Comprehensive Reproductive System: Male & Female Anatomy, Menstrual Cycle, and Fertility
1/124
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
125 Terms
What external structures are included in the male reproductive system?
The penis, scrotum, and testes.
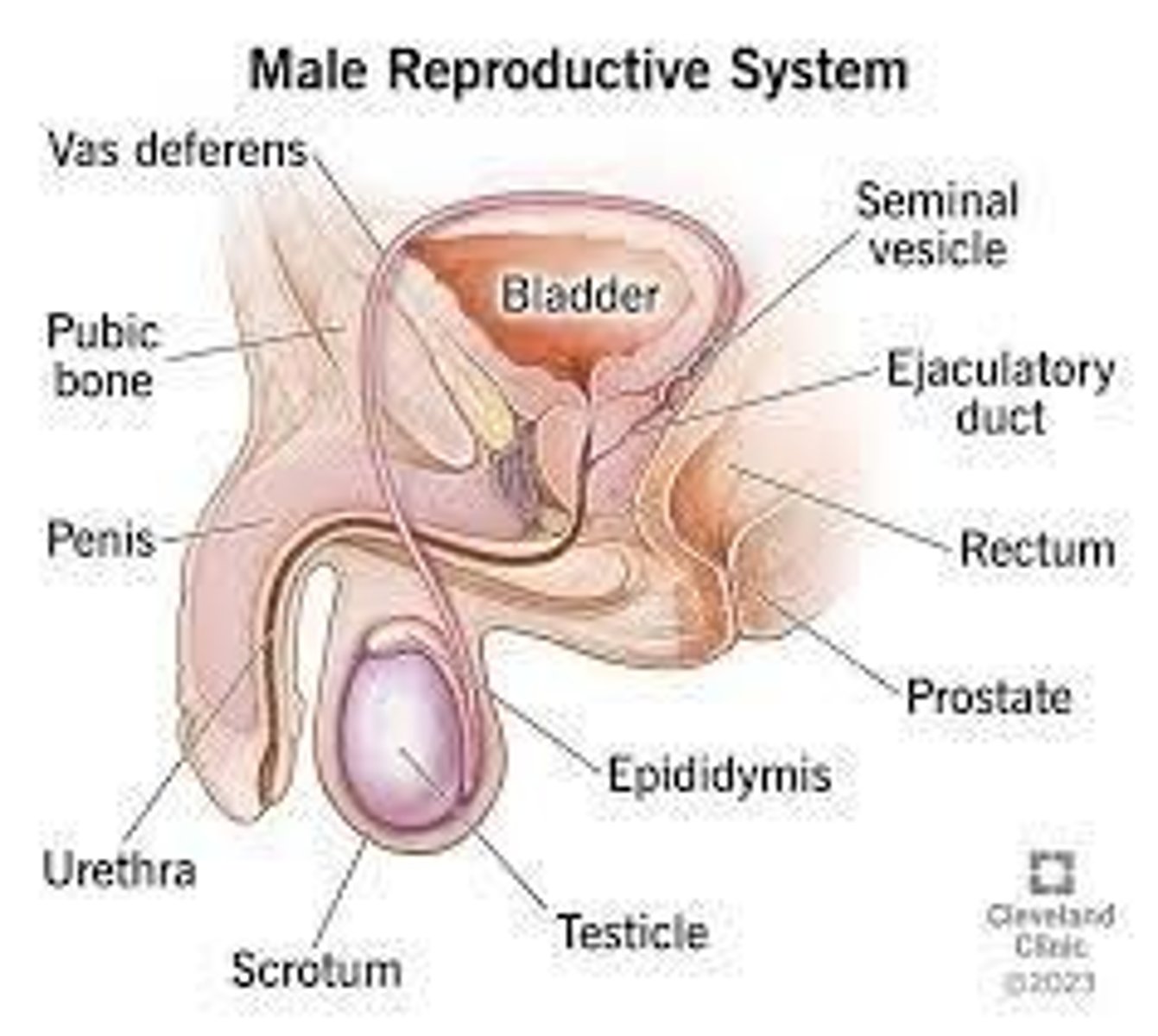
What is the function of the scrotum?
It supports the testes and regulates their temperature to promote sperm production and viability.
How does the scrotum respond to cold and hot temperatures?
In cold weather, the scrotal muscle contracts to bring the testes closer to the body; in hot weather, it relaxes to allow the testes to fall away from the body.
What are the two main components of the testes?
Leydig's cells and seminiferous tubules.
What is the role of Leydig's cells in the testes?
They are responsible for the production of the male hormone testosterone.
What do seminiferous tubules produce?
Spermatozoa.
What is a characteristic of the positioning of the testes in the scrotum?
One testis is slightly larger and lower than the other.
Where do the testes form in a fetus before descending?
In the pelvic cavity.
What is cryptorchidism?
A condition where the testes do not descend properly, often seen in male preterm infants.
What is the primary function of the penis?
To serve as an outlet for both the urinary and reproductive tracts.
