Immunology and disease
5.0(1)
Card Sorting
1/96
There's no tags or description
Looks like no tags are added yet.
Last updated 7:20 PM on 5/25/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
97 Terms
1
New cards
Define endemic
disease occurring frequently, at a predictable rate, in a specific location or population
2
New cards
Define carrier
an infected person or other organism, showing no symptoms but able to infect others
3
New cards
Define disease reservoir
the long-term host of a pathogen, with few or no symptoms, always a potential source of a disease outbreak
4
New cards
Define toxin
a small molecules (e.g. peptide made in cells or organisms) that causes disease following contact or absorption. Toxins often affect macromolecules (e.g. enzymes, cell surface receptors)
5
New cards
Define pandemic
epidemic over a very wide area, crossing international boundaries, affecting a large number of people
6
New cards
Define antigen
molecules that causes the immune system to produce antibodies against it
7
New cards
Define antigenic type
different individuals of the same pathogenic species with different surface proteins, generating different antibodies
8
New cards
Define epidemic
rapid spread of infectious disease to a large number of people within a short period of time
9
New cards
Define vector
a person, animal or microbe that carries and transmits an infectious pathogen into another living organism
10
New cards
Define antibiotic
substance produced by a fungus, which diminishes the growth of bacteria
11
New cards
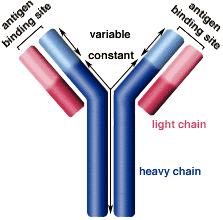
Define antibody
an immunoglobulin produced by the body’s immune system in response to antigens
12
New cards
Define vaccine
a weakened or killed pathogen, or a toxin or antigen derived from it, which stimulates the immune system to produce an immune response against it without causing infection
13
New cards
What is the pathogen that causes cholera? Is it gram-positive or gram-negative?
* *Vibrio cholerae*
* gram-negative bacteria
* gram-negative bacteria
14
New cards
How is cholera transmitted?
through contaminated water or food
15
New cards
What are the symptoms of cholera?
* severe watery diarrhoea
* dehydration → decreased blood pressure
* dehydration → decreased blood pressure
16
New cards
How can cholera be prevented?
* good sanitation and hygeine
* vaccine available → temporary protection but only given to those who are very high risk
* better sewage treatment and water purification
* safe food handling
* regular hand washing
* vaccine available → temporary protection but only given to those who are very high risk
* better sewage treatment and water purification
* safe food handling
* regular hand washing
17
New cards
How can cholera be treated?
* electrolytes given orally or intravenously → replace water and ions
* bacteria treated with antibiotics
* bacteria treated with antibiotics
18
New cards
What is the pathogen that causes tuberculosis?
*Myobacterium tuberculosis*
19
New cards
How is tuberculosis transmitted?
* aerosol transmission
* inhalation of bacteria-laden moisture droplets from sneezes and coughs
* inhalation of bacteria-laden moisture droplets from sneezes and coughs
20
New cards
What are the symptoms of tuberculosis?
* chest infection causing pain and persistent cough
* cough up phlegm (sputum) with blood
* swollen lymph glands
* fever
* loss of appetite
* cough up phlegm (sputum) with blood
* swollen lymph glands
* fever
* loss of appetite
21
New cards
How is tuberculosis treated?
long course of antibiotics but does show some antibiotic resistance
22
New cards
How is tuberculosis prevented?
BCG vaccine → given to babies and, if negative, people up to 16
23
New cards
What is the pathogen that causes smallpox?
*Variola major*
24
New cards
How is smallpox transmitted?
* aerosol transmission
* saliva transmission
* skin contact
* saliva transmission
* skin contact
25
New cards
What are the symptoms of smallpox?
* rash
* pustules (fluid filled blisters)
* fever
* blindness
* limb deformities
* pustules (fluid filled blisters)
* fever
* blindness
* limb deformities
26
New cards
How is smallpox prevented?
vaccination → uses live *Vaccina* virus (close relative to smallpox virus) → produces strong immune response
27
New cards
How is smallpox treated?
* given fluids
* drugs to control fever and pain
* antibiotics to control bacterial infections
* drugs to control fever and pain
* antibiotics to control bacterial infections
28
New cards
What is the pathogen that causes influenza?
*Influenza A,B and C*
29
New cards
How is influenza transmitted?
aerosol transmission
30
New cards
What are the symptoms of influenza?
* sore throat
* fever
* coughs caused by infection of mucus membranes in respiratory system
* fever
* coughs caused by infection of mucus membranes in respiratory system
31
New cards
How is influenza prevented?
