Chapter 1: Overview of Community Health Nursing
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
44 Terms
Chapter 1: Overview of Community Health Nursing
Population-focused approach: Planning, delivering, and evaluating nursing care for communities.
Broad field: Nurses practice in diverse settings with varied populations.
Goal: Promote health and welfare across the lifespan and in different cultural groups.
Management of Care
Advocacy: Use advocacy resources to support clients.
Ethical Practice
Provide care consistent with the nursing code of ethics.
Performance Improvement (Quality Improvement)
Define and participate in quality assurance/performance improvement activities.
Health Promotion and Maintenance
Health Promotion/Disease Prevention: Educate clients on actions to maintain health and prevent illness.
Health Screening: Conduct targeted screenings (e.g., vision, nutrition).
Key Takeaway
Nurses in community settings should understand:
Foundations of community health nursing
Guiding principles
Health promotion and disease prevention strategies
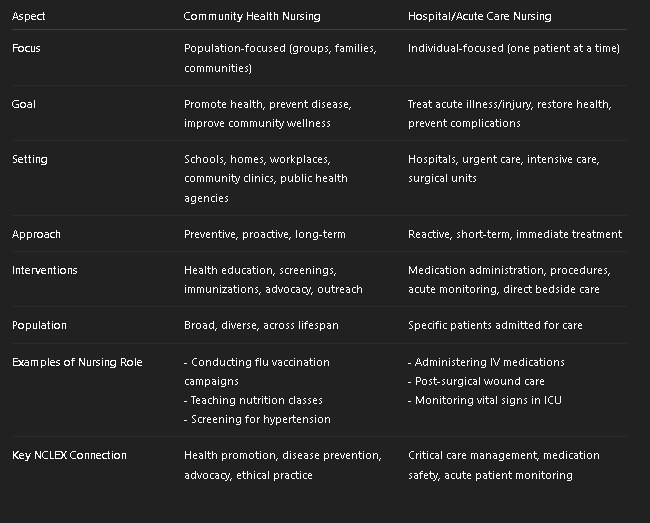
Community Health Nursing vs. Hospital/Acute Care Nursing (Table)
Population-focused (groups, families, communities)
Preventative
Individual-focused (patient)
Reactive
Foundations of Community Health Nursing
Historical Roots
Public health concepts date back to caring for the poor and displaced.
Advances in health knowledge → education of providers + regulation of water/environmental factors.
Development of Public Health Service
Established in 1798.
Early 1800s: Nursing care in homes began.
Late 1800s: Local health boards formed to:
Monitor disease
Promote health
Collect community statistics
Guiding Principles
Nursing practice in the community is shaped by:
Multiple theories
Specific definitions of care
Systems Thinking
Studies how individuals/units interact with organizations/systems (cause-effect relationships).
Upstream Thinking
Focus on prevention and health promotion (rather than treating illness after it occurs).
Health linked to environment.
Health viewed as a continuum.
Strong focus on preventive care.
Nurse emphasizes clean, safe, supportive environments.
Improve community spaces (parks, walkways, lighting) to encourage physical activity
Nightingale’s Environmental Theory
Purpose: Predict or explain health behaviors.
Focus: Individual-level change
Assumes preventive actions are taken to avoid disease.
Factors influencing likelihood of action:
Perceived susceptibility, seriousness, threat of disease.
Modifying factors: demographics, knowledge.
Cues to action: media, disease effects, advice from others.
Perceived benefits vs. perceived barriers.
Nurse addresses how people perceive obesity risks.
Educate individuals about risks of diabetes/heart disease, highlight benefits of weight loss, reduce barriers (like cost of gym).
Health Belief Model
Expands on Health Belief Model.
Focus: Community-level change
Links health deficits to lack of resources.
Behavior changes in large groups → social change.
Nurse links obesity to limited access to healthy food/exercise options.
Work with policymakers to provide affordable fresh produce, create safe walking trails, and expand school wellness programs.
Milio’s Framework for Prevention
Similar to Health Belief Model but not based on health risk.
Focus: Factors influencing health promotion & protection.
Key factors:
Personal (biological, psychological, sociocultural), behaviors, self-efficacy.
Feelings, barriers, benefits tied to the action.
