SYS Path 1
1/96
Earn XP
Description and Tags
hemolymphatics,
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
What is included in myeloid tissue
bone marrow, any circulating cells derived there
RBC, neutrophils, eosinophils, basophils, etc
What is included in lymphoid tissue
Lymph nodes, spleen, thymus, circulating lymphocytes, bursa of Fabricius
What are primary lymphoid organs
bone marrow, thymus
where lymph is born
What are secondary lymphoid organs
lymph nodes, tonsils, spleen, MALT
Three main places where hematopoiesis occurs
Yolk sac: embryo → shifts to liver and spleen in fetus
Liver and spleen: fetus → shifts to bone marrow prior to birth
When mature: is location of extramedullary hematopoiesis
Bone marrow: young → all marrow spaces
When mature: marrow spaces of the axial bones, proximal humerus and femur
3 main patterns to consider in gross pathology of bone marrow
Colour → yellow (fat), red (hematopoietic tissue), white (fibrosis, necoris)
Location → epiphyseal, metaphyseal, diaphyseal, endosteal
Distribution → diffuse/general, focal, multifocal
Reasons for diffuse and generalized decreased/empty/replaced hematopoietic bone marrow
Myelofibrosis
Nutritional deficiencies
Infectious agents → viral, protazoal, fungi
Destruction → radiation, chemotherapy, drugs, estrogen, immune mediated
Reasons for focal and multifocal decreased/empty/replaced hematopoietic bone marrow
Multiple myeloma
Non-myeloid/lyphoid neoplasia
Metastatic neoplasia
Reasons for diffuse extra hematopoietic bone marrow
Age (physiological, NOT pathological in young)
Hyperplasia (longstanding increased demand)
Myeloid/lymphoid leukemia
Myelodysplastic syndrome
Patchy and multifocal reasons for extra hematopoeitic bone marrow
Leukemia, lymphoma
Endosteal reasons for extra hematopoeitic bone marrow
Hyperplasia (>3 weeks of increased demand)
Reasons for hemorrhagic bone marrow
Trauma
Bone cyst
Infarction
Necrosis
Reasons for inflamed bone marrow
Myelitis
Infectious agents
What are 4 main reasons that bone marrow is decreased, empty, or replaced
