BOC Blood Bank — All Questions
1/381
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
382 Terms
b. 12.5 g/dL
All donors, regardless of sex, requires a minimum hemoglobin of 12.5 g/dL. The value must not be performed on an earlobe stick.
BLOOD PRODUCTS
1. The minimum hemoglobin concentration in a fingerstick from a male blood donor is:
a. 12.0 g/dL (120 g/L)
b. 12.5 g/dL (125 g/L)
c. 13.5 g/dL (135 g/L)
d. 15.0 g/dL (150 g/L)
c. history of jaundice of uncertain cause
Jaundice is a sign of liver impairment, which might be due to HBV or HCV. Infection with HBV and HCV is a cause for indefinite deferral.
2. A cause for permanent deferral of blood donation is:
a. diabetes
b. residence in an endemic malaria region
c. history of jaundice of uncertain cause
d. history of therapeutic rabies vaccine
c. 22 year old college students who has a temperature 99.2F and states that he feels well, but is nervous about donating.
The receipt of blood products is a 6-month deferral, the deferral for travel to areas endemic for malaria is 12 months regardless of antimalarial prophylaxis, and a person taking antibiotics may have bactermia. The requirement for temperature is not over 99.5F.
3. Which of the following prospective donors would be accepted for donation?
a. 32 year old woman who received a transfusion in a complicated delivery 5 months previously.
b. 19 year old sailor who has been stateside for 9 months and stopped taking his anti-malarial medication 9 months previously.
c. 22 year old college students who has a temperature 99.2F and states that he feels well, but is nervous about donating.
d. 45 year old woman who has just recovered from a bladder infection and is still taking antibiotics.
d. confirmed positive test for HBsAg 10 years previously.
A positive test for HbsAg at any time is an indefinite deferral.
4. Which one of the following constitutes permanent rejection status of a donor?
a. a tatoos 5 months previously
b. recent close contact with a patient with viral hepatitis
c. 2 units of blood transfused 4 months previously
d. confirmed positive test for HBsAg 10 years previously.
b. spontaneous abortion at 2 months of pregnancy, 3 months previously
A woman who had a spontaneous abortion at 2 months of pregnancy, 3 months previously would be acceptable. A donor is acceptable if she has not been pregnant in the previous 6 weeks.
5. According to AABB standards, which of the following donors may be accepted as a blood donor?
a. traveled to an area endemic for malaria 9 months previously.
b. spontaneous abortion at 2 months of pregnancy, 3 months previously
c. resides with a known hepatitis patient.
d. received a blood transfusion 22 week previously
b. 1
The Hct must be >38%. A donor may be 16 unless state law differs. Temperature must not exceed 99.5F, blood pressure must be <180 mm Hg systolic and <100 mm Hg diastolic, pulse 50-100 unless an athlete (which can be lower). Toxoids and vaccines from synthetic or killed sources have no deferral.
6. Below are the results of the history obtained from a prospective female blood donor:
Age: 16
Temperature: 99.0F
Hct: 36%
History: tetanus toxoid immunization 1 week previously
How many of the above results excludes this donor from giving blood for a routin transfusions?
a. none
b. 1
c. 2
d. 3
a. 150 x 10^3/uL (150 x 10^9/L)
The minimum platelet count required for frequent repeat donors is 150x10^3/uL. A platelet ount is not required prior to the first donation or if the interval between donations is at least 4 weeks.
7. For apheresis donors who donate platelets more frequently than every 4 weeks, a platelet count must be performed prior to the procedure and be at least:
a. 150 x 10^3/uL (150 x 10^9/L)
b. 200 x 10^3/uL (200 x 10^9/L)
c. 250 x 10^3/uL (250 x 10^9/L)
d. 300 x 10^3/uL (300 x 10^9/L)
a. hypochlorite
The minimum platelet count required for frequent repeat donors is 150x10^3/uL. A platelet count is not required prior to the first donation or if the interval between donations is at least 4 weeks.
8. Prior to blood donation, the intended venipucture site must be cleaned with a scrub solution containing:
a. hypochlorite
b. isopropyl alcohol
c. 10% acetone
d. PVP iodine complex
d. serological test for syphilis
Testing for syphilis was the first mandated donor screening test for infectious disease and is still part of donor screening.
9. All donor blood testing must include:
a. complete Rh phenotyping
b. anti-CMV testing
c. direct antiglobulin test
d. serological test for syphilis
b. cooled towards 20-24C
Platelets are prepared and stored at 20-24C for optimum function.
10. During the preaparation of platelet Concentrates from Whole Blood, the blood should be:
a. cooled towards 6C.
b. cooled towards 20-24C
c. warmed to 37C
d. heated to 57C
b. HBsAg
The most common ostransfusion hepatitis is hepatitis B. The estimated risk of transmission is 1:220,000 units transfused. The risk of hepatitis C transmission is 1:1,800,000 units. Hepatitis B surface antigen (HBsAg) is required donor test for detection of acute or chronic HBV infection.
11. The most common cause of posttransfusion hepatitis can be detected in donors by testing for:
a. anti-HCV
b. HBsAg
c. anti-HAV IgM
d. anti-Hbe
b. anti-HIV-1
Western blot uses purified HIV proteins to confirm reactivity in samples whose screening test for anti-HIV is positive.