Competing demands/preferences of the individual.
Nurse looks at personal factors (self-efficacy, cultural values, preferences).
Encourage clients to set personal fitness goals, highlight enjoyment of activities (sports, dance), and support confidence in making changes.
Pender’s Health Promotion Model
Concept: Change occurs gradually in stages.
Stages:
Precontemplation – Individual unaware of need to change.
Contemplation – Considers change, weighs pros/cons.
Preparation – Plans to take action.
Action – Actively makes the change.
Maintenance – Sustains behavior over time.
Termination – No longer needs conscious effort (rarely reached).
Nurse helps clients move through stages:
Precontemplation → “I don’t think obesity is a problem.”
Contemplation → “Maybe I should exercise.”
Preparation → “I signed up for a gym.”
Action → “I started going to workouts.”
Maintenance → “I’ve been exercising for 6 months.”
Transtheoretical Model (TTM) / Stages of Change (SOC)
Similar to TTM/SOC.
Precontemplation – Individual unaware of need to change.
“Unengaged” stage
Contemplation – Considers change, weighs pros/cons.
Preparation – Plans to take action.
Action – Actively makes the change.
Maintenance – Sustains behavior over time.
Termination – No longer needs conscious effort (rarely reached).
Unique feature: Includes “unengaged” stage (between being unaware and contemplating).
No termination stage
Nurse addresses people who never thought about obesity as a problem.
Precaution Adoption Process Model
Community Health Nursing Theories
Nightingale’s Environmental Theory
Health linked to environment.
Health viewed as a continuum.
Strong focus on preventive care.
Health Belief Model
Purpose: Predict or explain health behaviors.
Focus: Individual-level change
Assumes preventive actions are taken to avoid disease.
Factors influencing likelihood of action:
Perceived susceptibility, seriousness, threat of disease.
Modifying factors: demographics, knowledge.
Cues to action: media, disease effects, advice from others.
Perceived benefits vs. perceived barriers.
Milio’s Framework for Prevention
Expands on Health Belief Model.
Focus: Community-level change
Links health deficits to lack of resources.
Behavior changes in large groups → social change.
Pender’s Health Promotion Model
Similar to Health Belief Model but not based on health risk.
Focus: Factors influencing health promotion & protection.
Key factors:
Personal (biological, psychological, sociocultural), behaviors, self-efficacy.
Feelings, barriers, benefits tied to the action.
Competing demands/preferences of the individual.
Transtheoretical Model (TTM) / Stages of Change (SOC)
Concept: Change occurs gradually in stages.
Stages:
Precontemplation – Individual unaware of need to change.
Contemplation – Considers change, weighs pros/cons.
Preparation – Plans to take action.
Action – Actively makes the change.
Maintenance – Sustains behavior over time.
Termination – No longer needs conscious effort (rarely reached).
Precaution Adoption Process Model
Similar to TTM/SOC.
Unique feature: Includes “unengaged” stage (between being unaware and contemplating).
Does not include a termination stage.
Community Health Nursing
Synthesis: nursing + public health theory.
Goals: Promote, preserve, and maintain population health by delivering services to individuals, families, and groups.
Practice settings:
Community health clinics, county health departments.
Extends to environments such as homes, schools, workplaces.
Focus: population and subpopulations, not just individuals.
Builds relationships with clients while providing direct care for acute and chronic conditions.
Community
Group of people/institutions sharing geographic, civic, or social characteristics.
Varies in health needs.
Essentials of Community Nursing
Determinants of Health
Factors influencing health: nutrition, stress, social support, education, finances, transportation, housing, biology/genetics, personal practices.
Termed Social Determinants of Health (SDOH).
Health Indicators
Examples: mortality rates, disease prevalence, physical activity, BMI, tobacco/substance use.
Used to measure community health and set improvement targets.
Assessing Community Health
Nurses examine if the community’s collective needs are being met.
Core Functions of Public Health (CDC)
1. Assessment
Use systematic methods to monitor population health.
Examples:
Monitor health status to identify problems.
Diagnose and investigate health hazards.
2. Policy Development
Create laws/practices to improve population health using evidence.
Examples:
Inform, educate, empower people.
