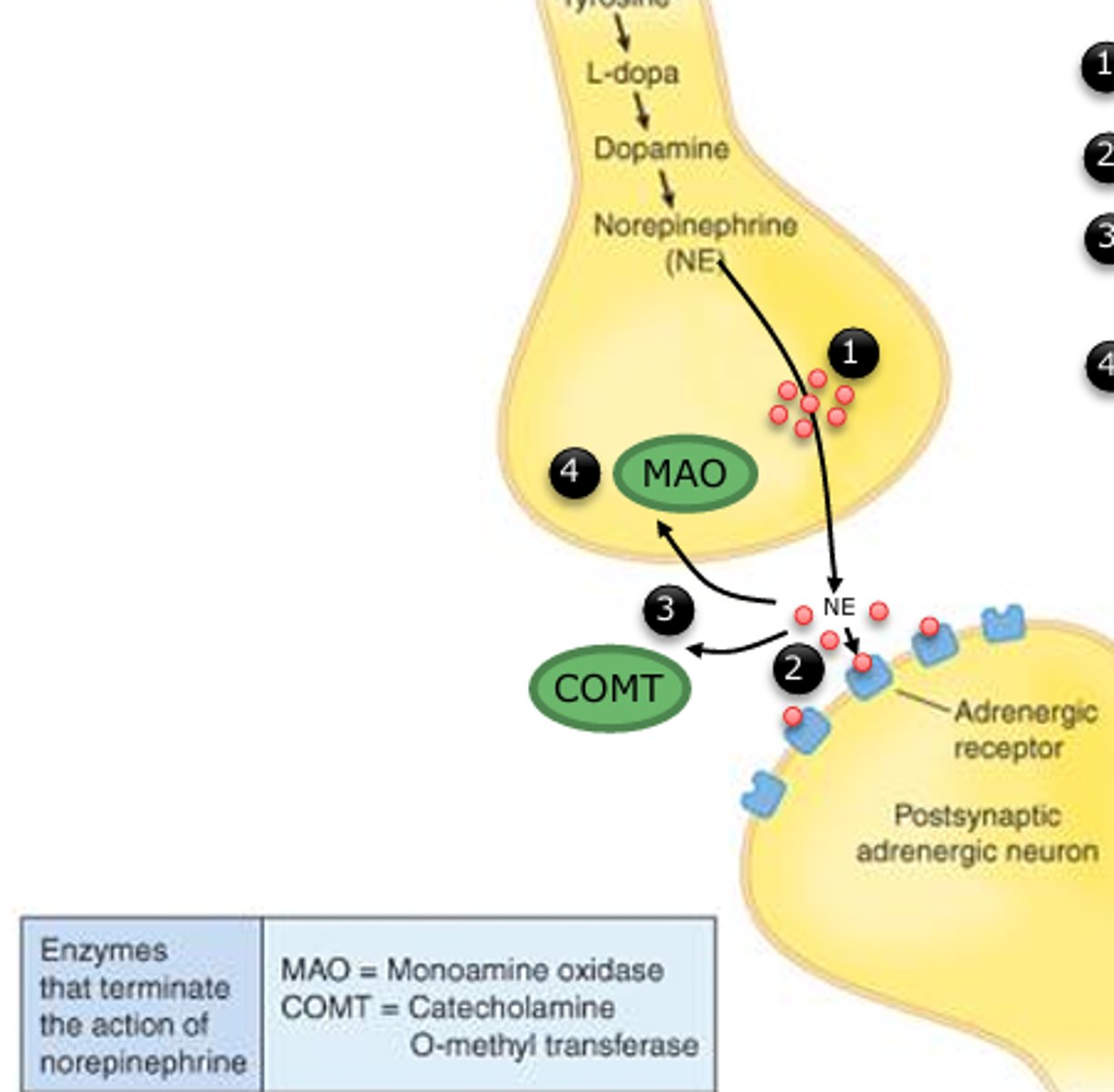
Monoamine Oxidase Inhibitors (MAOIs)
1. NE is released
2. NE binds with its receptor
3. The action of NE is terminated by MAO and COMT
4. If MAO is inhibited, NE is not broken down as quickly; thus NE action is prolonged
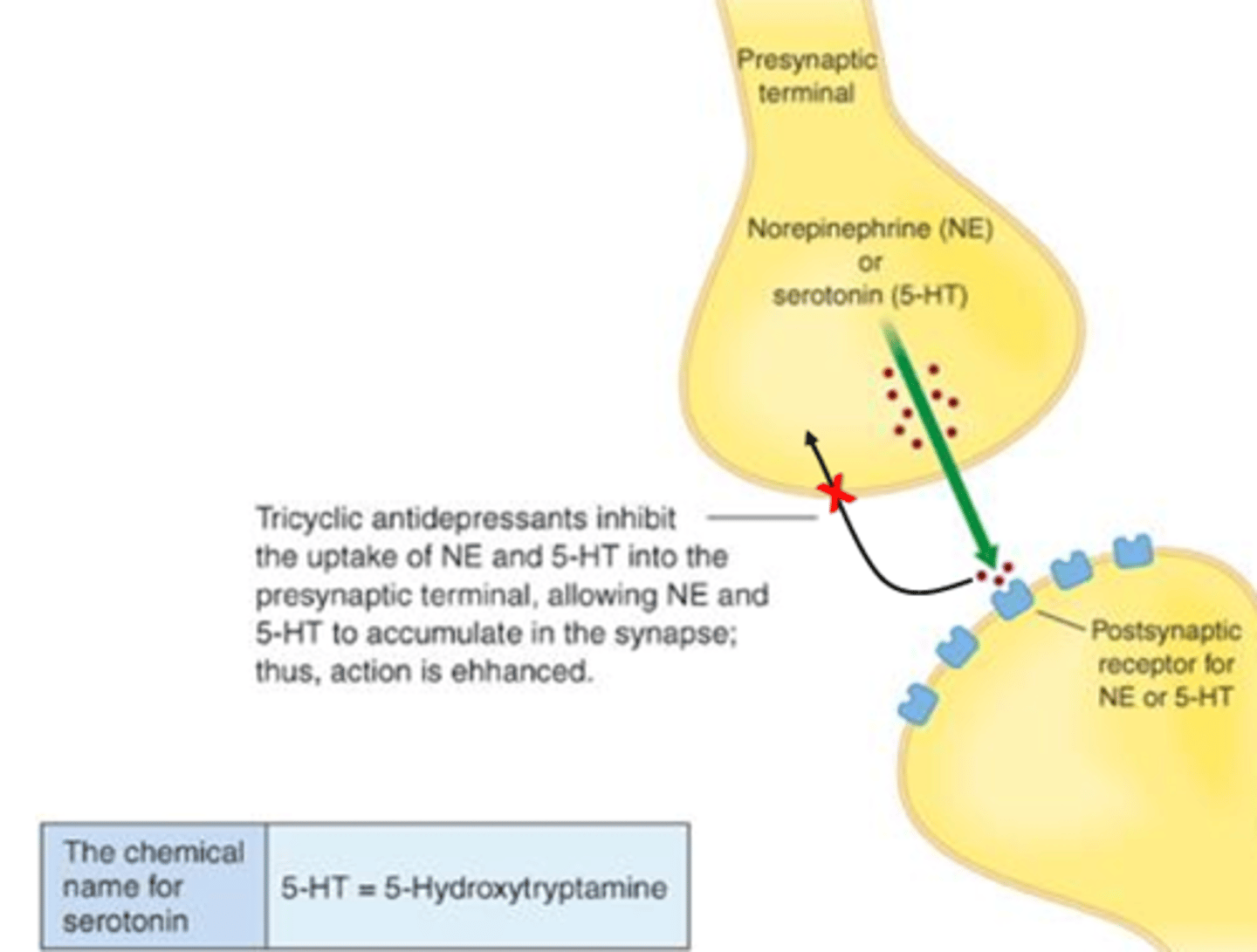
Tricyclic Antidepressants (TCAs)
Novel or Dual Antidepressants
- Serotonin-norepinephrine reuptake inhibitor (SNRI)
- Norepinephrine-dopamine reuptake inhibitor (NDRI)
*Block the reuptake of serotonin and norepinephrine
Monoamine Oxidase Inhibitors - Typical Antidepressants
Generic Drugs:
- Phenelzine
- Tranylcypromine
Mechanism of Action:
- Inhibit monoamine oxidase
Therapeutic Effect:
- Increased NE
- Increased serotonin
- Increased dopamine
Key Side Effects:
- Orthostatic hypotension (hypertensive crisis with tyramine), headache, insomnia, diarrhea
Serious Interactions:
- Tyramine, many OTC, and prescription drugs
Tricyclic Antidepressants - Typical Antidepressants
Generic Drugs:
- Imipramine
- Clomipramine
- Amitriptyline
- Desipramine
- Doxepin
- Trimipramine
Mechanism of Action:
- Inhibit NE, serotonin, and dopamine reuptake
Therapeutic Effect:
- Increased NE
- Increased serotonin
- Increased dopamine
Key Side Effects:
- Anticholinergic effects (sweating, sedation, orthostatic hypotension)
Serious Interactions:
- MAO inhibitors
Selective Serotonin Reuptake Inhibitors - Typical Antidepressants
Generic Drugs:
- Fluoxetine
- Sertraline
- Paroxetine
- Fluvoxamine
- Citalopram
Mechanism of Action:
- Inhibit serotonin reuptake
Therapeutic Effect:
- Increased serotonin
Key Side Effects:
- Nervousness, insomnia, sexual dysfunction, weight gain
Serious Interactions:
- MAO inhibitors
- Warfarin
Norepinephrine (NE) Reuptake Inhibitors - Atypical Antidepressants
Generic Drugs:
- Reboxetine
- Atomoxetine
Mechanism of Action:
- Inhibit NE reuptake
Therapeutic Effect:
- Increased NE
Key Side Effects:
- Dry mouth, hypotension, decreased libido, constipation, increased heart rate
Serious Interactions:
- MAO inhibitors
NE & Dopamine Reuptake Inhibitors - Atypical Antidepressants
Generic Drugs:
- Bupropion