Increased destruction → immune mediated, toxic, infectious, radiation
Reduced production or function → hereditary, nutritional deficiencies
Demand exceeds production capacity → overwhelming bacterial infection
Replacment (myelophthisis) → myelofibrosis, diffuse neoplasia

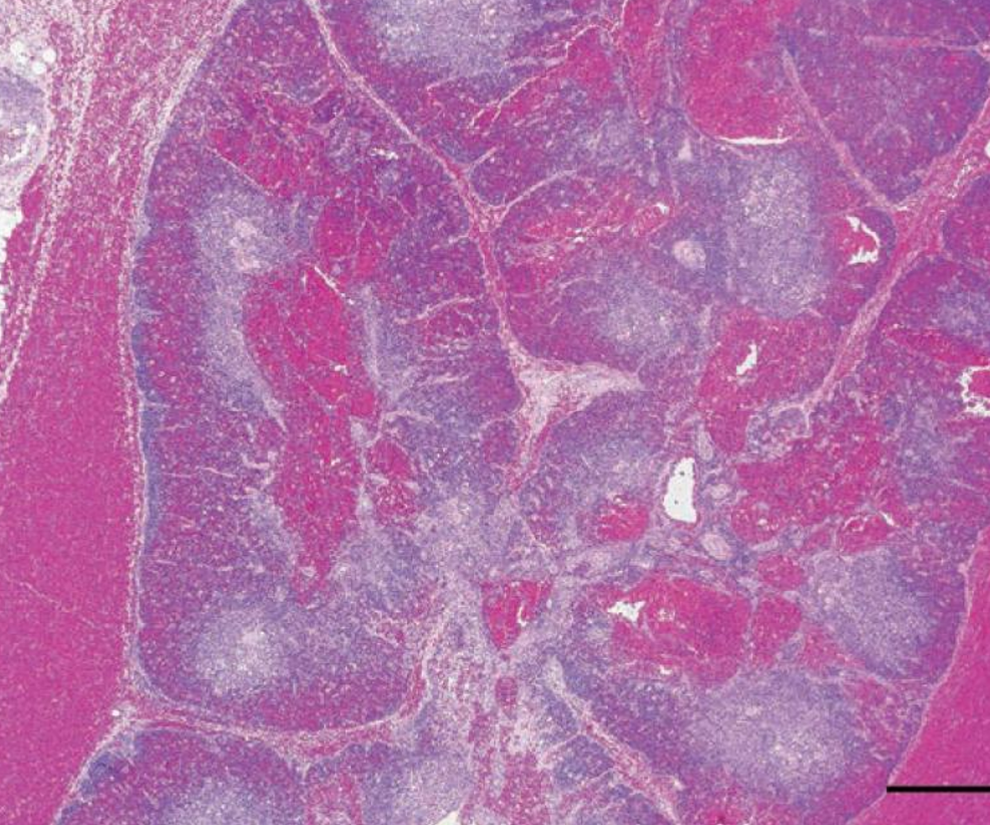
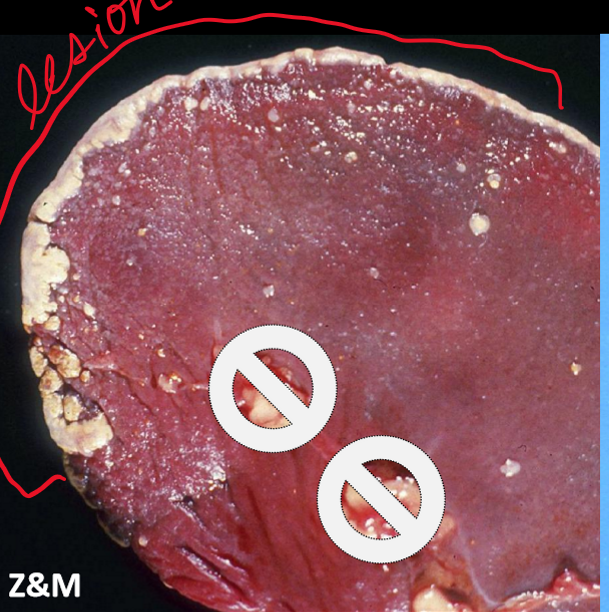
What is this, and what causes it
Hyperplasia of bone marrow
Loss of red blood cells/ platelets due to hemorrhage, hemolytic anemia, etc
Inflammatory stimulus from liver abscess, pneumonia, etc.
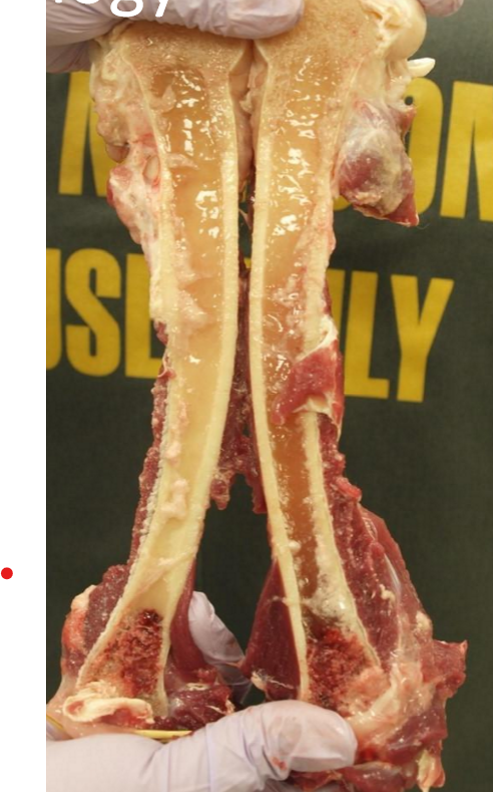
What is this, and what causes it
Serous atrophy of fat (gelatinous transformation of fat)
From cachexia or starvation → the fat is metabolized, bone marrow reticular cells produce mucoid substance to replace

What is this, and what causes it
Neoplasia
Myeloid/lymphoma (leukemia, lymphoma, multiple myeloma)
Non-myeloid/lymphoid (hemangiosarcoma, metastatic neoplasia)

What is this, and what causes it
Infection → osteomyelitis, myelitis
What are the 3 main functions of the thymus
Differentiation, selection, and maturation of T cells
T cell receptor rearrangement
Positive selection (MHC binding)
Negative selection (self-reactive)
only 2% of T cells exit the thymus
3 zones of the thymus
Subcapsular: T-cells from the bone marrow enter the thymus
Cortex: positive/negative selection, and TCR rearrangement
Medulla: negative selection
2 main types of cell in the thymus
Lymphocytes
Epithelial cells (hassall’s corpuscles)
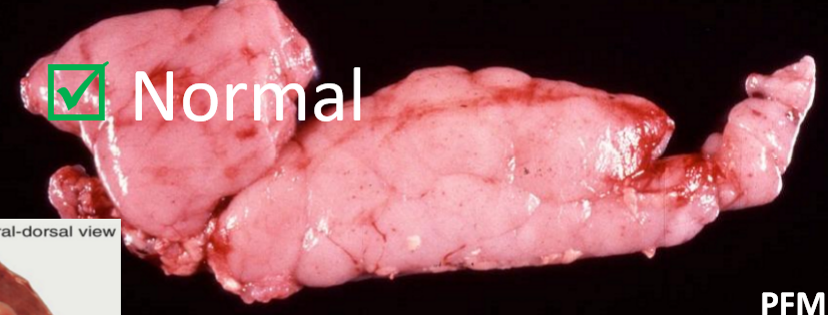
What does a normal thymus look like on gross pathology
Located intrathoracic mediastinum cranial to the heart and ventralto trachea, in ruminants sometimes cervical
Is pink and lobulated in a young animal, involutes as the animal ages (shrinks) when sexual maturity approaches
When would you suspect a lesion in the thymic resion
Masses in the region, diffuse expansion of the thymus
How will a thymic lesion be detected in small animals?