* regular hand washing
* using and discarding tissues for sneezing and coughing
* quarantine
* vaccines → variable in their success as surface antigens change so new vaccine needed annually
* using and discarding tissues for sneezing and coughing
* quarantine
* vaccines → variable in their success as surface antigens change so new vaccine needed annually
32
New cards
Why is flu more common in winter than in summer?
* - survives better when:
* air is dry
* low ultraviolet light in environment
* air is dry
* low ultraviolet light in environment
33
New cards
What is antigenic drift and what is it caused by?
* gradual change in surface proteins of a virion
* caused as no RNA proofreading enzymes → after replication every new virion has a new mutation
* caused as no RNA proofreading enzymes → after replication every new virion has a new mutation
34
New cards
What is antigenic shift and what is it caused by?
the combination of 2 strands of RNA from 2 viruses that have different combinations of surface proteins → new virus made
35
New cards
Why is the genetic material of influenza so unusual?
it has 8 single strands of RNA instead of 1
36
New cards
What is the role of Haemagglutanin?
role in virus entering host cell
37
New cards
What is the role of Neuraminidase?
role in virus exiting host cell
38
New cards
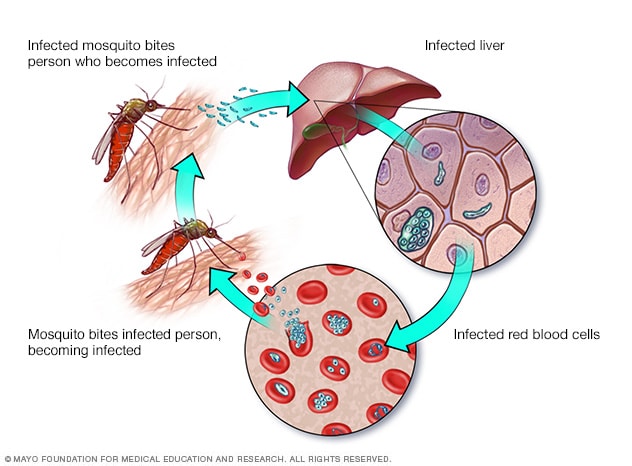
What is the pathogen which causes malaria and what are the 2 most deadly types?
*Plasmodium → P. falciparum and P. vivax*
39
New cards
What is malaria transmitted by?
female *Anopheles* mosquitoes → vectors that infect humans with sporozoites that are in their saliva
40
New cards
What are the symptoms of malaria?
fever
41
New cards
How is malaria prevented?
* sleep under nets
* mosquitoes feed between dusk and dawn
* nets treated with pyrethoid insecticide
* kill mosquitoes
* spray indoor walls with insecticide
* kills mosquitoes that rest on walls after feeding
* drain/cover stagnant water
* removes mosquitoes’ access to egg-laying sites
* film of oil on water
* lowered surface tension prevents larvae piercing water to obtain oxygen
* fish introduced into water
* fish eat larvae
* infecting mosquitoes with *Wolbachia*
* blocks *Plasmodium* development in mosquitoes
* sterilise male mosquitoes with x-rays
* no offspring produced
* mosquitoes feed between dusk and dawn
* nets treated with pyrethoid insecticide
* kill mosquitoes
* spray indoor walls with insecticide
* kills mosquitoes that rest on walls after feeding
* drain/cover stagnant water
* removes mosquitoes’ access to egg-laying sites
* film of oil on water
* lowered surface tension prevents larvae piercing water to obtain oxygen
* fish introduced into water
* fish eat larvae
* infecting mosquitoes with *Wolbachia*
* blocks *Plasmodium* development in mosquitoes
* sterilise male mosquitoes with x-rays
* no offspring produced
42
New cards
How is malaria treated?
* drugs don’t attack when plasmodium in cells so have to be used when in the blood
* currently combination of artemisinin with other drugs → unlikely plasmodium develops resistance to all drugs at same time
* currently combination of artemisinin with other drugs → unlikely plasmodium develops resistance to all drugs at same time
43
New cards
Why is there no vaccine for malaria?
mutates frequently and produces many antigenic types
44
New cards
Why are antibiotics alone not a cure for cholera?
* stop growth of bacteria but toxin may remain
* may be antibiotic resistant
* antibiotics will pass through gut before able to act on bacteria
* may be antibiotic resistant
* antibiotics will pass through gut before able to act on bacteria
45
New cards
Why are viruses difficult to treat with drugs?
