MCAT Biology - The Cardiovascular System
1/131
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
132 Terms
humoralism
the human body is composed of four fluids or substances called humors: black bile, yellow bile, phlegm, and blood
health is balance of these four fluids; illness is caused by an imbalance
bealieved and practiced as late as 19th c. from Greak/ROman physicians
bloodletting
physicians would withdraw significant amounts of blood from their patients to restore balance to the four humors; drawing blood from major veins/arteries, scarificator devices, leeches
modern medical uses of leeches
in microsurgery to help prevent blood coagulation
in reconstructive surgery to stimulate circulation to the reattached tissue
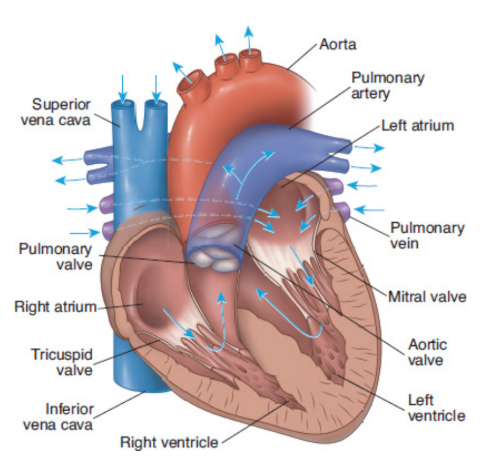
cardiovascular system
consists of a muscular four-chambered heart, blood vessels, and blood
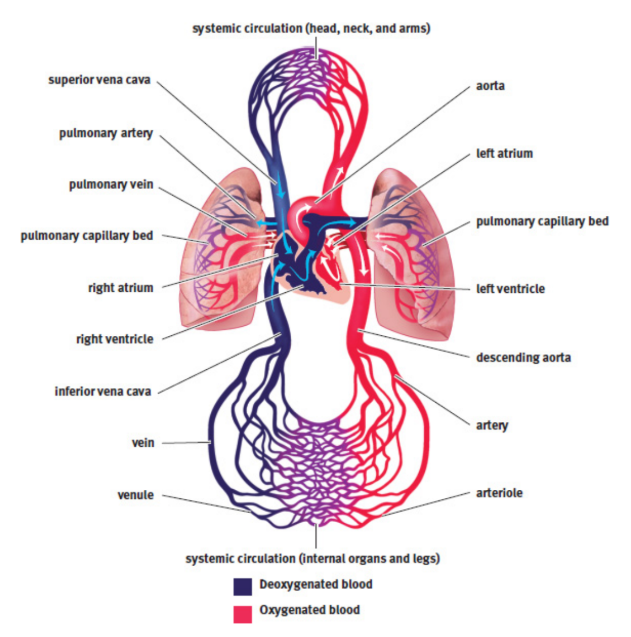
heart
acts as (two) pump(s), distributing blood through the vasculature; four-chambered structure composed predominantly of cardiac muscle; left side of the heart is more muscular than the right side of the heart
vasculature/blood vessels
arteries, capillaries, and veins
blood
connective tissues that carries oxygen and nutrients around the body
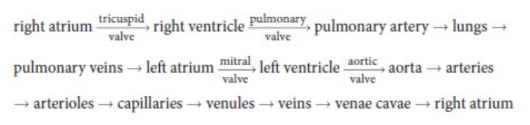
pulmonary circulation
first pump; right side of the heart accepts deoxygenated blood returning from the body and moves it to the lungs by way of the pulmonary arteries
systemic circulation
second pump; the left side of the heart, which receives oxygenated blood from the lungs by way of the pulmonary veins and forces it out to the body through the aorta
atria
thin-walled structures where blood is received; contract to push blood into the ventricles
venae cavae
deoxygenated blood entering the right atrium
pulmonary veins
oxygenated blood entering the left atrium
ventricles
contract to send blood out of the heart; more muscular
pulmonary arteries
blood from right ventricle to lungs
aorta
blood from left ventricle to systemic circulation
atrioventricular valves
separates atria from ventricles
semilunar valves
ventricles are separated from the vasculature; three leaflets
tricuspid valve
between right atrium and the right ventricle; three leaflets
mitral/bicuspid valve
between the left atrium and the left ventricle; two leaflets
circulatory valves
allow the heart muscle to create the pressure within the ventricles necessary to propel the blood forward within the circulation, while also preventing backflow of blood
pulmonary valve
separates the right ventricle from the pulmonary circulation
aortic valve
separates the left ventricle from the aorta
SA node
Impulse initiation; generates 60–100 signals per minute without requiring any neurological input; small collection of cells is located in the wall of the right atrium; depolarization wave spreads from the SA node, causes the two atria to contract simultaneously
atrial kick
increase in atrial pressure during atrial systole that forces a little more blood into the ventricles; accounts for about 5–30 percent of cardiac output
AV node
sits at the junction of the atria and ventricles; signal is delayed here toallow the ventricles to fill completely before they contract
bundle of His
after AV node; embedded in the interventricular septum (wall)
Purkinje fibers
distribute the electrical signal through the ventricular muscle
intercalated discs
connect muscle cells; contain many gap junctions directly connecting the cytoplasm of adjacent cells; allows for coordinated ventricular contraction
electrical conduction system of heart
Cardiac muscle has myogenic activity, meaning that it can contract without any neurological input. The SA node generates about 60–100 beats per minute, even if all innervation to the heart is cut. The neurological input to the heart is important in speeding up and slowing the rate of contraction, but not generating it in the first place.
