MISSED Q'S FROPM CANVAS cna
1/118
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
119 Terms
Stress is best defined as
Blaming another for one’s problems.
The main cause of illness.
A response to any demand made on an individual.
A vague feeling of apprehension.
A response to any demand made on an individual.
When should changes in a resident’s condition be reported?
During the resident care conferences
As soon as possible
Right away
During the end-of-shift report
Right away
Which form of communication may reveal the most about a resident’s true feelings?
Written communication
Verbal communication
Body language
Listening skills
Body language
he Nurse Assistant sees water on the floor. The Nurse Assistant should immediately:
Report the water to the nurse.
Call the housekeeping staff.
Place a paper towel over the water.
Clean up the water.
Clean up the water.
Which of the following items is NOT a fire hazard?
A broken three-pronged electrical plug.
An open can of cleaning fluid.
A full waste basket.
A damaged electrical cord.
A full waste basket.
When applying soft postural supports to a resident, the Nurse Assistant MUST:
Apply the postural supports tightly.
Apply lotion to the skin.
Apply padding over bony areas.
Tie the postural supports to the side rails.
Apply padding over bony areas.
After hearing the emergency code for fire, the Nurse Assistant should:
Close all room doors and report to the nurse in charge.
Wait for the fire fighters to give directions
Wait for the nurse in charge to give directions.
Provide a list of all assigned residents by name and room number.
Close all room doors and report to the nurse in charge.
The Nurse Assistant is caring for a resident who is wearing wrist restraints. The Nurse Assistant should remove the restraints and perform passive range-of-motion exercises for the resident at least every:
8 hours.
2 hours.
4 hours.
24 hours.
2 hours.
Which of the following devices would not be used for resident activities of daily living?
A walker, a cane, and crutches.
A stethoscope, a blood pressure cuff, and a thermometer.
A cup or glass holder and silverware attached to a splint.
Plate guards and silverware with cuffs or curved handles.
A stethoscope, a blood pressure cuff, and a thermometer.
The Nurse Assistant is cleaning the nose of a resident who is receiving continuous oxygen by a nasal tube. The Nurse Assistant should NOT use:
Warm water.
An oil-based lubricant.
Soap and water.
A water-based lubricant.
An oil-based lubricant.
Which is the main reason that the Nurse Assistant MUST report broken equipment?
The information will go in an incident report.
The Nurse Assistant could be held legally responsible for the broken equipment.
The Nurse Assistant must care about resident and staff safety.
The information is needed by the nurse in charge.
The Nurse Assistant must care about resident and staff safety.
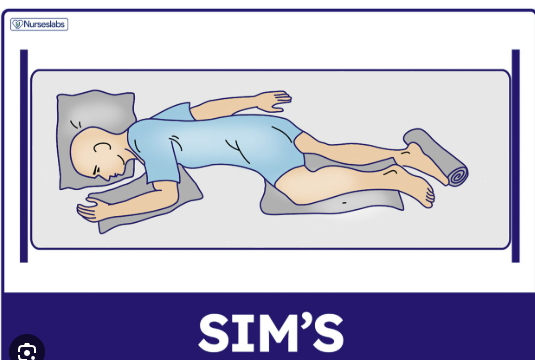
what is sims position?
a semiprone position where a patient lies on their left side with their right knee and thigh drawn up, and the left arm extended back
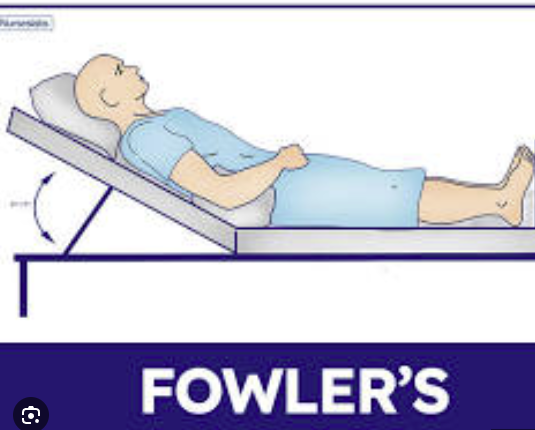
what is semifowlers position
a semiprone position where a patient lies on their left side with their right knee and thigh drawn up, and the left arm extended back
When placing a resident in the lateral position, you promote good body alignment by placing pillows for support under the:
Head, shoulders and ankles.