* only active inside cells → drugs would damage cells of host
* viruses aren’t cellular → don’t have metabolic pathways
* viruses enter host cells → unrecognisable by immune system
* antigenic variation/drug resistance
* viruses aren’t cellular → don’t have metabolic pathways
* viruses enter host cells → unrecognisable by immune system
* antigenic variation/drug resistance
46
New cards
What is the lytic cycle?
* when virus immediately reproduces using host metabolism to copy own nucleic acid and protein coat
* released by:
* lysis of host cell
* budding → they acquire an envelope from the host cell’s membrane
* released by:
* lysis of host cell
* budding → they acquire an envelope from the host cell’s membrane
47
New cards
What is a lysogenic virus?
* a virus that integrates its nucleic acid into the host cell genome and remain in cell with no effect
* enter lytic cycle later and then produce symptoms
* enter lytic cycle later and then produce symptoms
48
New cards
What are the different ways in which a virus can be pathogenic?
* cell lysis
* toxins
* cell transformation
* immune suppression
* toxins
* cell transformation
* immune suppression
49
New cards
What is pathogenicity due to cell lysis?
* bacteria infected with bacteriophage → pressure of new virus particles inside causes bacteria to burst
* in virus-infected animal cells, inflammation caused by antibodies = lysis
* in virus-infected animal cells, inflammation caused by antibodies = lysis
50
New cards
What is pathogenicity due to toxins?
* many viral components and their by-products (toxins) are toxic
* measles virus = chromosome fusion
* herpes virus = cell fusion
* viral proteins inhibit RNA, DNA and protein synthesis
* measles virus = chromosome fusion
* herpes virus = cell fusion
* viral proteins inhibit RNA, DNA and protein synthesis
51
New cards
What is pathogenicity due to cell transformation?
* viral DNA integrates into host chromosome
* if DNA inserts pro-oncogene or tumour suppressor gene = rapid, uncontrolled division (cancer)
* if DNA inserts pro-oncogene or tumour suppressor gene = rapid, uncontrolled division (cancer)
52
New cards
What is pathogenicity due to immune suppression?
* suppression of reactions that cause mature B and T lymphocytes
* reduction in antibody formation
* reduction of phagocytic cells engulfing microbes
* reduction in antibody formation
* reduction of phagocytic cells engulfing microbes
53
New cards
How is malaria transmitted?
1. mosquito injects sporozoites when taking blood meal
2. sporozoites produce merozoites
3. blood cells infected with merozoites which develop to further stage
4. red blood cells burst and release more merozoites
5. some merozoites become gametozoite
6. infects mosquito when blood meal taken
54
New cards
How does cholera cause dehydration and diarrhoea?
* vibrio cholerae arrive in small intestine
* secrete toxins that move into cells of small intestine
* toxin causes Cl- ions to diffuse out of the small intestine cell walls and into the lumen
* this decreases water potential of lumen so water diffuses out of cells and into lumen by osmosis
* water excreted as diarrhoea
* dehydration occurs
* secrete toxins that move into cells of small intestine
* toxin causes Cl- ions to diffuse out of the small intestine cell walls and into the lumen
* this decreases water potential of lumen so water diffuses out of cells and into lumen by osmosis
* water excreted as diarrhoea
* dehydration occurs
55
New cards
What are the different types of antimicrobials?
* antiseptics → used on living tissue
* disinfectants → used on non-living surfaces
* antibiotics
* disinfectants → used on non-living surfaces
* antibiotics
56
New cards
Why are antibiotics not harmful to the patient’s cells?
* only act on bacteria
* don’t act on eukaryotic cells or viruses
* don’t act on eukaryotic cells or viruses
57
New cards
What are broad-spectrum antibiotics?
antibiotics that target many bacteria (both gram-positive and gram-negative)
58
New cards
What are narrow-spectrum antibiotics?
antibiotics that target specific bacteria (either gram-negative or gram-positive)
59
New cards
What do bactericidal antibiotics do?
kill bacteria
60
New cards
What do bacteriostatic antibiotics do?
prevent bacterial multiplication but don’t cause death
61
New cards
How does penicillin work?