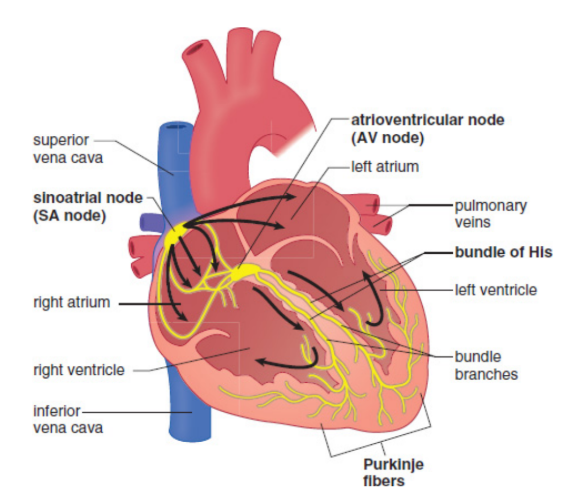
electrocardiogram (ECG or EKG)
heart’s electrical impulses can be detected on the body’s surface by placing electrodes on the skin on opposite sides of the heart; incredibly powerful tools for assessing the status of a patient’s heart

circulation
the flow of blood through the body
vagus nerve
parasympathetic signals slow down heart rate
systole
ventricular contraction and closure of the AV valves occurs and blood is pumped out of the ventricles; Contraction of the ventricles generates a higher pressure
diastole
ventricles are relaxed, the semilunar valves are closed, and blood from the atria fills the ventricles; relaxation of atria causes the pressure to decrease
The Cardiac Cycle
normal events of one heartbeat, including pressures in the left atrium, left ventricle, and aorta; left ventricular volume; normal and pathologic heart sounds; and an EKG
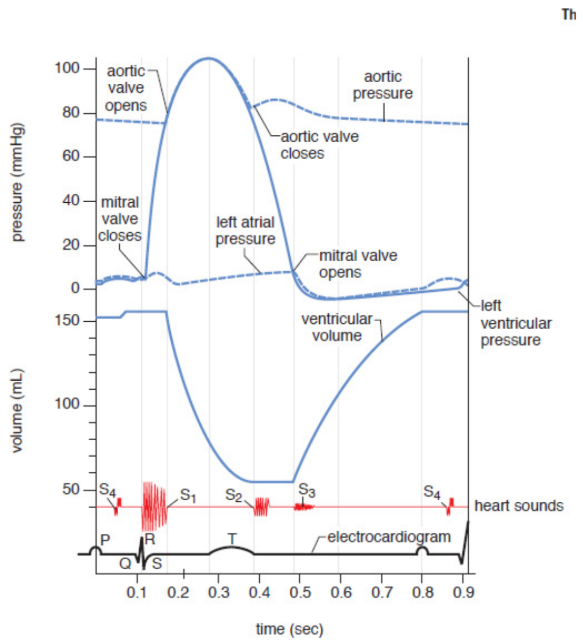
cardiac output
total blood volume pumped by a ventricle in a minute; same in each; connected in series; product of heart rate and stroke volume
about 5 liters per minute
heart rate (HR)
beats per minute
stroke volume (SV)
volume of blood pumped per beat
lub-dub
first sound, S1, is produced when the two AV valves close at the start of systole to prevent backflow into the atria
second sound, S2, is produced when the two semilunar valves close at the end of systole to prevent backflow into the ventricles
extra sounds - stiffness of the heart muscle or high blood pressure
Heart murmurs
so loud as to be audible without a stethoscope, may arise when the valves malfunction and become either narrow and stiff or wide and floppy, resulting in abnormal flow patterns across the valve
ventricular tachycardia
very rapid rate of ventricular contraction; cannot properly fill with blood and, paradoxically, stops pumping blood despite its fast rate. Systemic pressures drop precipitously. Death will result unless the heart is forced out of this abnormal rhythm.