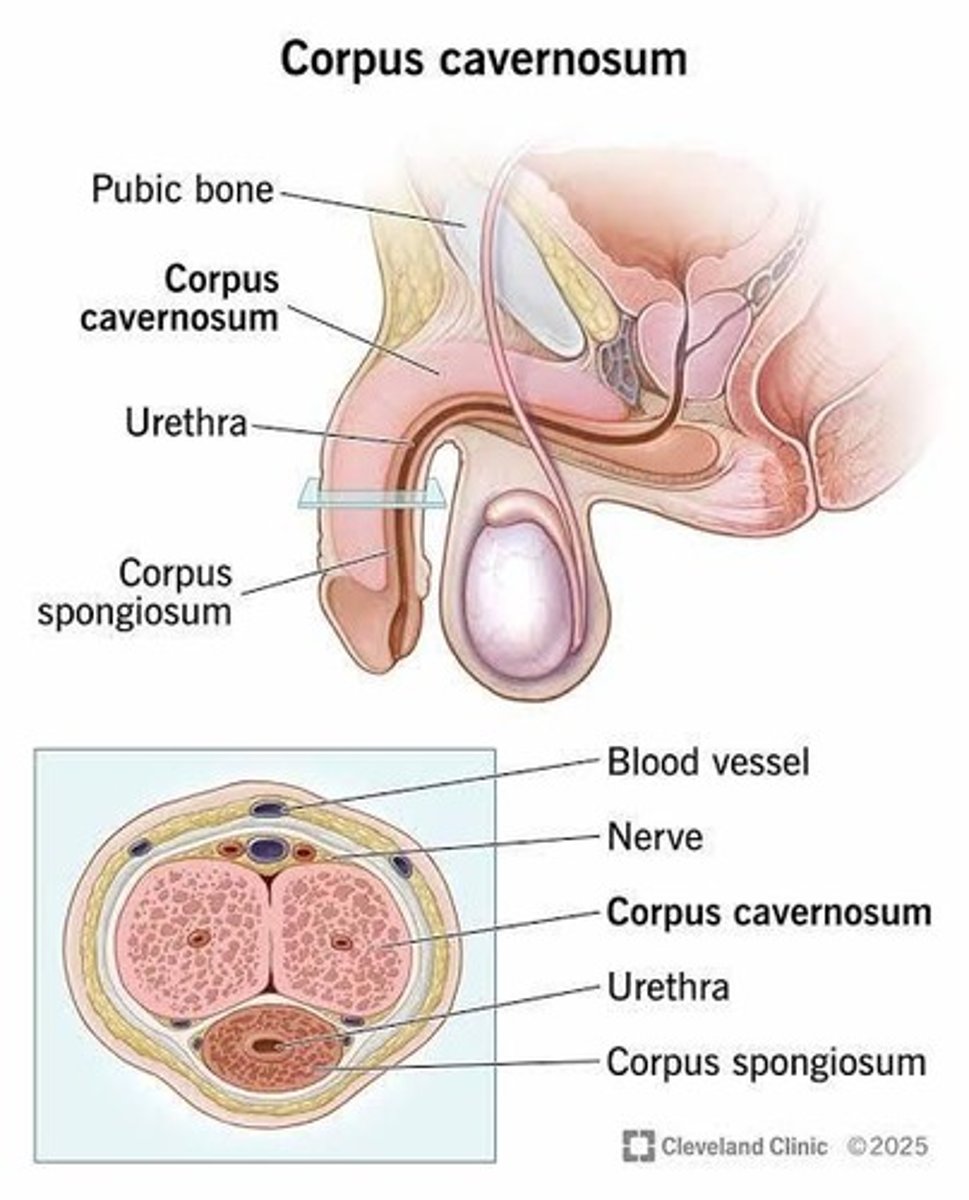
What are the three cylindrical masses of erectile tissue in the penis?
Two corpus cavernosa and one corpus spongiosum.
What is the epididymis responsible for?
Conducting sperm from the testis to the vas deferens.
How long is the epididymis and how long does it take for sperm to mature there?
Approximately 20 feet long; sperm take 12-20 days to travel through and 64 days to mature.
What is aspermia?
A condition characterized by the absence of sperm.
What is the vas deferens and its role?
A hollow tube that carries sperm from the epididymis through the inguinal canal to the abdominal cavity.
What is a varicocele?
An enlargement of the veins within the scrotum.
What is a vasectomy?
A surgical procedure for male sterilization where the vas deferens are cut and sealed to prevent sperm from entering the urethra.
What are seminal vesicles and their function?
Two pouches that lie along the lower portion of the bladder, emptying into the urethra via the ejaculatory ducts.
What do the ejaculatory ducts do?
They pass through the prostate and join the seminal vesicles to the urethra.
What is the function of the prostate gland?
To secrete a thin alkaline fluid that protects sperm from the acidic environment of the urethra.
What are bulbourethral glands and their role?
Glands that secrete an alkaline fluid to counteract the acidity of the urethra, ensuring safe passage of spermatozoa.
What are the main components of semen and their respective contributions?
Semen is derived from the prostate gland (60%), seminal vesicles (30%), epididymis (5%), and bulbourethral glands (5%).
What is the normal volume of semen per ejaculation?
Averages 2.5 ml (1 teaspoon).
How many sperm are typically found in an ejaculate?
50-200 million sperm per cc, or approximately 400 million per ejaculation.
How long can sperm remain capable of fertilization after ejaculation?
Sperm can be fertilizing for 3-4 days after ejaculation.
How quickly do sperm reach the cervix and the outer end of the fallopian tube after deposition?
Sperm generally reach the cervix in 80 seconds and the outer end of the fallopian tube within 5 minutes.
What is the function and length of the urethra in males?
The urethra is a hollow tube leading from the base of the bladder to the outside through the shaft and glans penis, approximately 8 inches (18-20 cm) long.
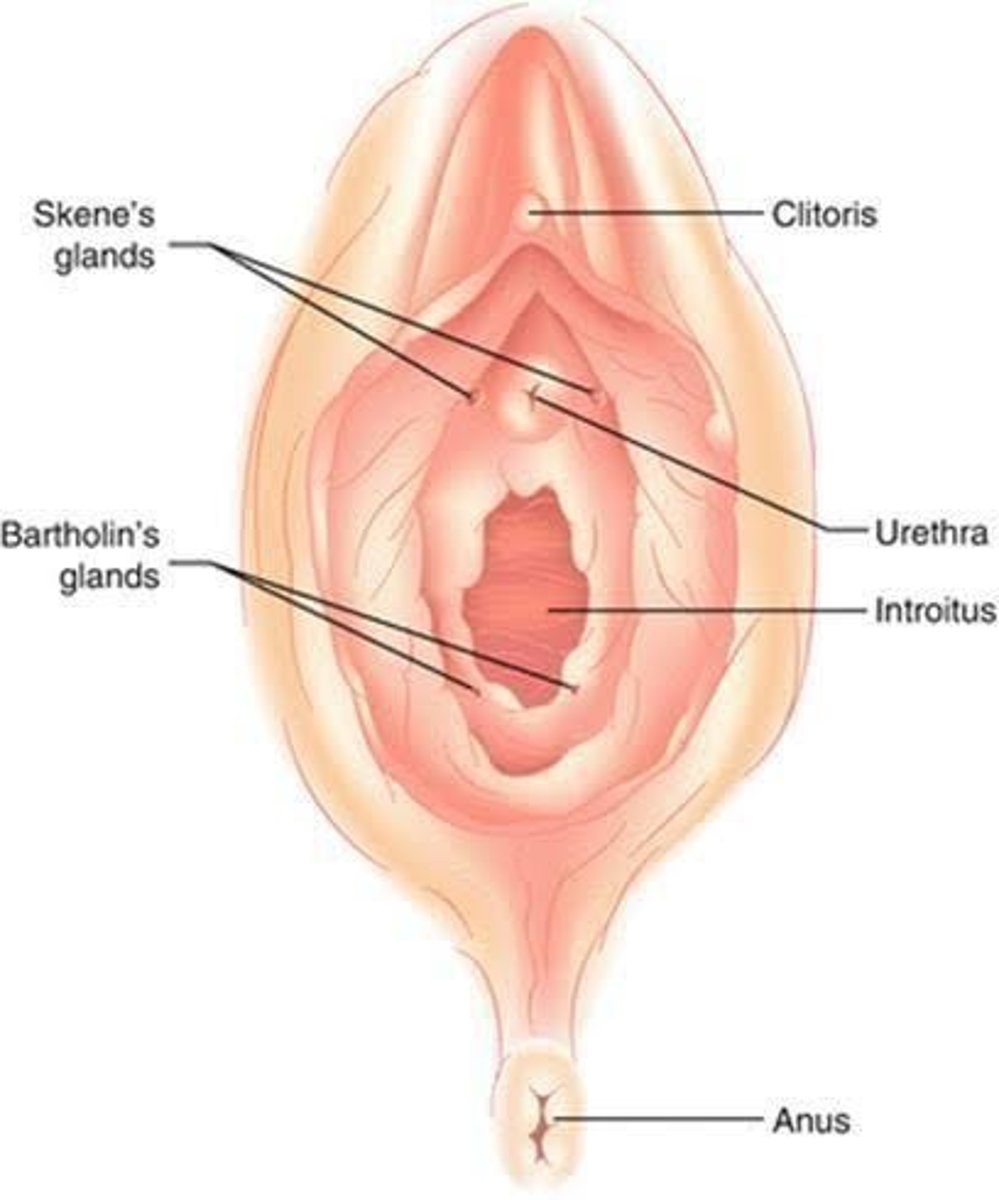
What is the mons pubis and its function?