Mechanism of Action:
- Inhibit NE and dopamine reuptake
Therapeutic Effect:
- Increased NE
- Increased dopamine
Key Side Effects:
- Increased appetite
Serious Interactions:
- MAO inhibitors
Serotonin & NE Reuptake Inhibitors
Generic Drugs:
- Venlafaxine
Mechanism of Action:
- Inhibit serotonin and NE reuptake
Therapeutic Effect:
- Increased NE
- Increased serotonin
Key Side Effects:
- Nausea, headache, nervousness, hypertension
Serious Interactions:
- MAO inhibitors
Non
Electroconvulsive Therapy (ECT) - Non-Pharmacological Treatment
- ETC is a procedure that electrically stimulates a generalized seizure and has a 70-90% effective treatment ratee for depression
- Given under a general anesthetic with complete muscle relaxation because the motor component of the seizure does not contribute to the therapeutic effects of the treatment
- A brief electrical current is passed through the brain to produce a generalized seizure lasting 25-150 seconds
- The patient doesn't feel the stimulus or recall the procedure
- On average 6-8 treatments are given at 2-day intervals over a period of 2-4 weeks
- After symptoms have improved, antidepressant medications are used to prevent relapse
- ETC produces an upregulation in serotonin: Occurs when there is a deficiency in the messenger; ETC increases the influx of calcium in the brain and has effects on second messenger systems
- ETC has been shown to up-regulate levels of BDNF
*Currently only indicated for patients whose depression is resistant to conventional treatments
First & Second Messengers of Depression
First:
- The neurotransmitters
Second:
- Involved in converting the chemical signal into a physiological one that moves the nerve impulse across the nerve cell and onto the next nerve cell
Non-Pharmacological Treatments
- Light therapy
- Vagal nerve stimulation
- Transcranial magnetic stimulation
- Psychotherapy: Cognitive behavioural therapy, mindfulness, psychodynamic, interpersonal
- Promote increased connectivity at the synapse and nerve cell growth
Light Therapy
- Uses artificial light to influence the production of melatonin and the function of the catecholamine systems
