Dementia
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
intellectual, loss, aphasia
Dementia
-Progressive impairment in ____________ function with ____ of memory and at least one other cognitive deficit like _______, apraxia, or agnosia
progressive, delirium, aging, executive, loss, word, visuospatial
Clinical Presentation: Background
-___________ neurocognitive decline
-Rule out acute _________, normal ______, and pseudo dementia
-________ dysfunction → easy distractibility, impulsivity, mental inflexibility, concrete thought, slowed processing speed, poor planning and organization, or impaired judgement
-Short-term memory ____
-Word-finding difficulty
-Apathy
-__________ dysfunction
-Apraxia
cognitive, mild, biased, impaired, quantifies
Neuropsychological Assessment
-Detecting _______ impairment → Folstein Mini MSE, mini-cog, Montreal Cognitive Assessment (MoCA)
-Important limitations of standard test → insensitive to ____ cognitive impairment, may be _______ negatively by the presence of language or attention problems, and don’t correlate with functional capacity
-A neuropsychiatric evaluation to enhance localization by defining ________ cognitive domains, _________ the degree of impairment
cognitive, B12, TSH, HIV
Diagnostic Testing
-Should be measured for any patient with _________ symptoms → serum levels of Vitamin ___, free T4 and TSH, CBC, CMP, lipid panel
-Consider VRDL/RPR and ___ tests
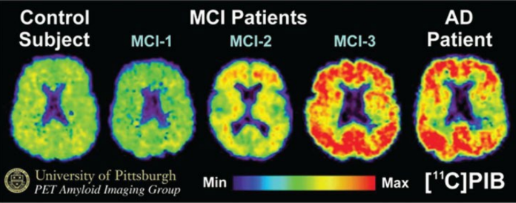
new, without, PET, specific, Alzheimer’s, beta-amyloid, decline
Diagnostic Imaging
-Indicated in any patient with a ___, progressive cognitive complaint → brain imaging with MRI/CT ________ contrast
-PET with FDG → doesn’t confirm or exclude any _______ cause of dementia. May be useful in discriminating _________’_ disease vs frontotemporal dementia
-PET imaging with radiolabeled ligand for ____-_______ is highly sensitive to amyloid pathology. May provide positive evidence for Alzheimer disease in a patient with cognitive _______
increasing, 65, younger
Alzheimer Disease (AD)
-Most common dementia, present in up to 50% of patients
-The greatest known risk factor is __________ age
Majority of patients with Alzheimer’s under __ have younger-onset Alzheimer’s disease
-200,000 Americans under 65 have _______-onset Alzheimer Disease
-Etiology is not very clear, but there may be a family component
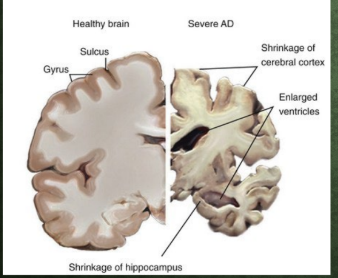
shrinkage, ventricles
Alzheimer’s Dementia: Pathophysiology, pt 1
-__________ of cerebral cortex → temporal, frontal, parietal
-Enlarged ___________ → hydrocephalus ex vacuo
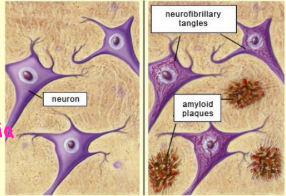
plaques, beta-amyloid, APP, between, signaling, angiopathy, fibers, tau, inside, apoptosis
Alzheimer’s Disease: Pathophysiology, Pt. 2
-________ and tangles damage and destroy nerve cells
Plaques are deposits of a protein fragment called ____-______, which is a byproduct of ___ degradation.
