Complex-Endocrine Part 3 DKA, HHS
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
What makes up Diabetic ketoacidosis?
hyperglycemia
Ketosis
metabolic acidosis
What does Insulin do in the body at the cellular level?
Promotes glycogenesis (not gluconeogenesis)
Promotes lipogenesis (not lipolysis)
Promotes protein synthesis (not catabolism
Inhibits glucagon release
Role in appetite regulation
What conditions does Insulin help treat clinically?
DM I, II, GD
DKA & HSS
Stress-related hyperglycemia
Treat hyperkalemia
What is Diabetic Ketoacidosis (DKA)?
Series of metabolic derangements: uncontrolled hyperglycemia, ketonemia, & acidemia
Result = abnormal metabolism of carbohydrates, fats, proteins with the production of highly acidic ketones bodies, leads to metabolic acidosis
Life threatening complication of diabetes (can lead hypovolemic shock)
Typically seen in type I diabetics
Most common acute hyperglycemic complication of type 1 diabetes mellitus
What are the causes of DKA?
Lack of Insulin
Sepsis
Sickness (Stomach virus & Flu) = most common
Stress (surgery, any source)
Skip insulin: pump failure, can be unknown
Other: Undiagnosed DM, medications
No insulin. No sugar in cell.
Fuel = ketones. Faster onset. Younger population.
Easier fix than HHS
What is the pathophysiology of Diabetic Ketoacidosis?
Lack of insulin
Lack of intracellular glucose, rise in serum BG
Gluconeogenesis (noncarbs leads to glucose)
Hyperglycemia results
Kidneys secrete excess glucose along with water & electrolytes (Na, K) = Osmotic diuresis leads to polyuria
Dehydration & electrolyte loss with glucosuria
Lipolysis leads to FFA & glycerol leads to FFA converted to ketone bodies = acidic
Metabolic acidosis results
What are the clinical manifestations of Hyperglycemia due to DKA?
Polyuria, polydipsia
Marked fatigue, weakness
Blurred vision
Headache
Orthostatic hypotension (if hypovolemic); thready pulse, tachycardia
What are the clinical manifestations of Ketosis/Acidosis due to DKA?
GI SS (anorexia, N/V/abd pain)
Palpitation, chest pain
Acetone breath (fruity odor)
Hyperventilation (why?)
Alert, lethargic, comatose
What is the most serious complication of DKA?
Cerebral edema due to rapid shifts in fluid within the brain, often resulting from the treatment of DKA, rather than the DKA itself
High blood glucose in DKA creates a high osmotic pressure in the blood, drawing water from brain cells. During treatment, rapid reductions in glucose and plasma osmolality can cause a sudden shift of water back into brain cells, leading to swelling
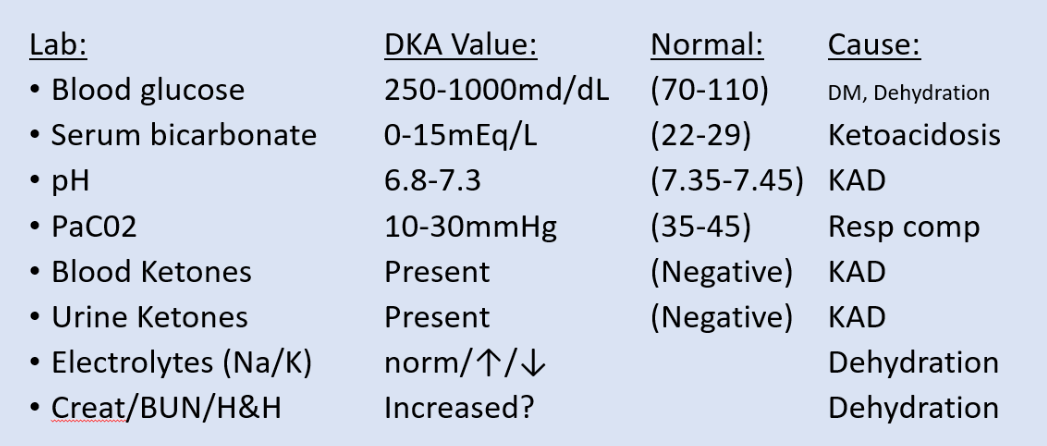
What Assessment and Diagnostic findings are seen w/ DKA?
What DKA management is needed if the pt needs Rehydration?
Fluid loss: polyuria, hyperventilation, diarrhea, vomiting
Goals: maintain tissue perfusion & promotes renal excretion of excess glucose
Treat: IVF (crystalloids)
initially 0.9% sodium chloride rapid infusion (0.5-1L/h x 2-4h)
0.45% NaCl for HTN, hypernatremia, heart failure or after first few hours
Once BG <300mg/dL, change to dextrose 5% in water (D5W)
Monitor: Frequent labs, exam, VS, I&O
Watch: peds/elderly, renal insufficiency, HF
How would you Restore electrolytes in a pt w/ DKA?
Potassium replacement asap
Rehydration may cause hypokalemia
Rehydration causes ↑UO and potassium excretion
Insulin treatment drives potassium into cells
Potassium replacement even if normal plasma levels since blood levels ↓ during DKA treatment
(contraindicated for EKG abnormalities or anuria)
Avoid hypokalemia arrhythmias
Initially frequent ECGs (q2-4h) & potassium labs
How would you reverse acidosis in a pt w/ DKA?
