3.1.1, 3.1.2, 3.1.3, 3.1.4 Nosocomial Nightmare
1/70
Earn XP
Description and Tags
hi <3
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
Epidemiologist
health care experts who study trends in health issues in populations and deploy public announcements, education initiatives, and protocols to protect the health of the nation.
role is a lot like that of a detective
investigate health-related matters such as disease outbreaks and chronic illnesses by:
gathering information
examining data
looking for patterns
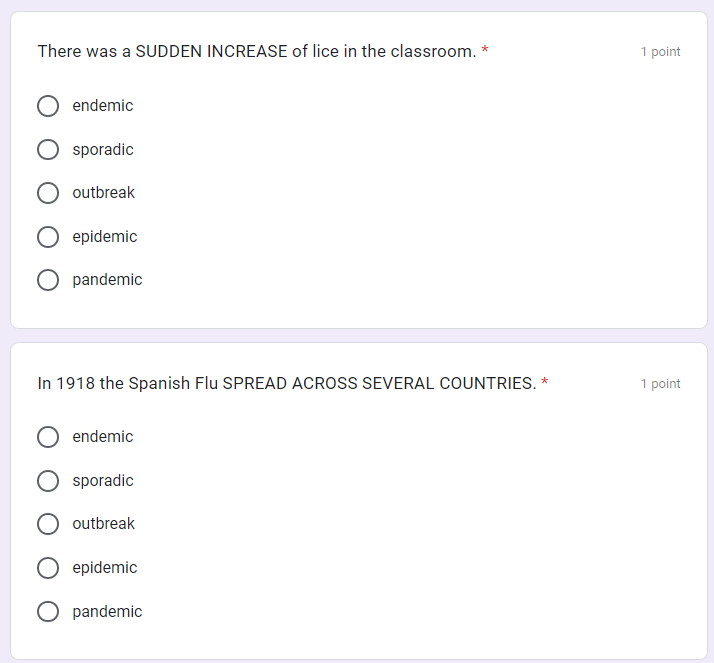
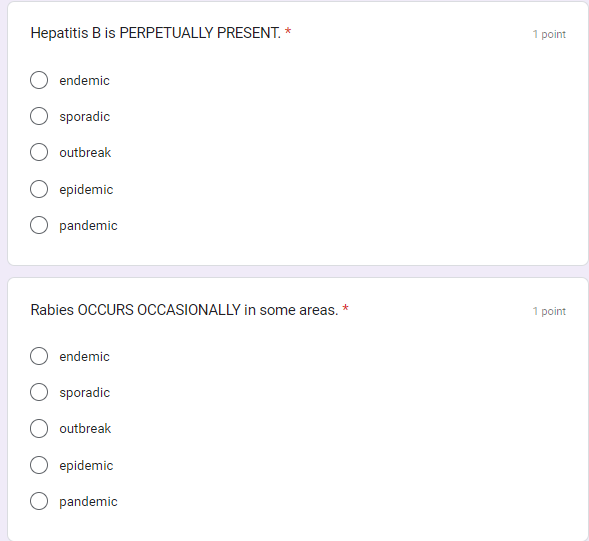
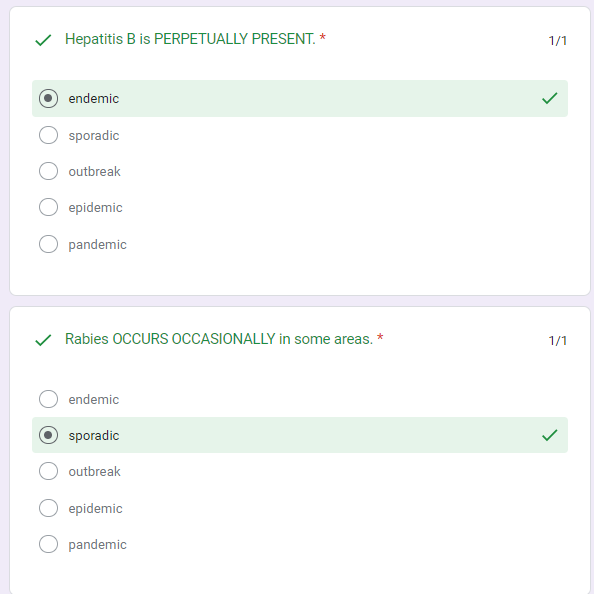
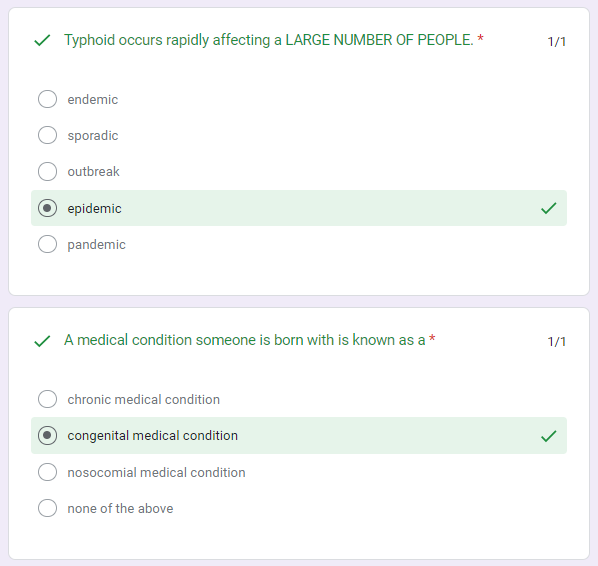
Endemic
a disease perpetually present in a community or population within a specific geographic area. Malaria is endemic to parts of Africa, South America, and Asia
sporadic
a disease that occurs only occasionally. E.coli infections caused by eating tainted food...these occur now and then (and are usually in the news)