Head, upper arm, upper leg and behind the back.
Head, abdomen and upper arms.
Head, lower back, arms and resident’s sides.
Head, upper arm, upper leg and behind the back.
When assisting a resident with left sided weakness to transfer from the bed to a chair, the chair should be located:
At the foot of the bed, on resident’s left side.
Across the room to encourage the resident to get up and walk.
At the middle of the bed directly across from where the resident sits in the bed.
At the head of the bed, on resident’s right side.
At the head of the bed, on resident’s right side
When positioning a resident in a side lying position, the Nurse Assistant must first:
Log roll the resident toward the nearest side rail.
Move the resident to the side of the bed where the Nurse Assistant is standing.
Move the resident toward the foot of the bed.
Log roll the resident toward the opposite side rail by yourself.
Move the resident to the side of the bed where the Nurse Assistant is standing.
Your resident is paralyzed from the waist down (paraplegia) and has maintained good upper body strength. The resident wants to be able to move himself in bed, somewhat, without assistance. Which of the following pieces of equipment might be used for this purpose?
Pillow
Trapeze
Gurney
Gait belt
Trapeze
Good body alignment is needed:
When standing
When sitting
When lifting
All the time
All the time
When giving bedside care, the bed should be:
In Fowler’s position.
At its highest horizontal level.
At its lowest horizontal level
Level with your waist.
Level with your waist.
Before moving Mr. G up in bed, you need to:
Put nonskid footwear on him.
Apply a transfer belt.
Lock the bed wheels.
Raise the head of the bed.
Lock the bed wheels.
Asepsis means:
Clean technique
The process of destroying pathogens
An infection acquired after admission to a health care agency
Being free of disease-producing microbes
Being free of disease-producing microbes
Who can develop nosocomial or Healthcare Associated Infection (HAI)?
Health Team
Nursing Team
Doctors
Residents
Residents
Standard Precautions apply to:
All residents
Persons with infections
Health team
All persons
All persons
The hepatitis B vaccination involves:
1 injection
2 injection
4 injection
3 injections
3 injections
The Nurse Assistant is leaving an isolation room. After hand washing, the Nurse Assistant should:
Open the door with clean, washed hands.
Use a disposable glove to open the door and put glove in the basket outside the room.
Use a paper towel to open the door and put the paper towel in the basket outside the room.
Use a paper towel to open the door and put the basket inside the room near the door.
Use a paper towel to open the door and put the basket inside the room near the door.
The correct order for removing protective clothing before leaving a resident’s isolation room is:
Gloves, gown, mask, and wash hands.
Mask, gown, gloves, and wash hands.
Mask, gloves, gown, and wash hands
Gown, gloves, mask and wash hands
Gloves, gown, mask, and wash hands.
When caring for a resident who is in isolation, how would the Nurse Assistant safely remove soiled linen?
Wear gloves when bringing out the soiled linen.
Take soiled linen to a container outside of the room.
Double-bag the soiled linen when required by your facility.
Leave soiled linen in room for housekeeping to remove.
Double-bag the soiled linen when required by your facility.
The licensed nurse tells the Nurse Assistant that a resident’s bedpan needs to be cleaned. The MOST effective way to kill all the organisms would be to:
Put the bedpan in a bedpan washer.
Wash the bedpan with soap and water
Wash the bedpan in hot water.
Use a chemical disinfectant on the bedpan
Use a chemical disinfectant on the bedpan
Your resident ate the following items for lunch: ½ cup string beans, 3 oz. fish, 6 oz. milk, 2 oz. Jello. What was his fluid intake?
