Lec 22 Blood Vessels
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
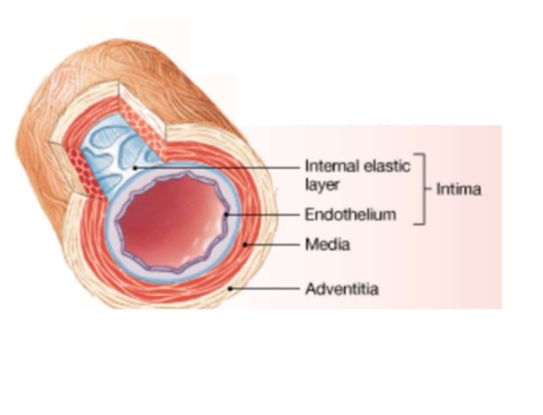
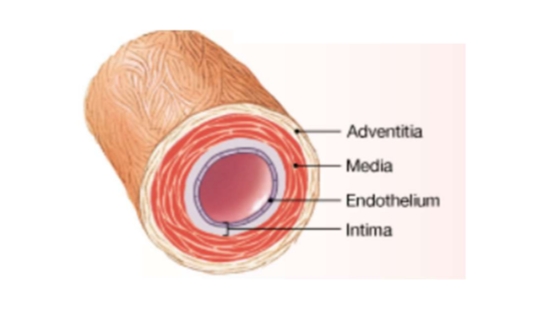
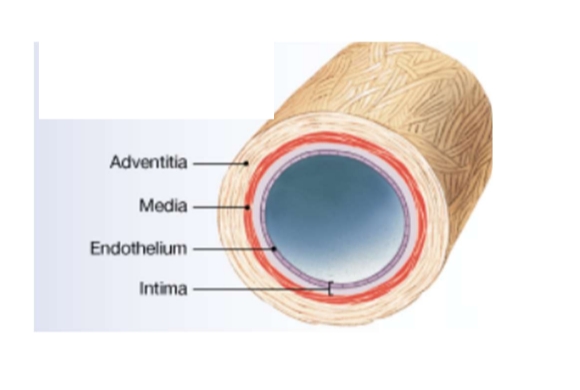
Layers of blood vessels
Adventita
media
Intima
outermost layer of blood vessels
tunica adventitia.
This layer is very thick, composed mainly of collagen fibers. fibroblasts
In veins, this layer is thicker.
The outer adventitia (ad-ven-TISH-a) (tunica externa) forms a connective tissue sheath around the vessel. This layer is very thick, consisting Of collagen fibers with s scattered bands g of elastic fbers. The connective tissue fibers of the adventitia typically blend into those of adjacent tissues, stabilizing and anchoring the blood vessel.
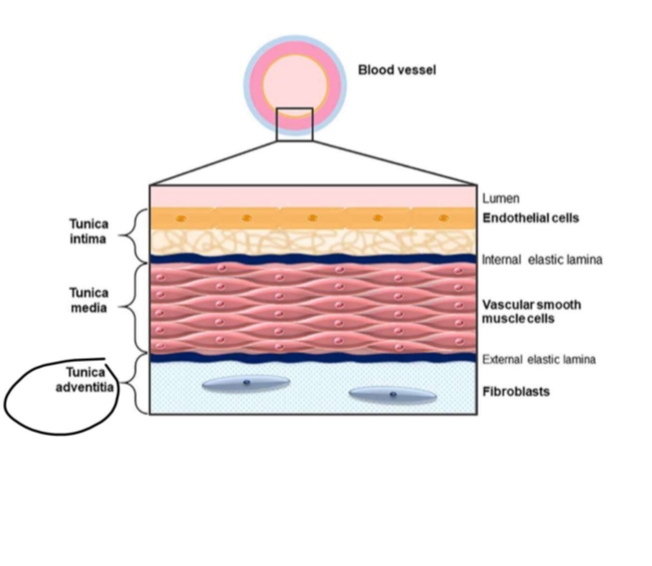
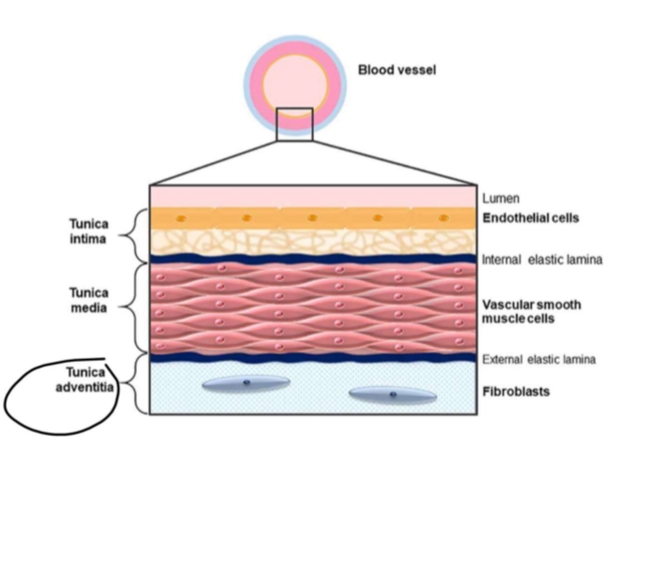
middle layer of blood vessels
tunica media
This layer contains smooth muscle interwoven in loose connective tissue.