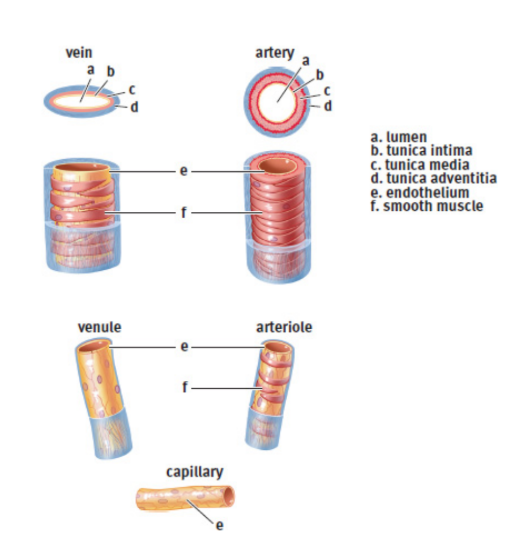
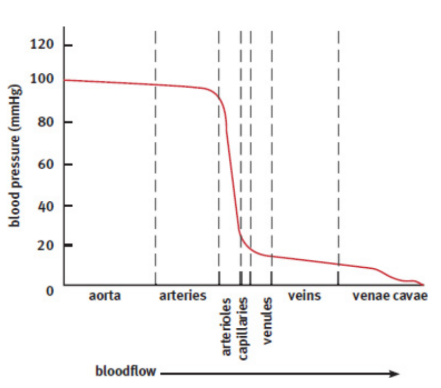
arteries
Blood travels away from the heart; Most arteries contain oxygenated blood (except pumonary and umbilical); highly muscular and elastic, creating tremendous resistance; maintains a high pressure and forces blood forward
arterioles
smaller, muscular arteries; connect arteries to capillaries
capillaries
vessels with a single endothelial cell layer and are so small that red blood cells must pass through the capillaries in a single-file line; perfuse the tissues; allows easy diffusion of gases (O2 and CO2), nutrients (most notably, glucose), wastes (ammonia and urea, among others), hormones
venules
small veins; connect capillaries to the larger veins of the body
veins
Blood enters the heart; usually deoxygenated blood (except pulmonary and umbilical); less recoil than arteries; stretch to accommodate larger quantities of blood; large ones contain valves to push the blood forward and prevent backflow
endothelial cells
maintain the vessel by releasing chemicals that aid in vasodilation and vasoconstriction; allow white blood cells to pass through the vessel wall and into the tissues during an inflammatory response; release certain chemicals when damaged that are involved in the formation of blood clots to repair the vessel and stop bleeding
heart attack / myocardial infarction
lack of bloodflow through the coronary arteries, which results in decreased oxygen delivery to the cardiac muscle itself
β-blocker
blocks the sympathetic stimulation of the heart, resulting in lower heart rate and lower contractility; oxygen demand is diminished, which helps to prevent further damage to cardiac tissue
bruise / contusion
capillaries are damaged, blood can leave the capillaries and enter the interstitial space
varicose veins
distended where blood has pooled
pulmonary emboli (thromboemboli)
clots that block segments of the pulmonary arteries and produce rapid, labored breathing and chest pain; may be fatal
deep vein thrombosis
may form in the deep veins of the legs as a result of injury, inactivity (blood stasis), or a hypercoagulable state (a tendency for the blood to clot excessively)
heparin/warfarin
prevent clots
blood flow through heart
RA →RV→lungs→LA→LV→body and back
portal systems
blood will pass through two capillary beds in series before returning to the heart
hepatic portal system
blood leaving capillary beds in the walls of the gut passes through the hepatic portal vein before reaching the capillary beds in the liver
hypophyseal portal system
blood leaving capillary beds in the hypothalamus travels to a capillary bed in the anterior pituitary to allow for paracrine secretion of releasing hormones
renal portal system
blood leaving the glomerulus travels through an efferent arteriole before surrounding the nephron in a capillary network called the vasa recta
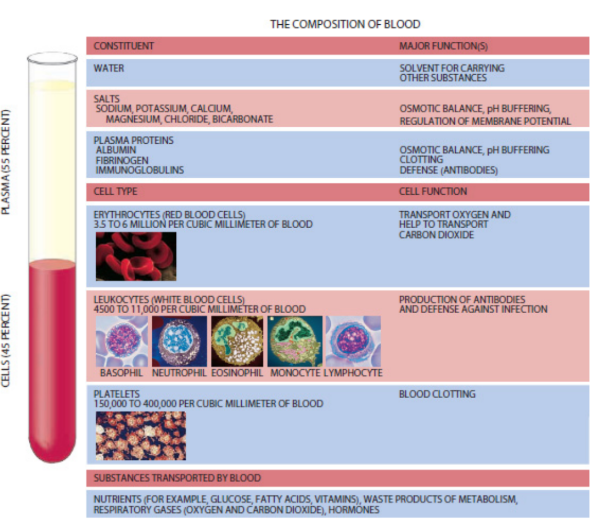
Plasma
liquid portion of blood, an aqueous mixture of nutrients, salts, respiratory gases, hormones, and blood proteins; 55% of blood
serum (pl. sera)
