Vascular pathology
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
Finish the pathway of the circulatory system
From LV: to the ____ arteries to the ____ arteries to ____ which go to ____ then to ____ to ____ then to ____ and ____
elastic arteries
muscular arteries
arterioles
capillaries
venules
small veins
medium and large veins
What is the Vasa vasorum
the “vessels of vessels” a tiny network of blood vessels which supply the walls of both arteries and veins
What’s the difference between atherosclerosis and arteriolosclerosis
atherosclerosis is the most common type of plaque formation
arteriolosclerosis affects small arteries and arterioles
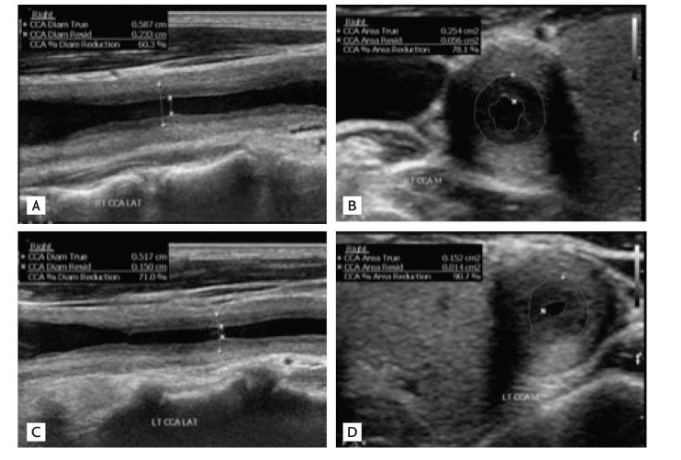
Where does atherosclerosis most commonly form at, what makes it form
-usually at the carotid bifurcation, (any bifurcation), aorta iliac system, and the CFA
formed as a result of a deposition of material in the arterial walls between the intima and media, its an accumulation of lipid containing material, smooth muscle cells, fibrin and platelets,
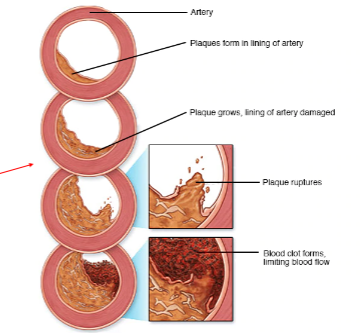
What are the types of plaque ( the atherosclerotic process)
(Fatties find cute ultrasound images )
fatty streak- thin layer of lipid material on the intimal layer
fibrous plaque- lipids become covered by more material (collagen, elastic fiber deposits)
complicated lesion- a fibrous plaque that contains fibrous tissue, more collagen, calcium and cellular debris
ulcerative lesion- the deterioration of the normally smooth surface of the fibrous cap, this gives a higher tendency to shed debris causing emboli to travel distally
intraplaque hemorrhage: plaque bleeding from within
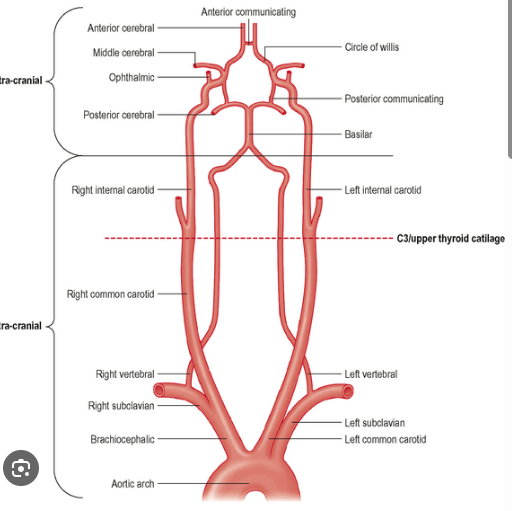
Write out the entire cerebrovascular anatomy, including the circle of willis
-remember innominate is the same as brachiocephalic
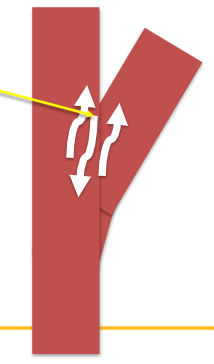
What is the boundary layer separation
at branch points where blood flow can have both forward and backward velocity components
the effective velocity is zero
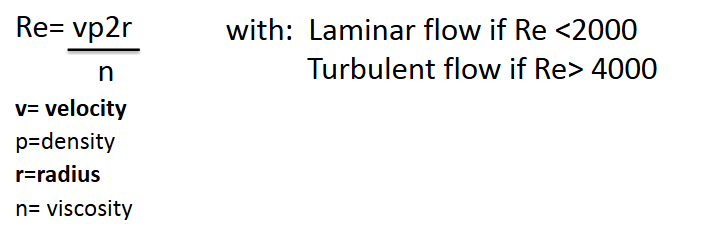
What is Reynolds number, what is it associated with
its calculates the ratio that helps predict if when fluid patterns will be turbulent
shows that turbulence depends on the size of the vessel and the velocity of the blood flow
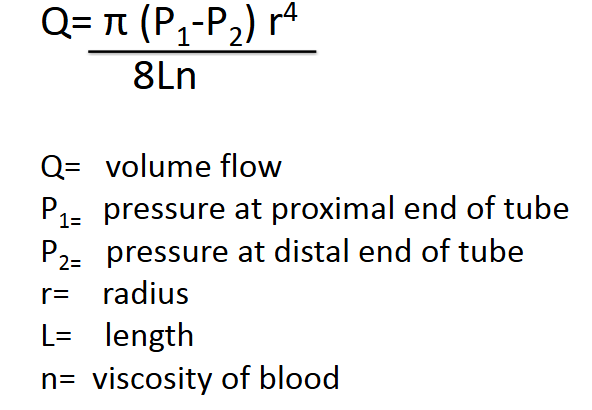
What is Poiseuille’s law and equation, what does it determine
its used to understand how vessel narrowing (stenosis) or dilation significantly affects blood flow.