Builds up in the space ________ nerve cells, creating issues with neuron to neuron __________
Builds up around brain vessels (amyloid _______)
-Tangles are twisted _______ of a protein called ___
Builds up ______ cells
Poor signaling within neuron → __________, for the neuron cannot compensate
remembering, newly, learning, entorhinal, temporal, hippocampus, neocortex, acetylcholine
Alzheimer Disease (AD)
-The most common early symptom of Alzheimer’s is difficulty ____________ _____ learned information
-Alzheimer changes typically begin in the part of the brain that affects _________
-Begins in the __________ region of the medial _______ lobe, spreading to the ____________ later on in progression
-Then moves to the lateral and posterior temporal and parietal _________, causing decreased ___________ neurotransmitter

disrupts, planning, confusion, speaking, decreased, mood
10 Early Signs of Alzheimer Disease
Memory loss that _______ daily life
Challenges in ________/solving problems
Difficulty completing familiar tasks
___________ with time/place
Trouble understanding visual images/spatial relationships
New problems with words in __________/writing
Misplacing things/can’t retrace steps
__________/poor judgement
Withdrawal from work/social activities
Changes in ____ and personality
disorientation, confusion, suspicions, loss, swallowing
Alzheimer Disease Progression
-As it advances through the brain, it leads to:
____________
Mood/behavior changes
Deepening __________ about events
Time and place
Unfounded ___________ about family, friends, and professional caregiver
More serious memory ____ and behavior changes
Difficulty speaking, ___________, and walking
Mild
What stage of Alzheimer’s is this?
-Problems coming up with the right word or name
-Trouble remembering names when introduced to new people
-Challenges performing tasks in social or work settings
-Forgetting material that one has just read
-Losing or misplacing a valuable object
-Increasing trouble with planning or organizing
Moderate
What stage of Alzheimer’s Disease is this?
-Forgetfulness of events or about one’s own personal history
-Feeling moody or withdrawn, especially in socially or mentally challenging situations
-Being unable to recall their own address or telephone number
-Confusion about where they are or what day it is
-The need for help choosing proper clothing
-Trouble controlling bladder and bowels
-Changes in sleep patterns, such as sleeping during the day
-An increased risk of wandering and becoming lost
-Personality and behavioral changes
Severe
What stage of Alzheimer’s Disease is this?
-Need round-the-clock assistance with daily activities and personal care
-Lose awareness of recent experiences as well as of their surroundings
-Experience changes in physical abilities
-Have increasing difficulty communicating
-Become vulnerable to infections
cholinesterase, progression, symptomatic, diarrhea, cardiac, EKG
Alzheimer Disease Treatment: First Line Therapy
-_____________ inhibitors are first-line therapy for Alzheimer’s disease
Donepezil, rivastigmine, galantamine
-They do not prevent disease ______________
-Provide modest, ______________ treatment for cognitive dysfunction
-ADRs → nausea and ________ are common. Syncope and _______ dysrhythmia are uncommon but more serious. Order ___ before and after starting therapy in patients with cardiac disease or a history of syncope
Memantine, combination, neurons, vascular
Alzheimer Disease: Treatment
-_____________ → NMDA receptor antagonist that works well in _____________ with cholinesterase inhibitors
-Moderate to severe disease → can restore physiologic function of _________ to improve symptoms, as well as protects from further damage (especially in __________ dementia)
amyloid, beta, mild, modest
Alzheimer Disease Treatment
-_________ targeted therapies → Lecanamab, Donanemab
-Recombinant monoclonal antibodies directed against amyloid ____
-Indicated only in patients with ____ cognitive impairment/mild dementia
-Efficacy is ______; need to weigh risks of ADR
E, functional, cognitive
Alzheimer’s Disease Treatment: Antioxidants
-Vitamin _ at a dose of 2000 IU per day confers a modest benefit in delaying __________ progression in patients with mild to moderate
-Selegiline has some benefit in the treatment of _________ benefits ± behavior and mood
admission, avoided, delirium
Dementia Patients Need to Stay Home
-_____________ to the hospital should be _________ due to increased risk of developing hospital-acquired __________
behavioral, Citalopram, Trazodone, antihistamines, apathy
Alzheimer Dementia: Treatment of Mood and Behavioral Disturbance
-Agitation
