Physiology Final Cumulative Objectives
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
Describe the fluid compartments of the body and know their relative sizes in comparison to one another
Intracellular fluid > Interstitial fluid > Plasma
Define homeostasis and describe the meaning of “dynamic equilibrium”
Homeostasis - a “dynamic equilibrium” where levels change over short periods of time, but remain relatively constant over long periods of time near the “set point”
Know the components of a homeostatic reflex arc
Afferent pathway - carry receptor info to control center
Efferent pathway - carry command from control center to effector
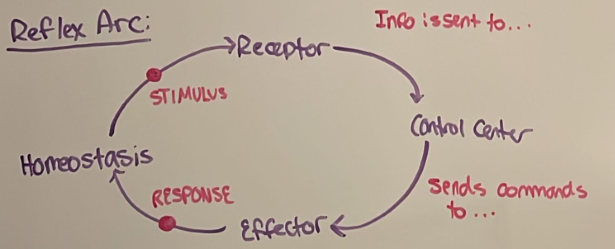
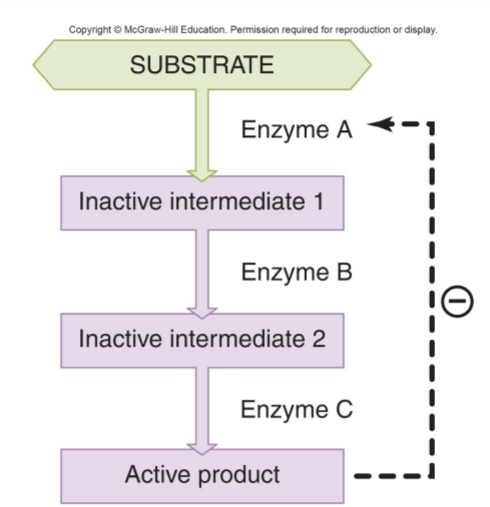
How do negative feedback loops preserve homeostasis?
Production of a substance inhibits further production of that substance » return fluctuations in levels to their set point
Define active transport, secondary active transport, and facilitated diffusion. Think of some examples in specific body systems.
Facilitated diffusion - uses a permeable barrier where flow is down a concentration gradient (ex. sodium flows out of the descending limb)
Active transport - uses energy to transport against a concentration gradient (ex. Na+/K+ pump)
Secondary active transport - uses energy from a pre-existing gradient of a different solute to transport against the gradient
Know the three membrane junctions and their functions
Gap junctions - allow ions and other molecules to pass
Tight junctions - form a barrier
Desmosomes - strong attachment
Describe how size and solubility determine whether a substance can cross a membrane by diffusing through the lipid bilayer, or whether it needs to pass through a transport protein
Pass by diffusion » small and nonpolar molecules
Pass by transport protein » ions and water-soluble, larger molecules
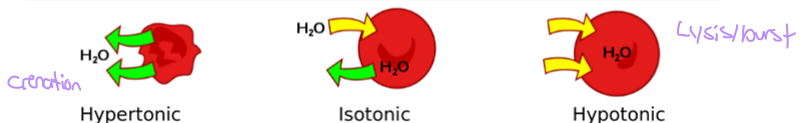