12. The Western blot is a confimatory test for the presence of:
a. CMV antibody
b. anti-HIV-1
c. HBsAg
d. serum protein abnormalities
b. anti-HIV 1,2
The causative agent for AIDS is the human immunodeficiency virus types 1 and 2.
13. The test that is currently used to detect donors who are infected with the AIDS virus is:
a. anti-Hbc
b. anti-HIV 1,2
c. HBsAg
d. ALT
d. enzyme-labeled immunosorbent assay (ELISA)
The ELISA method is a very sensitive method employed to screen donors for markers of transfusion-transmitted viruses.
14. A commonly used screening method for anti-HIV-1 detection is:
a. latex agglutination
b. radioimmunoassay (RIA)
c. thin-layer-chromatography (TLC)
d. enzyme-labeled immunosorbent assay (ELISA)
c. restore 2,3-DPG and ATp to normal levels
Rejuvenation of RBCs uses additives to restore or enhance 2,3-DPG and ATP levels.
15. Rejuvenation of a unit of Red Blood Cells is a method used to:
a. remove antibody attached to RBC's
b. inactivate viruses and bacteria
c. restore 2,3-DPG and ATP to normal levels
d. filter blood clots and other debris
d. the original date of the unsplit unit
Sterile docking devices allow entry into donor units without affecting the expiration date of the product.
16. A unit of packed cells is split into 2 aliquots under closed sterile conditions at 8 AM. The expiration time for each aliquot is now:
a. 4 PM on the same day
b. 8 PM on the same day
c. 8 AM on the same day
d. the original date of the unsplit unit
d. 35 days
Sterile docking devices allow entry into donor units without affecting the expiration date of the product.
17. A unite of Red Blood Cells expiring in 35 days is split into 5 small aliquots using a sterile pediatric quad set and a sterile connecting device. Each aliquot must be labeled as expiring in:
a. 6 hours
b. 12 hours
c. 5 days
d. 35 days
c. every 4 hours
If storage devices do not have automated temperature recording, temperature must be manually monitored every 4 hours.
18. When platelets are stored on a rotator set on an open bench top, the ambient air temperature must be recorded:
a. once a day
b. twice a day
c. every 4 hours
d. every hour
b. Fresh Frozen Plasma, -20C
Fresh Frozen plasma is stored at -18C or below for 12 months.
19. Which of the following is the correct storage temperature for the component listed?
a. Cryopreciptated AHF, 4C
b. Fresh Frozen Plasma (FFP), -20C
c. Red Blood Cells, Frozen, -40C
d. Platelets, 37C
d. record the return and place the unit back into inventory.
Blood may be returned to the blood bank after issue provided that 1. the contianer has not been entered, 2. at least 1 sealed segment is attached to the contianer, 3. visual inspection of the unit is satisfacotry and documented, and 4. the unit has been maintained at the appropriate storage or transport temperature. Studies have shown that refrigerated components retain an acceptable temperature of <10C for up to 30 minutes after removal from the refrigerator.
20. A unit of Red Blood Cells is issued at 9:00 am. At 9:10 am the unit is returned to the Blood Bank. The container has NOT been entered, but the unit has NOT been refrigerated during the time span. The best course of action for the technologist is to:
a. culture the unit for bacterial contamination
b. discard the unit if not used within 24 hours
c. store the unit at room temperature
d. record the return and place the unit back into inventory
a. -80C
red blood cells, frozen with 40% glycerol are stored at -65C or lower.
21. The optimum storage temperature for Red Blood Cells, Frozen is:
a. -80C
b. -20C
c. -12C
d. 4C
d. 4C
Red Blood Cells are stored at 1-6C.
22. The optimum storage temperature for Red Blood Cells is:
a. -80C
b. -20C
c. -12C
d. 4C
b. 24
If the seal is broken during the processing, components are considered to be prepared in an open system, rather than a closed system. the expiration time for Red Blood Cells in an open system is 24 hours.
23. If the seal is entered on a unit of Red Blood Cells stored at 1C to 6C, what is the maximum allowable storage period, in hours?
a. 6
b. 24
c. 48
d. 72
a. -20C
Cryoprecipitated AHF is stored at -18C or lower.
24. The optimum storage temperature for cryoprecipitated AHF is:
a. -20C
b. -12C
c. 4C
d. 22C
a. 4 hours
Cryoprecipitate must be transfused within 4 hours of pooling.
25. Cryoprecipitated AHF must be transfused within what period of time following thawing and pooling?
a. 4 hours
b. 8 hours
c. 12 hours
d. 24 hours
d. 5 days
Whole Blood-derived platelets are stored at 20-24C with continuous gentle agitation. Platelets prepared by the PRP method may be stored for up to 5 days.
26. Platelets prepared in a polyolefin type contianer, stored at 22C-24C in 50 mL of plasma, and gently agitated can be used for up to:
a. 24 hours
b. 48 hours
c. 3 days
d. 5 days
d. 22C
the required temperature for storage of platelets is 20-24C.
27. The optimum storage temperature for platelets is:
a. -20C
b. -12C
c. 4C
d. 22C
a. 24 hours
Per AABB standards, thawed FFP should be stored at 1-6C for no more than 24 hours.
28. According to AABB standards, Fresh Frozen Plasma must be infused within what period of time following thawing?
a. 24 hours
b. 36 hours
c. 48 hours
d. 72 hours
c. 12 months
Cryopreciptate has a shelf life of 12 months in the frozen state.