Mobilize partnerships to solve problems.
Develop supportive policies/plans.
Enforce laws → equity, protection, safety.
3. Assurance
Ensure services and workforce are available & accessible.
Examples:
Link people to needed health services.
Maintain competent public health workforce.
Evaluate service effectiveness, accessibility, and quality.
Public Health Nursing
Population-focused nursing.
Combines nursing knowledge + social/public health sciences.
Goal: Promote health & prevent disease.
Public health provides 10 essential services → includes research + 3 core functions (CDC).
1. Assessment
Use systematic methods to monitor population health.
Examples:
Monitor health status to identify problems.
Diagnose and investigate health hazards.
2. Policy Development
Create laws/practices to improve population health using evidence.
Examples:
Inform, educate, empower people.
Mobilize partnerships to solve problems.
Develop supportive policies/plans.
Enforce laws → equity, protection, safety.
3. Assurance
Ensure services and workforce are available & accessible.
Examples:
Link people to needed health services.
Maintain competent public health workforce.
Evaluate service effectiveness, accessibility, and quality.
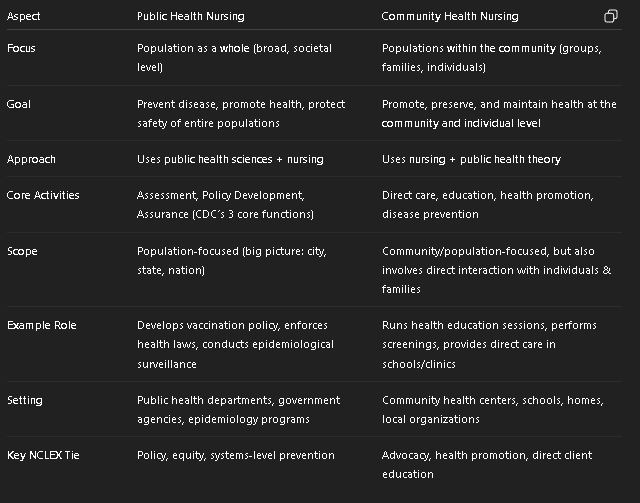
Public Health Nursing vs. Community Health Nursing
Big Picture (policy, population, prevention at societal level).
Bridge (works with populations but also touches individuals/families directly).
Determine to which of the three core functions each essential service listed below belongs.
Monitor health status
Evaluate effectiveness, accessibility, and quality of health services
Enforce laws and regulations for health and safety
Diagnose and investigate health problems
Inform, educate, and empower people
Link individuals to health services
Develop policies and plans
Ensure competent health workforce
Mobilize community partnerships
Assessment
Policy Development
Assurance
Assessment
Monitor health status
Diagnose and investigate health problems
Policy Development
Enforce laws and regulations for health and safety
Inform, educate, and empower people
Develop policies and plans
Mobilize community partnerships
Assurance
Evaluate effectiveness, accessibility, and quality of health services
Link individuals to health services
Ensure competent health workforce
Community Health Nursing (Table)
Community-Oriented Nursing
Focus of Care: Aggregates, communities, populations (public health).
Includes at-risk or underserved groups.
Primary Goal: Health promotion & disease prevention.
Nursing Activities:
Usually indirect (programs, outreach, advocacy).
May include direct care for at-risk populations.
Example: Organizing a community-wide flu vaccination program.
Community-Based Nursing
Focus of Care: Individuals & families.
Primary Goal: Management of acute or chronic conditions.
Nursing Activities:
Direct (one-on-one) care.
Illness management where people live, work, or attend (schools, homes, workplaces, camps, prisons).
Example: Providing wound care for a diabetic patient at home.
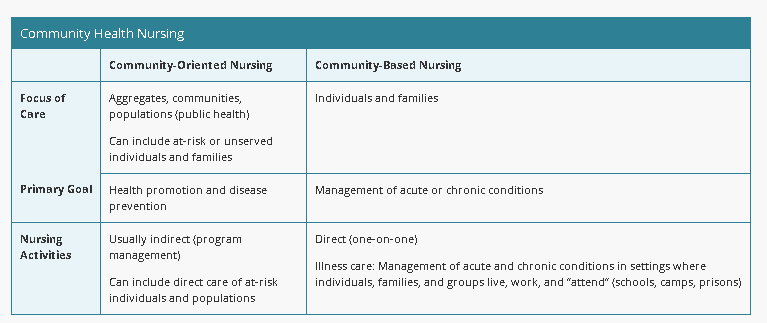
Community-Oriented Nursing (CO) vs Community-Based Nursing (CB)
Public health lens (big picture, prevention, policy, programs).