120ml
330ml
240ml
300ml
240ml
A complete bed bath would be given to a resident who:
Cannot step into a bath tub.
Is unconscious
Is paralyzed on one side.
Has difficulty using his right hand.
Is unconscious
n preparing the bath for the dependent resident, the Nurse Assistant should:
Adjust the water temperature to 105( F.
Fill the tub with no more than two inches of water.
Position the resident in the tub before adding water.
Make sure that the water temperature is at least 120( F.
Adjust the water temperature to 105( F.
When bathing a dependent resident, the Nurse Assistant should:
Leave the room at intervals to encourage the resident to bathe on his own.
Rinse off all soap completely and dry the skin thoroughly.
Apply soap to all areas before rinsing with fresh water.
Rub the skin vigorously to stimulate circulation.
Rinse off all soap completely and dry the skin thoroughly.
When washing the face of a dependent resident, the Nurse Assistant should:
Use a separate washcloth for washing each eye.
Rinse the eyes by pouring a small amount of water on the forehead.
Wipe the eyes from the outer edge to the center.
Use different corners of the washcloth when washing each eye
Use different corners of the washcloth when washing each eye
In a complete bed bath, the water is changed:
Whenever the water becomes soapy or cool.
At the completion of the bath.
After each body area is washed.
After the front surfaces of the body are washed.
Whenever the water becomes soapy or cool.
To assist Mrs. B a resident, into a bathtub, the Nurse Assistant should:
Stand at the side of the tub and have the resident hold on to your shoulder as she steps into the tub.
Have the resident sit on the side of the tub, pick up both legs and pivot them over the side and into the tub.
Have the resident hold on to the grab bar in the tub enclosure as she steps into the tub.
Place a chair next to the tub and have the resident hold on to the chair as she steps into the tub.
Have the resident hold on to the grab bar in the tub enclosure as she steps into the tub.
Oral hygiene should be done:
Before and after meals or snacks.
After breakfast and after last meal or snack of the day.
Before and after each meal.
After each meal and at bedtime.
After each meal and at bedtime.
In what position should an unconscious resident be placed when performing oral care?
Supine (on the back) position.
Standing position
Lateral (side-lying, head to side) position.
Prone (on the stomach) position.
Lateral (side-lying, head to side) position.
Before combing or brushing a resident’s hair, the Nurse Assistant should:
Put on gloves.
Soak the resident’s comb and brush in a disinfectant solution.
Wet the hair with a spray bottle.
Place a towel over the resident’s shoulders.
Place a towel over the resident’s shoulders.
A bed shampoo will require:
Spray bottle, emesis basin and washcloth.
Shampoo tray, plastic sheet or bag, pitcher and basin.
Thermometer, graduate, bath basin, and several towels.
Extra sheet, pillow, and pitcher.
Shampoo tray, plastic sheet or bag, pitcher and basin.
After shaving a resident with his own electric razor, the Nurse Assistant should:
Clean the blades of the razor with a cleaning brush.
Soak the razor in a disinfectant solution.
Report the action to the charge nurse.
Apply an oil based lotion to the skin.
Clean the blades of the razor with a cleaning brush.
The Nurse Assistant is putting a pair of pants on a resident who cannot sit up because of weakness. The Nurse Assistant should slip both feet into the legs of the pants and then:
Attempt to sit the resident on the side of the bed and pull pants up toward the waist.
Pull the top of the pants under the buttocks up the waist with the resident flat on his back.
Assist the resident to roll from side to side as the Nurse Assistant pulls the pants up to the waist.
Ask the resident to bend his knees and raise his buttocks as the Nurse Assistant pulls the pants up to his waist.
Assist the resident to roll from side to side as the Nurse Assistant pulls the pants up to the waist.
A general rule for dressing a resident who is paralyzed or injured is:
Have clothing split and snaps applied for easy dressing.
Dress the affected side first and undress it last.
Dress the affected side last and undress it first.
Avoid dressing the affected side.
Dress the affected side first and undress it last.
If a resident is unable to stand up while being measured it is best to:
Measure the resident’s height while lying in bed.
