Fielding Chapter 11: Fluid Overload
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
What does the presence of fluid overload require?
Either excessive fluid administration or inadequate renal excretion
Fluid Overload in Renal Failure
Kidneys may be unable to remove the required amount of fluid from the extracellular fluid volume (ECFV) to maintain normal water balance
Most commonly occurs due to a decreased GFR
Less commonly, GFR may be normal but the kidneys eliminate an inappropriately low amount of water
Conditions Where Renal Function is Adequate but the Kidneys are “Tricked” Into Allowing Fluid Overload
Increased capillary permeability, hypoproteinemia, changes in interstitial compliance, heart failure
In increased capillary permeability, increased fluid accumulates within the interstitium and ECFV and total body water (TBW) will gradually exceed normal volumes but intravascular volume may be decreased or normal so the kidneys do not perceive a fluid overload
In heart failure, the kidneys perceive that additional intravascular volume is need in order to maintain cardiovascular function and this volume is maintained despite the excessive total body water and extracellular fluid volumes
What are risk factors for fluid overload?
Hypoproteinemia
Heart failure
Renal failure
Systemic inflammation
Blood product administration
Hypoproteinemia and Fluid Overload
Many conditions that result in hypoproteinemia are also associated with systemic inflammation
Difficult to delineate the contribution of hypoproteinemia, increased vascular permeability, and interstitial matrix compliance changes
Albumin concentrations less than 1-1.5 g/dL or total protein concentrations less than 4.0 g/dL have been anecdotally implicated as a threshold for edema formation in horses, there is no research to support these conclusions
In cases with hypoproteinemia where IV fluid administration will be initiated, the risk of edema formation may be higher
In cases where edema is present, identification of hypoproteinemia should not exclude the search for other causes contributing to a state of fluid overload
Renal Failure and Fluid Overload
Patients with compromised renal function will be at increased risk for fluid overload if they are unable to excrete the quantity of fluid that is being administered
Acute kidney injury is recognized with as little as a 0.3 mg/dl increase in serum creatinine concentrations so a single measurement of creatinine at the middle or upper end of a normal range may still be associated with renal insufficiency
Fractional excretion of sodium may be another means for identifying more subtle changes in renal function and patients at higher risk for fluid overload
Systemic Inflammation and Fluid Overload
Systemic inflammatory response can cause changes in renal function, cardiac function, capillary permeability, interstitial compliance, and plasma protein concentrations that can lead to fluid overload
Interstitial compliance is the change in interstitial volume resulting from a change in interstitial pressure
By creating greater negative pressure, it is possible for the interstitium to help increase net movement of fluid out of the vascular space
Blood Product Administration and Fluid Overload
Volume of transfused products and rate of transfusion were shown to be independent risk factors for fluid overload
Overload doesn't appear to be commonly identified with blood/plasma transfusions in equine medicine
Aggressive Fluid Resuscitation and Fluid Overload
In healthy horses, rates of 80 ml/kg/h seem to well tolerated over a 30 minute period
It seems likely that high rates of crystalloid fluid administration (>20-40 ml/kg/h for a prolonged period) could result in fluid overload particularly in patients with other risk factors
Using Changes in Body Weight to Recognize Fluid Overload
Body weight on presentation can be challenging to evaluate as patients may be severely dehydrated and a gain in body weight after fluid administration may be appropriate
Body weight change doesn't address the location of the excess fluid
In general, a patient who is at risk for fluid overload and consistently gains weight each day may be accumulating excess fluid
Using CVP to Recognize Fluid Overload
CVP represents the pressure within the intrathoracic vena cava
Elevated CVP (>15 cmH2O) may indicate the potential for fluid overload
A rise in CVP (>4 cmH2O) in response to a fluid challenge could indicate a risk for edema formation unless hypovolemia is present and baseline CVP is low
Ability to detect volume overload in horses in unclear
Pulmonary Function Deterioration as a Sign of Fluid Overload
Horses with systemic inflammation may be at risk for pulmonary disease (ARDS) as well as fluid overload
The excess fluid may not be a direct cause of the pulmonary dysfunction; rather the systemic inflammatory response may be the primary cause of excessive pulmonary fluid
Pulse oximetry and arterial blood gas monitoring are practical means of monitoring oxygenation and pulmonary function
Bioimpedance Analysis (BIA) to Recognize Fluid Overload
Bioimpedance analysis (BIA) is designed to be able to determine the amount of water accumulating in different fluid compartments and quantify the size of the ECFV, ICFV, and TBW
Appears to detect acute volume changes in healthy horses
Evidence that BIA may be influenced by electrolyte imbalances, which are common in critically ill patients
Relatively non-invasive but requires patients to remain still for short periods and avoid contact with metal
Pulse Pressure Variation to Recognize Fluid Overload
Pulse pressure variation (PPV) can be used to evaluate the need for fluid volume in patients undergoing mechanical ventilation
Calculated value is based on the difference between systolic and diastolic arterial pressure during the inspiratory and expiratory phases of positive pressure ventilation
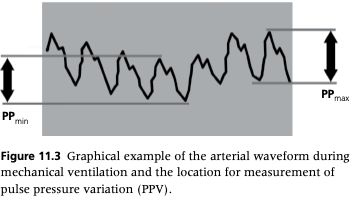
What pulse pressure variation indicates the need for additional IV fluids?