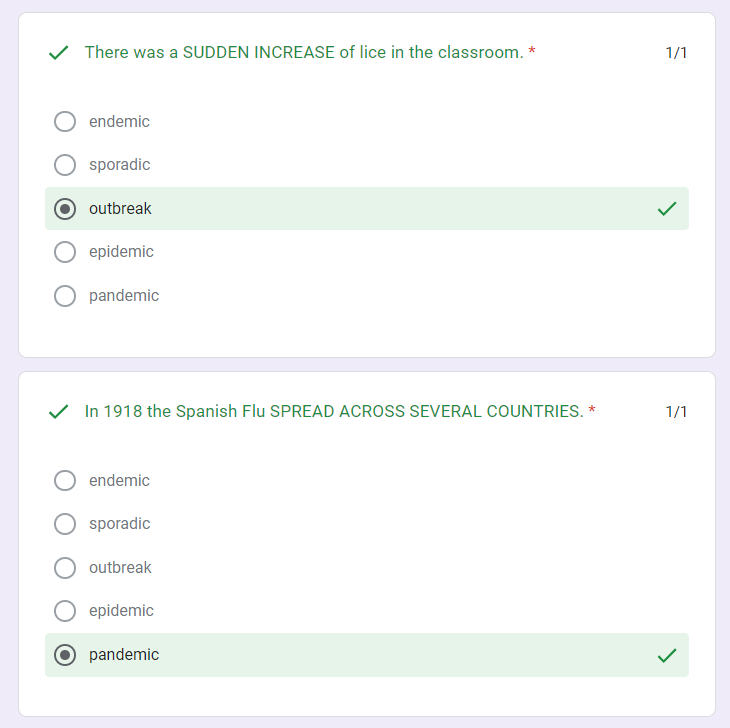
outbreak
A sudden increase in the occurrence of a disease in a localized area. The common flu can spread rapidly through a community
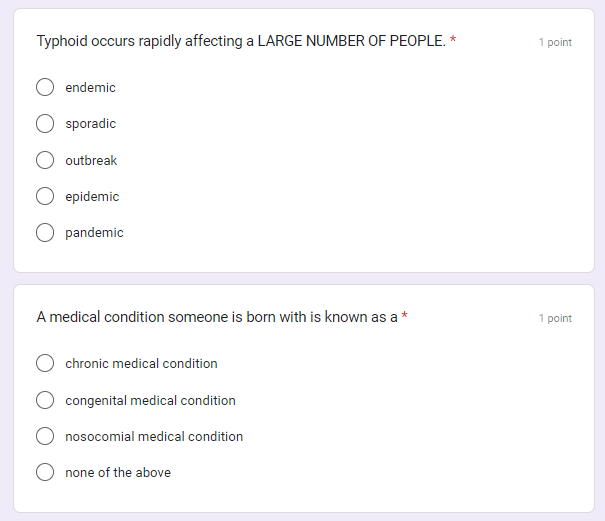
epidemic
a disease that rapidly spreads to a large number of people in a population within a short period of time. Western Africa Ebola epidemic (2013-2015
pandemic
An epidemic that has spread across several countries or continents and affects a large number of people. Covid-19 Pandemic
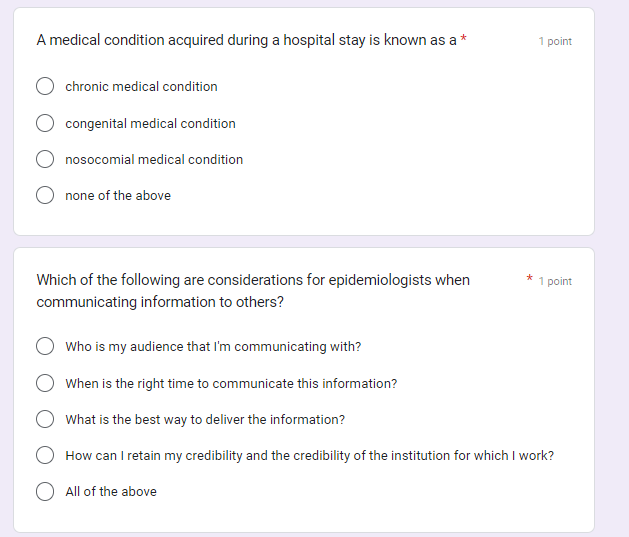
nosocomial infection
acquired during a patient’s stay at a hospital
hospital acquired infection or HAI
Center for Disease Control (CDC)
a federal agency of the United States responsible for protecting public health and safety by preventing and controlling diseases, injuries, and disabilities.
Disease
Disease occurs if and when the invasion and growth of a pathogen impair bodily functions.
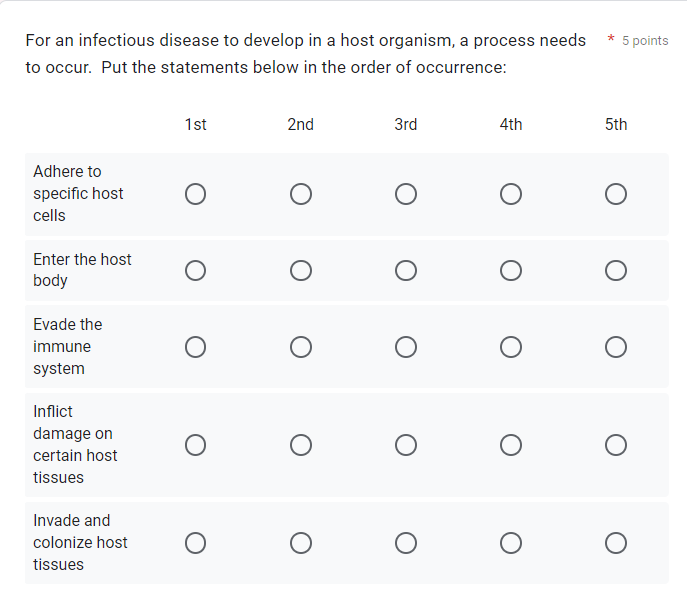
To cause disease, pathogens must:
enter the host body
evade the immune system
adhere to specific host cells
invade and colonize host tissues
inflict damage on those tissues.
inherited disease
genetic diseases
such as Sickle Cell Anemia and Familial Hypercholesterolemia.
infectious disease
infectious diseases are contracted, or caught. They are caused by agents outside of the human body that invade and cause harm. Because they can be transmitted to others, they are considered infectious.
pathogens
Pathogens are microorganisms that cause disease.
infection
An infection results when a pathogen invades and begins growing within another organism.
Host
The organism that is invaded is called the host.
Normal Flora
A healthy microbiome helps us digest food, protects us from invading organisms, and even provide us with some of the vitamins we need to stay healthy. We need our normal flora to survive
refers to the microorganisms that naturally inhabit the human body without causing disease under normal conditions.