These smooth muscles are responsible for vasoconstriction (reduce lumen diameter) and vasodilation (increase lumen diameter).
These changes affect blood pressure and blood flow through your body.
In veins, this layer is thinner.
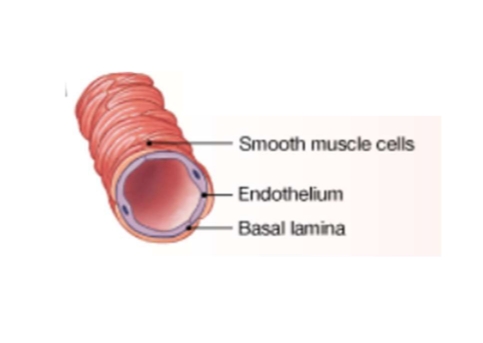
Vascular smooth muscle cells
The media (tunica media) is the middle layer. It contains layers Of circularly arranged smooth muscle. These layers form sheets that are organized and supported by a framework of elastic tissue.
innermost blood vessel layer
tunica intima.
endothelial cells
This layer contains an endothelial lining of the vessel AND an underlying layer of elastic fibers.
In veins, this layer is thinner.
The intima (tunica intima) is the innerost layer of the blood vessel. This layer includes the endothelial Iining of the vessel and an underlying layer of areolar tissue containing variabile amounts of elastic fibers and sometimes scattered smooth muscle cells.
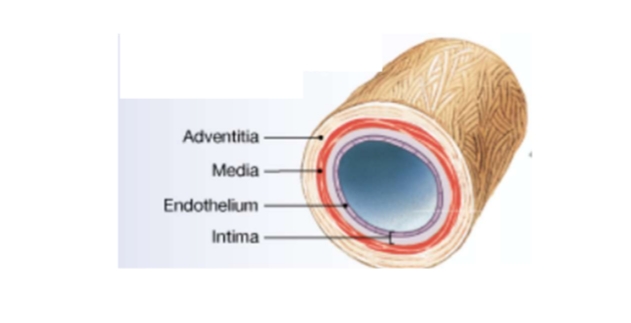
artery vs vein structure Elastic Artery (Largest Artery)
Intima layer has of elastic fiber
Media has a few smooth muscle and instead has a high density of elastic fiber
artery vs vein structure Muscular Artery
Thicker media with a greater percentage of smooth muscle cells
artery vs vein structure: Arterioles (smallest arteries)
The outermost layer of arterioles are mainly made of a media layer with scattered smooth muscle cells.
Poorly defined adventitia.

artery vs vein structure: Lining of capillaries are the exception
Capillaries only have an endothelial layer. Fenestered have pores Continuous have an endothelium tightly connected by tight junctions and desomosomes.

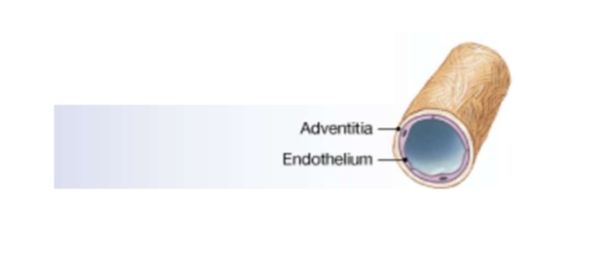
Artery vs vein structure: Venules (smallest veins)
Venules are the smallest veins in our circulatory system and they collect blood from our capillaries.