The mons pubis is a pad of fat over the symphysis pubis, covered by coarse, curly hair, and protects the pubic bone junctions from trauma.
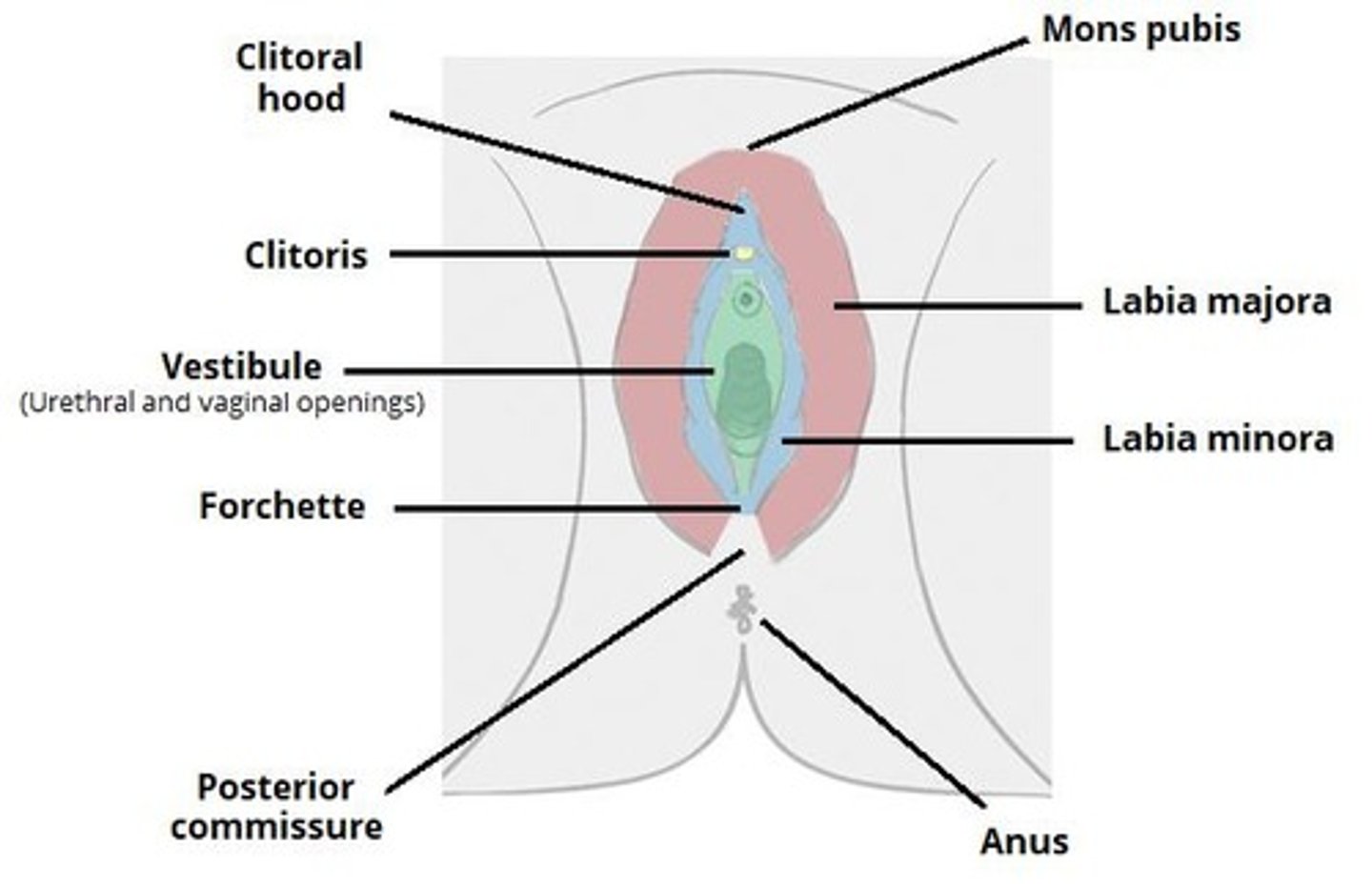
Describe the labia majora and their role in the female reproductive system.
The labia majora are two folds of adipose tissue covered by pubic hair that protect the external genitalia, distal urethra, and vagina.
What changes occur in the labia minora before and after menarche?
Before menarche, the labia minora are small; during childbearing age, they become firm and full; after menopause, they atrophy and become smaller.
What is the clitoris and its significance?
The clitoris is a small (1-2 cm) rounded organ of erectile tissue, sensitive to touch and temperature, and is the center of arousal and orgasm in females.
What are Skene's glands and their location?
Skene's glands (paraurethral glands) are located just lateral to the urinary meatus, with ducts opening into the urethra.
What are Bartholin's glands and their function?
Bartholin's glands are located just lateral to the vaginal opening, with ducts opening in the distal vagina, and their secretions help lubricate the external genitalia during coitus.
How do the secretions of Skene's and Bartholin's glands affect sperm?
The alkaline pH of their secretions helps improve sperm survival in the vagina.
What is the fourchette?
The fourchette is the ridge of tissue formed by the posterior joining of the two labia minora and labia majora.
What is the perineum and its role during childbirth?
The perineum is the muscular area posterior to the fourchette that stretches during childbirth to allow the passage of the fetal head.
What are Kegel exercises and their purpose?
Kegel exercises are performed to make perineal muscles flexible, allowing optimal expansion during birth to prevent tearing of tissue.