Microbes
tiny pathogens
only seen w/ a powerful microscope
Disease symptoms
Disease symptoms are signs or indications of an illness or abnormal condition in the body.
throat pain
difficulty swallowing
red and swollen tonsils that often have white patches of pus on them
tiny red spots on the soft or hard palate
swollen and tender lymph nodes in the neck
fever
headache
rash
fatigue
diagnosis
Clinical laboratory testing
→ involves identifying the specific condition or illness affecting an individual based on their symptoms, medical history, physical examination, and diagnostic tests.
disease transmission
These organisms can spread through airborne droplets when someone with the infection coughs or sneezes, or through shared food or drinks.
You can also pick up the organism from a surface and transfer them to your nose or mouth
treatment
antibiotics
involves administering medical interventions, such as medications, surgery, therapy, or lifestyle changes, aimed at alleviating symptoms, curing the illness, or managing its effects on the body.
role of epidemiology in investigating/resolving health events
SLIDES:
They investigate health-related matters such as disease outbreaks and chronic illnesses by gathering information, examining data, and looking for patterns. This information helps them define the health issue of concern, determine its cause(s), establish a timeline, and develop solutions, treatments, and preventive measures.
-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_-_
The role of epidemiology in investigating and resolving health events involves identifying patterns, causes, and risk factors associated with diseases or health issues in populations.
Epidemiologists gather and analyze data to understand the distribution and determinants of health-related events, which helps inform public health interventions and policies aimed at preventing, controlling, or mitigating the impact of health events on communities.
summarize how infectious diseases can be spread, treated and prevented
Infectious diseases can spread through various means including direct contact with infected individuals, contaminated objects or surfaces, airborne transmission, or through vectors like mosquitoes.
Treatment often involves targeting the infectious agent with medications such as antibiotics, antivirals, or antifungals, depending on the type of pathogen causing the disease. Supportive care, including rest, hydration, and symptom management, may also be provided.
Prevention strategies include vaccination, practicing good hygiene such as frequent handwashing, covering coughs and sneezes, using personal protective equipment when necessary, maintaining a clean environment, and implementing public health measures like quarantine and isolation during outbreaks. Additionally, education about the transmission of infectious diseases and promoting healthy behaviors can help reduce the risk of infection.
the role of effective communication when providing information about health events
Clear communication ensures understanding and reduces misinformation, fostering trust between health authorities and the public. Empowering individuals with accurate information promotes informed decision-making and healthier practices, while facilitating community engagement encourages active participation in response efforts, ultimately promoting positive health outcomes.
describe the characteristics of the six categories of infectious agents:
Bacteria: Bacteria are single-celled microorganisms that can be found virtually everywhere. They can be spherical (cocci), rod-shaped (bacilli), or spiral (spirilla). Bacteria reproduce by binary fission and can cause various diseases such as strep throat, tuberculosis, and food poisoning.
Viruses: Viruses are tiny infectious agents that consist of genetic material (DNA or RNA) surrounded by a protein coat. They can only replicate inside the cells of living organisms. Viruses cause diseases ranging from the common cold and influenza to more severe illnesses like HIV/AIDS and COVID-19.
Fungi: Fungi are organisms that include yeasts, molds, and mushrooms. They can be unicellular (yeasts) or multicellular (molds). Fungal infections can affect the skin, nails, respiratory system, and internal organs. Examples include athlete's foot, ringworm, and candidiasis.
Protozoa: Protozoa are single-celled organisms that can be found in various environments, including soil, water, and the bodies of humans and animals. Some protozoa are parasitic and can cause diseases such as malaria, giardiasis, and toxoplasmosis.
Helminths: Helminths are parasitic worms that infect humans and animals. They include flatworms (such as tapeworms and flukes) and roundworms (such as hookworms and pinworms). Helminthic infections can cause a range of health problems, including intestinal blockages, anemia, and malnutrition.
Prions: Prions are infectious agents composed solely of protein. They cause neurodegenerative diseases in humans and animals, such as Creutzfeldt-Jakob disease (CJD) in humans and bovine spongiform encephalopathy (BSE) in cows. Prion diseases result in the accumulation of abnormal proteins in the brain, leading to progressive neurological decline.