29. Cryopreciptated AHF, if maintained in the frozen state at -18C or below, has a shelf life of:
a. 42 days
b. 6 months
c. 12 months
d. 36 months
d. 24 hours
Once thawed, FFP is stored at 1-6C for up to 24 hours.
30. Once thawed, Fresh Frozen Plasma must be transfused within:
a. 4 hours
b. 8 hours
c. 12 hours
d. 24 hours
b. plasma pH
The pH of platelets should be maintained at 6.2 or above throughout the storage period.
31. An important determinant of platelet viability following storage is:
a. plasma potassium concentration
b. plasma pH
c. prothrombin time
d. activated partial thromboplastin time
a. 1-6C
The required temperature for storage of thawed plasma is 1-6C.
32. In the liquid state, plasma must be stored at:
a. 1-6 C
b. 22C
c. 37C
d. 56C
c. Red Blood Cells
2,3-DPG declines during storage of red blood cells, causing a "shift to the left" in the oxygen dissociation curve and an impaired ability to deliver oxygen to the tissues.
33. During the storage, the concentration of 2,3-diphosphoglycerate (2,3-DPG) decreases in a unit of:
a. Platelets
b. Fresh Frozen Plasma
c. Red Blood Cells
d. Cryoprecipated AHF
a. is indicated for fibrinogen deficiencies
Cryoprecipitate is used primarily for fibrinogen replacement. It is stored at room temperature (20-24C) after thawing and must be infused within 6 hours. If pooled with other cyro units, it must be infused within 4 hours.
34. Cryoprecipitated AHF:
a. is indicated for fibrinogen deficiencies
b. should be stored at 4C prior to administration
c. will not transmit hepatitis B virus
d. is indicated for the treatment of hemophilia B.
c. a directed donation given by a mother to her son
Blood products from blood relatives containing viable lympocytes must be irradiated to inhibit the proliferation of T cells and subsequent GVHD.
35. Which apheresis platelets product should be irradiated?
a. autologous unit collected prior to surgery
b. random stock unit going to a patient with DIC
c. a directed donation given by a mother to her son
d. a directed donation given by an unrelated family friend.
b. lymphocytes
Irradiation inhibits proliferation of T lymphocytes.
36. Irradiation of a unit of Red Blood Cells is done to prevent the replication of donor:
a. granulocytes
b. lymphocytes
c. red cells
d. platelets
c. the entry ports from becoming contaminated with water
FFP thawed in the water bath should be protected so that entry ports are not contaminated with water. One can may use a plastic overwrap or keep ports above the water level.
37. Plastic bag overwraps are recommended when thawing units of FFP in 37C water baths because they prevent:
a. the FFP bag from cracking when it contacts the warm water
b. water from slowly dialyzing across the bag membrane
c. the entry ports from becoming contaminated with water
d. the label from peeling off as the water circulates in the bath
b. Fresh Frozen Plasma
Fresh Frozen Plasma (FFP) must be separated and frozen within 8 hours of Whole Blood collection.
38. Which of the following blood components must be prepared within 8 hours after phlebotomy?
a. Red Blood Cells
b. Fresh Frozen Plasma
c. Red Blood Cells, Frozen
d. Cryoprecipitated AHF
b. 80
Cryoprecipitate contains t least 80 units of AHF.
39. Cryopreciptated AHF contains how many units of Factor VIII?
a. 40
b. 80
c. 130
d. 250
b. Cryoprecipitated AHF
Cryoprecipitated AHF contains at elast 80 IU of Factor VIII concentrated in about 10 mL of plasma.
40. Which of the following blood components contains the most Factor VIII concentration relative to volume?
a. Single-Donor Plasma
b. Cryoprecipitated AHF
c. Fresh Frozen Plasma
d. Platelets
d. Cryoprecipitated AHF
Cryoprecipitate is indicated as a source of fibrogen for hypofibrinogenemia. It contains a minimum of 150 mg of fibrinogen concentrated in a small volume of plasma.
41. The most effective component to treat a patient with fibrinogen deficiency is:
a. Fresh Frozen Plasma
b. Platelets
c. Fresh Whole Blood
d. Cryoprecipitated AHF
b. Cryoprecipitated AHF
Cryoprecipitate is the fraction of plasma proteins that precipitate when FFP is slowly thawed at 1-6C.
42. A blood component prepared by thawing Fresh Frozen Plasma at refrigerator temperature and removing the fluid portion is:
a. Plasma Protein Fraction
b. Cryoprecipitated AHF
c. Factor IX Complex
d. FP24
d. quarantine for Gram Stain and culture
Clots in the unit may indicate contamination
43. Upon inspection, a unit of platelets is noted to have a visible clots, but otherwise appears normal. The technologist should:
a. issue without concern
b. filter to remove the clot
c. centrifuge to express off the clots
d. quarantine for Gram Stain and culture.
c. 3.0x10^11
Per AABB standards, at least 90% of platelet pheresis units sampled must contain at least 3.0x10^11 platelets.