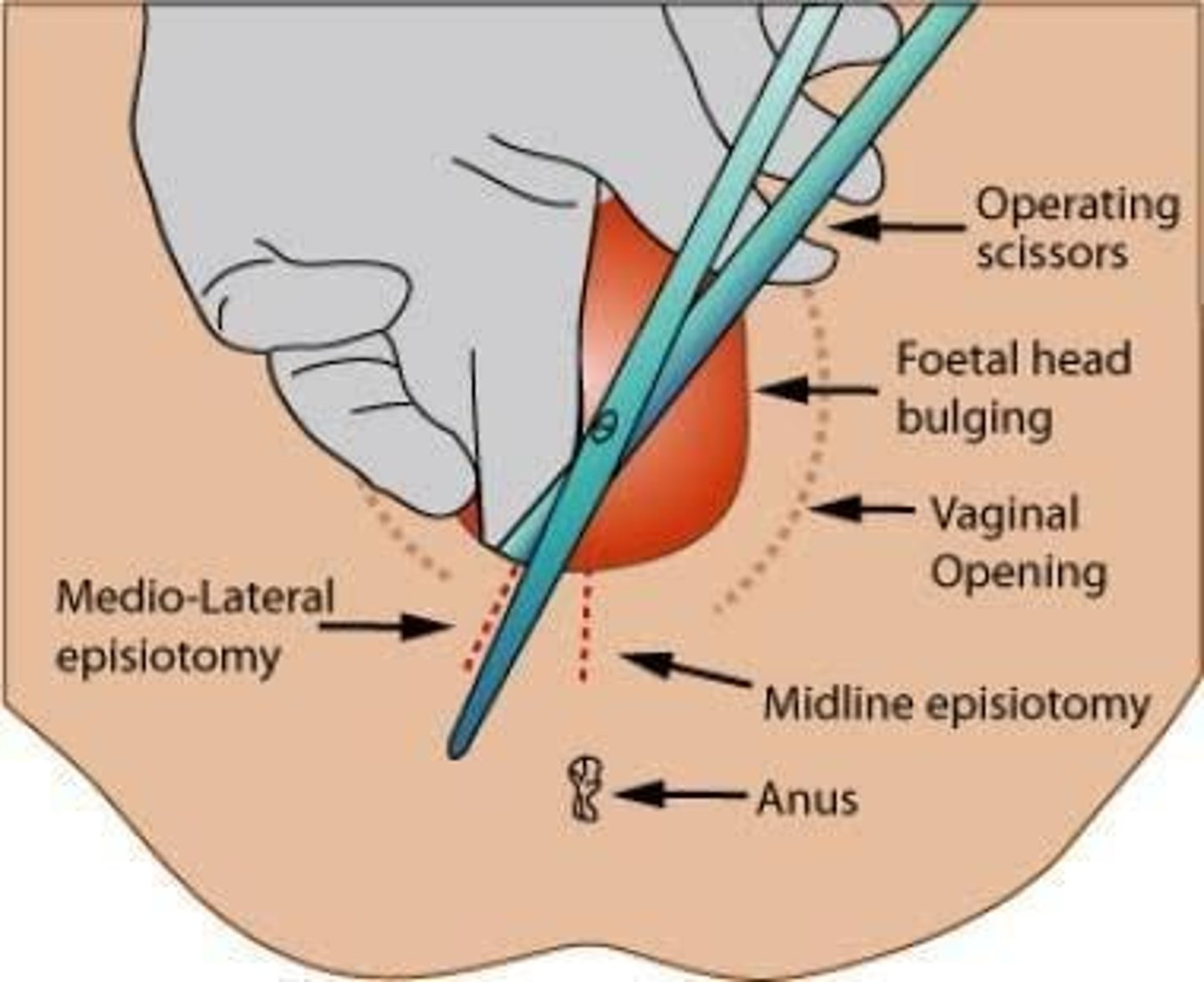
What is an episiotomy and when is it performed?
An episiotomy is performed during the second stage of labor to create an enlarged opening for the baby to pass through easily.
What is the blood supply of the external genitalia?
Pudendal artery and a portion of the inferior rectus artery.
What is the role of the pudendal vein?
It is responsible for venous return from the external genitalia.
What can cause varicosities in the pudendal vein during childbirth?
Pressure from the fetal head can cause extensive back-pressure.
What are the consequences of varicosities in the pudendal vein?
They can lead to large hematomas and rapid healing of tears in the area following birth.
What is the vestibule in female anatomy?
A flattened smooth surface inside the labia.
What is the urethral meatus?
The external opening of the urethra.
What is the vaginal orifice?
The external opening of the vagina, typically covered by a thin membrane called the hymen in children.
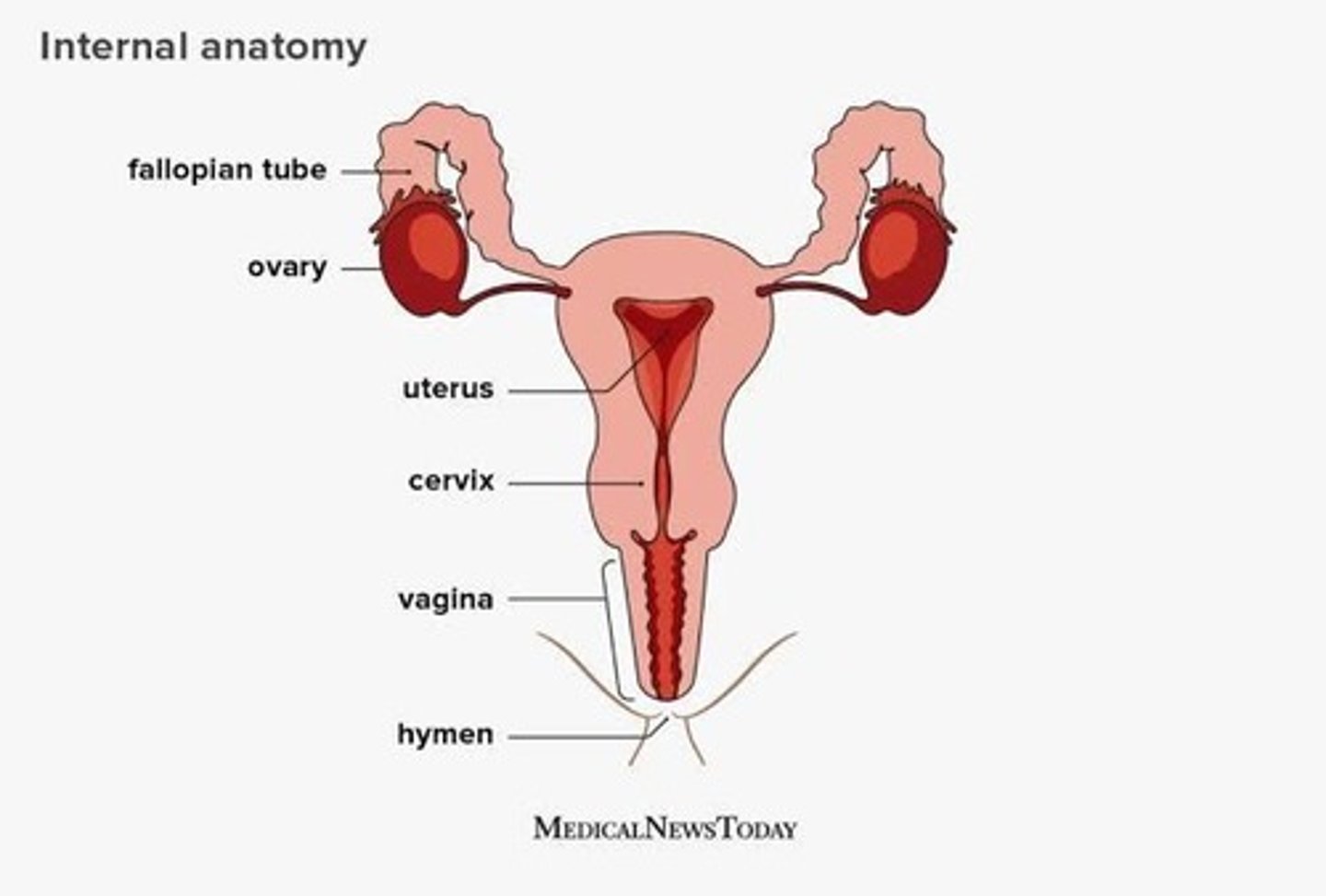
What are the main internal structures of the female reproductive system?