Define hyper-, hypo-, and isotonic. Explain how these solutions affect the movement of water across membranes and describe the effect on cell size
Hypertonic - water moves out of cell » crenation/shrivel
Isotonic - water moves in and out of cell » no change
Hypotonic - water moves into cell » lysis/burst
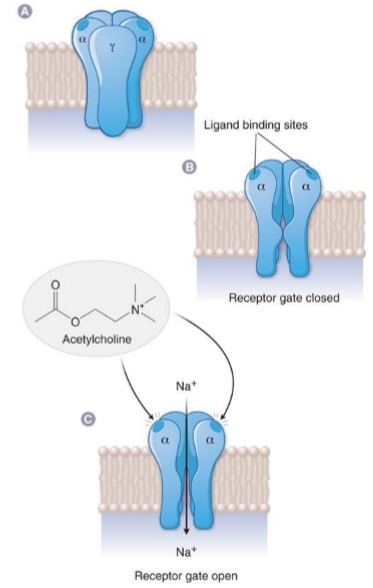
Describe the ligand gated ion channel and how it transduces signals in the cell
agonist binds and opens channel
changes membrane potential
+ ions IN » depolarize cell
- ions IN » hyperpolarize cell
+ ions OUT » hyperpolarize cell
Ex. nicotinic ACh receptor
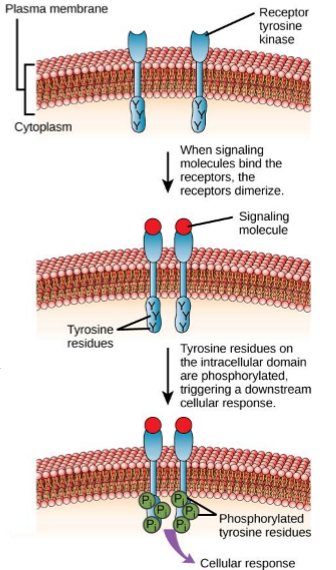
Describe the enzyme linked receptor and how it transduces signals in the cell
receptor that has enzyme activity and phosphorylates target proteins in the cell (kinases)
Ex. Insulin receptor
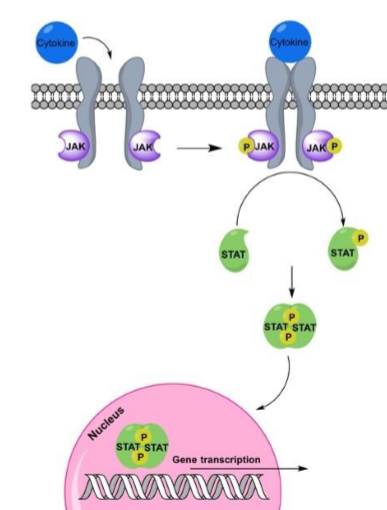
Describe the JAK/STAT receptor and how it transduces signals in the cell
receptor activates janus kinase (JAK) that phosphorylates proteins (STAT)
STAT proteins often travel to nucleus as transcription factors
Ex. cytokine receptors
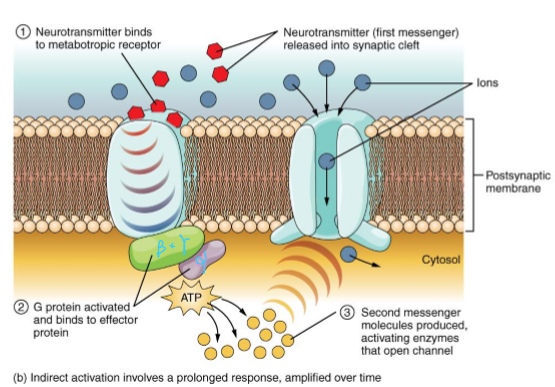
Describe the GCPR and how it transduces signals in the cell
G protein located on membrane surface with 3 subunits
Alpha subunit binds GTP and dissociates from beta/gamma subunit
Alpha subunit activates second messenger molecules
Gs - stimulate adenylyl cyclase » more cAMP
Gi - inhibits adenylyl cyclase » less cAMP
Gq - activates phospholipase C » increase IP3, DAG, and Ca2+
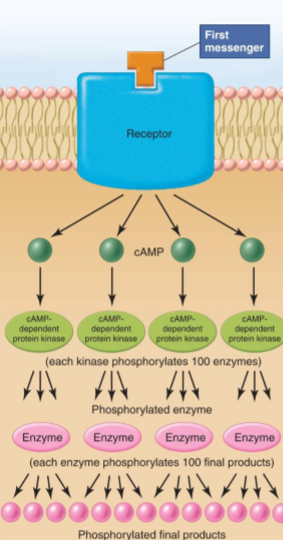
Describe how second messengers like cAMP lead to signal amplification
A first messenger activates a second messenger like cAMP that creates a signal cascade by phosphorylating 100s of enzymes, which then phosphorylate 100s more enzymes » signal amplification
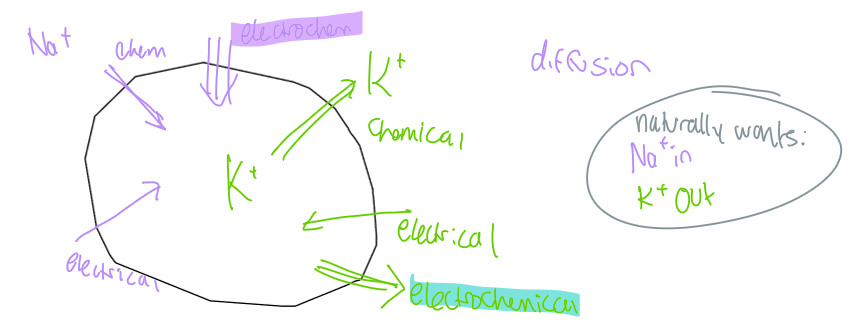
How is resting membrane potential maintained?
