Systems Path Section 6 - Obstructed Lung diseases (pg 1-53)
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
what is an indication of tissue hypoxia?
nail clubbing
hallmarks of all obstructive lung diseases
wheezing, normal FVC, reduced FEV1
obstructive lung disease characterized by destruction of alveolar septa in central area of acinus
emphysema
signs and symptoms of emphysema
enlarged acini -> dyspnea, wheezing, cough, weight loss, barrel chest
those with emphysema are described as what?
pink puffers
how does emphysema develop?
deceased elasticity of alveoli associated with destruction, enlargement, collapse due to increase ROS and protease activity
who/why would someone get emphysema?
smoking
MC type of emphysema which destroys central acinus
centriacinar
what type of emphysema is characterized by uniform acinus destruction and is due to a1-antitrypsin deficiency
panacinar
obstructive lung disease characterized by excessive mucous production, chronic coughing, wheezing, frequent infections, weight gain and cyanosis
chronic bronchitis
how would you diagnose someone with chronic bronchitis?
productive cough (3+ months for 2+ consecutive years)
how would someone get chronic bronchitis?
irritant causing mucus hypersecretion and decreased mucociliary clearance
who is most likely to get chronic bronchitis and why?
males 40-65 with history of smoking/exposure to irritants
those with chronic bronchitis are referred to as what?
blue bloaters
chronic bronchitis + emphysema
chronic obstructive pulmonary disease (COPD)
risks associated with developing COPD
smoking and air pollution
reversible obstructive lung disease characterized by dyspnea, coughing, and wheezing (potential death in status asthmaticus)
asthma
how does someone get asthma?
airway obstruction by bronchial sm. constriction and increase production of mucus
atopic asthma is caused by
allergic trigger and genetic susceptibility
non-atopic asthma is caused by
hypersensitivity
Asthma primarily involves difficult performing ________
exhalation
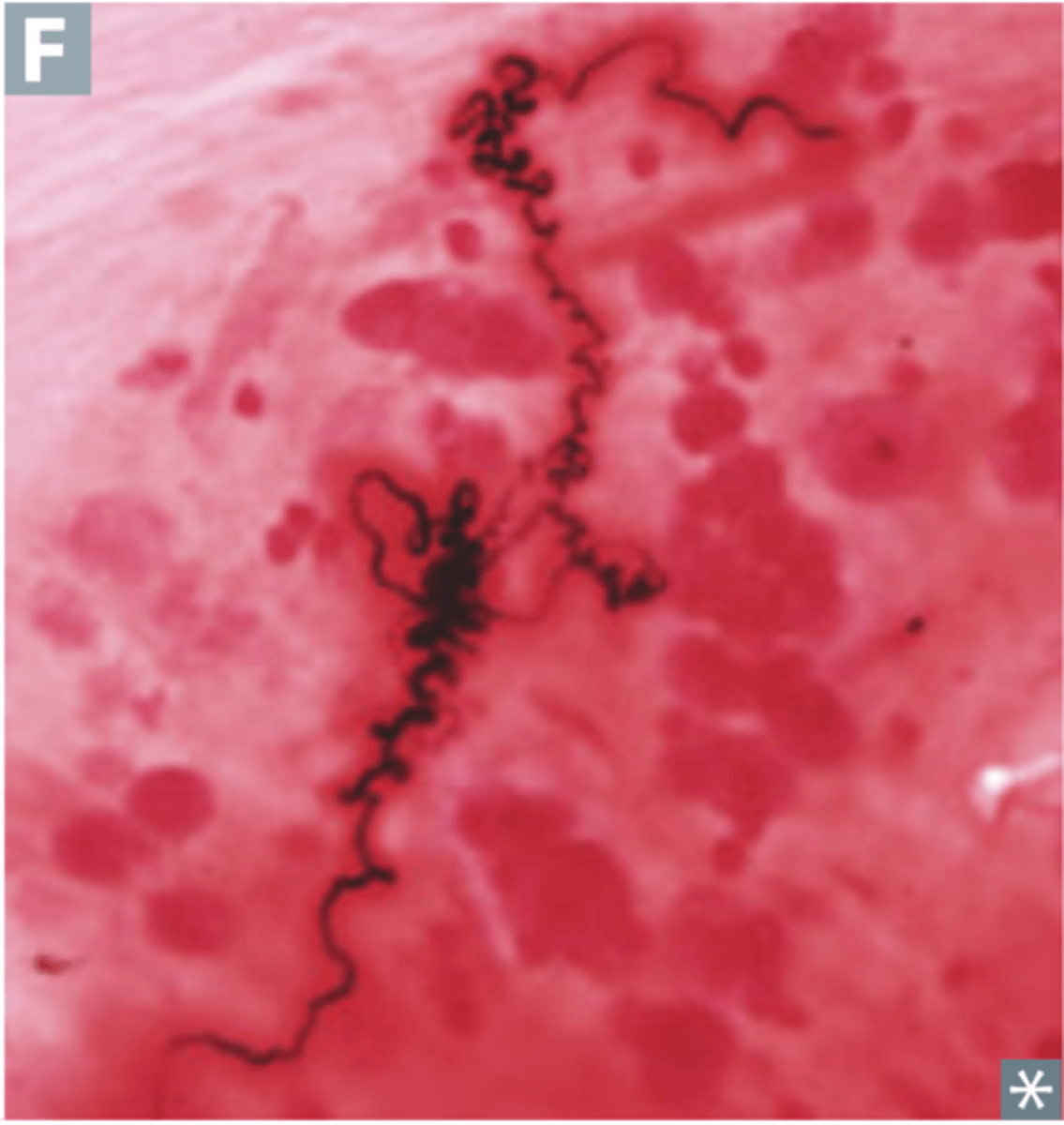
hallmarks of asthma
curschmann spirals and charcot-leyden crystals
atopic asthma
Initiated by a type I IgE-mediated hypersensitivity reaction induced by exposure to an extrinsic antigen; most common type
MC type of asthma which is childhood onset and induced by environmental antigens
atopic
what type of asthma is less common, characterized by bronchial inflammation and hyper-responsiveness to stimuli such as cold, exercise, stress
non-atopic
what type of asthma is characterized by prolonged severe wheezing/dyspnea, bronchial narrowing, and hyper inflated acini
chronic
a severe, life-threatening asthma attack that is not responsive to bronchodilators or steroids
status asthmaticus
obstructive lung disease associated permanent dilation of bronchi causing destruction of CT/musculature
bronchiectasis
How does bronchiolitis develop?
obstruction leads to necrotizing infection/destruction of airway
"tram-track" sign is associated with which pathology?
bronchiectasis
bronchiectasis signs and symptoms
severe coughing, hemoptysis, purulent foul-smelling sputum
inherited dysfunction of cilia body wide due to mutated dynein
kartagener syndrome
how does kartagner syndrome develop?
results in deceased mucociliary clearance and risks for bronchiectasis