Chart that the measurement was not done because the resident could not stand.
Ask the resident how tall he was when ambulatory.
Estimate the resident’s height.
Measure the resident’s height while lying in bed.
A resident was admitted to the nursing unit several days after surgery. To prevent problems, the Nurse Assistant should:
Leave the resident in bed at all times.
Leave the resident alone to rest all day.
Tell the resident to cough and deep breathe every two hours.
Tell the resident to remain in the same position at all times.
Tell the resident to cough and deep breathe every two hours.
. When changing a colostomy bag, the Nurse Assistant should know:
All colostomy residents have liquid stools.
The colostomy bag needs to be changed when the bag is leaking.
The colostomy bag must be changed every two hours.
A skin barrier will hold the bag in place without a belt.
The colostomy bag needs to be changed when the bag is leaking.
Which of the following foot care procedures is required for the resident who is paralyzed from the waist down?
Wash and dry feet carefully and thoroughly, and check for any pressure signs.
Wash feet carefully, trim toenails and apply lubricant to keep area between toes moist.
Wrap the feet in hot towels, trim toenails if needed, and lubricate feet.
Soak the feet in hot water after bathing.
Wash and dry feet carefully and thoroughly, and check for any pressure signs.
he Nurse Assistant should clean the resident’s genital and anal areas:
Only when the resident is soiled.
Once during each shift.
Once a day and when the resident is soiled.
Every time the resident uses the bathroom.
Once a day and when the resident is soiled.
Which of the following might the Nurse Assistant do to keep a resident from being incontinent of urine?
Offer the resident the toilet, bedpan or urinal at regular intervals.
Tell the resident that he will be assisted to the bathroom every four hours.
Leave a bedpan under the resident.
Tell the resident not to drink as much water.
Offer the resident the toilet, bedpan or urinal at regular intervals.
The Nurse Assistant should know that dentures should be cleaned at which of the following times?
Before breakfast and at bedtime.
After breakfast, lunch and supper.
Before breakfast, lunch, supper, and at bedtime.
After breakfast and at bedtime.
Before breakfast, lunch, supper, and at bedtime.
What is the preferred position for giving an enema?
Prone or supine position.
Fowler’s or semi-fowlers position.
Sims’ or left side lying position.
Supine or right side-lying position.
Sims’ or left side lying position.
Water temperature for an enema solution for adults usually is
105ᵒ
Body temperature.
110ᵒ
100ᵒ
105ᵒ
The nurse asks you to strain a person’s urine. To do this, you need
Elastic tape.
A 24-hour urine specimen.
A strainer or gauze.
A midstream urine specimen.
A strainer or gauze.
Mucus from the respiratory system that is expelled through the mouth is
Sputum.
Saliva.
Phlegm.
Ketone.
Sputum.
When collecting a sputum specimen, the person coughs up sputum from the
Throat.
Bronchi and trachea.
Upper airway.
Mouth.
Upper airway.
Which of the following is a characteristic of normal urine?
Straw-colored urine.
Red-colored urine.
Pale-yellow urine.
Clear urine.
Pale-yellow urine.
A resident is up all day. What kind of bed should you make?
Closed bed.
Occupied bed.
Open bed.
Surgical bed.
Closed bed.
The bottom sheet is placed on the bed correctly if
It completely cover the plastic drawsheet.
The hem-stitching faces outward.
The hem-stitching is down.
The top edge is even with bottom of the mattress.
The hem-stitching is down.
Drainage that is thick green, yellow, or brown is
Sanguineous drainage.
Purulent drainage.
Serosanguineous drainage.
Serous drainage.
Purulent drainage.
Which will help prevent skin tears?
Practice hand hygiene before and after giving care.
Wear simple earrings.
Wear gloves.
Keep your fingernails short and smoothly filed.
Keep your fingernails short and smoothly filed.
A resident is going to be discharged. What must occur before the person can leave?
The person must be transported to the exit area by wheelchair or stretcher.