44. According to AABB standards, at least 90% of all Apheresis Platelets units tested shall contain a minimum of how many platelets?
a. 5.5x10^10
b. 6.5x10^10
c. 3.0x10^11
d. 5.0x10^11
a. 5.5x10^10 platelets per unit in at least 90% of the units tested
Per AABB standards, at least 90% of the platelet units prepared from Whole Blood that are sampled must contain at least 5.5X10^10 platelets
45. According to AABB standards, Platelets prepared from Whole Blood shall have at least:
a. 5.5x10^10 platelets per unit in at least 90% of the units tested
b. 6.5x10^10 platelets per unit in 90% of the units tested
c. 7.5x10^10 platelets per unit 100% of the units tested
d. 8.5x10^10 platelets per unit in 95% of the units tested
a. light spin followed by a hard spin
Whole blood-derived Platelets are prepared by a light spin to separate the Red Blood Cells from the platelet-rich plasma (PRP), followed by a heavy spin of the PRP to concentrate the platelets.
46. Which of the following is proper procedure for preparation of Platelets from Whole Blood?
a. light spin followed by a hard spin
b. light spin followed by 2 hard spins
c. 2 light spins
d. hard spin followed by a light spin
b. 6.2
Per AABB standards, at least 90% of platelet units sampled must have a pH of at least 6.2 at the end of the allowable storage.
47. According to AABB standards, what is the minimum pH required for Platelets at the end of the storage period?
a. 6.0
b. 6.2
c. 6.8
d. 7.0
a. gently agitate if stored at room temperature
Per AABB standards, store Platelets at 20-24C with continuous agitation. Platelets must be serparated from whole blood units and maintained at temperature of at least 20C. The pH must be at least 6.2 at the end of the storage time.
48. According to AABB standards, Platelets must be:
a. gently agitate if stored at room temperature
b. separated within 12 hours of Whole blood collection
c. suspended in sufficient plasma to maintain a pH of 5.0 or lower
d. prepared only from Whole Blood units that have been stored at 4C for 6 hours.
b. 5.5x10^10 platelets
Whole blood-derived (random donor) platelets should contain at least 5.5x10^10 platelets, be stored with continuous agitation at 20-24C and have a pH of 6.2 or higher when tested at the end of the storage period.
49. A unit of Whole Blood-derived (random donor) Platelets should contain at least:
a. 1.0x10^10 platelets
b. 5.5X10^10 platelets
c. 5.5x10^11 platelets
d. 90% of the platelets from the original unit of Whole Blood
c. 3x10^10 platelets
Apheresis (single donor) Platelets should contain at least 3.0x10^11 platelets, be stored with continuous agitation at 20-24C, and have a pH of 6.2 or higher when tested at the end of the storage period.
50. Platelets prepared by apheresis should contain at least:
a. 1X10^10 platelets
b. 3X10^10 platelets
c. 3x10^10 platelets
d. 5x10^11 platelets
d. transfuse through a Log^3 leukocyte-removing filter
Newly diagnosed bone marrow candidates are at great risk for severe sequelae of CMV infections. Infection can best be reduced by using leukocyte-reduction filters. CMV-seronegative units are rarely used since leukocyte reducing via filtration is so effective. Washing does not remove as many leukocytes as filtering.
51. Leukocyte-Reduced Red Blood Cells are ordered for a newly diagnosed bone marrow candidate. What is the best way to prepare this product?
a. crossmatch only CMV-seronegative units
b. irradiate the unit with 1,500 rads
c. wash the unit with saline prior to infusion
d. transfuse through a Log^3 leukocyte-removing filter
d. Leukocyte-reduced red blood cells
Leukoreduction of blood products reduce donor leukocytes to less than 5x10^6 and decreases the risk of HLA alloimmunization.
52. Of the following blood components, which one should be used to prevent HLA alloimmunizatoin of the recipient?
a. Red Blood Cells
b. Granulocytes
c. irradiated Red Blood Cells
d. Leukocyte-reduced red blood cells
a. apheresis
The apheresis process is to remove whole blood, the desired component removed, and the remaining portion of blood returned to the donor/patient.
53. A father donating Platelets for his son is connected to a continuous flow machine, which uses the principle of centrifugation to separate platelets from Whole Blood. As the Platelets are harvested, all other remaining elements are returned to the donor. This method of Platelet collection is known as:
a. apheresis
b. autologous
c. homologous
d. fractionation
b. 11 g/dL (110 g/L)
Autologous donors have less stringent criteria than allogeneic donors. Donations must be collected at least 72 hours prior to surgery.
54. To qualify as a donor for autologous transfusion a patient's hemoglobin should be at least:
a. 8 g/dL (80 g/L)
b. 11 g/dL (110 g/L)
c. 13 g/dL (130 g/L)
d. 15 g/dL (150 g/L)
a. ABO and Rh typically
Only ABo and Rh is required with the patient's sample. Each autologous unit must be confirmed ABO and Rh from an integrally attached segment.
55. What is/are the minimum pretransfusion testing requirement(s) for autologous donations collected and tranfused by the same facility?
a. ABO and Rh typically
b. ABO/Rh type, antibody screen
c. ABO/Rh type, antibody screen, crossmatch
d. no pretransfusion testing is required for autologous donations.
c. 80
FDA requires that 4 representative units be tested each month for Factor VIII levels of 80 IU or higher. If the average value is less than 80 IU of Factor VIII, corrective action must be taken.
56. In a quality assurance program, Cryoprecipitated AHF must contain a minimum of how many international units of Factor VIII?
a. 60
b. 70
c. 80
d. 90
d. 81
To determine the total IU of Factor VIII per bag of cryoprecipitate, multiple the assayed value/mL by the number of mL in the container.