DKA acidosis is secondary to lipolysis
Treat with INSULIN
MOA = inhibits lipolysis (ceases ketone formation and acid build up)
Treatment: slow continuous REGULAR insulin infusion (5 units/h)
Monitor: q1h blood glucose (BG)
IVF + glucose (D5NS, D50.45%NS) for BG of 250-300mg/dL to prevent hypoglycemia
Continue IV insulin until subcutaneous insulin administered; (Goal is serum bicarb or BG level)
↑ rate/conc of dextrose IVF to prevent hypoglycemia prn & until patient eating (since BG levels corrected before acidosis)
Avoid bicarb infusion to correct severe acidosis since results in sudden drop in potassium
What makes up Hyperglycemic Hyperosmolar Syndrome (HHS)?
Hyperglycemia
High Serum Osmolality
Absence of Acidosis
What is Hyperglycemic Hyperosmolar Syndrome (HHS)?
Defined: metabolic disorder of type II diabetes secondary to relative insulin deficit caused by illness raising insulin demand
Predominantly hyperosmolality & hyperglycemia with minimal to absent ketones
because there is enough insulin present to suppress fat breakdown (lipolysis) and ketogenesis
Affects sense of awareness (altered sensorium)
Defect lack of effective insulin (insulin resistance)
Population: Older pts (50-70 years old); no known diabetic history or have DMII
Causes: infection, acute illness (eg stroke), some meds (eg thiazides), treatment (eg dialysis)
What is the pathophysiology of Hyperglycemic Hyperosmolar Syndrome (HHS)?
Severe Hyperglycemia
Blood glucose levels often exceed 600 mg/dL (33.3 mmol/L).
Unlike diabetic ketoacidosis (DKA), there is usually no significant ketosis.
The insulin level is low, but sufficient to prevent ketogenesis, which is why there's no acidosis.
Hyperosmolarity
The extremely high glucose draws water out of the cells into the bloodstream.
This leads to severe dehydration and increased serum osmolality (>320 mOsm/kg).
Osmotic Diuresis
High glucose spills into the urine (glucosuria), pulling water and electrolytes with it.
This causes polyuria, electrolyte imbalances (especially potassium), and further dehydration.
Altered Mental Status
As the brain becomes dehydrated due to hyperosmolarity, neurological symptoms arise:
Confusion
Lethargy
Seizures
Coma (in severe cases)
What are the causes of Hyperglycemic Hyperosmolar Syndrome?
infection, acute illness (eg stroke), some meds (eg thiazides), treatment (eg dialysis), stressful events
Some insulin allows sugar in cell. (no ketones).
Higher BG, more dehydration, slower onset, older population, more symptoms, higher mortality, more severe neuro symptoms. Harder fix.
What are the clinical manifestations of HHS?
Hypotension
Profound dehydration
Dry mucous membranes
Poor skin turgor
Tachycardia
Variable neurologic symptoms
Altered consciousness, seizures, weakness, hallucinations
Polyuria, polydipsia, polyphagia
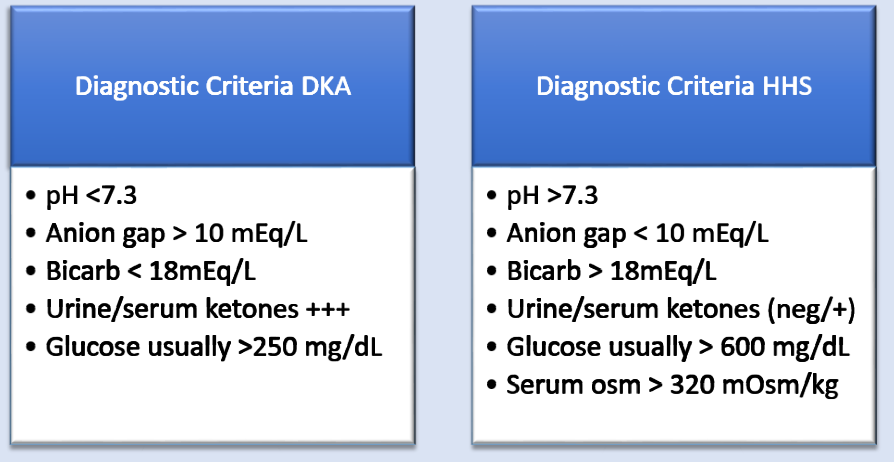
What is some diagnostic criteria differences b/w DKA/HHS?
How do you manage HHS?
Identify underlying issue
Like DKA: fluid replacement, electrolyte correction, insulin (less)
IVF: 0.9% NS then hypotonic IVF (Na level and degree of hypovolemia will dictate this)
Central venous or hemodynamic pressure monitoring guides IVF
Potassium added to IVF if good UO
Frequent labs and continuous EKG monitoring
Rehydration fixes hyperglycemia
Insulin lesser role since no acidosis
Continuous low rate with replacement dextrose IVF (once BG 250-300mg/dL)
Monitor: volume status, electrolyte imbalances, HF, arrhythmias
What Reassessment is needed for a pt w/ HHS?
Maintain fluid & electrolyte balance
BG hourly
Rehydration signs
BP, HR, cap refill,
Skin color, warm temp
UO (30ml/hr)
Low spec gravity (1.005-1.030)
What IV med is needed for managing HHS?
Potassium
Telemetry first!
Never IV push
10-20mg max/hour on pump
Site: central line and slow infusion
What insulin is needed for management of HHS?
IV insulin, REGULAR only (DKA)
Then SQ or insulin pump (HHS)
What should be monitored when managing HHS?
Fluid overload, hypo/hyperglycemia, hypokalemia, cerebral edema
Arrhythmias (K+)
What Education is needed for managing HHS?
DM self-management/care, DKA/HHS prevention, medication consistency, diet, sick day rules
Can take 3-5 days for resolution of neurologic SS (older population)
HHS treatment ongoing after metabolic abnormalities resolved
May or may not need insulin & meds after recovery
Self-management of BG is the best prevention!
Educate!