Give the person prescriptions written by the doctor.
The person must pay the bill.
The person must sign a consent form.
The person must be transported to the exit area by wheelchair or stretcher.
An elastic bandage is applied from the
Top part to the lower part.
Back to front.
Lower part to the top part.
Front to back.
Lower part to the top part.
A resident objects to a transfer or a discharge. An ombudsman makes sure that the person’s best interests are considered.
True
False
true
When using a fracture pan, the larger end is placed under the buttocks.
True
False
False
Which of the steps mentioned below should the Nurse Assistant not do as part of taking a rectal temperature for an adult?
Insert the thermometer one inch into the rectum.
Shake down the thermometer until it registers below 96 °F.
Position the patient in the prone position.
Position the patient in the prone position.
A resident has a temperature of 102( F. What can the Nurse Assistant do to assist in lowering the fever without a physician’s order?
Apply an ice cap to the resident’s forehead.
Place the patient on a hypothermia blanket.
Encourage the resident to drink cool fluids, if allowed to have oral intake.
Give the resident an alcohol bath.
Encourage the resident to drink cool fluids, if allowed to have oral intake.
Which of the following signs is not associated with a fever?
Skin dry and hot to touch.
Decreased pulse.
Flushed face.
Thirst.
Decreased pulse.
When a resident experiences difficult, painful or labored breathing, it is known as:
Dyspnea.
Apnea.
Tachypnea.
Bradypnea.
Dyspnea.
When a resident must be in a sitting position in order to breathe, this is known as:
Cheyne-stokes respiratory.
Hyperventilation.
Snoring.
Orthopnea.
Orthopnea.
How much fluid should the average adult take in each day?
1,500 milliliters.
2,500 milliliters.
800 ounces.
4,000 milliliters.
1,500 milliliters.
A resident has a gastrostomy tube. The Nurse Assistant knows that this is:
A tube inserted through the nose to the stomach for feeding.
A tube inserted through the abdominal wall into the stomach for feeding.
A tube that introduces high-density nutrients into a large vein.
The same as total parenteral nutrition (TPN).
A tube inserted through the abdominal wall into the stomach for feeding.
Approximately how much daily urine output is normal for an average adult?
800 ounces.
1,500 milliliters.
4,000 milliliters.
2,500 milliliters.
1,500 milliliters.
When caring for a resident who receives tube feedings the Nurse Assistant must always:
Position the resident in the orthopneic position for each feeding.
Check the placement of the tube.
Elevate the head while the feeding is infusing.
Change the bag at the end of a shift.
Elevate the head while the feeding is infusing.
Hot liquids are best tested by:
Placing a few drops of liquid on the Nurse Assistant’s wrist.
Placing a few drops of liquid on the resident’s wrist.
Touching the outside of the dish or cup.
Inserting a thermometer into the center of the liquid.
Placing a few drops of liquid on the Nurse Assistant’s wrist.
While feeding a resident, a Nurse Assistant is observed doing all the following actions. Which of the following is not correct?
Only using a spoon for solids.
Standing at eye level.
Alternating liquid and solid food.
Feeding the resident in his room.
Correct answer
Question 19
Standing at eye level.
Which of the following are causes for hypoglycemia?
Too much insulin, omitting a meal, vomiting.
Not enough insulin.
Stress, increased activity.
Decrease activity, vomiting, and undiagnosed diabetes.
Too much insulin, omitting a meal, vomiting.
Mr. Jones is showing the following signs and symptoms: dizziness, headache, weakness on his right side, and aphasia. What could be the cause?
Shock.
CVA
Heart attack.
Syncope.
CVA
Mr. G is coughing forcefully after swallowing a piece of meat. The Nurse Assistant should:
Stay with Mr. G to monitor coughing.
Abdominal thrusts only if not coughing.
Give Mr. Gomez a glass of water.
Call for help.
Stay with Mr. G to monitor coughing.
While eating, a resident suddenly has a problem breathing but is able to say, “I’m choking” and is not coughing. Which of the following should the Nurse Assistant do?