Respiratory symptoms, look at thoracic radiographs
Intrathoracic mediastinal masses/cysts, or hemorrhage
Detection of paraneoplastic syndromes
How will thymic lesions be detected in large animals
Cervical swelling (masses, cysts)
What are some reasons for absent or small thymus
Involution (PHYSIOLOGICAL)
Inadequate nutrition
Stress (increased glucocorticoids)
Infectious agents (virus)
Intoxicants (leads, mercury)
Medical treatment (radiation, chemotherapy)
Aplasia
What are some reasons for diffuse enlargement of thymus
Variation (physiological!)
Hyperplasia (repeated immunization)
Neoplasia (lymphoma)
What are some reasons for focal and localized enlarged thymus
Custs (persist during involution, or acquired)
Neoplasia (thymoma)
What are some reasons for an inflamed thymus
Thymitis (uncommon)
What are some reasons for hemorrhagic thymus
Etiologic vs. idiopathic
What is this
involuted thymus (should be tightly packed)
What is this
panleukopenia thymus
No obvious cortical/medullary distinction
What are 3 important features of signalment/history for thymic hemorrhage
age
access to rodenticide
trauma
What are 3 common differential diagnoses for thymic hemorrhage
idiopathic hemorrhage
anticoagulant toxicity (rodenticide)
traumatic hemorrhage
What are some antimortem diagnostic tests for thymic hemorrhage
cbc
clotthing time
What is a proposed pathogenesis to spontaneous idiopathic thymic hemorrhage
Thymic involution (this MUST be occuring) → thin walled vessels, no longer with structural support from adjacent parenchyma → slight trauma or sudden increase in BP → hemorrhage
This is a diagnosis of exclusion, must first rule out toxicitiy and trauma
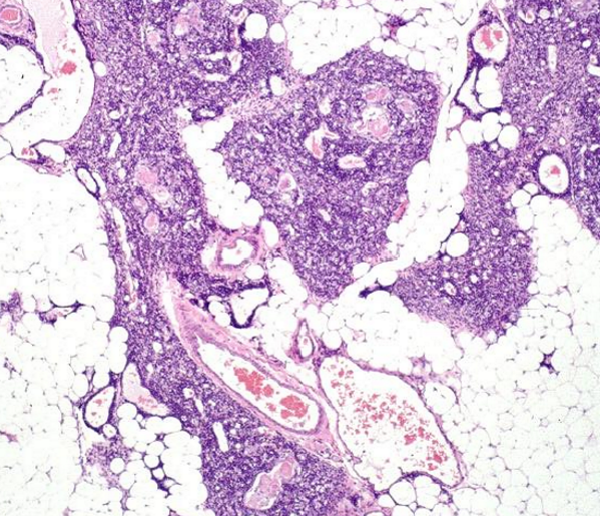
What are the main histologic findings here
Absence of any evidence of thymic involution
extensive hemorrhage