Bonus? An assay of plasma from a bag of Cryoprecipitated AHF yields a concentration of 9 international units (IU) of Factor VIII per mL of Cryoprecipitated AHF. If the volume is 9 mL, what is the Factor VIII content of the bag in IU?
a. 9
b. 18
c. 27
d. 81
b. anti-P1
BLOOD GROUP SYSTEMS
57. Which of the following antibodies is usually clinically significant?
a. anti-P
b. anti-P1
c. anti-Pk
d. anti-p
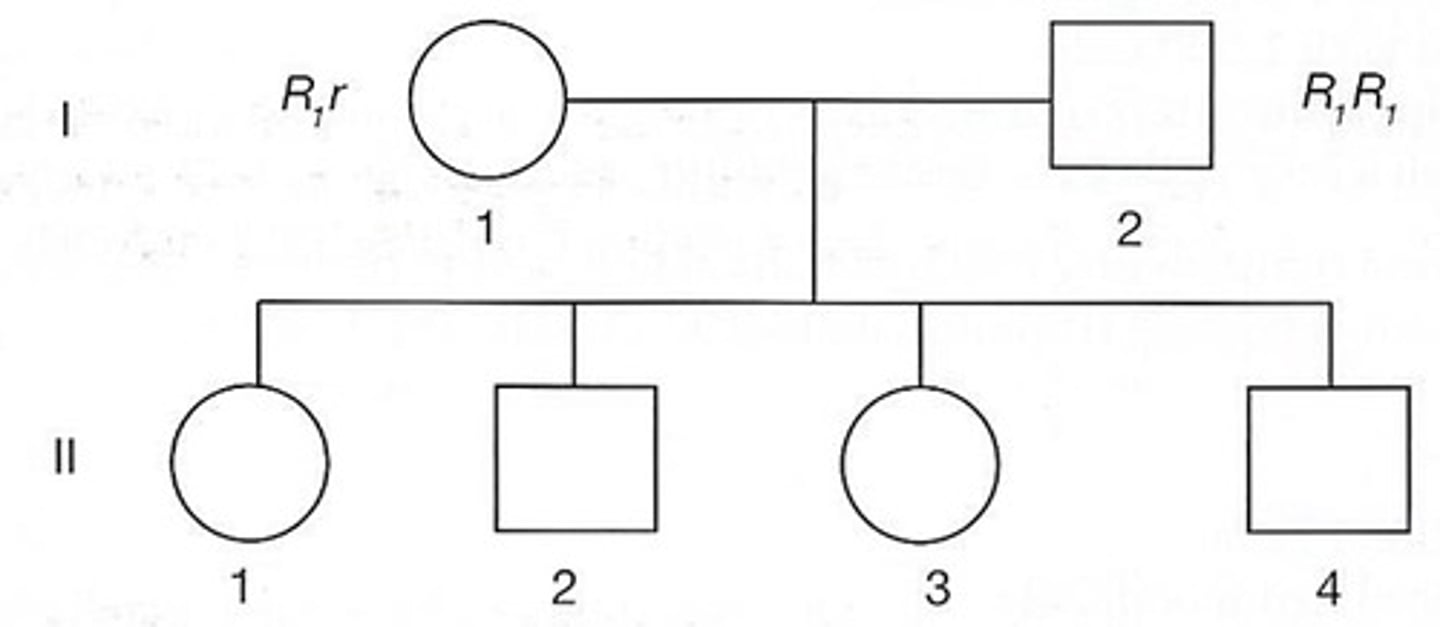
b. 50% will be R1r, and 50% will be R1R1
The mother has a 50% chance of passing on R1 and 50% chance of passing on r. The father will always pass on R1. Statistically, 50% of the children will be R1r and 50% of them will be R1R1.
58. Refer to the following diagram:
Given the most probable genotypes of the parents, which of the following statements best describes the most probable Rh genotypes of the 4 children?
a. 25% will be R0r1, 25% will be R1r, and 50% will be R1R1
b. 50% will be R1r, and 50% will be R1R1
c. 100% will be R1r
d. 100% will be R1r1
d. haplotype
The entire set of HLA antigens located on one chromosome is a haplotype.
59. The linked HLA genes on each chromosome constitute a(n):
a. allele
b. trait
c. phenotype
d. haplotype
d. DCe/dce
The patient lacks E. Since C and c are alleles, C is inherited from one parent and c from the other. Since the person is homozygous for e, one of the genes needs to code for ce (RHce) and the otehr Ce (RHCe). The RHD gene is more likely inherited with genotype is DCe/dce. This genotype is found in 31% of the white and 15% of the black populations.
60. An individual's red blood cells give the following reactions with Rh antisera:
Anti-D 4+
anti-C 3+
anti-E 0
anti-c 3+
anti-e 3+
Rh Control 0
The individual's most probable genotype is:
a. DCe/DcE
b. DcE/dce
c. Dce/dce
d. DCe/dce
c. O
The A and B structures can not be developed since there is no H precursor substance due to the lack of the H gene in the blood donor.
61. A blood donor has the genotype: hh, AB. Using anti-A and anti-B antisera, the donor's red cells will type as group:
a. A
b. B
c. O
d. AB
a. KK
This individual cannot have the k antigen on their cells. K0K0 is rare and no Kell system antigens are detected on the red blood cells. Those individuals usually produce antibodies that are reactive with all normal cells. KK is the most probable genotype.