- Artificial light is believed to trigger a shift in the patient's circadian rhythm to an earlier time
- Exposure to this light source has produced improvement and relief of depressive symptoms for significant numbers of seasonally depressed individuals
Vagal Nerve & Transcranial Magnetic Stimulation
*Used for those that do not respond to medications or ECT
Vagal Nerve Stimulation:
- Involves using an implanted stimulator that sends electric impulses to the left vagus nerve in the neck via a lead wire implanted under the skin
- It is believed that VNS has antidepressant properties via its effects on the locus coeruleus, an area in the brain stem from which norepinephrine neurons originate
Deep Brain Stimulation:
- Involves the implantation of electrodes which are connected to a surgically implanted impulse generator that delivers electrical stimulation to the ventral striatum which has been found to have functional dysregulation in depression
- The ventral striatum is connectionally associated with the limbic system
Transcranial Magnetic Stimulation:
- Involves stimulation of the dorsolateral prefrontal cortex by using weak electric currents which are induced in the tissue by rapidly changing magnetic fields or electromagnetic induction
- In this way, brain activity can be triggered in the prefrontal cortex which has decreased volume and activity in depression
*Used under experimental investigation
Psychotherapy Focused
- Cognitive behavioural therapy (CBT) is psychotherapy focused on identifying, analyzing and ultimately changing the habitually inflexible and negative cognitions about oneself, others, and the world that occur with depression
- Aids in a more normal functioning of BDNF, neurotransmission, neuroendocrine abnormalities, and reduction and/or prevention of the neuroanatomical changes of depression
- The use of cognitive therapy in the acute phase of treatment may be considered first line treatment for mildly to moderately depressed outpatients
- Especially helpful for patients with a history of childhood adversity or recent stress
Psychotherapy Diagram