Na+ is higher concentration outside of cell » Na+ wants to flow in
K+ is higher concentration inside of cell » K+ wants to flow out
maintained by an electrochemical gradient of both ions
explain how an action potential is generated and how voltage gated Na+ and K+ channels are involved
At rest » Na+ and K+ closed
Stimulus » Na+ open and flows into cell
Peak depolarization » Na+ channel deactivates, K+ open and flows out of cell
Voltage falls to hyperpolarization » K+ close, Na+ are resting closed
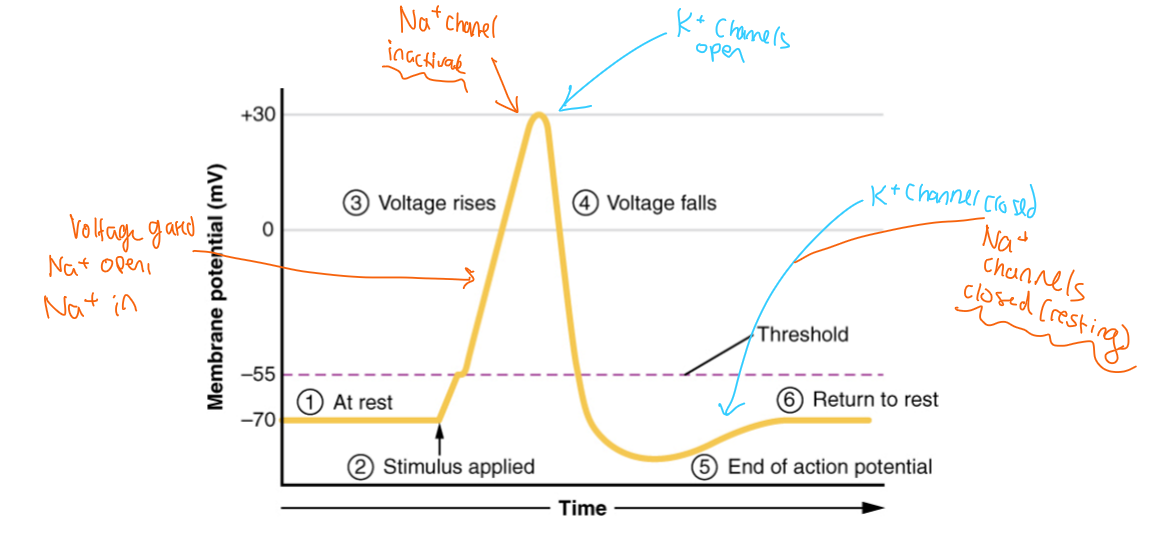
Describe absolute and relative refractory periods
Absolute - cell is incapable of depolarizing
Relative - cell can depolarize if supplied with a stronger than usual stimulus
helps maintain signals as individuals
Describe how action potentials propagate and how propagation is affected by axon diameter and myelination
Larger diameter and thicker myelination » faster propagation
Resting membrane is depolarized to threshold by local current of AP
Once AP propagates down axon, membrane behind AP is refractory and cannot stimulate a second AP
What is the link between Ca2+ and neurotransmitter release?
AP triggers Ca2+ channels to open and flow into axon terminal » Ca2+ in terminal facilitates vesicles fusing into cleft and release NT into synaptic cleft
Define EPSP and IPSP and how they’re different from AP
Excitatory Postsynaptic Potentials (EPSP) - depolarize membrane towards threshold
Inhibitory Postsynaptic Potentials (IPSP) - hyperpolarize membrane away from threshold
can summate into an AP or away from an AP
What are the neurotransmitters and receptors involved in signaling for the sympathetic nervous system?
NE and Epi » Alpha and Beta andregenic receptors
What are the neurotransmitters and receptors involved in signaling for the parasympathetic nervous system?