Distinct cortical medullary distinction
Pathogenesis of rodenticide toxicity
Ingestion of anticoagulant rodenticide → Vit K deficiency → clotting factors consumed without replacement → hemorrhagge
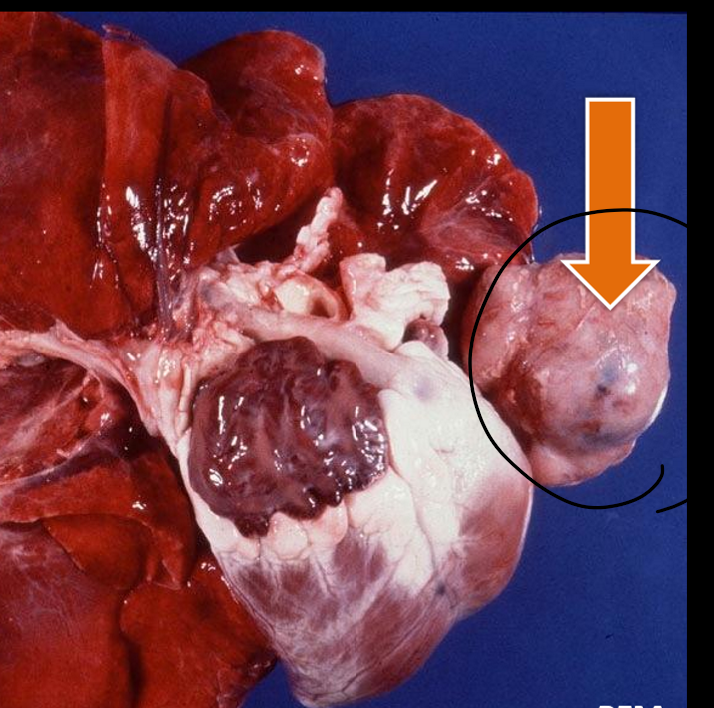
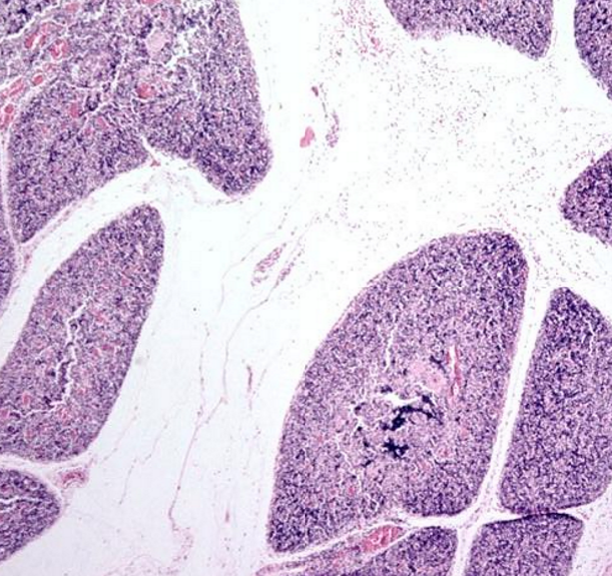
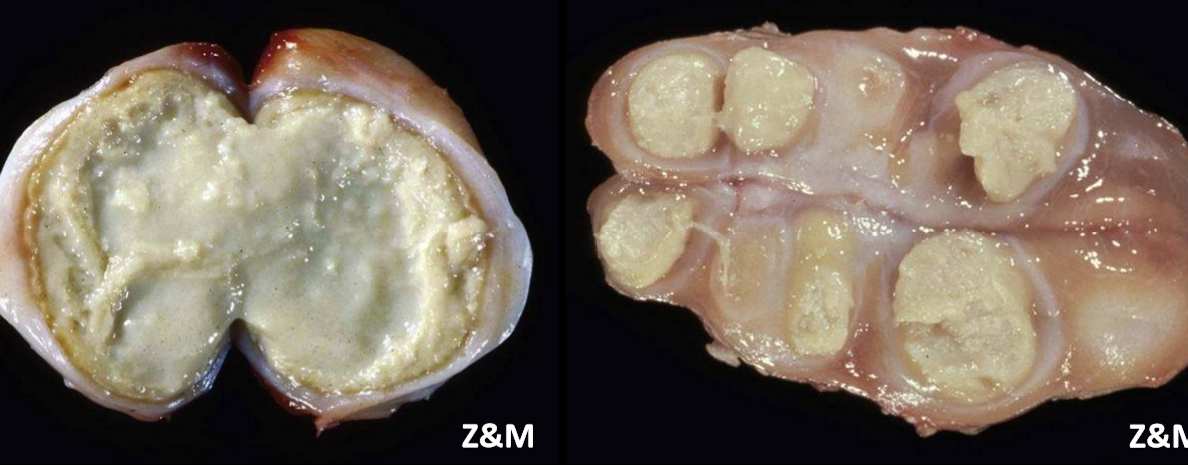
What is this
thymoma
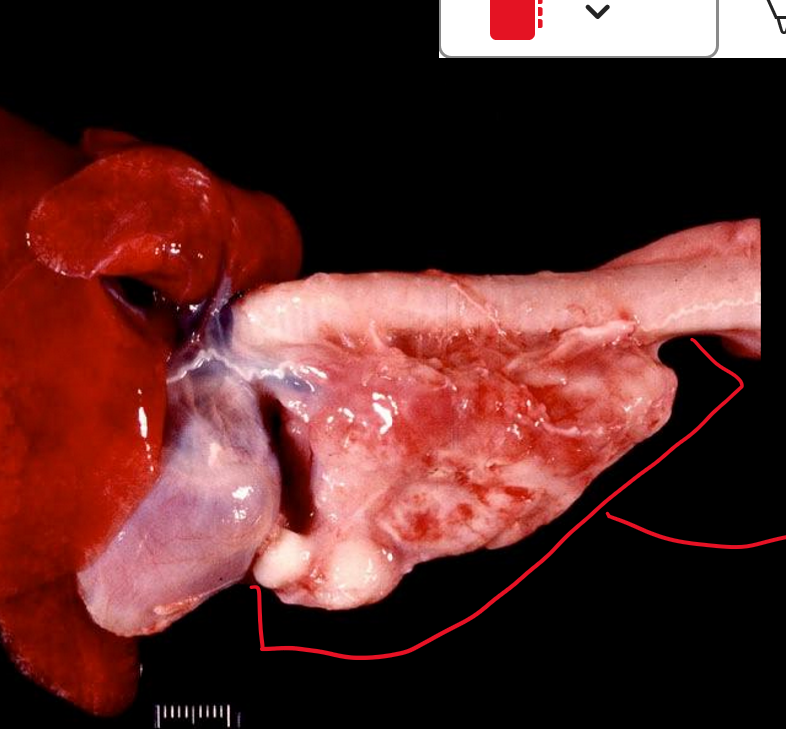
What is this
lymphoma
What are the two types of thymic neoplasia
Thymoma, thymic carcinoma
Lymphoma
(generally uncommon)
How to differentiate thymoma and lymphoma
Thymoma → focal, localized, with epithelial or lymphoid tissue
Lymphoma → diffuse
Paraneoplastic syndromes of dogs and cats
Dogs = myasthenia gravis
Cats = exfoliative dermatitis
What is the pathogenesis of thymoma to secondary myasthenia gravis in dogs
Thymoma → autoantibodies develop against thymic myoid cells, which have Ach receptors → antibodies in systemic circulation → binds to AchRs on postsynaptic membrane at the neuromuscular junction → prevents Ach from binding → prevents muscle contraction → muscle weakness
3 min causes of thymitis (rare)
Porcine circovirus type 2 in pigs
Epizootic bovine abortion": foothill abortion in cattle
Salmon poisoning disease in dogs (neorickettsia helminthoeca)
Cell types in the stroma of spleen
endothelium
smooth muscle cells
fibroblasts
cell types of red pulp in spleen
erythrocytes
histiocytes (macrophages)
The function of red pulp in the spleen
Innate immune function
Storage
extra medullary hematopoiesis
Cell types in the white pulp of the spleen
lymphocytes
histiocytes (dendritic cells)
What is the function of the white pulp in spleen
Adaptive immmune function
When would you suspect a splenic lesion
Patient with hemoabdomen
Abdominal imaging shows splenic mass, or splenomegaly