These venules only have two layers (tunica adventitia AND intima).
No media layer.
Artery vs vein structure Medium-sized veins
Media layer is thin and contains few smooth muscle cells.
Artery vs vein structure Large Sized Veins
Large sized veins include superior and inferior vena cava
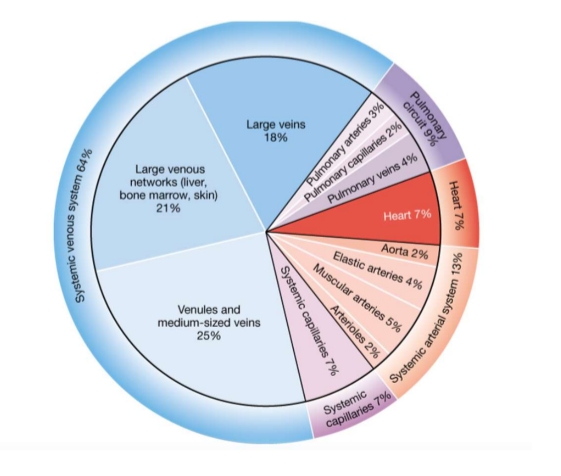
Most of our blood volume is in the venous system
Veins carry 65-70% of our total blood volume (3.5 L).
Arteries, heart, and capillaries contain about 30-35% of our total blood volume (1.5 L)
Veins can stretch easily, and their elastic walls stretch recoil, causing changes in blood pressure in the venous system.
If hemorrhaging (bleeding) occurs, venoconstriction occurs.... Leading to reducing of blood volume in venous system.
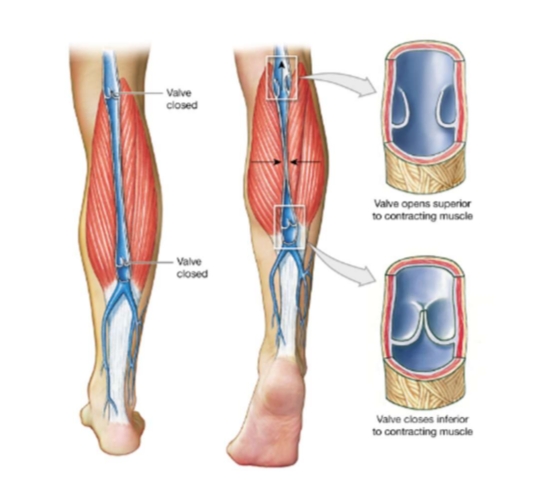
Valves in Venous System Prevents Backflow of Blood
Valves in medium sized veins prevent backflow of blood.
Contraction of skeletal muscles creates pressure that assists maintain blood flow.