Fallopian tubes, ovaries, and uterus.
What is the size and shape of an ovary?
Approximately 4 cm long, 2 cm in diameter, and 1.5 cm thick, resembling the size and shape of an almond.
How do the ovaries change after puberty?
They grow larger and change from a smooth surface to a pitted grayish appearance due to scarring from ovulation.
What is unique about the ovaries compared to other pelvic structures?
They are not covered by peritoneum.
What are the two main functions of the ovaries?
To produce and discharge mature ova and to produce estrogen and progesterone, regulating menstrual cycles.
What is progesterone commonly referred to as?
The hormone of pregnancy.
What are the primary roles of estrogen in the female body?
It is responsible for the maturation and maintenance of secondary sexual characteristics, prevents osteoporosis, and reduces cholesterol levels.
How is estrogen used in menopausal women?
It is prescribed to prevent osteoporosis.
What are potential risks of long-term estrogen therapy?
It may contribute to breast cancer.
What is the structure and function of the fallopian tubes?
They are open at their distal ends to allow conception but can lead to peritoneal infection if germs spread from the uterus.
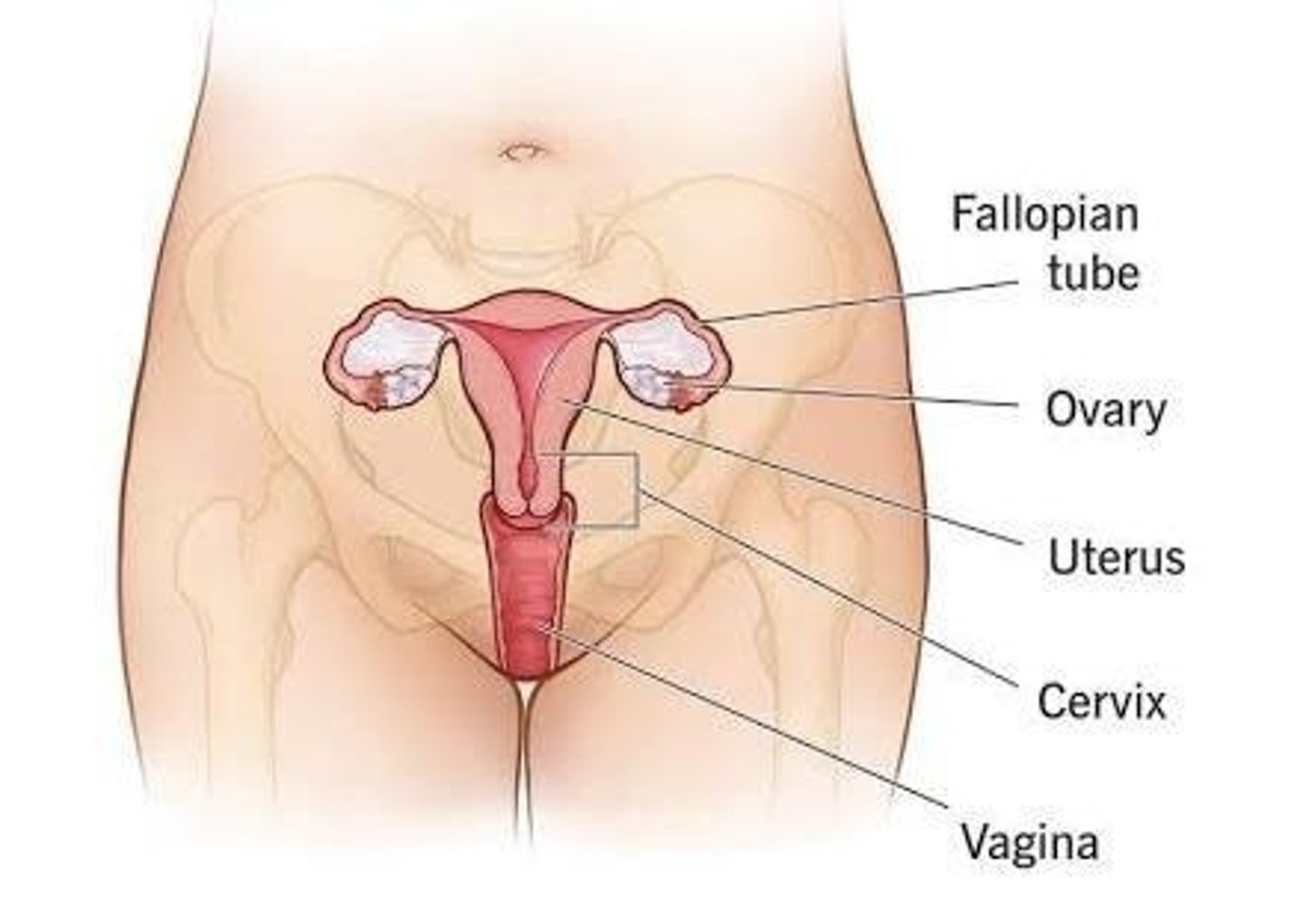
Describe the uterus in terms of its shape and location.
It is a hollow muscular, pear-shaped organ located in the lower pelvis, posterior to the bladder and anterior to the rectum.
What is the size of the uterus during childhood?
It is the size of an olive.