discovered that a small change in radius results in a large change in volume flow ( 50% decrease in radius leads to a 95% decrease in volume flow)
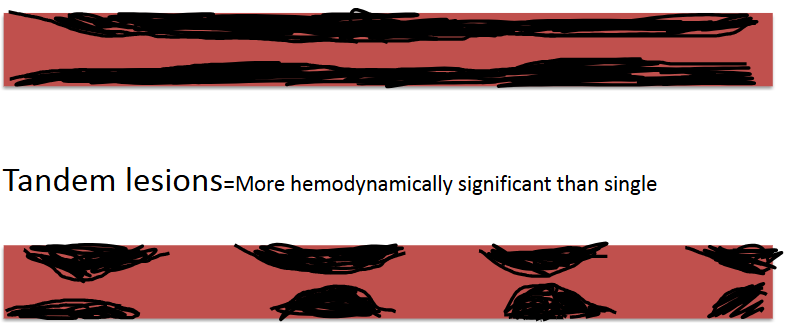
What’s the difference between stenosis and tandem lesions
tandem lesions is when there are two or more stenotic lesions occurring in a serios, they had a more pronounced effect on blood pressure and flow then a stenosis does
stenosis- single long lesion, less hemodynamically significant.
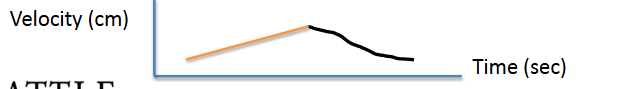
explain this waveform, where is it seen
tardus parvus: indicates a severe upstream artery stenosis or occlusion, has a slow and delayed upstroke and a low amplitude velocity.
its caused by a narrowed vessel forcing blood flow to arrive slowly and at a reduced velocity ( usually at renal, carotid, and hepatic arteries)
if a low resistive waveform becomes abnormal its ____ if a high resistive waveform becomes abnormal its ___
damped
monophasic
What does it mean if a venous waveform becomes pulsatile
indicates elevated right atrial pressure or systemic venous congestion
usually seen in conditions like right heart failure
What is the thoracic outlet, what pathology comes from this
the space created by the scalene muscle, clavicle and first rib.
Subclavian artery, Subclavian vein and Brachial nerve travel
through this space
TOS (thoracic outlet syndrome) : occurs with abduction of the patients arm. with abduction the Sub A, Sub V, and brachial nerve can become compressed the order of compression is the nerve first, vein then the artery
symptoms: Nerve only- tingling and numbness
Vein and nerve- addition of pain and swelling
Vein nerve and artery- addition of paleness and loss of pulse
use can do two exams: segmental exam: using the PPG of the digits while patient performs dynamic maneuvers
Duplex exam: evaluating the distal subclavian artery while patient performs dynamic maneuvers
TOS maneuvers
90 degrees to the side ( arms in a T)
180 degrees from sides ( arms in a I)
Military stance ( arms pulled back at sides with elbows bent)
adsons- arms at 90 degrees with head turned toward arm, then away from the arm being tested
symptomatic position: the position the patient feels symptoms.