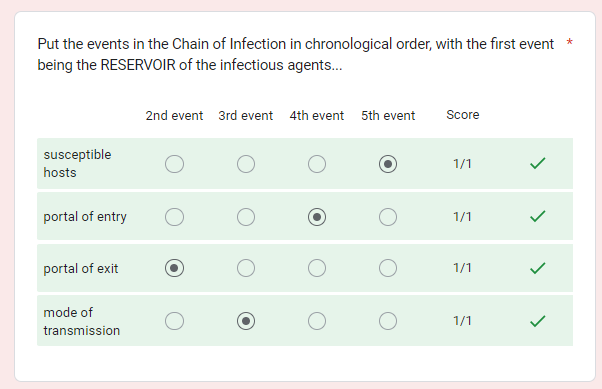
susceptible host
Infectious agents can infect a host that is vulnerable to infection, called a susceptible host.
reservoir of infectious agent
A pathogen resides in a reservoir (usually human or other animal),
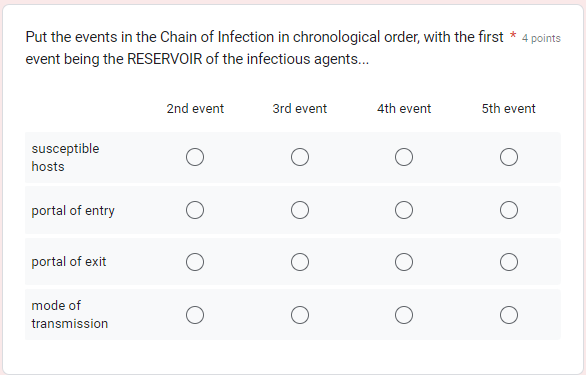
Chain of infection
A pathogen resides in a reservoir (usually human or other animal), exits, is transmitted to another host, enters the host, and causes an infection. This cycle is called the Chain of Infection.
R.E.T.E.I = robust experiments to explore immunology (HAHA)
Example:
Someone has the flu (reservoir).
They sneeze (virus droplets exit the host).
Flu virus is transmitted through the air.
Virus droplets inhaled by new host (enters).
Virus infects a cell & replicates (infection).
Direct contact vs indirect contact
Direct Contact: when a susceptible host touches an infected individual or is exposed to their body fluids via direct contact. This requires close contact between an infected person and a susceptible host. Droplets from a cough or sneeze that travels a very short distance (a few feet, like during a hug) from host to host is also considered direct contact.
Indirect Contact: when a susceptible host inhales infected suspended airborne particles (dust having pathogens on it, for example), touches an infected object (such as door knobs or money), or is bitten by an infected insect or animal vector.
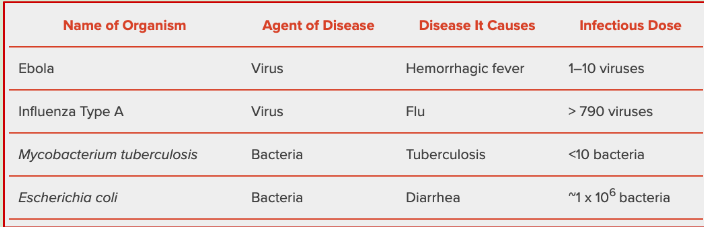
infectious dose
The number of organisms it takes to cause illness following exposure is known as the infectious dose.
SARS-CoV-2 and Covid 19
In January of 2020, the world began battling a pandemic caused by a coronavirus. This virus, called Severe Acute Respiratory Syndrome Coronavirus 2, or SARS-CoV-2, causes the disease COVID-19, or Coronavirus Disease 2019.
SARS-CoV-2 is an RNA virus, meaning it has RNA as its nucleic acid component, not DNA.
RNA viruses can cross species barriers and can cause illness in humans.
It is believed that SARS-CoV-2 originated in a bat and jumped species to humans.
RNA virus vs. DNA virus
RNA virus: has RNA as its nucleic acid component, not DNA.
Innate immunity
nonspecific defense mechanisms
Non-specific immune defense mechanisms that we are born with. These mechanisms work to keep any “non-self” thing outside of us from infecting cells.