Plasma can be further refined via the removal of clotting factors and fibrinogens; used in a variety of medical testing procedures such as antibody testing and blood typing
hematopoietic stem cells
originate in the bone marrow; orgin of all blood cells
erythrocyte / red blood cell
specialized cell designed for oxygen transport; contains about 250 million molecules of hemoglobin; biconcave (no nucleus, mitochondria or other organelles) - fits through capillaries and increases surface area; live for 120 days in the bloodstream before cells in the liver and spleen phagocytize them for their parts.
adult hemoglobin (HbA)
protein complex made of four cooperative subunits, each of which has a prosthetic heme gorup that can bind a molecule of oxygen at the central iron ion; measured in grams per deciliter (13.5 - 17.5 for males, 12.0 - 16.0 for females); also has low affinity for CO2 and high affinity for protons (H+)
Hematocrit
measure of how much of the blood sample consists of red blood cells, given as a percentage; 41 - 53% for males and 36 - 46% for females.
Leukocytes / white blood cells
comprise less than 1 percent of total blood volume; about 4,500–11,000 leukocytes per microliter of blood; crucial part of the immune system, acting as our defenders against pathogens, foreign cells, cancer, and other materials not recognized as self
granulocytes
granular leukocytes; contain cytoplasmic granules that are visible by microscopy that contain a variety of compounds that are toxic to invading microbes, relased through exocytosis; involved in inflammatory reactions, allergies, pus formation, and destruction of bacteria and parasites
neutrophils
type of phagocytic granulocyte
eosinophils
type of granulocyte; one of the immune system components responsible for combating multicellular parasites and certain infections in vertebrates
basophils
largest and least common type of granulocyte
agranulocytes
do not contain granules that are released by exocytosis
lymphocytes
important in the specific immune response; some act as primary responders against an infection, while others function to maintain a long-term memory bank of pathogen recognition; vaccination
specific immune response
the body’s targeted fight against particular pathogens, such as viruses and bacteria
B-cells
lymphocytes that mature in the bone marrow; responsible for antibody generation
T-cells
lymphocytes that mature in the thymus; kill virally infected cells and activate other immune cells
monocytes
phagocytize foreign matter such as bacteria
macrophages
monocytes that enter an organ
microglia
macrophages in CNS
Langerhans cells
macrophages in skin
osteoclasts
macrophages in bone
thrombocytes / platelets
cell fragments or shards released from megakaryocytes; assist in blood clotting; present in high concentrations (150,000–400,000 per microliter of blood); come into contact with exposed collagen → release their contents and begin to aggregate
megakaryocytes
bone marrow cells that shatter into platelets
hematopoiesis
production of blood cells and platelets; triggered by a number of hormones, growth factors, and cytokines
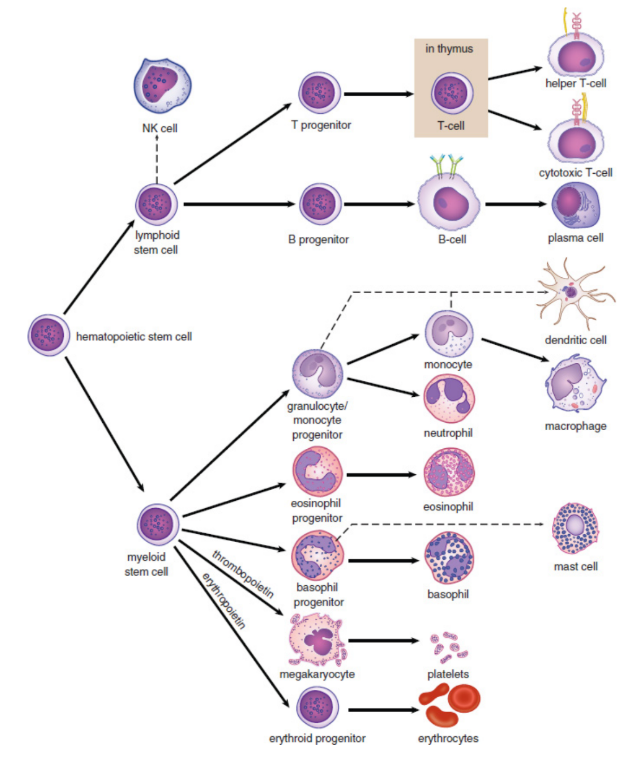