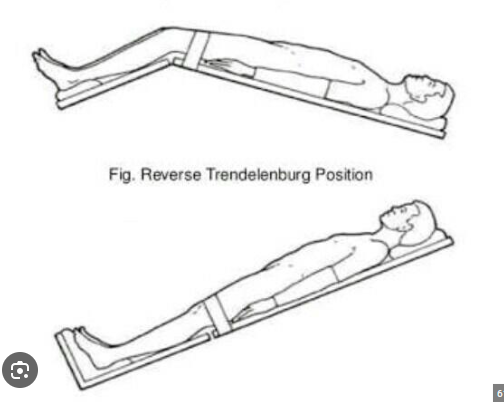
What position is Trendelenburg and reverse Trendelenburg
Trendelenburg: head lowered with legs in the arm
Reverse Trendelenburg: head up with legs down ( shown in image)
reverse Trendelenburg is better for venous exams to get blood flowing to your legs better.
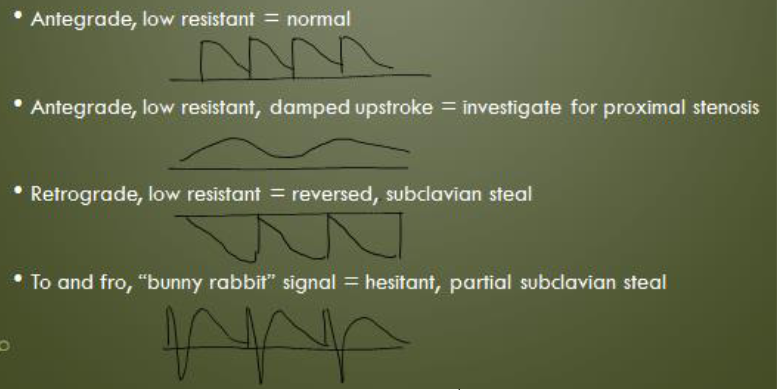
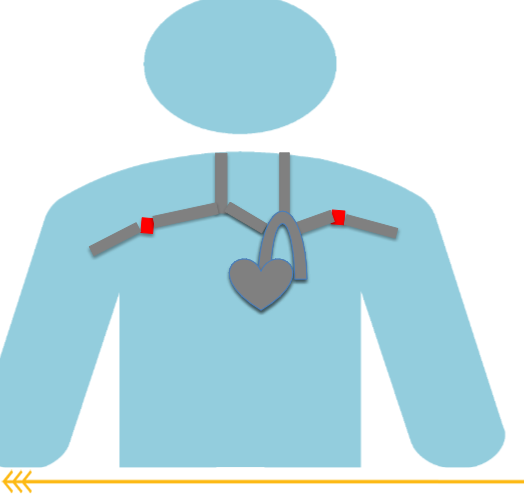
What is subclavian steel, when does it occur
occurs when a significant stenosis is in the subclavian artery proximal to the vertebral artery
this decreases the pressure in the subclavian artery causing the vertebral artery to change direction (retrograde)
for diagnosis you need a hemodynamically significant stenosis in subclavian, damped waveforms distally
a greater than 20 mmHg difference between right and left brachial BP
hesitant or reversed flow in the vertebral artery

What causes arterial dissection what is it?
the intimal layer tears and separates from the arterial wall
common causes: genetic diseases like marfans or ehlers- danlos
atherosclerosis
FMD
neck trauma
HTN and smoking increase risk
Patients may be asymptomatic or describe neck pain, coughing or dizziness
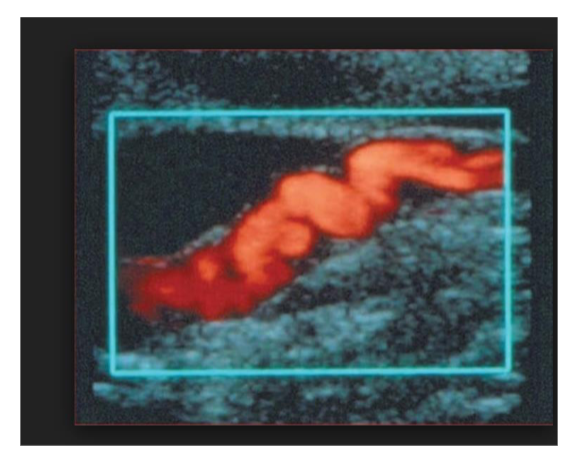
Whats FMD, fibromuscular dysplasia, what does it mostly affect
more likely in young women (25-50)
usually occurs in the ICA, renal artery, brachial, iliac and femoral
FMD is an overgrowth of the smooth muscle cells and fibrous tissue in muscle walls
patients usually have HTN due to decreased renal artery blood flow
has a string of pearls appearance, occurs mid to distal vessel, at least 1 cm from bifur. creates tandem stenosis effect within vessel. Common differential with vessel tortuosity.