62. An individual has been sensitized to the k antigen and has produced anti-k. What is the most probable Kell system genotype?
a. KK
b. Kk
c. kk
d. K0K0
a. African American
Fy(a-b-) individuals are very rare with all populations otehr than the individual of African descent. 68% of African Americans are Fy(a-b-).
the Fy[a-b-] phenotype occurs in 68% of the population of African descent, but is extremely rare in the other ethnic backgrounds. Lu[a-b-], Jk[a-b-] and K-k- are very rare in all ethnic backgrounds.
Bonus?: Given the following typing results, what is this donor's likely racial ethnicity?
Le(a-b-); Fy(a-b-); Js(a+b+)
a. African American
b. Asian American
c. Native American
d. Caucasian
c. Fy(a-b-)
the Fy[a-b-] phenotype occurs in 68% of the population of African descent, but is extremely rare in the other ethnic backgrounds. Lu[a-b-], Jk[a-b-] and K-k- are very rare in all ethnic backgrounds.
63. Anti-Fy3 will fail to react with which of the following enzyme treated red cells?
a. Fy(a+b-)
b. Fy(a-b+)
c. Fy(a-b-)
d. Fy(a+b+)
a. r'r'
The baby is Rh-negative and lacks c, since there is no evidence of HDFN. Inheritance of no D and no c is denoted as r'. The baby must have inherited this gene from both parents, and is homozygous r'r'.
64. A mother has the red cell phenotype D+C+E-c-e+ with ant-c (titer of 32 at AHG) in her serum. The father has the phenotype D+C+E-c+e+. the baby is Rh-negative and not affected with hemolytic disease of the newborn. What is the baby's most probable Rh genotype?
a. r'r'
b. r'r
c. R1R1
d. R1r
a. anti-c
The most common genotype in Rh-negative individuals is rr. Anti-e would not be formed because the recipient's red cells contain the e antigen. The first antibody most likely to develop would be anti-c.
65. In an emergency situation, Rh-negative red cells are transfused into an Rh-postive person of the genotype CDe/CDe. The first antibody MOST likely to develop is:
a. anti-c
b. anti-d
c. anti-e
d. anti-E
d. autosomal codominant
Blood group genes are autosomal; they are not carried on the sex gene. Whenever the gene is inherited, the antigen is expressed on the red blood cells, which is known as codominant.
66. Most blood group systems are inherited as:
a. sex-linked dominant
b. sex-linked recessive
c. autosomal recessive
d. autosomal codominant
c. Xg(a-) sons and Xg(a+) daughters
The Xg blood group is unique in that the genes encodes on the X chromosome. A negative mother would not have the Xg(a) to pass on. A positive father would, however, transmit the Xg(a) to all his daughters.
67. The mating of an Xg(a+) man and an Xg(a-) woman will ONLY produce:
a. Xg(a-) sons and Xg(a-) daughters.
b. Xg(a+) sons and Xg(a+) daughters.
c. Xg(a-) sons and Xg(a+) daughters.
d. Xg(a+) sons and Xg(a-) daughters.
d. R1R2
All common Rh antigens are present on the red blood cells. R1 (DCe) and R2 (DcE) are frequent genotypes.
68. Refer to the following data:
anti-C: +
anti-D: +
anti-E: +
anti-c: +
anti-e: +
Given the reactions above, which is the most probable genotype?
a. R1R1
b. R1r'
c. R0r"
d. R1R2
a. R0R0
R0R0 is the only correct choice here. R0 = D+C-E-c+e+.
69. A patient's red cells type as follows:
anti-D: 4+
anti-C: 0
anti-E: 0
Which of the following genotype would be consistent with these results?
a. R0R0
b. R1r
c. R1R2
d. Rzr
c. Le(a+b-)
The Lewis antigens are developed by gene interaction. Both the Lewis and Secretor gene are required for red cells to type as Le(a-b+). If a person has a Lewis gene, but not Secretor gene, then the cells type as Le(a+b-). The Le(a-b-) phenotype is derived when the Lewis gene is abesent and the Secretor gene may or may not be present. The Le(a+b-) pehnotyp eoccurs in 22% of the population, and Le(a-b-) occurs in 6%, so the most likely phenotype of a nonsecretor (se/se) is Le(a+b-).
70. The red cells of a nonsecretor (se/se) will most likely type as:
a. Le(a-b-)
b. Le(a+b+)
c. Le(a+b-)
d. Le(a-b+)
a. rr
Anti-f will react with cells that carry c and e on the same Rh polypeptide. No other listed genotypes produce an Rh polypeptide.
71. Which of the following phenotypes will react with anti-f?
a. rr
b. R1R1
c. R2R2
d. R1R2
a. R1R2
Non reactivity with anti-f indicates the cells do not have an Rh polypeptide that possesses both c and e, which is necessary to type as f+. R1R2 is the most likely genotype.
72. A patient's red blood cells gave the following reactions:
Anti-D: +
Anti-C: +
anti-E: +
anti-c: +
anti-e: +
anti-f: 0
The most probable genotype of this patient is:
a. R1R2
b. R2r"
c. Rzr
d. RzRz
d. 9
About 90% of people LACK the K antigen, thus capable of producing Anti-K. 9/10 units would be K-antigen-negative.
73. Anti-K is identified in a patient's serum. If random crossmatches are performed on 10 donor units, approximately how many would be expected to be compatible?
a. 1
b. 3
c. 7
d. 9
b. 3
The N antigen is lacking in 30% of the Caucasian population.