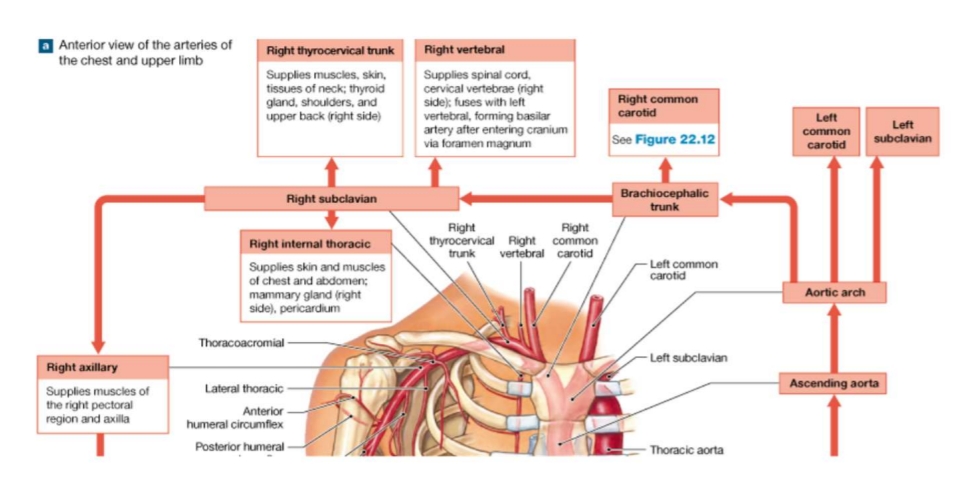
Ascending Aorta Pathway
1. The ascending aorta begins at the aortic semilunar valve of the left ventricle
2. The ascending aorta then ascends to the aortic arch.
Three arteries originate from the aortic arch:
A) left subclavian artery (blood to head, neck, shoulders, upper limb on left side)
B) left common carotid artery (neck/head/brain)
C) brachiocephalic trunk
3. The brachiocephalic trunk ascends for a short distance and then branches into:
A) right common carotid artery
B) right subclavian artery
4. The subclavian arteries arise into three branches:
A) Thyrocervical trunk (muscles/skin)
B) Internal thoracic artery (pericardium/wall of chest)
C) Vertebral artery (brain/spinal cord)
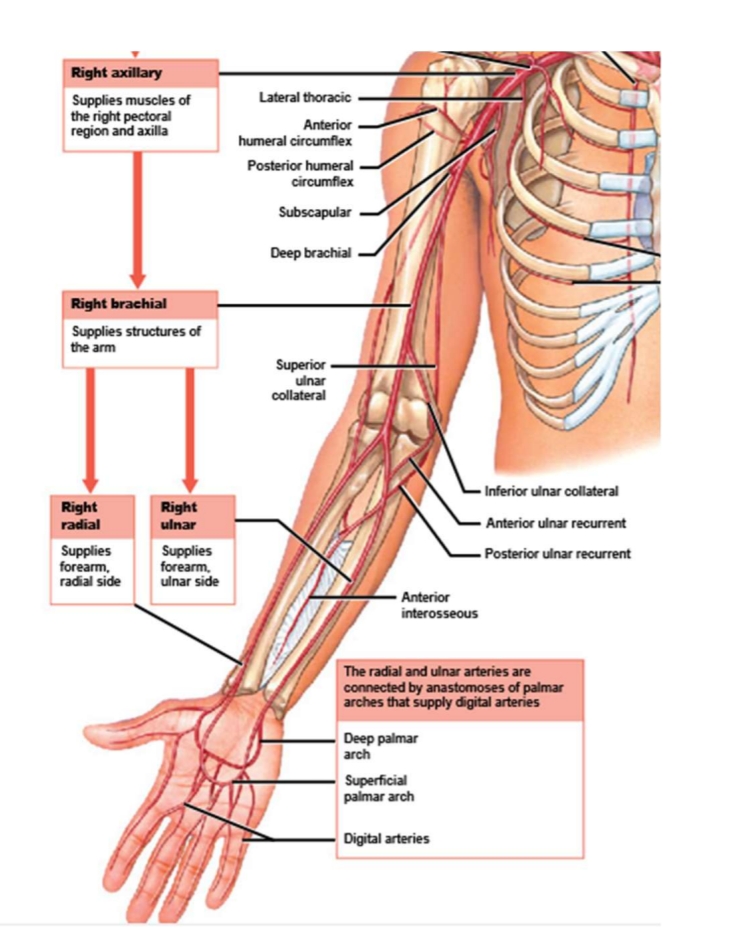
5. The subclavian arteries then leaves the thoracic cavity and becomes the axillary artery.
6. The axillary artery then becomes the brachial artery.
7. The brachial artery becomes the radial AND ulnar arteries.
8. The radial and ulnar arteries are connected by openings of palmar arches that supply the digits (fingers).
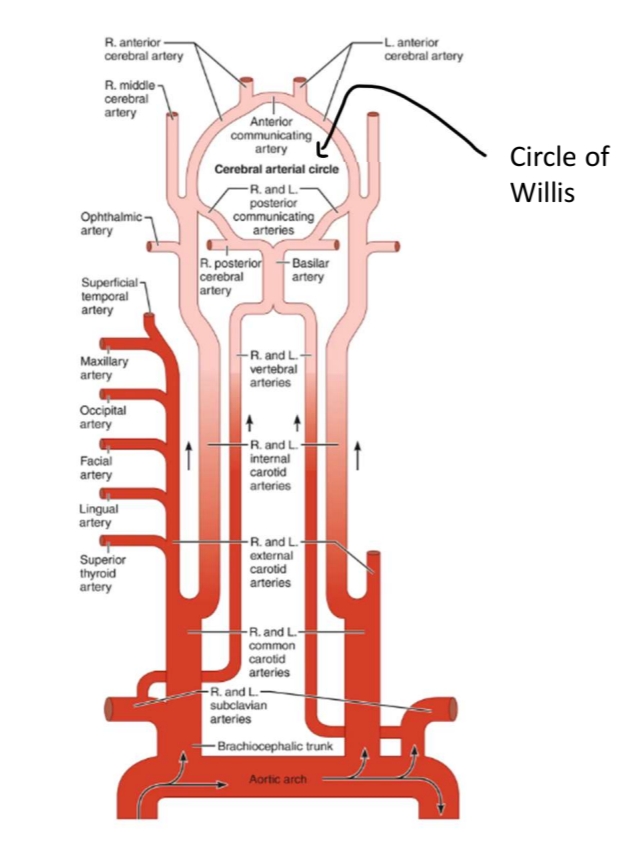
What branches from the common carotid arteries?