* diffuses through cell wall of gram-positive bacteria → can enter some gram-negative bacteria through porins (surface molecules)
* penicillin binds to DD-transpeptidase
* bacteria continually make and break down parts of their cell walls
* enzyme DD-transpeptidase catalyses cross-link formation between amino acid side chains and peptidoglycan molecules
* breakdown by hydrolysis continues → more cell wall lost than gained
* cell wall weakened so when water enters by osmosis, increased pressure potential causes cell lysis
* penicillin binds to DD-transpeptidase
* bacteria continually make and break down parts of their cell walls
* enzyme DD-transpeptidase catalyses cross-link formation between amino acid side chains and peptidoglycan molecules
* breakdown by hydrolysis continues → more cell wall lost than gained
* cell wall weakened so when water enters by osmosis, increased pressure potential causes cell lysis
62
New cards
What are the 2 types of fungi species used in Penicillin production?
* *Penicillium notatum*
* *Penicillium chrysogenum*
* *Penicillium chrysogenum*
63
New cards
What type of antibiotic is tetracycline?
* broad-spectrum
* bacteriostatic
* bacteriostatic
64
New cards
How does tetracycline work?
* inhibits protein synthesis
* diffuses and is pumped into bacterial cells
* binds to 30S subunit of ribsomes and blocks tRNA attachment in 2nd position
* no new amino acids can be added
* bind reversibly → bacteriostatic
* diffuses and is pumped into bacterial cells
* binds to 30S subunit of ribsomes and blocks tRNA attachment in 2nd position
* no new amino acids can be added
* bind reversibly → bacteriostatic
65
New cards
What are the 2 sources of antibiotic resistance alleles?
* mutation conferring resistance that arises after replication
* bacteria divide rapidly → high mutation rate
* plasmids conferring resistance may be acquired from their environment
* plasmids replicate inside bacteria and are passed onto daughter cells when they replicate
* bacteria divide rapidly → high mutation rate
* plasmids conferring resistance may be acquired from their environment
* plasmids replicate inside bacteria and are passed onto daughter cells when they replicate
66
New cards
How might bacteria adapt to become resistant to penicillin?
* secrete β-lactamase → enzyme that degrades penicillin
* altered PBP → penicillin can’t bind
* fewer or smaller porins → reduce penicillin entry
* altered PBP → penicillin can’t bind
* fewer or smaller porins → reduce penicillin entry
67
New cards
How might bacteria adapt to become resistant to tetracycline?
* pump tetracycline out of cell
* dislodge bound tetracycline
* prevent tetracycline attaching to ribosome
* dislodge bound tetracycline
* prevent tetracycline attaching to ribosome
68
New cards
How does antibiotic resistance in bacteria arise through the use of antibiotics?
* antibiotic kills bacteria susceptible to antibiotics
* those with mutation for antibiotic resistance survive
* divide to pass on advantageous allele
* new population of antibiotic resistant bacteria
* those with mutation for antibiotic resistance survive
* divide to pass on advantageous allele
* new population of antibiotic resistant bacteria
69
New cards
What are the causes of antibiotic resistance in bacteria?
* over-prescribing of antibiotics
* patients not finishing antibiotics course
* lack of hygiene and poor sanitation
* poor infection control in hospitals and clinics
* overuse of antibiotics in livestock and fish farming
* patients not finishing antibiotics course
* lack of hygiene and poor sanitation
* poor infection control in hospitals and clinics
* overuse of antibiotics in livestock and fish farming
70
New cards
What is the innate immune system?
physical, chemical and biological defences that are used to reduce the chance of pathogens entering the body
71
New cards
Which structures make up the innate immune system and how are they a barrier to infection?
* skin
* keratin (epidermal cells) → makes skin waterproof
* collagen → makes skin tough
* skin flora → out-compete pathogenic strains because skin flora not easily washed off
* blood clots → seal wounds
* inflammation → raised temperature from increased blood flow unfavourable to microbes
* decreased pH → inhospitable for pathogens
* mucus (e.g. in gut/trachea)
* contains lysosome → hydrolyses peptidoglycan
* tears
* contains lysosome → hydrolyses peptidoglycan
* saliva
* contains lysosome → hydrolyses peptidoglycan
* sweat
* contains lysosome → hydrolyses peptidoglycan
* stomach
* HCl kills bacteria
* vagina
* low pH → inhospitable for pathogens
* keratin (epidermal cells) → makes skin waterproof
* collagen → makes skin tough
* skin flora → out-compete pathogenic strains because skin flora not easily washed off
* blood clots → seal wounds
* inflammation → raised temperature from increased blood flow unfavourable to microbes
* decreased pH → inhospitable for pathogens
* mucus (e.g. in gut/trachea)
* contains lysosome → hydrolyses peptidoglycan
* tears
* contains lysosome → hydrolyses peptidoglycan
* saliva
* contains lysosome → hydrolyses peptidoglycan
* sweat
* contains lysosome → hydrolyses peptidoglycan
* stomach
* HCl kills bacteria
* vagina
* low pH → inhospitable for pathogens
72
New cards
What is the adaptive immune system?
immune response that produces a specific response to each antigen
73
New cards
What are the 2 components of the adaptive response?