What are some reasons for bloody nodules in the spleen
Neoplasia
Hematoma
Acute infarct
What are some reasons for enlarged nodule in the spleen
Neoplasia
Abscess/granuloma
Nodular hyperplasia
Non-acute infarct
Siderotic plaques
What are some reasons for extra, or multiple spleens
Ectopic
Fracture
Splenosis
What are some reasons for diffuse bloody spleen
Acute septicemia/infection
Barbituates
Volvulus/torsion
Acute IMHA
What are some reasons for diffuse enlargement of the spleen
Neoplasia
Extramedullary hematopoiesis
Phagocytosis
Storage material
Chronic IMHA
Subacute/chronic infection

What is this
splenic venous infarct, acute
What is this
splenic infarct, chronic and fibrosing
What is this
Siderotic plaques
BENIGN common splenic lesion in dogs

What type of histiocytic sarcoma is this (+ ddx)
Macrophagic histiocytic sarcoma → is diffusely meaty, in red pulp
lymphoma and amyloidosis are ddx when examining grossly
What type of histiocytic sarcoma is this (+ ddx)
Dendritic cell → in follicles, and nodular
Metastatic neoplasia and abscesses are ddx when examining grossly
2 main reasons for bloody splenic nodules
Hematoma (can occur secondary to other lesions)
Hemangiosarcoma
4 main reasons for meaty splenic nodules
Primary neoplasia → benign (myelolipoma, follicular lymphoma), malignant (splenic sarcoma, lymphoma, histiocytic sarcoma)
Metastatic neoplasia
Nodular hyperplasia
Granuloma/abscess
What is a reason for a raised lesion (but not nodules)
Acute infarct (bloody)
Non-acute infarct (meaty)
Siderotic plaques (meaty)

What is this, and what are some differential diagnoses
barbituates
volvulus
acute septicemia (extra blood incoming)

What is this, and what causes it
Amyloidosis of spleen
From buildup of amyloids in extracellular space
Bloody, diffuse reasons for splenomegaly
Acute septicemia/infection