The common carotid arteries branch into the following:
External carotid (which branches to: superficial temporal , maxillary , occipital, facial, lingual, superior thyroid)
Internal carotid (which branches to: ophthalmic , middle cerebral , and becomes anterior cerebral which is part of the Circle of Willis which includes communicating arteries and branches of the vertebral arteries from the subclavian artery)
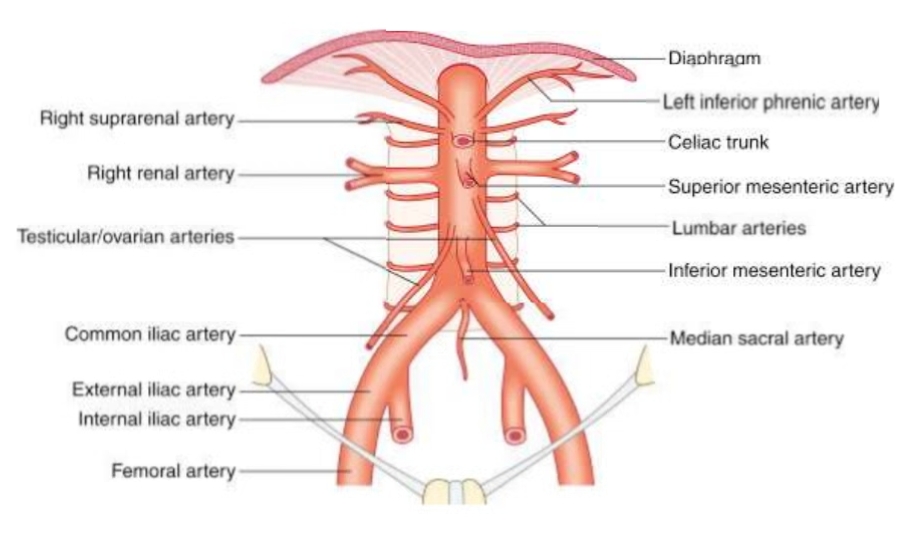
Descending Aorta pathway
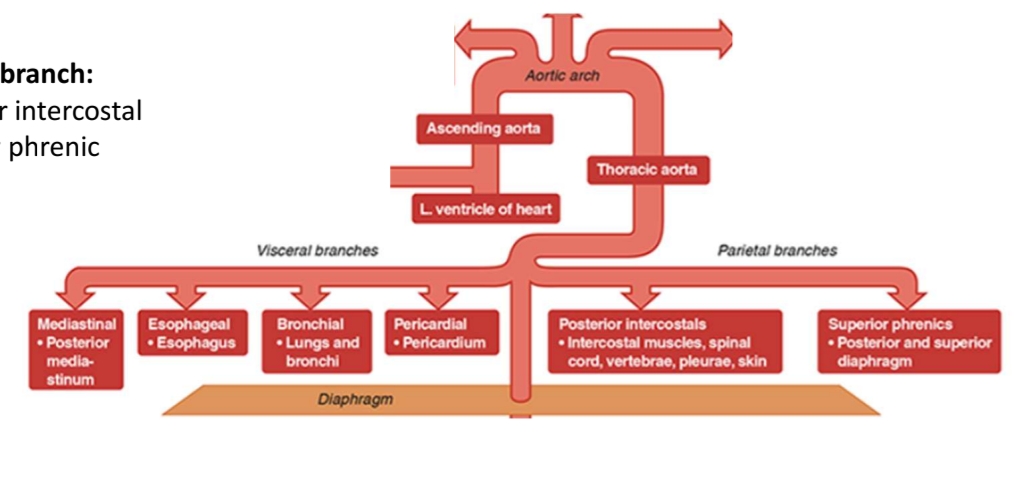
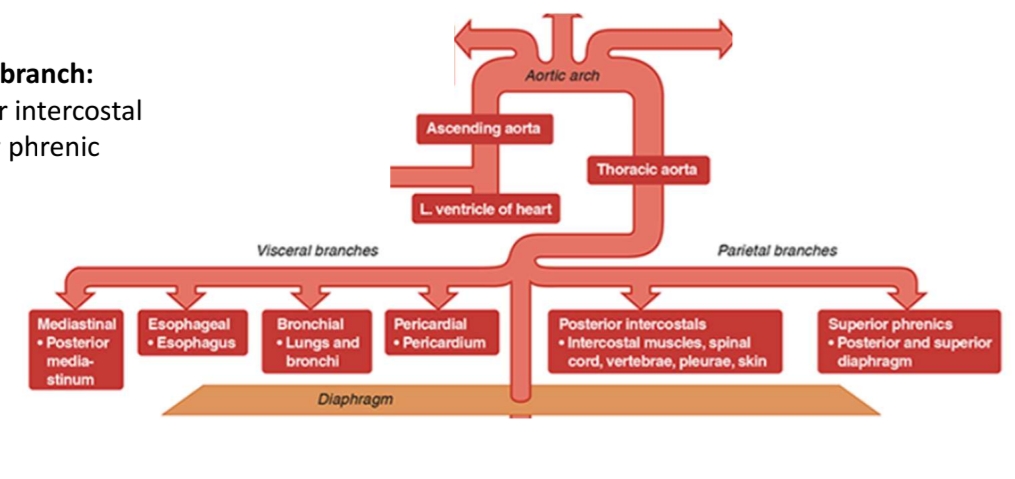
1. Descending from the aortic arch will be the descending aorta.
2. The descending aorta divides into a superior thoracic aorta.
A) begins at the level of vertebra T5 and penetrates the diaphragm at the level of vertebra T12
B) grouped as either visceral branches (supplies blood to organs of the chest) (Visceral branch: Mediastinal Esophageal Bronchial Pericardial) OR parietal branches (supplies blood to chest wall) (parietal branch: Posterior intercostal Superior phrenic)
3. Inferior to the diaphragm, the thoracic aorta now becomes the abdominal aorta.
4. There are three unpaired arteries branching from the abdominal aorta:
A) celiac trunk (divided as left gastric, splenic, and common hepatic artery)
B) superior mesenteric (pancreas, small and large intestine)
C) inferior mesenteric (colon/rectum)
5. There are five paired arteries branching from the abdominal aorta:
A) inferior phrenic arteries (esophagus/diaphragm) B) suprarenal arteries (kidney)
C) renal arteries (kidney)
D) gonadal arteries (testicular/ovarian arteries)
E) lumbar arteries (spinal cord)