* the humoral response
* the cell-mediated response
* the cell-mediated response
74
New cards
What is the difference between the humoral response and the cell-mediated response?
* humoral response results in the production of antibodies
* cell-mediated response results in the activation of phagocytic cells (more emphasis on T lymphocytes than B)
* can stimulate cells from humoral response to make antibodies but doesn’t directly produce antibodies
* cell-mediated response results in the activation of phagocytic cells (more emphasis on T lymphocytes than B)
* can stimulate cells from humoral response to make antibodies but doesn’t directly produce antibodies
75
New cards
What happens in the humoral response?
* Antigen presenting cell (phagocyte) presents foreign protein to B-lymphocytes
* B-lymphocytes undergo:
* clonal selection
* specific receptors that match antigen are selected
* clonal expansion
* proliferation by mitosis (replication)
* B-lymphocytes then differentiate into:
* memory cells
* remain dormant in circulation
* divide to form more B-lymphocytes if same antigen encountered in future
* plasma cells
* release antibodies (immunoglobulins)
* antibodies agglutinate (clump) antigen together
* neutralise them (prevent pathogen entering cell)
* B-lymphocytes undergo:
* clonal selection
* specific receptors that match antigen are selected
* clonal expansion
* proliferation by mitosis (replication)
* B-lymphocytes then differentiate into:
* memory cells
* remain dormant in circulation
* divide to form more B-lymphocytes if same antigen encountered in future
* plasma cells
* release antibodies (immunoglobulins)
* antibodies agglutinate (clump) antigen together
* neutralise them (prevent pathogen entering cell)
76
New cards
What happens in the cell-mediated response?
* Antigen presenting cell (phagocyte) presents foreign protein to T-lymphocytes
* T-lymphocytes undergo:
* clonal selection
* specific receptors that match antigen are selected
* clonal expansion
* proliferation by mitosis (replication)
* T-lymphocytes then produce:
* T-memory cells
* remain dormant in circulation
* divide to make more T-lymphocytes if same antigen encountered in future
* T-killer/cytotoxic cells
* lyse pathogenic cells that possess antigens (use word **lysis;** NOT KILL)
* T-suppressor cells
* regulate immune response
* T-helper cells
* release cytokines that stimulate:
* phagocytic cells to engulf pathogens
* B and T lymphocytes to undergo clonal expansion
* B-lymphocytes to make antibodies
* T-lymphocytes undergo:
* clonal selection
* specific receptors that match antigen are selected
* clonal expansion
* proliferation by mitosis (replication)
* T-lymphocytes then produce:
* T-memory cells
* remain dormant in circulation
* divide to make more T-lymphocytes if same antigen encountered in future
* T-killer/cytotoxic cells
* lyse pathogenic cells that possess antigens (use word **lysis;** NOT KILL)
* T-suppressor cells
* regulate immune response
* T-helper cells
* release cytokines that stimulate:
* phagocytic cells to engulf pathogens
* B and T lymphocytes to undergo clonal expansion
* B-lymphocytes to make antibodies
77
New cards
Where are T-lymphocytes produced and where do they mature?
* made in bone marrow
* mature in thymus gland
* mature in thymus gland
78
New cards
Where are B-lymphocytes produced and where do they mature?
* made in bone marrow
* mature in spleen and lymph nodes
* mature in spleen and lymph nodes
79
New cards
What is the structure of an antibody?
* Y-shaped glycoprotein → immunoglobulin
* quaternary structure → 4 polypeptides held together by disulphide bonds
* have variable portions → specific to each antigen
* each antibody can bind to 2 antigens → agglutinate
* quaternary structure → 4 polypeptides held together by disulphide bonds
* have variable portions → specific to each antigen
* each antibody can bind to 2 antigens → agglutinate
80
New cards
What happens in the primary immune response?
* macrophages engulf foreign antigen or cell/virus antigen is attached to
* incorporate antigenic molecules into their cell membrane → antigen presentation
* T helper cells detect antigens
* secrete cytokines
* B plasma cells secrete antibodies for about 3 weeks
* incorporate antigenic molecules into their cell membrane → antigen presentation
* T helper cells detect antigens
* secrete cytokines
* B plasma cells secrete antibodies for about 3 weeks
81
New cards
What happens in the secondary immune response?