___________ interventions are the first line → reorientation and distraction from anxiety-provoking stimuli
____________ or low doses of an atypical antipsychotic → caution in patient’s with a fall risk
-Insomnia
_____________ at bedtime prn
Don’t use _____________ or benzodiazepine medications → can worsen cognition and precipitate delirium
-______
Psychostimulants may help, but may also increase CV risk and agitation
post-stroke, speaking, headache, numbness
Vascular Dementia: Background
-Sudden ____-______ change in thinking and perception may include:
Confusion
Disorientation
Trouble _________ or understanding speech
Physical stroke symptoms (sudden _________)
Difficulty walking
Poor balance
___________ or paralysis on one side of the face or body
Asian, intracranial, increasing, hypertension
Vascular Dementia
-Vascular dementia is more common in _______ countries due to higher prevalence of ____________ atherosclerosis
-Rates of vascular dementia are __________ in developing countries due to vascular risk factors like ____________, hypercholesterolemia, and diabetes mellitus
underlying, Alzheimer’s
Vascular Dementia Management
-Treat the _________ disease → HTN, hyperlipidemia, or diabetes
-No drugs specifically for vascular dementia → _________’_ drugs do not show benefit
visual, Parkinsonism, rapid, sleepiness
Dementia with Lewy Bodies (DLB)
-______ hallucinations
-_____________
-Fluctuating alertness
-Neuroleptic sensitivity
-_____ eye movement (REM) sleep behavior disorder (RBD)
-Hyposomnia and excessive daytime ____________
-Delusions related to persecution, invasion, and person or place identity
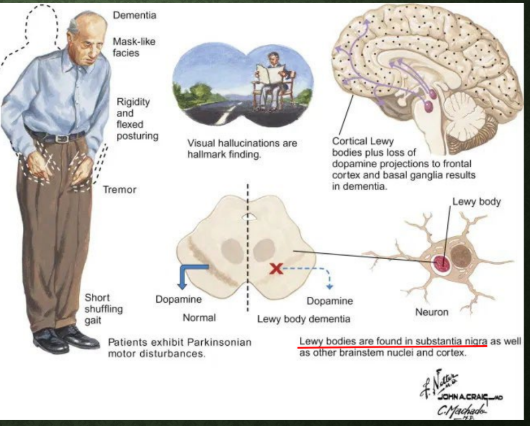
brainstem, substantia, orthostatic, parkinsonism, intraneuronal, synuclein, PAS, antibodies
Dementia with Lewy Bodies: Pathophysiology
-Both PDD and DLB may be accompanied or preceded by symptoms referable to __________ pathology below the ________ nigra:
Constipation, _________ lightheadedness (distinguish from __________ if present), depression/anxiety, and REM sleep behavior disorder
-Neuropathy: Lewy bodies are ____________ cytoplasmic inclusions composed of abnormal a-__________ protein
Intraneuronal cytoplasmic inclusions stain with periodic acid-Schiff (___)
Now identified with __________ to the presynaptic protein, a-synuclein
behavioral, Cholinesterase, parkinsonism, atypical, melatonin
Dementia with Lewy Bodies: Management
-Symptomatic management (no disease modifying effects)
Start with __________ interventions
___________ inhibitors are first-line therapy
± Memantine
-Don’t use antipsychotics → exacerbation of __________, confusion
If must be used only give _________ in tiny doses
-REM sleep disorder → low dose ________ or clonazepam
behavior, comprehending, memory, judgement, behavior
Frontotemporal Dementia: Background
-Younger patients (40-60 years)
-Deterioration in __________, personality, and/or difficulty with producing or ___________ language
-Less likely to begin with _______ problems
-More likely to present with difficulties with ___________, mood, executive control, movement, and __________
tau, TDP43
Frontotemporal Dementia: Etiology
-There are a number of different diseases that cause frontotemporal degenerations
-The two most prominent are:
Group of brain disorders involving the protein ___
Group of brain disorders involving the protein called _____
These are why PET scans can be helpful
behavior, SSRI, antipsychotic, cholinesterase
Frontotemporal Dementia Management
-No current FDA approved treatment
-________ therapy → speech and psychiatric behavior therapy
-Pharmacologic symptom management → ____ for behavior problems, atypical __________ for agitation
-____________ inhibitors are not given for frontotemporal dementia, for they may worsen behavioral symptoms
MDD, caudate, personality, progressive, HIV, liver
Additional Differential Diagnoses to Consider
-Pseudodementia → often co-existing ___
-Huntington’s Disease (______ degeneration) → progressive dementia with _________ changes and choreoathetosis
-Creutzfeldt-Jacob Disease → rapidly __________ dementia
-AIDS Dementia Complex → dementia and focal neurological symptom in ___+ person
-Wilson’s Disease → executive dementia with psychotic disturbances, movement disorder and _____ dysfunction
quickly, months, prion, Hashimoto, paraneoplastic
Rapidly Progressive Dementia
-When dementia develops ________, with obvious decline over a few weeks to a few ______, we need to rule out the following:
(1) _____ disease
(2) Infection
(3) Toxins
(4) Neoplasms
(5) Autoimmune/inflammatory disease → corticosteroid-response (__________) encephalopathy, antibody-mediated _____________ syndromes