Community Overall Nursing
Bedside in the community (direct care for illness outside the hospital).
Community Bedside Nursing
A nurse manager at a community agency is developing content for an orientation program for newly hired nurses to highlight the differences between community-based and community-oriented nursing activities.
Match each nursing activity with the type of community nursing.
A home health nurse performing wound care for a client who is immobile
An occupational health nurse providing classes on body mechanics at a local industrial plant
A school nurse teaching a student who has asthma about medications
A parish nurse teaching a class on low-sodium cooking techniques
A mental health nurse discussing stress management techniques with a support group
Community-based
Community-oriented
Community-based
A home health nurse performing wound care for a client who is immobile
A school nurse teaching a student who has asthma about medications
Community-oriented
An occupational health nurse providing classes on body mechanics at a local industrial plant
A parish nurse teaching a class on low-sodium cooking techniques
A mental health nurse discussing stress management techniques with a support group
Population-Focused Nursing
Involves assessing community/population needs, protecting/promoting health, and preventing disease within groups.
Focus can be:
At-risk groups (e.g., hypertension, uninsured).
Knowledge-deficit groups (e.g., lack of health education).
Models & Partnerships
Public Health Intervention Wheel: Framework for the 10 essential public health services (from MN Dept. of Health & CDC).
Community Partnership:
Community members, agencies, businesses actively participate in health promotion & disease prevention.
Partnerships are essential for effective strategies.
Key Principles
Primary Prevention First → stop disease before it starts.
Greatest Good for the Greatest Number → prioritize population impact.
Client as Partner in Health → involve the community in decisions.
Wise Use of Resources → maximize outcomes with efficiency.
Key Principles of Public Health Nursing
Primary Prevention First → stop disease before it starts.
Greatest Good for the Greatest Number → prioritize population impact.
Client as Partner in Health → involve the community in decisions.
Wise Use of Resources → maximize outcomes with efficiency.
Public health nurses can apply ethical principles through core functions as they collect and manage information (assessment), develop policies that are in the best interest of the people in an area (policy development), and create interventions that promote healthcare equality across population groups (assurance).
Principles Guiding Community Health Nursing
Ethics
Advocacy
Evidence-based practice
Quality
Professional collaboration & communication
Ethics in Community Health Nursing
Prevent harm, do good.
Respect individual & community rights.
Support autonomy, diversity.
Provide confidentiality, competency, trustworthiness, advocacy.
Nursing Concerns
Protect, promote, preserve, and maintain health.
Prevent disease.
Balance individual rights vs community rights (ethical challenge).
Client Rights
Information disclosure.
Privacy and confidentiality.
Informed consent.
Participation in treatment decisions.
Research in Communities
Use ethical decision-making to promote and protect client rights.
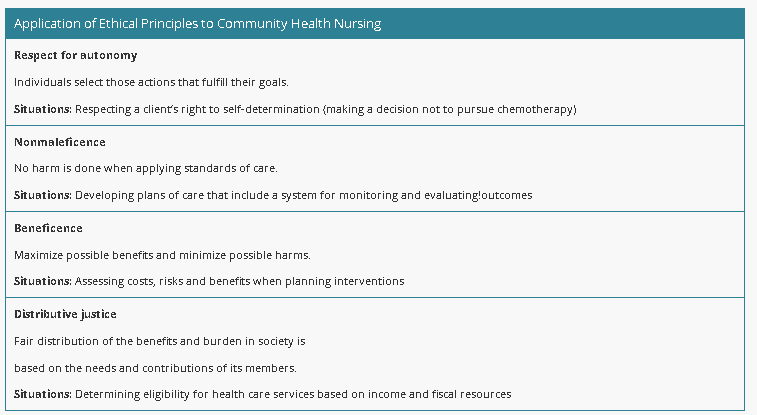
Ethical Principles in Community Health Nursing (BAND)
Beneficence
Definition: Maximize benefits, minimize harms.