Non-specific): 1st Line of Defense
Acquired immunity
adaptive immunity
This is acquired after cells are infected by a specific pathogen. Cells & antibodies are used to target specific pathogens for destruction. There are two forms:
(Adaptive/ Specific / Cell-mediated): 2nd Line of Defense
Active immunity
Active immunity: acquired following infection and recovery, or from a vaccine. After an infection is over, your body continues to make low levels of antibodies so they can attack the pathogen if it ever invades again.
naturally acquired immunity
if you get the pathogen and your body had to fight it (RISKKK)
artificially acquired immunity
vaccines and stuff (controlled → little to no risk)
passive immunty
Passive immunity: acquired from the mother. Antibodies are passed through the placenta to a fetus, then through breast feeding, giving immunity for about 6 months.
antigen
In lymph node, Dendritic Cell shows the antigens to WBC Helper T Cells until it finds one that “matches” the antigen type.
→ After that, the Helper T Cell clones themselves…
T cells
A dendritic cell (from Innate Immunity) travels to a lymph gland and activates a Helper T-cell
Some Helper T cells activate B-Cells
Some Helper T-cells become Cytotoxic T-cells & go to injury → kill infected cells
B cells
helper T-cells activates B-cells (AKA “Plasma cells”) to divide and make antigen-specific antibodies.
the antibodies bind to the pathogen’s antigens and “handcuff” the pathogen, disabling it.
Macrophages eat up the disabled pathogens
Antibodies
the type of cells that make antibodies are called B-cells
the role of antibodies:
Blocking pathogens from entering cells
Preventing bacteria from ingesting nutrients
Binding toxins released by pathogens to prevent them from harming the host
Memory T cells
By the end of the infection, some Helper T cells become Memory T Cells
Memory B cells
some B cells become Memory B Cells which can be activated quickly if you are infected with the same pathogen again one day.
inflammation
Blood vessels “get leaky”, allowing plasma into damaged tissue, causing inflammation (redness, swelling and heat).
Inflammation attracts Compliment: toxic chemicals that kill pathogens.
Herd Immunity
“Herd Immunity (AKA Community Immunity) is a situation in which enough of a population is immune to an infectious disease (through vaccination and/or prior illness) to make the pathogen unlikely to spread from person to person.
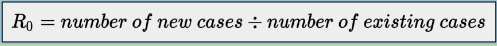
R-naught (R0)
R-naught, or R0, is a term used to measure how infectious an agent of disease is. The R0 of an infection can be thought of as the expected number of new infections that come about from one infected person
describe how infectious diseases can be transmitted
Direct Contact: Transmission occurs through direct physical contact with an infected person, such as through touching, kissing, or sexual intercourse.
Indirect Contact: Transmission occurs through contact with contaminated objects or surfaces, such as doorknobs, utensils, or shared items.
Airborne Transmission: Transmission occurs through respiratory droplets expelled when an infected person coughs, sneezes, or talks. These droplets can be inhaled by others nearby.
Vector-borne Transmission: Transmission occurs through the bite of an infected arthropod vector, such as mosquitoes (malaria, dengue), ticks (Lyme disease, Rocky Mountain spotted fever), or fleas (plague).
Waterborne Transmission: Transmission occurs through the ingestion of contaminated water containing pathogens, such as bacteria, viruses, or parasites.
Foodborne Transmission: Transmission occurs through the ingestion of contaminated food products, which may harbor bacteria, viruses, parasites, or toxins.
Vertical Transmission: Transmission occurs from mother to child during pregnancy, childbirth, or breastfeeding, allowing pathogens to pass from the mother's bloodstream to the fetus or newborn.
explain ways to stop the spread of infectious diseases
Vaccination: Vaccines stimulate the immune system to produce antibodies against specific pathogens, preventing infection and reducing the transmission of diseases within communities.
Hand Hygiene: Regular handwashing with soap and water for at least 20 seconds helps remove pathogens from the hands and reduces the risk of transmission through direct contact or contaminated surfaces.
Respiratory Hygiene: Covering the mouth and nose with a tissue or elbow when coughing or sneezing helps prevent the spread of respiratory droplets containing infectious agents.
Physical Distancing: Maintaining a safe distance (usually 6 feet or 2 meters) from others, especially in crowded or indoor settings, reduces the risk of airborne transmission of infectious diseases.
Wearing Masks: Wearing face masks, particularly in situations where physical distancing is challenging, helps reduce the spread of respiratory droplets and protects others from potential exposure to infectious agents.