ACh » Muscarinic receptors
Define the concept of autonomic tone
One division is dominant (SNS or PSNS)
Ex. heart rate has PSNS tone, so resting heart rate is 70 bpm rather than 100 bpm
Define receptor potential and describe how receptor potentials can lead to the generation of an AP in a sensory neuron
Local changes in potential in response to stimuli (stronger stimuli » larger potential)
Summation can lead to an AP
Define adaptation, why it’s important, and why a neuron may be slow or quick adapting
Rapid adaptor - (ex. light touch to skin) quickly adapts to stop firing even with a simuli, when stimulus is removed, we notice removal
Slow adaptor - (ex. more important stimuli) that fires AP as long as the stimulation is present
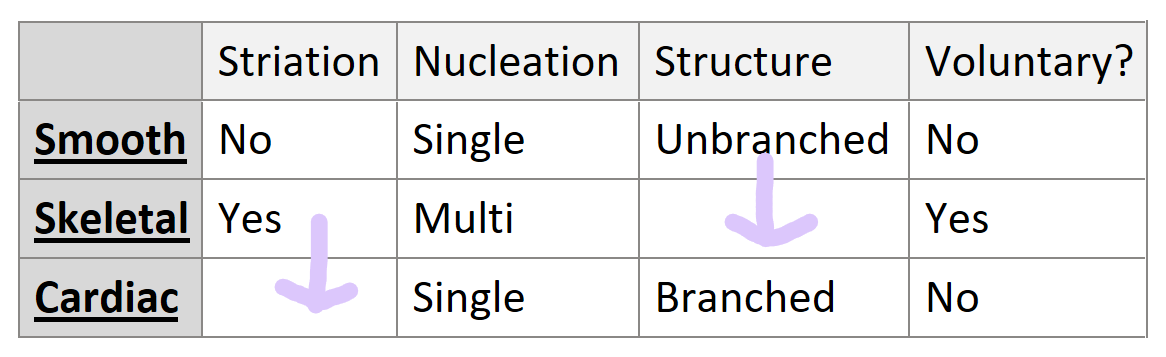
Describe similarities between the three muscle types: shape/size, striation, and voluntary/involuntary
How does signal travel from a motor neuron to a skeletal muscle fiber? Once it reaches the fiber, how does it cause contraction?
AP arrives to neuromuscular junction » ACh is released and triggers AP in T-Tubules » Ca2+ is released from SR and binds to troponin, moving off of actin binding sites » myosin head binds to binding site and causes a power stroke » muscle contracts
Why does rigor mortis develop after death?
ATP is depleted » muscles cannot relax » body stiffens
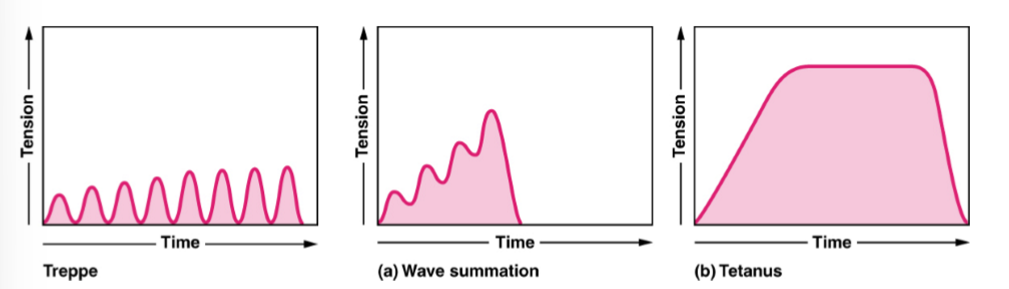
Describe the frequency tension relationship in muscles and how it leads to generation of prolonged muscle tension
Depolarizing muscle with frequent stimuli generates more tension than one twitch
Successive AP summation » increased muscle tension
Tetanus - maintained contraction
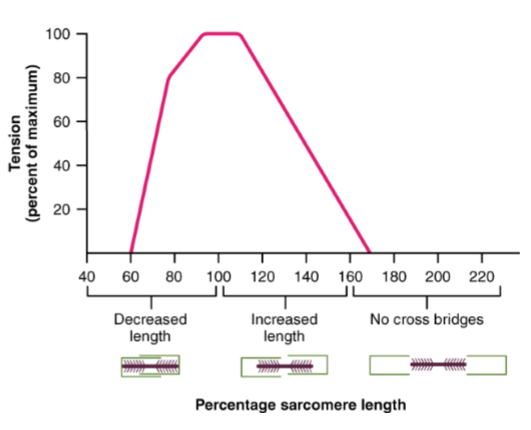
Describe the length tension relationship
There is an optimal amount of stretch that allows a maximum tension in muscle fiber
Over or under stretched muscles are weaker
Due to overlap of filaments » FRANK STARLING MECHANISM
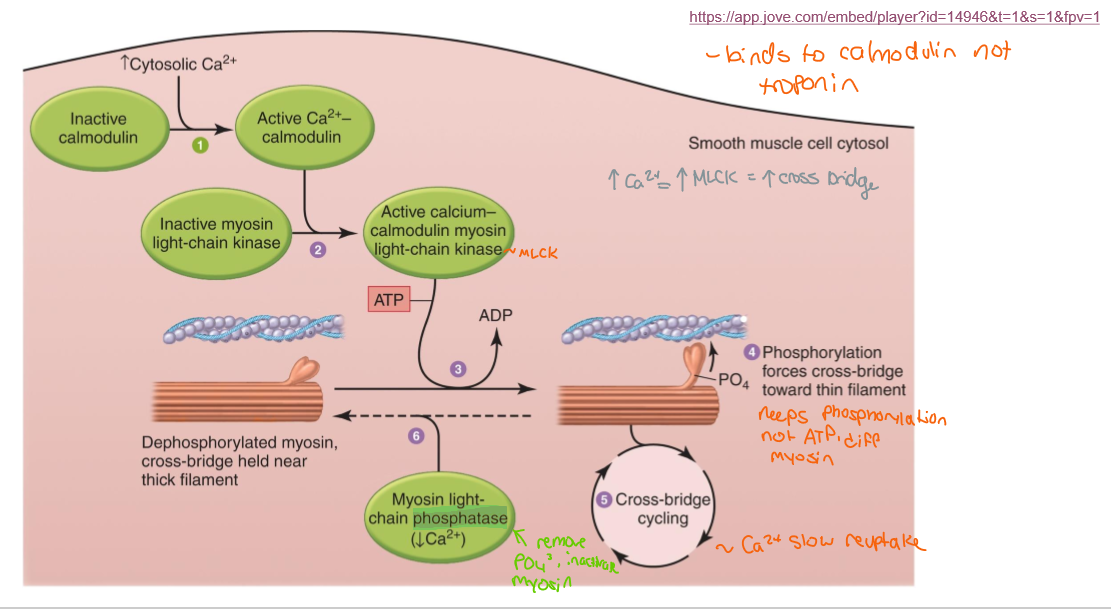