Situation Example: Weighing costs, risks, and benefits before planning interventions.
Autonomy
Definition: Clients choose actions that fulfill their goals.
Situation Example: Respecting a client’s right to refuse treatment (e.g., declining chemotherapy).
Nonmaleficence
Definition: Do no harm when applying care standards.
Situation Example: Creating care plans that include monitoring/evaluating outcomes to avoid harm.
Distributive Justice
Definition: Fair distribution of benefits and burdens in society.
Situation Example: Determining eligibility for health services based on income and available resources.
Advocacy (Client Advocates) in Community Health
Nurse = informer, supporter, mediator.
Core principles:
Clients are autonomous (right to make own decisions).
Clients deserve a trust-based nurse-client relationship (respect, collaboration, shared decision-making).
Clients are responsible for their own health.
Nurses must advocate for needed resources/services.
Requires assertiveness, prioritizing client values, and persistence through chain of command.
Also at the community/population level → e.g., promoting rural access to clinics.
Evidence-Based Practice (EBP) in Community Health
Data
Nurse evaluates research for:
Quality (minimizing bias).
Quantity (number of studies/participants).
Consistency (repeatability of results).
Use the highest level of evidence (validated by peer review).
In the Community
Guides policy development, program planning, and evaluation (Assessment → Policy → Assurance)
Examples:
Media campaigns with high-level evidence for immunizations.
Using Community Preventive Services Task Force (CPSTF) guidelines for interventions.
Factors to consider:
Cost, benefit, client satisfaction, safety, cultural/demographic fit.
Some interventions effective at population level may not work for individual clients.
Contribution to research:
Nurses add to evidence by participating in community-based research.
Community-Based Participatory Research (CBPR):
Involves community partners in identifying health issues.
Encourages leadership within community.
Builds trust and collaboration.
Advocacy vs EBP
Protecting client/community rights & access.
Ensuring care and policies are backed by strong, consistent, peer-reviewed evidence.
Quality in Community Health Nursing
Assurance, improvement, and management = key to improving health care.
Promoted through:
Licensure & credentialing of providers.
Adherence to facility policies & legal guidelines.
Ongoing professional development.
Specialty certification for community health roles.
Quality report cards (managed care & public health organizations):
Contain health profiles, needs assessments, quality of life, health status data.
Nurses use them to develop/revise strategies for community care.
Example: Teaching diabetic clients about frequency of HbA1c testing.
Total Quality Management (TQM)
Approach to improve quality + performance that meets or exceeds expectations.
Continuous Quality Improvement (CQI)
Ongoing process improvement using objective data.
Applied in assessment, assurance, and policy development.
Key aspects of quality in care:
Effectiveness → provide services to those who will benefit.
Timeliness → reduce waits & harmful delays.
Client-centered → client values guide decisions.
Equity → equal care without discrimination (e.g., gender, race, SES).
Safety → prevent injuries to clients.
Efficiency → avoid waste in supplies, ideas, energy.
Total Quality Management (TQM) vs Continuous Quality Improvement (CQI)
Approach to improve quality + performance that meets or exceeds expectations.
Ongoing process improvement using objective data.
Applied in assessment, assurance, and policy development.
Uses 6 pillars of quality: Effective, Timely, Client-centered, Equitable, Safe, Efficient.
A public health nurse is reviewing the outcomes of an exercise program at various locations within a community. Which of the following aspects of care does this finding evaluate?
a
Timeliness
b
Client-centered
c
Equity
d
Safety
c Equity
Professional Collaboration and Communication
Nurses use communication to:
Care for individuals.
Collaborate in teams and groups.
Interact with other professionals.
Inform the public and stakeholders.
Nurses facilitate client communication during care transitions (one level of care to another).
Nurse leaders apply communication in mentoring, coaching, managing conflict, and supervising.
Use clear, respectful language across written, electronic, and print communication.
Adapt communication to verbal/nonverbal variations, literacy levels, and client preferences.
Bound by laws on privacy and confidentiality in all forms of communication.
Benefits
Increased adherence to treatment plans.