erythropoietin
secreted by the kidney; stimulates mainly red blood cell development
thrombopoietin
secreted by the liver and kidney; stimulates mainly platelet development
antigens
surface proteins that identify a cell; any specific target (usually a protein) to which the immune system can react
ABO Antigens
comprised of three alleles for blood type; A/IA and B/IB are codominant, O/i is recessive; dominant allles express self-antigen and produce anti-other antibodies
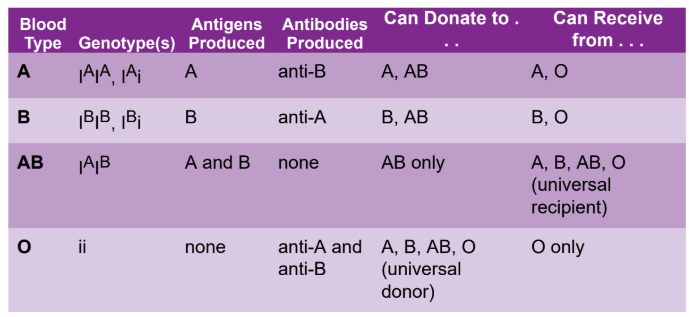
universal donors
type O; blood will not cause ABO-related hemolysis in any recipient
universal recipients
type AB; receive blood from all blood types: no blood antigen is foreign to individuals who have AB blood, so no adverse reactions will occur upon transfusion
Antibodies
created in response to an antigen, and they specifically target that antigen
Rh factor
first described in rhesus monkeys; surface protein expressed on red blood cells; Rh-positive (Rh+) or Rh-negative (Rh-) refers to the presence or absence of a specific allele called D; can also be indicated with a plus or minus superscript on the ABO blood type; autosomal dominant inheritance
erythroblastosis fetalis
if mother is Rh- and first baby is Rh+, the risk exists for every subsequent RH+ child that maternal anti-Rh antibodies can cross the placenta and attack the fetal blood cells, resulting in hemolysis of the fetal cells
sphygmomanometer
measure the gauge pressure in the systemic circulation, which is the pressure above and beyond atmospheric pressure (760 mmHg at sea level)
Blood pressure
measure of the force per unit area exerted on the wall of the blood vessels; expressed as a ratio of the systolic (ventricular contraction) to diastolic (ventricular relaxation) pressures; normal between 90/60 and 120/80; regulated using baroreceptors in the walls of the vasculature
ΔP = CO × TPR
where ΔP is the pressure differential across the circulation, CO is the cardiac output, and TPR is the total peripheral (vascular) resistance
hypertension
high blood pressure; pathological state that may result in damage to the blood vessels and organs
Baroreceptors
specialized neurons that detect changes in the mechanical forces on the walls of the vessel
blood pressure low → sympathetic nervous system → vasoconstriction → increasing the blood pressure
blood pressure high → sympathetic impulses decrease → vasodilation→ lowering the blood pressure
chemoreceptors
sense when the osmolarity of the blood is too high, possible dehydration
promotes the release of ADH/vasopressin → increasing blood volume and pressure, diluting blood
renin–angiotensin–aldosterone system
Low perfusion to the juxtaglomerular cells of the kidney → aldosterone release → increases the reabsorption of sodium → by extension, water → increasing the blood volume and pressure
atrial natriuretic peptide (ANP)
specialized atrial cells secrete hormone; aids in the loss of salt within the nephron, acting as a natural diuretic with loss of fluid
concentration gradients
one side of a semi-permeable mebrane has a higher concentration of a given substance than the other