Describe the process of smooth muscle contraction involving myosin light chain kinase (MLCK) and myosin light chain phosphatase (MLCP)
MLCK stays active as long as Ca2+ is present
MLCP is always active
When MLCK activity is less than MLCP » smooth muscle relaxes
Smooth muscle can stay contracted (latch state) if Ca2+ remains elevated in the cytosol
Increased Ca2+ = increased MLCK = increased cross bridge
List the chemical classes of hormones. What can we infer about a hormone’s mechanism of action based on its chemical class?
Amines - derived from tyrosine
often GCPR
TH, Epi, NE, DA
Peptides/proteins - large diverse molecules
RTK, GCPR, JAK/STAT
Angiotensin II, Insulin
Prepro delayed activation form
Steroids - derived from cholesterol
act at nuclear receptors to alter gene activity
Define tropic and trophic
Topic - 1st hormone causes secretion of 2nd hormone
Trophic - 1st hormone stimulates growth of the gland that makes 2nd hormone
Describe how the hypothalamus regulates the release of pituitary hormones, and how this mechanism differs from the anterior to posterior pituitary gland.
Anterior: hypothalamus stimulates anterior pituitary to secrete “releasing hormones” which act on 3rd glands
Posterior: hypothalamus creates hormones which are stored in posterior pituitary
Explain how hormone release is regulated between the hypothalamus, pituitary and “third glands” including negative feedback
Hypothalamus » anterior pituitary » 3rd gland
Third gland secretes hormones that create a negative feedback loop
Describe the effects of cortisol on the body and what happens if there is too much or too little
CRH » ACTH » Cortisol
EFFECTS:
Maintains BP through permissive action on smooth muscle catecholamine activity
maintains levels of metabolic enzymes
keeps immune system in check
increases alpha receptors » stronger catecholamine reaction
Too much = Cushing’s syndrome » weight gain, high blood sugar, immune suppression
Too little = Addison’s disease » fatigue, low blood sugar, weight loss and low BP
What are the effects of thyroid hormone?