Reduced acute care admissions.
Lower cost of care.
Shared decision-making with clients and families.
Reduced medication errors.
A nurse is advocating for local leaders to place a newly approved community health clinic in an area of the city that has fewer resources than other areas. The nurse is advocating for the leaders to uphold which of the following ethical principles?
a
Distributive justice
b
Fidelity
c
Respect for autonomy
d
Veracity
a Distributive justice
Health Promotion and Disease Prevention
Terms often used interchangeably.
Strategies aim to:
Improve overall health.
Reduce overall disease risk.
Reduce risk for specific conditions (e.g., influenza, motor vehicle injuries).
Levels of Prevention
Primary Prevention – Prevent disease before it occurs.
Example: Vaccinations, seatbelt laws, health education.
Secondary Prevention – Early detection & prompt intervention.
Example: Screenings (BP checks, mammograms), case finding.
Tertiary Prevention – Reduce complications of established disease.
Example: Rehab programs, support groups, medication adherence teaching.
Healthy People National Goals
Direct nurses in planning strategies for both individual and community health.
Based on scientific data & trends from prior decade.
Initiated: 1979 → Updated every 10 years.
Current version: Healthy People 2030 (launched August 2020).
Coordinated by U.S. Dept. of Health & Human Services (HHS).
Provides national health objectives to guide promotion & prevention strategies.
Benefits
Improves quality of health.
Reduces healthcare costs.
Extends lifespan.
Focus
Access to health services
Adolescent health
Chronic kidney disease
Disability
Genomics
Global health
Health-related quality of life & well-being
Hearing/communication disorders
Nutrition & weight status
Older adults
Oral health
Preparedness
Family planning
Food safety
Mental health & mental disorders
Medical product safety
LGBTQ+ health
Substance abuse
Sleep health
Role of the Community Health Nurse
Help clients adopt healthy lifestyle changes (physical + psychosocial).
Provide preventive services:
Health education & counseling.
Immunizations.
Preventive medication.
Lifestyle change support.
Implement screening programs for at-risk groups.
Ensure screening programs are:
Accurate (validity).
Consistent (reliability).
Efficient (predictive value, low risk, cost-effective).
Primary Prevention
Goal: Prevent the initial occurrence of disease or injury.
Nutrition education
Family planning & sex education
Smoking cessation programs
Communicable disease education
Hygiene/health education for specific groups (e.g., daycare, food workers)
Safety education (seatbelt, helmet use)
Prenatal classes
Immunizations
Advocacy for access to care & healthy environments
Secondary Prevention
Goal: Early detection & treatment to limit severity and adverse effects.
Community health assessments
Disease surveillance (e.g., communicable diseases)
Screenings:
Cancer (breast, cervical, testicular, prostate, colorectal)
Diabetes mellitus
Hypertension
Hypercholesterolemia
Sensory impairments
Tuberculosis
Lead exposure
Genetic/metabolic disorders in newborns
Control of communicable disease outbreaks
Tertiary Prevention
Goal: Reduce disability & promote rehabilitation after disease/illness.
Maximize recovery post-injury/illness (rehab programs)
Nutrition counseling (e.g., Crohn’s disease)
Exercise rehabilitation
Case management (chronic illness, mental illness)
Physical & occupational therapy
Support groups
Exercise for chronic conditions (e.g., hypertension)
Primary vs Secondary vs Tertiary Disease Prevention
Prevent (before it happens).
Screen (catch it early).
Treat (rehab, reduce complications).
A community health nurse is planning to implement health programs with several populations in the local area.
Match the program with the level of prevention it meets.
Performing a home safety check at a client’s home
Teaching healthy nutrition to clients who have hypertension
Providing influenza immunizations to employees at a local preschool
Implementing a program to notify individuals exposed to a communicable disease
Reviewing colonoscopy screening guidelines at a community center.
Primary
Secondary
Tertiary
Primary
Providing influenza immunizations to employees at a local preschool
Secondary
Performing a home safety check at a client’s home
Implementing a program to notify individuals exposed to a communicable disease
Reviewing colonoscopy screening guidelines at a community center.
Tertiary
Teaching healthy nutrition to clients who have hypertension