6. Descending aorta then divides into:
A) median sacral artery
B) common iliac artery
C) external iliac artery
D) internal iliac artery
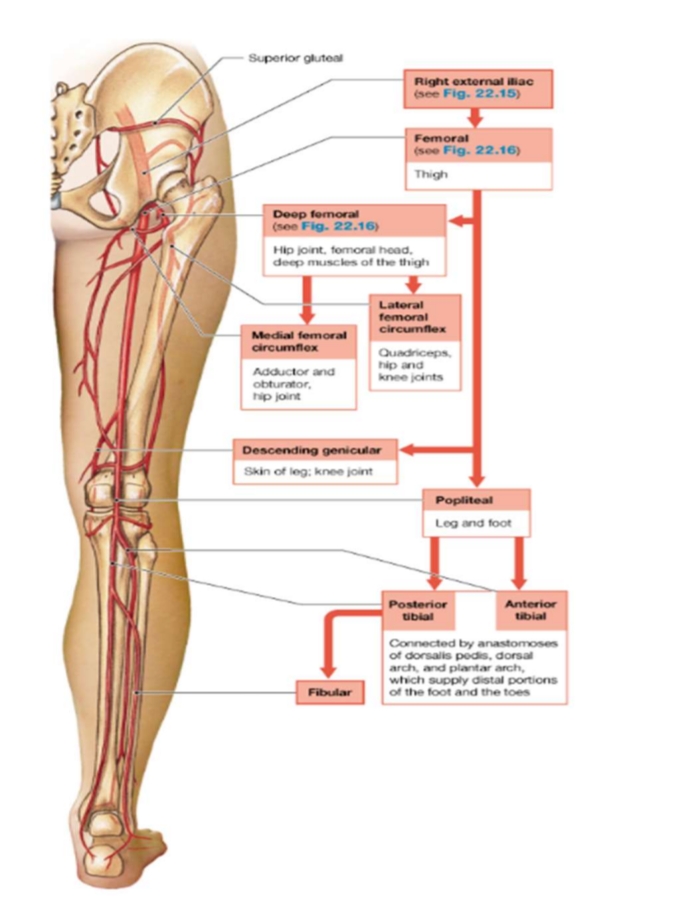
7. External iliac artery becomes the femoral artery.
8. Femoral artery becomes deep femoral artery, descending genicular artery, and popliteal artery.
9. Popliteal artery becomes posterior tibial, anterior tibial, and fibular arteries.
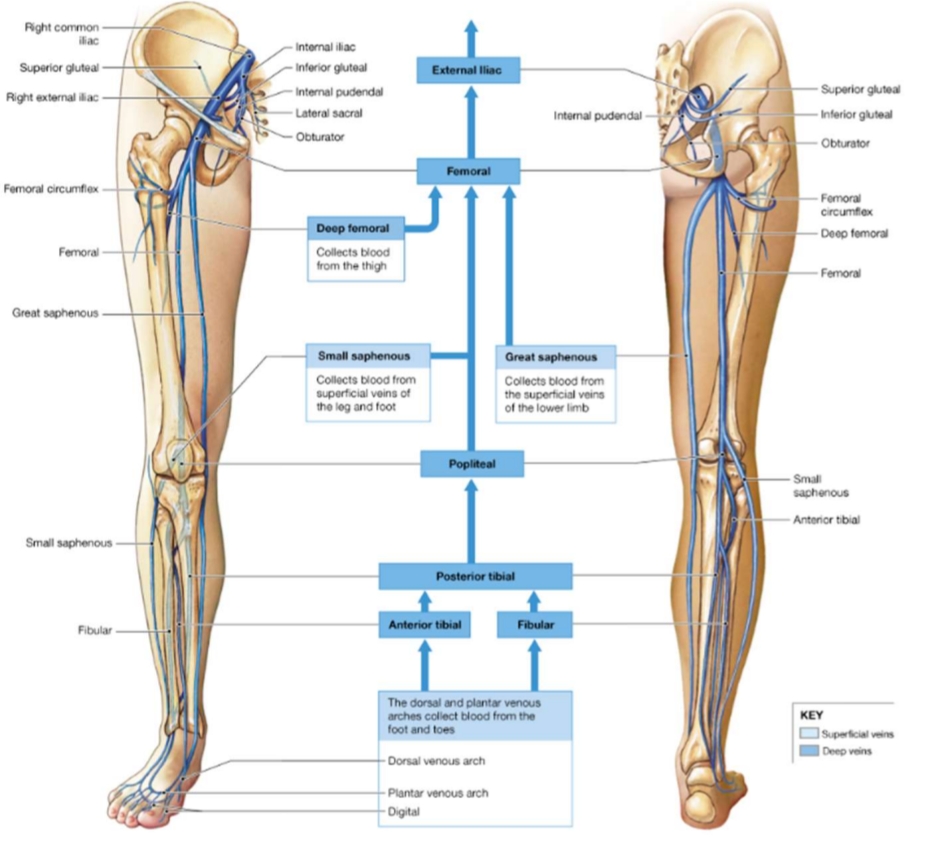
Inferior Vena Cava (Lower Limb Drainage)
1. The anterior tibial vein AND fibular vein collect blood from dorsal and plantar venous arches.
2. Both veins allow blood to travel to posterior tibial vein.
3. Posterior tibial vein then becomes popliteal vein. Popliteal vein becomes femoral vein.
4. Other veins that travel to femoral vein:
A) small and great saphenous (surgeons use this blood vessel as a graft for coronary artery bypass) B) deep femoral vein
Special Vein Terms
Azygous vein – vein that is unpaired running up the right side of the thoracic vertebral column to the superior vena cava
Basilic vein – large superficial vein of the upper limb that drains the hand and forearm (commonly seen under skin of arm/forearm)
Jugular vein – takes venous blood from the head back to the superior vena to heart