Metabolic activity
increase carb absorption
increased fatty acid release from adipose
increased Na/K ATPase activity
calorigenic
GH long bone growth
Permissive effect on fat mobilization in response to Epi
Describe how levels of TH and TSH are related
TSH increases T3/T4.
High T3/T4 = low TSH (negative feedback).
Low T3/T4 = high TSH.
What are the physiological effects of parathyroid hormone?
Low Ca2+ » secrete PTH » increase osteoclasts, absorb Ca2+ in intestine, decrease Ca2+ excretion in kidney
Trace the path of blood flow through the heart, including the chambers and valves
PULMONARY:
Vena cava » RA » tricuspid » RV » pulmonary valve » pulmonary artery
SYSTEMIC:
Pulmonary vein » LA » mitral » LV » aortic valve » aorta
Describe SA node, AV node, and other important structural components of the conduction system
SA node - pacemaker, initiates electrical impulse » atrial contraction
AV node - delays SA impulse so atrial contraction can finish before ventricular contraction, can act as SA backup if SA fails
Bundle of His - moves impulses from AV to ventricles
Purkinje fibers - carry impulse through the ventricles (apex to base)
Explain cardiac action potential and how it differs from the action potential in neurons and skeletal muscle
unlike nerves and skeletal AP, cardiac AP has a long plateau
longer AP » depolarization and contraction have the same duration » no tetanus » ventricles have time to fill with blood before being pumped
Identify and explain the significance of the P wave
atrial depolarization
Identify and explain the significance of the QRS complex
Ventricular depolarization
Identify and explain the significance of the T wave
ventricular repolarization
Identify and explain the significance of the P-R interval
AV node delay
Identify and explain the significance of the Q-T interval
duration of ventricular AP
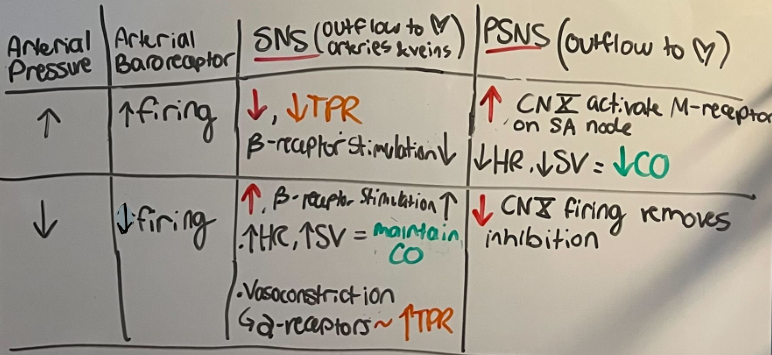
Define cardiac output and how it is regulated by the ANS
amount of blood pumped (L/min)
CO = HR (bpm) x SV (mL)
SNS = higher HR and SV
PSNS = lower HR
Define heart rate and how it is regulated by the ANS
measured in bpm
PSNS - CN X, ACh, M receptors, Atria, lower HR
SNS - thoracic spinal nerves, NE, beta receptors, Atria and ventricles, increase HR
Define stroke volume and how it is regulated by the ANS
amount of blood ejected by one ventricle per heartbeat
SNS - increases ejection fraction
NE and Epi bind to beta receptor » active cAMP » release Ca2+ » stronger contraction
Explain the significance of the Frank Starling mechanism and how it relates to actin and myosin filaments
*stretch = more efficient contraction*
more blood » more stretch » better alignment of actin-myosin filaments » more cross bridge » stronger contraction » higher SV
Explain how the baroreceptor reflex works to maintain mean arterial pressure (MAP)
acts as a reflex arc
MAP (homeostasis) » baroreceptors (receptor to disturbances) » medullary cardiovascular center (control center) » cardiac and smooth muscle (effector) return MAP to set point
Describe the key components that are necessary for the blood to form a clot
Injury » collagen exposed » platelets activate and aggregate » ADP and Thromboxane Az » vasoconstriction & plug forms