Bonus?: Anti-N is identified in a patient's serum. If random crossmatches are performed on 10 donor units, how many would be expected to be compatible?
a. 0
b. 3
c. 7
d. 10
c. R1r
The baby appears to lack c since no HDFN was evident. The mom is most likely R1R1, so had to pass R1 onto the baby. The father must have passed on an Rh gene that also did not produce c. Given the choices, the father has to be R1r.
74. A woman types as Rh-positive. She has an anti-c titer of 32 at AHG. Her baby has a negative DAT and is not affected by hemolytic disease of the newborn. What is the father's most likely Rh phenotype?
a. rr
b. r"r
c. R1r
d. R2r
c. Fy(a-b-)
The Fy(a-b-) phenotype occurs in 60% of the population of African descent, but is extremely rare in the other ethinc backgrounds. Lu(a-b-), Jk(a-b-) and K-k- are very rare in all ethnic backgrounds.
75. Which of the following red cell types are most commonly found in the African American donor population?
a. Lu(a-b-)
b. Jk(a-b-)
c. Fy(a-b-)
d. K-k-
d. rare donor registry
The frequency of compatible donors for this patient can be calculated by multiplying the percentage of the population that is e-C x Fy(a-) x Jk(b-). The blood supplier's immunohematology reference laboratory may have units in stock or can request blood from other IRLs through the American Rare Donor Program.
76. Four units of blood are needed for elective surgery. The patient's serum contains anti-C, anti-e, anti-Fy^a, and anti-Jk^b. Which of the following would be the best source of donor blood?
a. test all units in current stock
b. test 100 group O, Rh-negative donors
c. test 100 group-compatible donors
d. rare donor registry
b. R1r
The most likely haplotype is DCe/dce.
77. A donor is teaed with Rh antisera with the following results:
anti-D: +
anti-C: +
anti-E: 0
anti-c: +
anti-e: +
Rh control: 0
What is his most probable Rh genotype?
a. R1R1
b. R1r
c. R0r
d. R2r
d. B35
From the frist 2 children it can be determined the mom has the haplotypes A2b12 and A23F18. The dad has the haplotype A1B3 and A3B35. The expected B antigen in child 3 is B35.
78. A family has been typed for HLA because 1 of the children needs a stem cell donor. Typing results are listed below:
father: A1,3;B8,35
mother: A2,23;B12,18
child 1: A1,2;B8,12
child 2: A1,23;B8,18
child 3: A3,23;B18,?
What is the expected B antigen in child 3?
a. A1
b. A2
c. B12
d. B35
b. N-Acetylgalactosamine
79. Which of the following is the immunodominant sugar responsible for the A antigen?
a. fucose
b. N-Acetylgalactosamine
c. galactose
d. N-Acetylglucosamine
c. 3.0
If an exact match of HLA-A and HLA-B antigens is necessary, siblings would be the most likely match, since siblings may have received the same haplotype from the parents.
80. A patient is group O, Rh-negative with anti-D and anti-K in her serum. What percentage of the general Caucasian donor population would be compatible with this patient?
a. 0.5
b. 2.0
c. 3.0
d. 6.0
c. 0.55
Use the Hardy-Weinberg equation: p^2+2pq+q^2=1.0. In this example, p^2 is the homozygous population, Jk(a+b-). The square root of p^2=p, which is the gene frequency of Jk^a in this population. OUt of 400 people, 122, or 30% are homozygous. The square root of 0.30= is 0.55.
81. The observed phenotypes in a particular population are:
Jk(a+b-) = 122 persons
Jk(a+b+) = 194 persons
Jk(a-b+) = 84 persons
What is the gene frequency of Jk in this population?
a. 0.31
b. 0.45
c. 0.55
d. 0.60
b. 48%
The Hardy-Weinberg equation states (p+q)^2=1.0. When the equation is expanded, it is p^2+2pq+q^2=1.0.
82. In a random population, 16% of the people are Rh-negative (rr). What percentage of the Rh-positive population is heterozygous for r.
a. 36%
b. 48%
c. 57%
d. 66%
a. Vel
83. Which of the following is considered to be a high prevalence antigen?
a. Vel
b. Js^a
c. s
d. K
d. H antigen is left unchanged by the absence of A and/or B transferase enzymes
84. The reason that group O individuals have the most amount of H antigen on their red cells compared to other ABO phenotypes is:
a. Group O individuals produce more precursor type I chain
b. Group A, B and AB individuals are heterozygous for the H gene
c. The O gene produces more transferase enzyme which produces more H antigen
d. H antigen is left unchanged by the absence of A and/or B transferase enzymes
d. Jk(a-b-)
85. Which phenotype could not result from the mating of a Jk(a+b+) female and a Jk(a-b+) male?
a. Jk(a+b-)
b. Jk(a+b+)
c. Jk(a-b+)
d. Jk(a-b-)
d. present in the child, but absent in the mother and alleged father.
When a marker is in a child that the mother and alleged father do not have, the alleged father can not be the biological father of the child. this is a direct exclusion.
Bonus?: In relationship testing, a "direct exclusion" is established when a genetic marker is:
a. absent in the child, but present in the mother and alleged father.
b. absent in the child, present in the mother and absent in the alleged father.
c. present in the child, absent in the mother and present in the alleged father.
d. present in the child, but absent in the mother and alleged father.
c. paternity may be excluded on the basis of ABo typing
The child's genotype does not included E. The alleged father is homozygous for E. If he was the father the child woudl also have E. The father can be excluded from paternity.