Barbituates
Volvulus/torsion
Acute IMHA
Acute infectious disease
Meaty, diffuse reasons for splenomegaly
Neoplasia (histiocytic sarcoma macrophage, lymphoma)
Phagocytosis
Chronic IMHA
Amyloidosis
Chronic infectious disease
Extramedullary hematopoiesis
What is splenosis
Acquired, autoimplantation of splenic tissue into other places
can be from trauma, with seeding of splenic tissue
What are 3 functions of lymph nodes
lymph filtering
Surveillance and processing incoming antigens
B-lymphocyte maturation, plasma cell development
What are the main regions of the lymph node
Cortex → lymphoid follicles
Paracortex → diffuse lymphoid tissue
Medulla → cords of lymphocytes/plasma cells and macrophages
Sinuses → lymph (subcapsular, paratrabecular, medullary)
What are some ways an animal with lymph node lesions will present
Multiple enlarged peripheral lymph nodes → painful or painless
Single enlarged peripheral lymph node → painful, painless
Multiple, or single enlarged internal lymph nodes, identified with medical imaging
Some reasons for small lymph nodes
Immunodeficiency
Cachexia/malnutrition
Aging
Viral infection → other than RETROVIRUSES
Radiation
What are some reasons for multifocal/focal enlarged lymph nodes
Metastatic neoplasia
Follicular hyperplasia
Aute/chronic lymphadenitis
Granulomatous
Caseous
Abscessation
What are some reasons for diffuse enlargement of lymph nodes
Viral infection of RETROVIRUS only
Primary neoplasia
Diffuse hyperplasia
Acute/chronic lymphadenitis
Sinus histiocytosis
Reasons for lymphadenomegaly OR lymphadenopathy in whole body vs. focal
systemic infection/inflammation/neoplastic process vs. localized infection/inflammation/neoplastic process

What is this, and what are some reasons for it
Sinus histiocytosis/macrophage hyperplasia
Due to response to draining antigens