Tissue factor » Factor Xa » Thrombin » converts fibrinogen to fibrin, creates factor XIII that stabilizes clot
Describe the four processes involved in respiration:
ventilation
gas transport
external respiration
internal respiration
Define ventilation
breathing
Define gas transport
movement of O2 and CO2 in blood
external respiration
lung O2 » blood
blood CO2 » lungs
Define internal respiration
blood O2 » tissue
cell O2 » blood
Explain how negative intrapleural pressure prevents the lungs from collapsing, and piercing of the chest wall can cause pneumothorax
negative intrapleural pressure creates suction that holds lungs open
if chest wall is pierced, air enters the pleural space » pressure equalizes » lung collapses
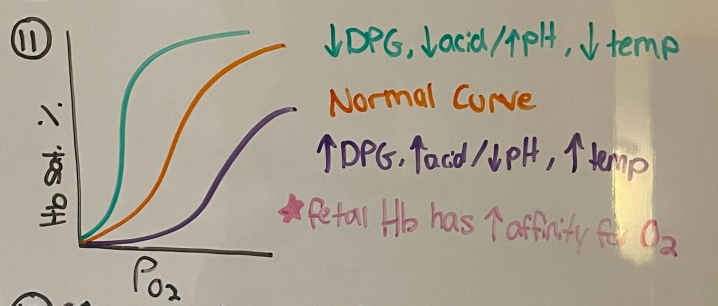
Explain the relationship between PO2 and hemoglobin saturation
increased PO2 » increased hemoglobin saturation
decreased PO2 » decreased hemoglobin saturation
Describe how hemoglobin saturation curve can shift based on pH, temperature, or 2,3-DPG
↓ pH (acidic), ↑ temperature, or ↑ 2,3-DPG → Right shift → ↓ O₂ affinity → more O₂ released to tissues
↑ pH (alkaline), ↓ temperature, or ↓ 2,3-DPG → Left shift → ↑ O₂ affinity → less O₂ released
List the ways that CO2 can be transported in blood
Carbonic acid (H2CO3) ~ 60%
Hb-bound in RBC ~ 30%
Dissolved in plasma ~ 10%
List the reaction that converts CO2 to carbonic acid
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3−
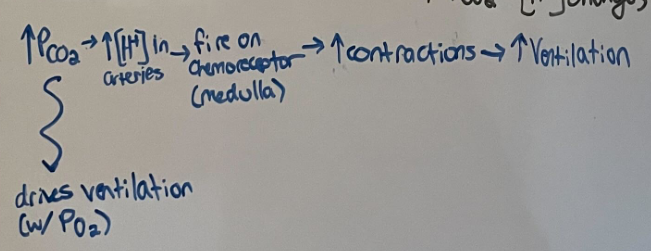
Describe how chemoreceptors regulate respiration and explain why CO2 is usually the most important driver of ventilation
if CO2 increases » pH lowers (acidic) » fires on chemoreceptors » increases ventilation
Describe the structure of the nephron and the sites of filtration, secretion, and reabsorption
Filtration: Glomerulus in Bowman's capsule
Reabsorption: Mainly in proximal tubule, also in loop of Henle, distal tubule, and collecting duct
Secretion: Proximal & distal tubules, collecting duct
What determines whether a substance is filtered? What determines whether a substance is secreted or reabsorbed?
Filtered: Based on size and charge—small, unbound solutes (<~70 kDa) pass through the glomerular filtration barrier.
Reabsorbed: Depends on transporters, concentration gradients, and body needs (e.g., glucose, Na⁺).
Secreted: Requires active transporters; used to remove excess ions, drugs, or waste (e.g., H⁺, K⁺, creatinine).
Explain how sodium reabsorption, including the role of Lumen Na+ channels and Na+/K+ ATPase.
Diffuses from lumen into endothelial cells
Actively transported out of cell (Na+/K+ pump) on basolateral side into interstitial fluid to be reabsorbed
Specific channels and transporters on luminal side differ in different regions of the tubule, but pattern remains the same
What hormone increases Na+ reabsorption, and where in the nephron does it take effect?
aldosterone
distal tubule and collecting duct
Describe the function of vasopressin and the location where it acts within the nephron
adds aquaporin channels to collecting duct » creates more concentrated urine
What happens when vasopressin levels are high or low?