When does the size of the uterus begin to increase?
At around 8 years of age.
What is the maximum size of the uterus typically reached by age 17?
5 to 7 cm long, 5 cm wide, and the widest upper part is 2.5 cm deep, weighing about 60 grams.
What are the functions of the uterus?
To receive the ovum from the fallopian tube, provide a place for implantation, nourish the growing fetus, protect the fetus, and expel it from the woman's body.
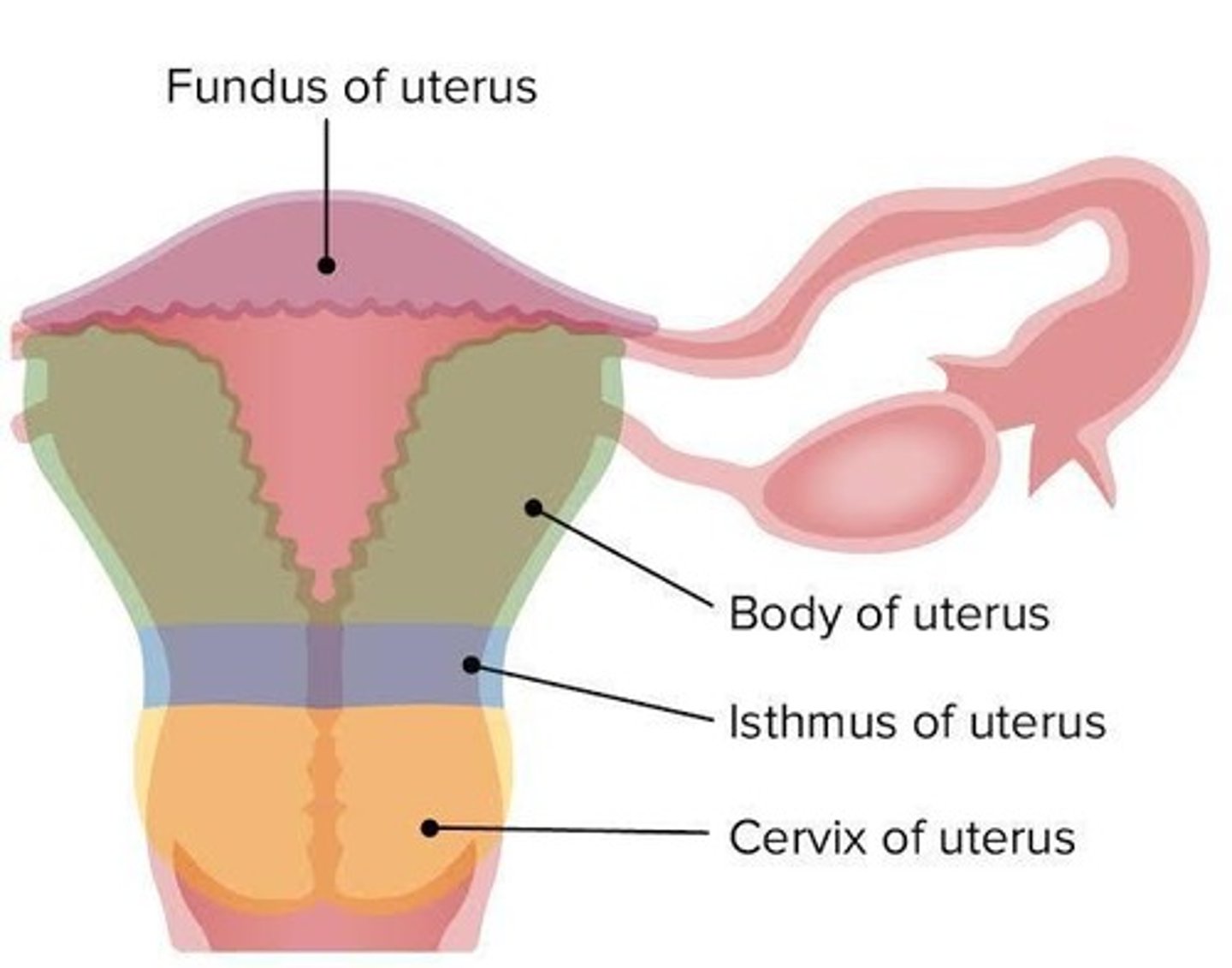
What are the three anatomical divisions of the uterus?
Body (corpus), Isthmus, and Cervix.
What is the function of the fundus of the uterus during pregnancy?
It expands to contain the growing fetus and is palpated to measure uterine growth and contractions.
What is the length of the isthmus of the uterus?
1-2 mm.
What is the role of the cervix in the female reproductive system?
It is the lowest portion of the uterus, approximately 2-5 cm long, and includes the central canal, internal cervix, and external cervix.
What are the two layers of the endometrium?
Basal layer (not influenced by hormones) and Glandular layer (influenced by estrogen and progesterone).
What is the function of the endocervix?
It secretes mucus to lubricate the cervix, aiding sperm passage and survival.
How much mucus can the cervical lining produce at peak estrogen levels?
700 ml per day.
What are the two layers of the uterus?
Myometrium (muscle layer) and Perimetrium (outer connective tissue layer).
What are the functions of the myometrium?
Constricts the tubal junction, holds the cervical os during pregnancy, and contracts to expel the fetus during delivery.