Bonus?: Relationship testing produces the following red cell phenotyping results:
ABO / Rh
alleged father: B / D+C-c+E+e-
mother: O / D+C+E-c-e+
child: O / D+C+E-c+e+
What conclusion may be made?
a. there is no exclusion of paternity.
b. paternity may be excluded on the basis of ABO typing.
c. paternity may be excluded on the basis of Rh typing
d. paternity may be excluded on the basis of both ABO and Rh typing.
b. direct
Direct exclusion of paternity is established when a genetic marker is present in the child but is absent from the mother and the alleged father.
Bonus?: In a relationship testing case, the child has a genetic marker that is absent in the mother and cannot be demonstrated in the alleged father. What type of paternity exclusion is this known as?
a. indirect
b. direct
c. prior probability
d. Hardy-Weinberg.
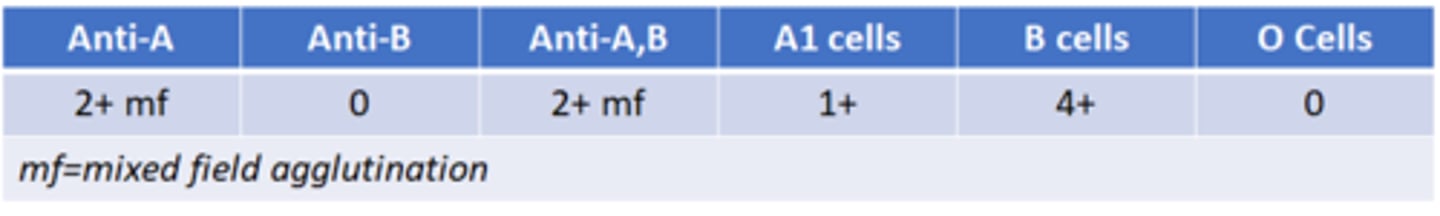
c. Ax; with an anti-A1
Ax cells are more strongly reactive with anti-A, B than with anti-A and the plasma frequently has anti-A1 present.
86. A patient is typed with the following results:
[Image]
The most probable reason for these finding is that the patient is group:
a. O, confusion due to faulty group O antiserum.
b. O; with an anti-A1
c. Ax; with an anti-A1
d. A1; with an anti-A
![<p>86. A patient is typed with the following results:</p><p>[Image]</p><p>The most probable reason for these finding is that the patient is group:</p><p>a. O, confusion due to faulty group O antiserum.</p><p>b. O; with an anti-A1</p><p>c. Ax; with an anti-A1</p><p>d. A1; with an anti-A</p>](https://knowt-user-attachments.s3.amazonaws.com/1c4a558c-c25e-47cd-98ac-151c5e108889.jpg)
c. Fy(a-b+)
87. Which of the following phenotypes is the results of homozygous inheritance of the corresponding genes?
a. Le(a+b-)
b. M+N+
c. Fy(a-b+)
d. Jk(a+b+)
c. A3
88. Given the following serologic reactions, what is the most likely A subgroup?
a. A1
b. A2
c. A3
d. Ax
c. give a mixed-field reaction with anti-A,B
Mixed-field reactivity with anti-A and anti-A,B is a typical finding for A3 subgroups.
Bonus?: Cells of the A3 subgroup will:
a. react with Dolichos biflorus
b. bE- with anti-A
c. give a mixed-field reaction with anti-A,B
d. bE-with anti-H
c. L-fucoysl transferase
Fucose is the immunodominant sugar for H.
89. The enzyme responsible for conferring H activity on the red cell membrane is alpha-:
a. galactosyl transferase
b. N-acetylgalactoaminyl transferase
c. L-fucosyl transferase
d. N-acetyglucosaminyl transferase
d. anti-H
Bombay phenotypes (Oh) lack H antigen on their red cells, and produce naturally occurring anti-H in their serum.
90. Even in the absence of prior transfusion or pregnancy, individuals with the Bombay phenotype (Oh) will always have naturally occurring:
a. anti-Rh
b. anti-K0
c. anti-U
d. anti-H
a. anti-Lu^a
Most examples of anti-Lu^a agglutinate saline suspended cells. Most examples of anti-Lu^b are IgG and reacts at 37C. Anti-Lu3 usually reacts at the AHG phase as does anti-Lu^ab.
91. Which of the following antibodies in the Lutheran system is most likely to be IgM and detected as a direct agglutinin?
a. anti-Lu^a
b. anti-Lu^b
c. anti-Lu3
d. anti-Lu^ab
b. anti-Ch
Anti-Ch and anti-Rg react at IAT with trace amounts of C4 (a component of complement) present on normal RBCs. The Ch and Rg substance is found soluble in plasma. neutralization studies with pooled plasma can help confirm the antibody reactvity in a patient's sample. if test procedures are used to coat cells with C4, a patient with anti-Ch or anti-Rg may agglutinate the cells directly.
92. Which of the following antibodies is neutralizable by pooled human plasma?
a. anti-Kn^a
b. anti-Ch
c. anti-Yk^a
d. anti-Cs^a
d. Kidd
93. Antibodies from which of the following blood group systems are notorious for causing delayed hemolytic transfusion reactions?
a. Rh
b. Kell
c. Duffy
d. Kidd