High vasopressin » water is reabsorbed » concentrated urine
Low vasopressin » water remains in ducts » dilute urine
Explain the short and long term mechanisms for blood pressure regulation using the autonomic nervous system and renin-angiotensin system
Short-Term (Autonomic Nervous System):
Sympathetic activation: ↑ heart rate (HR), contractility, and vasoconstriction → ↑ BP
Parasympathetic activation: ↓ HR → ↓ BP
Long-Term (Renin-Angiotensin System):
Renin release (from kidneys) due to low BP, low Na⁺, or sympathetic activation
Angiotensin II:
Vasoconstriction → ↑ BP
Stimulates aldosterone secretion → Na⁺ reabsorption → ↑ blood volume → ↑ BP
Stimulates ADH release → water retention → ↑ blood volume → ↑ BP
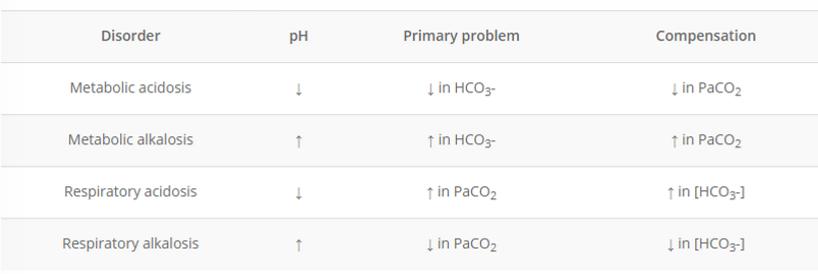
Explain how the lungs and kidneys can alter the balance of CO2/bicarbonate in the body and how these processes would change in order to compensate for alkalosis or acidosis.
Metabolic » same
Metabolic acidosis = (low pH) low HCO3, low CO2
Metabolic alkalosis = (high pH) high HCO3, high CO2
Respiratory » opposite
Respiratory acidosis = (low pH) high HCO3, high CO2
Respiratory alkalosis = (high pH) low HCO3, low CO2
Describe the structure and function of the GI tract wall
Mucosa: Inner lining with epithelium (secretes enzymes, absorbs nutrients), lamina propria (supports), and muscularis mucosa (helps movement).
Submucosa: Connective tissue with blood vessels, lymphatics, and nerves (provides nutrients, regulates secretion).
Muscularis externa: Two layers of smooth muscle (circular and longitudinal) for peristalsis and segmentation.
Serosa (or adventitia): Outer connective tissue layer (protects and anchors organs)
Describe how the GI wall varies within the major organs of the digestive system
Esophagus: Thick mucosa for protection against abrasion, mainly stratified squamous epithelium.
Stomach: Mucosa has gastric glands for acid secretion, muscularis externa has oblique muscle for churning.
Small intestine: Mucosa has villi and microvilli for nutrient absorption.
Large intestine: Mucosa contains goblet cells for mucus production (lubrication).
Describe the digestive processes that occur in the stomach
denaturation of proteins, making enzymes accessible
peristalsis mixes and breaks up food
not a lot of absorption
Glands secretions
parietal cells » secrete HCl and intrinsic factors
chief cells » secrete pepsinogen
g cells » secrete gastrin » stimulates parietal cells
Explain function of gastrin and CCK
gastrin - stimulates parietal cells » HCl
CCK - increases pancreatic enzyme secretion for digestion
What are the roles of pancreatic enzymes and brush border enzymes in digestion?
pancreatic enzymes - digest major molecule classes (carb, fat, protein, NA), activated in sm. intestine lumen
brush border enzymes - produced by intestine epithelial cells and activate pancreatic enzymes to perform digestion
What steps would a starch molecule go through between ingestion and absorption?
Mouth - salivary amylase breaks down alpha bonds in starch; polysaccharides » monosaccharides
Stomach - peristaltic mixing of food breaks down
Pancreas - pancreatic amylase and brush border enzymes perform majority of absorption
Intestines - monosaccharides are absorbed
Describe the effects of insulin on its target cells
Increases glucose uptake into cells
Promotes glycogenesis in liver and muscle
Inhibits gluconeogenesis in liver
Stimulates lipogenesis to create adipose fat storage
Increases protein synthesis from AA
Describe the homeostatic feedback loop involved in body temperature regulation, including the major effector mechanisms for gaining or losing heat
Stimulus: Body temp too high or too low
Sensor: Thermoreceptors in skin & hypothalamus
Control Center: Hypothalamus compares to 37°C set point
Effectors:
To cool down:
Vasodilation (heat loss through skin)
Sweating (evaporative cooling)
To warm up:
Vasoconstriction (retain core heat)
Shivering (muscle heat generation)
- Response: Temperature returns to normal → negative feedback stops the response