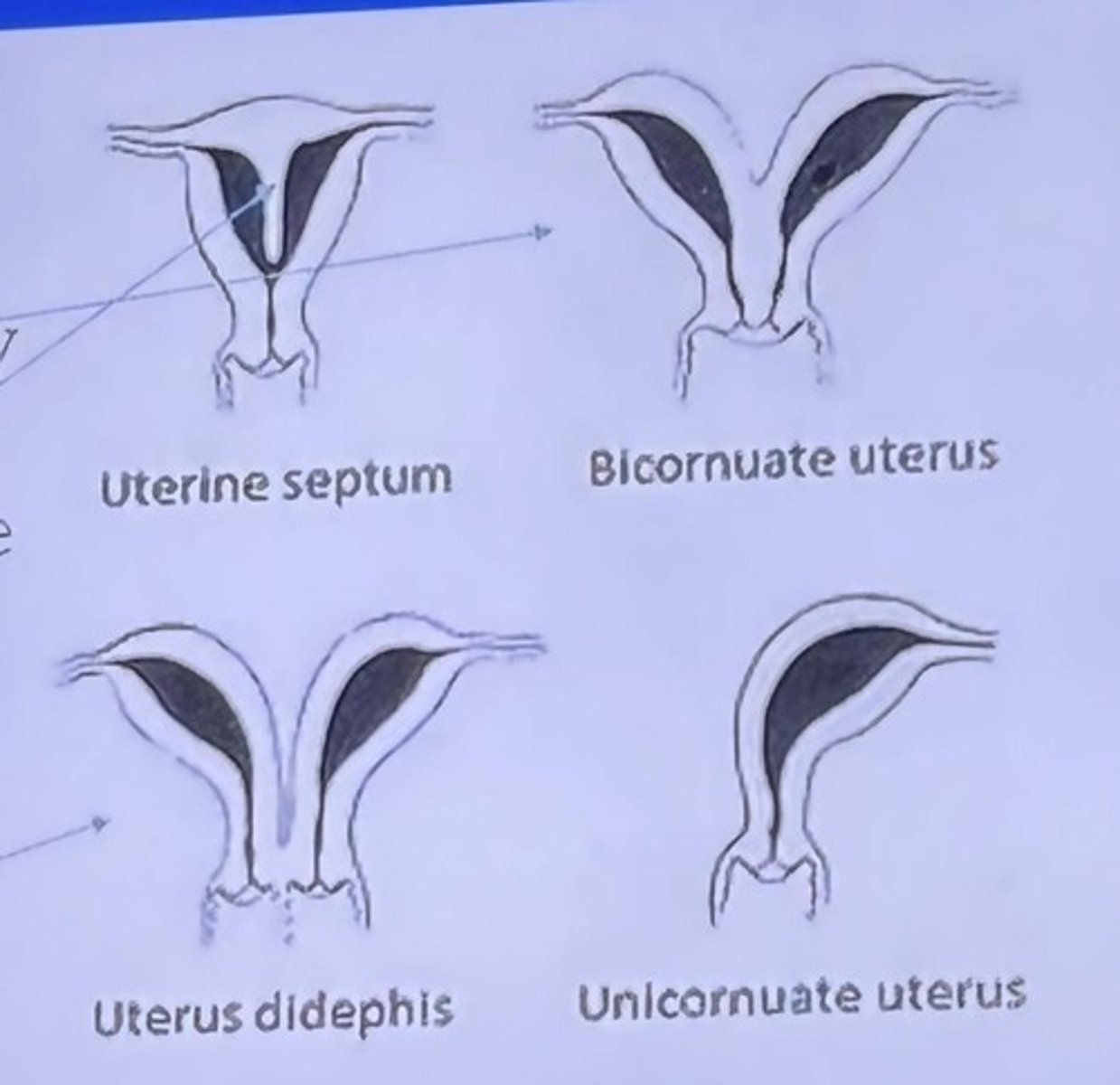
What are some deviations in the shape of the uterus?
Bicornuate uterus, septum dividing the uterus, and double uterus.
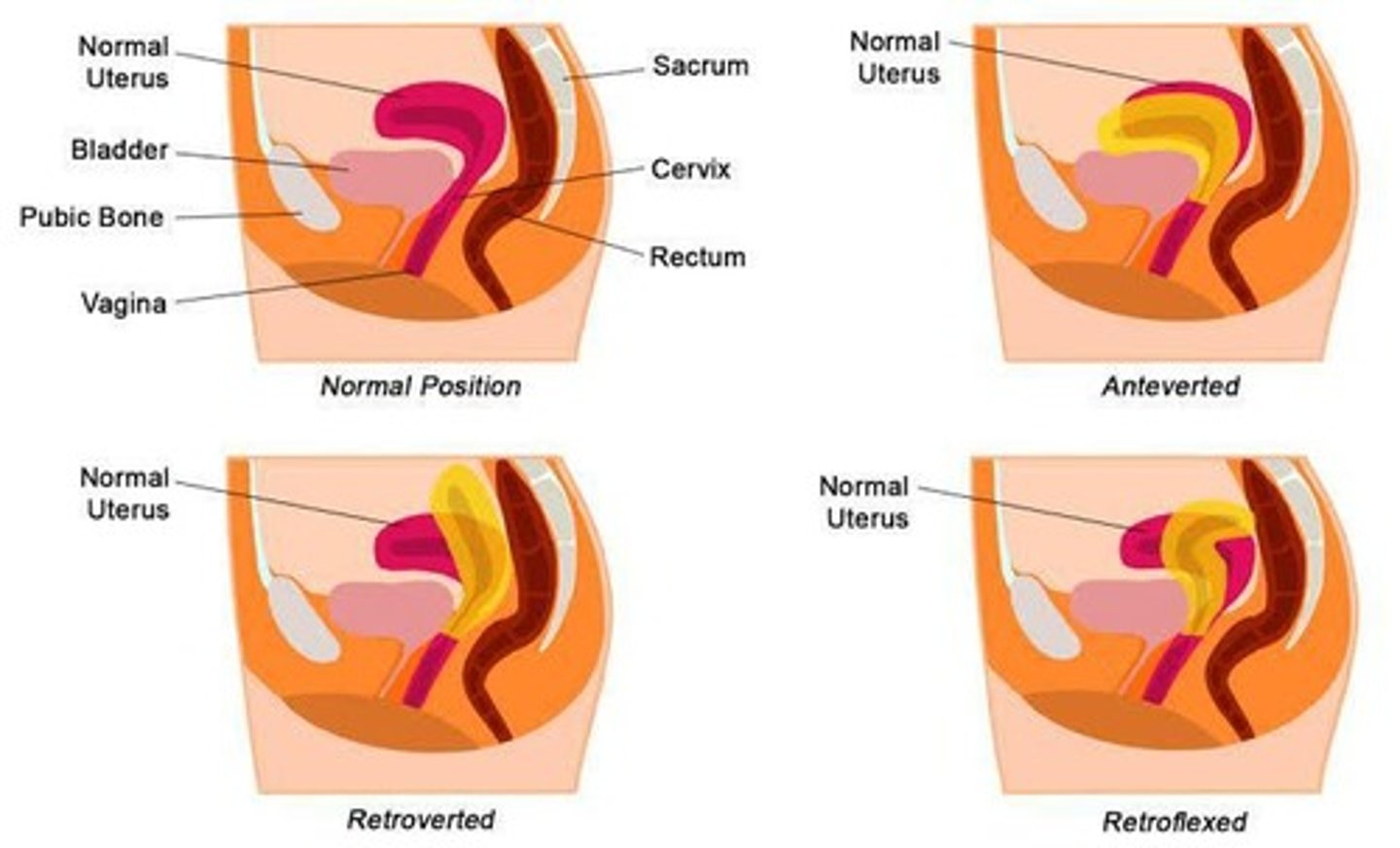
What are the deviations in the position of the uterus?
Anteversion (tipped forward), Retroversion (tipped back), Anteflexion (bent forward), and Retroflexion (bent back).
What is the vagina and its function?
A hollow, musculo-membranous canal that conveys sperm to the cervix and expands during childbirth.
What happens to the number of primitive follicles during maturation?
5-7 million are formed in utero, decreasing to about 2 million at birth, 500,000 at age 7, and 300,000 at age 22.