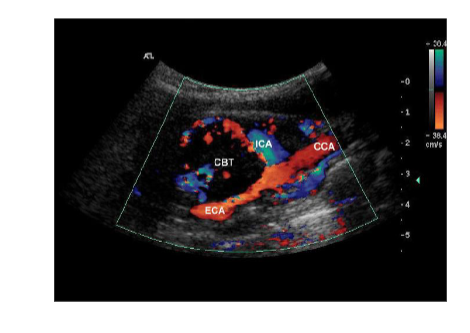
What causes a carotid body tumor (CBT) what is it?
its a tiny structure that controls PH, blood gas and BP, located at the carotid bifurcation
presents with palpable neck mass and headache, if untreated can cause stenosis, occlusion or rupture
On ultrasound it will bow out at the ICA and ECA bifurication
What is Moya Moya (MMD) who does it usually effect
rare progressive arterial occlusion of arteries in the basal ganglia section of the brain ( has puff and smoke appearance on angio)
not really seen on ultrasound but if u have a stenosis at the end of ICA and or the initial segment of the ACA and/or MCA
Usually affects children or young adults with a TIA or CVA as the first symptom
What is Takayasu’s arteritis, how does it look on ultrasound
rare vasculitis that affects large arteries ( aorta and branches)
this inflammation can cause narrowed or blocked vessels or aneurysms
more common in females, also known as pulseless disease due to lack of palpable extremity pulses
A >___ mmHg difference between left and right brachial systolic blood pressure is indicative of a hemodynamically significant stenosis on the ___
BP side
>20 mmHg
lower
this is because within a stenosis velocity increases and blood pressure decreases
If there is a hemodynamically significant stenosis or occlusion within a vessel, the blood pressures will decrease ____ to the stenosis or occlusion
distal
Lack of blood flow results in symptoms of 5 Ps in end vascular bed what are they
(Pain, Pallor, Paresthesia, Pulselessness, Paralysis)
What is Raynauds?
which the digital arteries become vasospastic
– Vasospasm (“vessel contraction”)
– Arteries close in response to cold, vibration, or emotional stress
– Often occurs bilaterally
– Can involve fingers and/or toes
Symptoms include skin changes (such as paleness, bluish discoloration, or dark red discoloration), numbness and pain
what is angioplasty and stent, where is it used and why
When a stenosis is found, physicians can use a catheter based procedure to insert a balloon to open the artery and reduce the plaque in the artery (angioplasty)
Stents enter artery compressed Then are opened with a balloon, Balloon is then deflated and stent remains
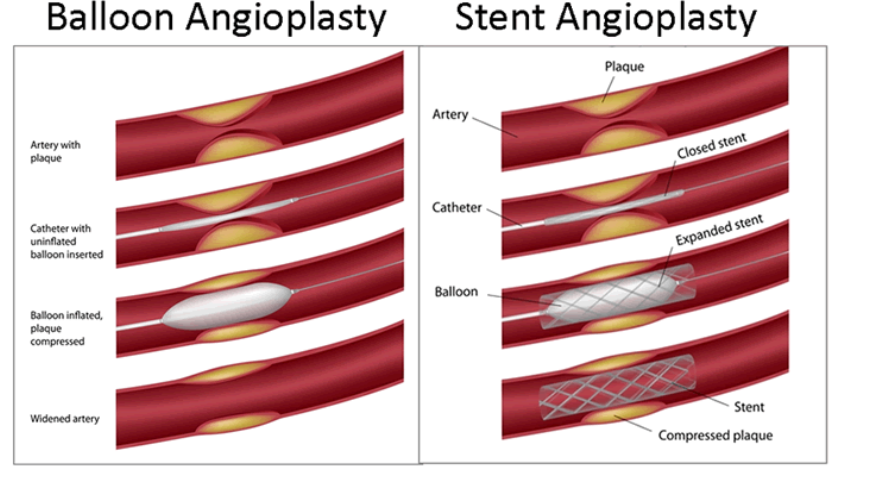
what’s the difference between Angioplasty/Stent and a Bypass Graft
When an artery becomes occluded, catheter based procedures are no longer possible, physician must then treat arterial insufficiency with bypass graft
– Graft a creation of a new arterial route for the patient
Bypass grafts connect patent artery proximal to occlusion to patent artery distal to arterial occlusion
what are the common UEA Bypass Grafts
Carotid to Subclavian (to revascularize patient with proximal subclavian occlusions)
Brachial artery to radial or ulnar artery (to revascularize patients with brachial artery or proximal radial or ulnar artery occlusions)
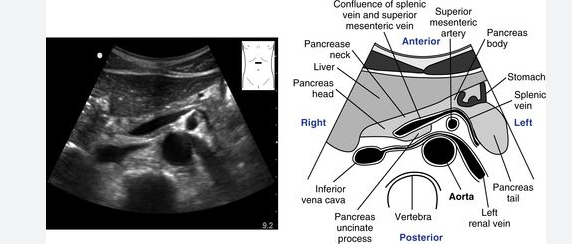
write down the anatomy.