Draining from catchment area
What is lymphadenitis
Non reactive hyperplasia of lymph node: inflammation has taken over
Acute and subactue lymphadenitis leads to chronic
How does strangles affect the lymph nodes
Streptococcus equi subsp. equi
Affects mandibular and retropharyngeal lymph nodes
When it spreads to abdominal lymph nodes → called bastartd strangles
Lymphadenitis from peripheral lymph nodes leads to liquefactive necrosis, which drains to abdomen/lungs, etc
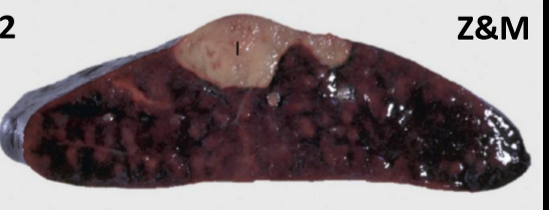
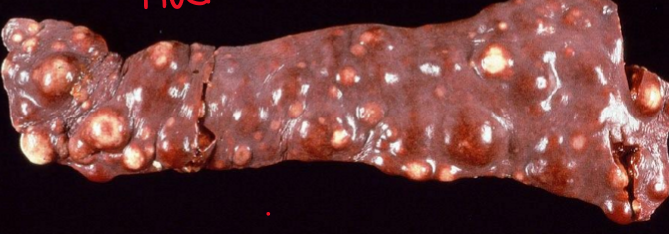
What is this and its pathogenesis
Caseous Lymphadentitis
skin wound (shearing in sheep) → Corynebacterium pseudotuberculosis penetrates skin → drains to regional lymph node → systemic circulation → localizes to internal lymmph nodes, lungs, spleen
What is this
granulomatous lymphadenitis
What are some causes of granulomatous lymphadenitis (infectious)
Corynebacterium pseudotuberculosis in sheep/goats
Rhodococcus equi in horses
PCV-2 in pigs
Mycobacterium bovis/avium complex in cattle
Mycobacterium paratuberculosis (Johne’s disease) in cattle
Fungal infection of various species → aspergillosis, histoplasmosis, blastomycosis, cryptococcosis
Feline infectious peritonitis in cats
2 neoplasias of the lymph node
Lymphoma → neoplastic lymphocytes forming solid tumors, secondary leukemia
Leukemia → neoplastic lymphocytes in bone marrow and blood, secondary formation of solid tumors
What is this
canine or feline lymphoma
LN is bulging and there is no cortical/medullary distinction
What are the features of sporadic bovine lymphoma
Not bovine leukemia virus
Multicentric → calves <6 months, in LN, organs, bone marrow
Thymic → 6-24 months, massive thymic enlargement
Cutaneous → 6-24 months, multifocal skin tumors
What are the features of enzootic bovine leukemia