What occurs to the follicles by menopause?
None are left.
Where are the mammary glands located?
Anterior to the pectoral muscle.
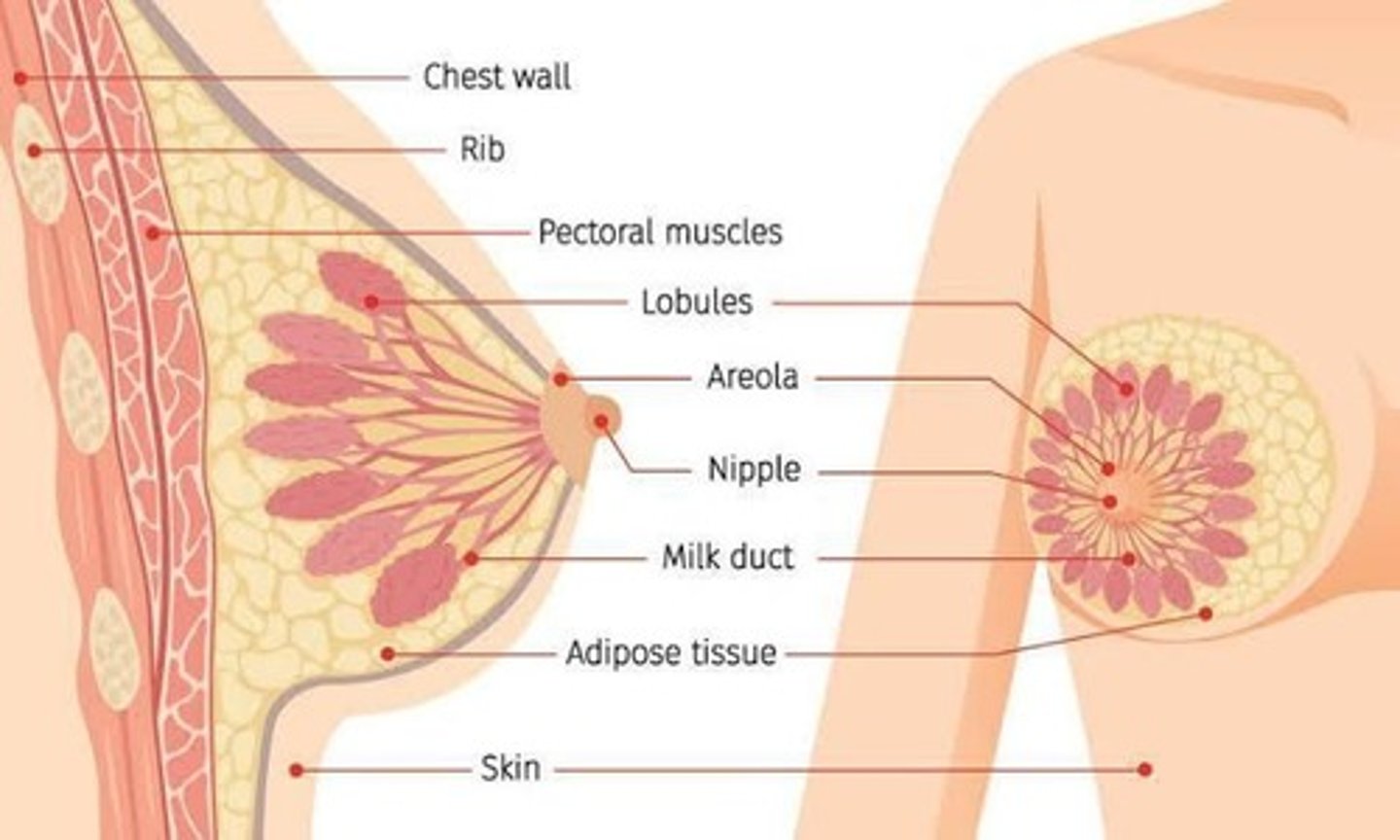
What triggers the release of oxytocin during breastfeeding?
Stimulation of the nipple.
What is the role of oxytocin in lactation?
It constricts milk gland cells to push milk into the ducts leading to the nipple.
What is the central canal of the cervix?
The central cavity of the cervix.
What is the external cervix?
The distal opening of the cervix to the vagina.
What is the significance of the cervical mucus in relation to sperm?
It provides a lubricated surface that decreases vaginal acidity, aiding sperm survival.
What is the function of the perimetrium?
It provides additional support and strength to the uterus.
What is the purpose of the folds of rugae in the vagina?
They allow for expansion during childbirth.
Where is milk produced and how is it delivered to the nipple?
Milk is produced in the acinar cell and delivered to the nipple by the lactiferous duct.
What surrounds the nipple and what is its approximate diameter?
The nipple is surrounded by a dark pigmented area called the areola, which is approximately 4 cm in diameter.
What are Montgomery's tubercles?
Sebaceous glands surrounding the areola.
What is the blood supply to the breast formed by?
The blood supply is profuse and formed by thoracic branches of the axillary, internal mammary, and intercostal arteries.
What is the menstrual cycle also known as?
The menstrual cycle is also termed the female reproductive cycle.
How can the menstrual cycle be defined?
It can be defined as episodic uterine bleeding in response to cyclic hormonal changes.
What is the purpose of the menstrual cycle?
To bring an ovum to maturity and renew a uterine tissue bed for potential fertilization.
What is menarche?
Menarche is the first menstrual period in girls, occurring as early as age 8 or 9 or as late as age 17.
What is the average age of onset for menarche?
The average age of onset for menarche is 12 or 13 years, with a range of 9 to 17 years.
What is the average interval between menstrual cycles?
The average interval between cycles is 28 days, but cycles of 23 to 35 days are not unusual.
What is the average duration of menstrual flow?
The average duration of menstrual flow is 2-7 days, with a range of 1-9 days.
How much menstrual flow is considered heavy bleeding?
Saturating a pad or tampon in less than an hour is considered heavy bleeding.
What is the typical color of menstrual flow?
The typical color of menstrual flow is dark red, consisting of blood and endometrial cells.
What hormone does the hypothalamus release to initiate menstruation?
The hypothalamus releases gonadotropin-releasing hormone (GnRH) or luteinizing hormone-releasing hormone (LHRH).
How does estrogen affect GnRH release?
The presence of estrogen represses the release of GnRH.
How does the sensitivity of the hypothalamus to estrogen change from childhood to puberty?
In childhood, the hypothalamus is sensitive to small amounts of estrogen, repressing GnRH release; during puberty, it becomes less sensitive and initiates GnRH release.
What hormones does the anterior pituitary gland produce in response to GnRH?
The anterior pituitary gland produces follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
What is the role of FSH in the menstrual cycle?
FSH is active early in the cycle and is responsible for the maturation of the ovum.