* memory cells undergo clonal expansion → faster than in primary response
* antibodies made more quickly → 100 times more concentrated than in primary response
* remain at high concentration in circulation for longer → no symptoms
* antibodies made more quickly → 100 times more concentrated than in primary response
* remain at high concentration in circulation for longer → no symptoms
82
New cards
What is active immunity?
when the body makes its own antibodies, stimulated by either infection or vaccination
83
New cards
Is active immunity temporary or long-lasting? Why?
* long-lasting
* body produces memory cells
* body produces memory cells
84
New cards
What can be used to make a vaccine?
* antigens isolated from pathogens
* weakened (‘attenuated’) strains of pathogen
* inactive or killed pathogen
* inactivated toxin
* weakened (‘attenuated’) strains of pathogen
* inactive or killed pathogen
* inactivated toxin
85
New cards
Why do vaccinations create active immunity?
* vaccine recognised as non-self
* immune system behaves as it would if pathogen were present → own antibodies made
* immune system behaves as it would if pathogen were present → own antibodies made
86
New cards
Why are boosters needed for vaccinations?
* number of memory cells decreases over time if not exposed to antigen again
* booster further exposes body to vaccine
* response is bigger, faster and longer-lasting than first
* more memory cells are made → body protected for longer
* booster further exposes body to vaccine
* response is bigger, faster and longer-lasting than first
* more memory cells are made → body protected for longer
87
New cards
What is passive immunity?
when the body receives antibodies produced by another individual
88
New cards
When does passive immunity naturally happen?
* from mother to foetus across the placenta
* to the baby in breast milk
* to the baby in breast milk
89
New cards
When are antibody injections given?
* when rapid resistance is needed and there is no time for an active immune response to develop
* cases of PIDD (primary immune deficiency disease) and cases of acquired immunity conditions
* cases of PIDD (primary immune deficiency disease) and cases of acquired immunity conditions
90
New cards
Is passive immunity temporary or long-lasting? Why?
* temporary
* injected antibodies are recognised as foreign and are killed off
* additionally, no memory cells produced
* injected antibodies are recognised as foreign and are killed off
* additionally, no memory cells produced
91
New cards
What is needed for a vaccine to successfully protect against a disease?
* antigen should be highly immunogenic
* single dose causes strong immune response
* rapidly makes large number of specific antibodies
* should only be one antigenic type of the pathogen
* if virus has mutated, memory cells produced in first exposure may not be stimulated in next exposure
* single dose causes strong immune response
* rapidly makes large number of specific antibodies
* should only be one antigenic type of the pathogen
* if virus has mutated, memory cells produced in first exposure may not be stimulated in next exposure
92
New cards
What is herd immunity?
when enough people are vaccinated that there are fewer live pathogens in the population, so even people who haven’t been vaccinated have some protection
93
New cards
Why might some people not get vaccinated?
* vaccination may not be medically advised
* immunocompromised
* chemotherapy
* HIV-AIDS
* very old
* very ill
* choose not to be vaccinated
* religious objections
* preference for ‘natural’/’alternative’ medicine
* mistrust of pharmaceutical companies that produce the vaccines
* safety fears
* immunocompromised
* chemotherapy
* HIV-AIDS
* very old
* very ill
* choose not to be vaccinated
* religious objections
* preference for ‘natural’/’alternative’ medicine
* mistrust of pharmaceutical companies that produce the vaccines
* safety fears
94
New cards
What must the authorities consider when making a decision about mass vaccination, apart from ethical objections?
cost effectiveness
95
New cards
Are vaccinations compulsory in the UK? Why? Are there any complications with this?
* No
* the government can’t infringe on the right of the individual to choose which medicine they take
* complication:
* should there be compulsory vaccinations for healthcare workers? → duty to not harm others which is jeopardised if not vaccinated
* the government can’t infringe on the right of the individual to choose which medicine they take
* complication:
* should there be compulsory vaccinations for healthcare workers? → duty to not harm others which is jeopardised if not vaccinated
96
New cards
What is the argument against vaccinations regarding side effects? What are common side effects?
considering complexity of living systems, it would be extraordinary for vaccinations to only affect one aspect of the body’s biochemistry
\
common side effects include:
* soreness at injection site
* fever
* fatigue
* muscle or joint pain
\
common side effects include:
* soreness at injection site
* fever
* fatigue
* muscle or joint pain
97
New cards
Why are severe side effects from vaccinations rare?
vaccinations are rigorously tested