From bovine leukemia virus
Multicentric: 4-8 years
widely distributedin LNs
In uterus, abomasum, myocardium
Lymhpoid tissue behind eyes, and in CNS
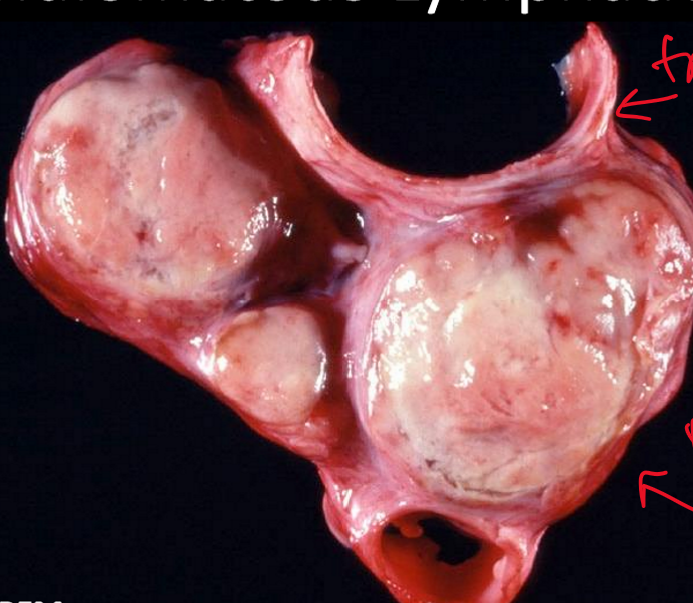
3 types of equine lymphoma
alimentary/internal → GI and regional LN, liver, spleen, peritoneum
Multicentric → peripheral LN, abdominal LN, mediastinal mass
Cutaneous

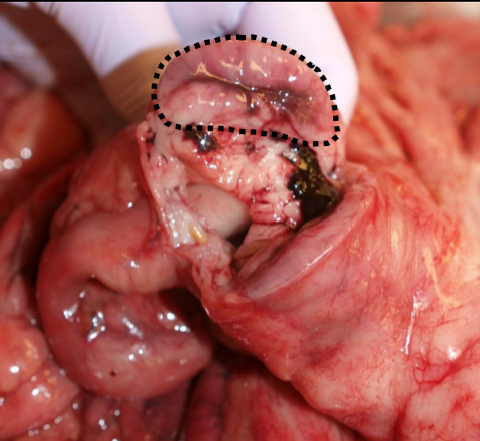
What is this
equine lymphoma
What is the normal function and characteristics of lymphatics
Transporting lymph
Grossly, not typically visible
Histologically, endothelial lined vessels, which are difficult to differentiate from veins
4 main types of lymphatic lesions
Lymphedema: accumulation of fluid in tissue secondary to blockage/damage (obstruction not common, arteriovenous shunt)
Lymphangitis: infection/inflammation of lymph vessels (usually occurs with lymphadenitis, secondary lesion)
Lymphangiectasia: abnormally dilated lymph vessels (developmental)
Acquired → obstruction, but usually idiopathic
Protein losing enteropathy clinically, with dilated lacteals
Lymphangiosarcoma: neoplasia of the lymphatics
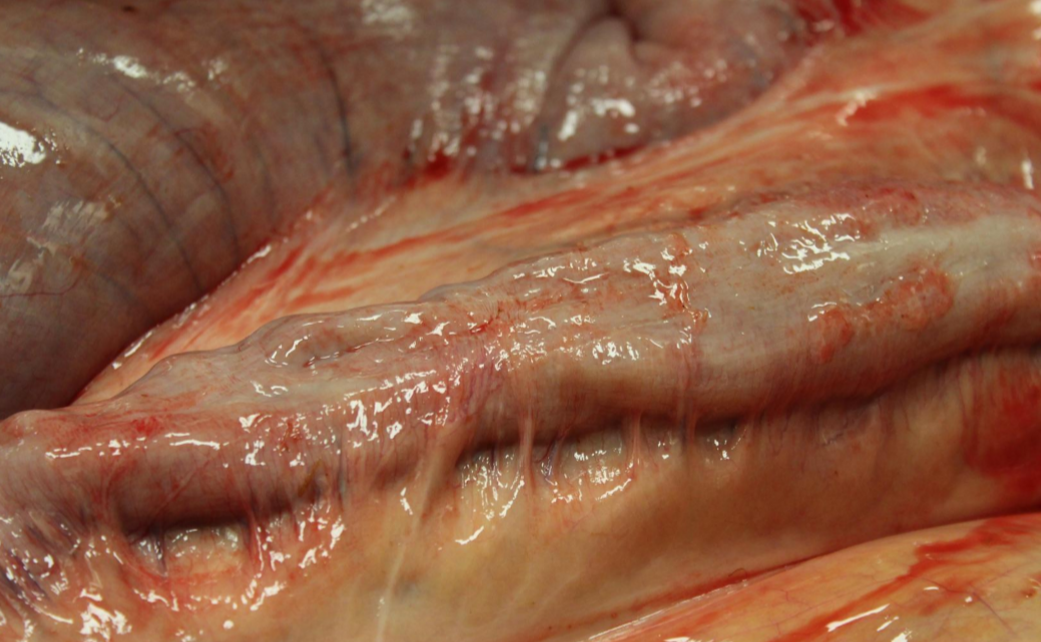
What is this
Lymphangitis, Johne’s Disease
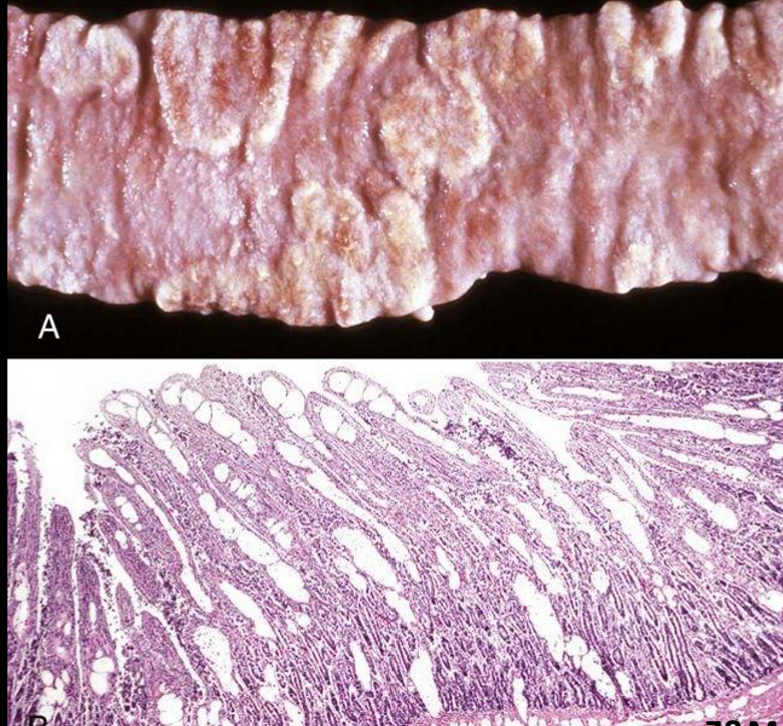
What is this
Lymphangiectasia
Lacteals in the middle of villi are very extended, not allowing absorption of proteins (PLE)
What is the function of MALT
Acts as sentinels, protecting mucosal barriers
B-cell development in Peyer’s patches (ruminants) and bursa of fabricius (birds)
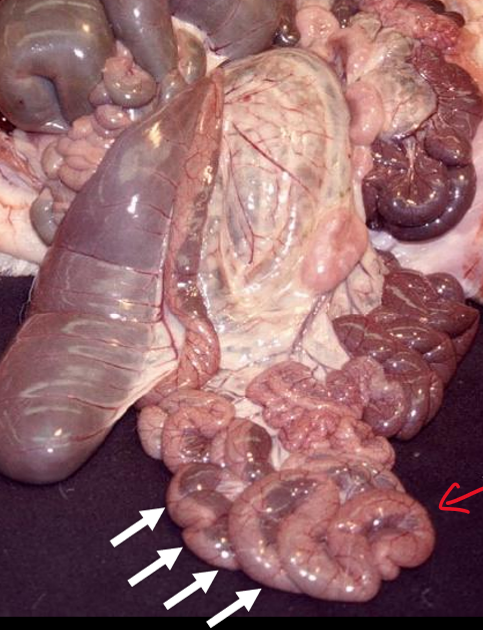
What is this
Peyer’s patches in ruminant
continuous strip of lymphoid tissue in goat intestine
What causes atrophy of MALT
viral infection, malnutrition/cachexia, aging, chemo, radiation
What causes hyperplasia of MALT
antigenic stimulation