In humans, PPV values of 12-13% have been used to discriminate between patients who will benefit from additional IV fluids and those in whom additional fluids could be detrimental
PPV value greater than 13% would indicate the need for additional IV fluids
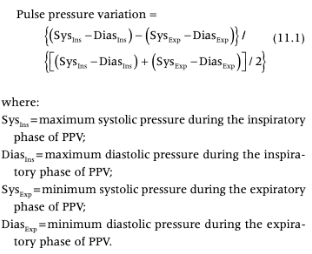
Pulse Pressure Variation Equation
When is treatment of fluid overload indicated?
Fluid overload is contributing to impairment of normal pulmonary function and oxygenation is inadequate
Fluid overload is contributing to impairment of normal cardiovascular function and perfusion is inadequate
Renal function is impaired and the fluid overload is unlikely to improve with time
What are the main components of treatment for fluid overload?
Modify/eliminate fluids being administered
Increase renal excretion of fluids if possible
Remove fluid accumulations (pleural, peritoneal) if possible
Treatment of Fluid Overload - Modification of the Fluid Therapy Plan
In some cases can just decrease the rate of fluid administration
For critically ill patients with poor perfusion, a high rate of fluids may be required to maintain cardiac output
If the rate of fluids can't be safely decreased you may be able to change fluid type
Treatment of Fluid Overload - Increased Renal Excretion of Fluid
Common drugs used to induce diuresis in horses include furosemide and mannitol
In cases of impaired renal function, particularly oliguria or anuria, mannitol could result in further volume overload because it cannot be eliminated
Furosemide is generally effective in achieving a negative fluid balance but it has the potential to cause deterioration in renal function and worsen electrolyte imbalances
Furosemide in Renal Failure
Controversy over the benefits of furosemide in renal failure
May decrease oxygen consumption in the loop of Henle and therefore be protective by decreasing potential ischemic injury
If furosemide is able to increase urinary flow, it could also improve intratubular obstruction
What is the most common treatment to increase renal excretion of fluid in horses?
In horses, furosemide likely represents the most practical and safe option to induce fluid diuresis and resolve volume overload
It is possible that renal function and electrolyte balance may be negatively affected by furosemide
In some cases, continued fluid administration (even hypertonic fluid) in combination with furosemide may be needed to maintain an appropriate fluid balance
Treatment of Fluid Overload - Removal of Fluid Accumulations
If there is large-volume fluid accumulation, removal may improve respiratory function (particularly in cases of pleural effusion) and help restore fluid balance
If fluid removal is too rapid, severe hypotension can result
Prognosis in Fluid Overload
Prognosis for survival following fluid overload depends on the inciting cause and the severity of overload
If the inciting cause can be resolved and renal function is adequate, fluid balance is likely to return to normal
If fluid accumulation is severe and due to renal failure following severe sepsis, the fluid accumulation may be difficult to resolve and the prognosis may be guarded/poor
Renal function is one of the more significant determinants of prognosis in cases of volume overload
In cases of severe overload, pulmonary function may be severely compromised and even if the underlying cause is treatable, respiratory failure may result before the excess fluid can be removed
Treatment with furosemide should be initiated as quickly as possible
Prevention of Fluid Overload - Selection of Fluid Type
Colloid administration has been implicated in fluid overload but it depends on the rate and volume administered
If colloids are required, the rate of fluid administration should be considered and moderated if possible
Prevention of Fluid Overload - Selection of Fluid Rate
Often 50% of the "maintenance rate" may be used in high-risk patients
Fluid boluses should be used only when absolutely necessary as they may cause a more rapid, albeit temporary, increase in central venous pressures than continuous rate administration
Prevention of Fluid Overload - Diuretic Treatment
Administration of a diuretic in conjunction or shortly following fluid resuscitation may help to mitigate fluid overload
Fluid Overload in Neonatal Foals
Risk factors for fluid overload in neonates include kidney failure, heart failure, hypoproteinemia, and inflammatory conditions
Many critical neonatal foals appear to be prone to fluid overload, particularly with the treatment of IV fluids
May be due to differences in capillary permeability or the compliance of their interstitium
Treatment of neonatal foals with fluid overload has similar options to adults
Modifying fluid administration is one consideration, but increasing fluid urinary excretion may be required with significant volume overload
Furosemide infusions are very effective at removing excess fluid from foals, but fluid and electrolyte balance must be monitored