Administer abdominal thrusts.
Give the resident black blows.
Do a finger sweep of the resident’s mouth.
Apply chest thrusts.
Administer abdominal thrusts.
The following are common with otitis media EXCEPT
Dizziness.
Pain.
Tinnitus.
Hearing loss.
Dizziness.
A malignant tumor
Invades nearby tissues.
Grows slowly and in a localized area.
Can spread to other parts of the body.
Is not cancer.
Can spread to other parts of the body.
The two most common causes of stroke are
Bleeding in the brain and blood clots
Hypertension and diabetes.
Aging and poor nutrition.
Infection and accidental injury.
Bleeding in the brain and blood clots
Care of a person after a stroke often includes the following except
A bowel and/or bladder training program.
Measures to prevent pressure ulcers.
Ostomy care.
ROM exercises to prevent contractures.
Ostomy care.
A resident has heart failure. The doctor is likely to order
Elastic stockings.
A cane or walker.
A splint or brace.
Trochanter rolls.
Elastic stockings
When the urinary bladder is removed, a new pathway is needed for urine to exit the body. The new pathway is called a
Ureterostomy.
Renal pathway.
Renal tubule.
Urinary diversion.
Urinary diversion.
You are applying an elastic bandage to a person’s left leg. Which is incorrect?
Start at the top (proximal) part of the extremity.
Position the part in good alignment.
Face the person during the procedure.
Expose the toes if possible.
Start at the top (proximal) part of the extremity.
A resident has glaucoma. What do you know about the person’s sight?
The person cannot see to the side.
Print and colors appear faded.
The person is blind in the affected eye.
The person’s vision is cloudy.
The person cannot see to the side.
Risk factors for stroke include the following except
Hypertension and a family history.
Diabetes, osteoporosis, and obesity.
Heart disease, inactivity, and excessive alcohol use.
Smoking and high blood cholesterol.
Diabetes, osteoporosis, and obesity.
A hallucination is
Seeing, hearing, smelling, or feeling something that is not real.
An exaggerated belief.
A persistent thought or idea.
A false belief.
Seeing, hearing, smelling, or feeling something that is not real
Delirium is
A false disorder of the mind.
The loss of cognitive function caused by changes in the brain.
A false belief.
A state of temporary but acute mental confusion.
A state of temporary but acute mental confusion.
Sundowning is
When signs, symptoms, and behaviors of Alzheimer’s disease increase during hours of darkness.
A state of temporary but acute mental confusion.
The loss of cognitive and social function caused by changes in the brain
A false dementia.
When signs, symptoms, and behaviors of Alzheimer’s disease increase during hours of darkness.
A resident has AD. The person has the following behaviors. Which has the greatest risk for danger?
Delusions.
Catastrophic reactions.
Screaming.
Wandering.
Catastrophic reactions.
Elastic bandages and elastic stockings do the following except
Promote circulation.
Promote comfort.
Prevent infection.
Prevent injury.
Prevent infection.
Hepatitis A is spread by
The fecal-oral route.
Blood.
Airborne droplets.
Direct contact.
The fecal-oral route.
What is the highest level of anxiety?
Panic.
Phobia.
Compulsion.
Obsession.
Panic.
Which is not an early warning sign of dementia?
.
Personality changes.
Not recognizing self or family members.
Getting lost in familiar places.
Poor or decreased judgment.
Not recognizing self or family members.
quadriplegia
you experience paralysis of all four limbs and the torso, which results in a complete loss of function and sensation in your arms and legs
The main therapy that assists residents to re-learn activities of daily living is:
Physical therapy
Cognitive therapy
Occupational therapy
Speech therapy
Occupational therapy
Which of the following is NOT an activity of daily living?
Dressing
Taking medications
Ambulating
Toileting
Taking medications
A complication of immobility that affects the gastrointestinal system is:
Hemorrhoids
Confusion
Diarrhea
Constipation
Constipation
People with disabilities are special and should be treated differently from other residents.
True
False
False