Cleaning and Disinfection: Regularly cleaning and disinfecting frequently touched surfaces, such as doorknobs, countertops, and electronic devices, helps eliminate pathogens and reduces the risk of surface transmission.
Isolation and Quarantine: Isolating individuals who are infected with a contagious disease and quarantining those who have been exposed to the infection help prevent further spread within the community.
Public Health Measures: Implementing public health measures such as contact tracing, testing, and targeted interventions help identify and contain outbreaks before they escalate.
Promoting Health Education: Providing accurate information and promoting awareness about the modes of transmission, symptoms, and preventive measures of infectious diseases empower individuals to take proactive steps to protect themselves and others.
Supporting Healthcare Systems: Strengthening healthcare systems' capacity to diagnose, treat, and manage infectious diseases, as well as ensuring access to healthcare services and resources, is essential for effective response and containment efforts.
summarize how the human body fights infection
PRIMARY RESPONSE: Innate Immunity
Your own damaged cells release cytokine chemicals into the tissue, alerting the immune system that they need help.
Meanwhile, the invading pathogens begin to damage the cells and tissue.
If the pathogen is bacteria: Invading Bacteria steal resources, leaving their toxic waste everywhere.
If the pathogen is virus: Invading Viruses enter cells & enslave them to make more viruses (infecting/killing more cells).
WBC Macrophages show up at the site: engulf and kill pathogens (up to 100!) and call for help.
WBC Neutrophils go to injured tissue, killing both your own tissue and pathogens with their toxic chemicals, creating pus.
Blood vessels “get leaky”, allowing plasma into damaged tissue, causing inflammation (redness, swelling and heat).
Inflammation attracts Compliment: toxic chemicals that kill pathogens.
SECONDARY RESPONSE: Adaptive Immunity (AKA Acquired/Cell Mediated Immunity)
WBC Dendritic Cells are attracted to the wound site, collecting antigens from the viruses or bacteria. Dendritic cells then display the antigens on the surface of their membrane. They then travel through the lymphatic vessels to a lymph node.
In lymph node, Dendritic Cell shows the antigens to WBC Helper T Cells until it finds one that “matches” the antigen type.
The Helper T Cell clones themselves…
One cloned group, now called Cytotoxic T Cells, go to the site of your damaged tissue/cells and
stimulate the Macrophages to keep killing the bacteria.
kill any of your own human cells that may be infected with a virus.
The other group of cloned Helper T Cells stimulate WBC B Cells to make specific antibody proteins.
B Cells make a huge number of antibodies that bind to the pathogen’s surface antigens, rendering them harmless. This is called the “humoral response” and takes about a week after infection to come to full force.
Macrophages gobble up any pathogens that have been bound up by antibodies, and the infection (hopefully) ends.
By the end of the infection, some Helper T cells become Memory T Cells, and some B cells become Memory B Cells which can be activated quickly if you are infected with the same pathogen again one day.
Etiology of disease
etiology refers to the cause of a disease or condition. This can include things like diet or other lifestyle factors, genetics, or as in this case, pathogens.
how to categorize different disease etiologies (infectious, inherited, etc.)
idk
congenital medical condition
something someone is born with
what type of pathogen is tinea pedis
fungi (athlete’s foot)
what kind of pathogen is Taenia
Helminths (tapeworm)
what type of pathogen is Creutzfeldt-Jakob disease? (CJD)
Prion (dementia stuff)
what type of pathogen is Giardia Lamblia (causes giardiasis)
protists
what type of pathogen is Covid 19, Flu
virus
what type of pathogen is mycobacterium (tuberculosis)
bacteria (obv) 😹😹
What type of pathogens can antibiotics treat?
bacteria
What do tuberculosis and strep throat have in common?
They can all be treated with antibiotics
Without medication, a pregnant woman who tests positive for the HIV virus can give birth to a baby who tests positive for the HIV virus. Categorize the HIV virus:
The HIV virus is the cause of an infectious disease.
Martin has tested positive for the HIV virus, but doesn't show or feel any symptoms. Which statement below is FALSE?
Martin has HIV disease
Organisms that are infectious and cause disease are called
Pathogens
u shud click on image to see full pic for both sides
Calculating R-naught (what’s the formula?)
Note: The R0 number only applies when everyone is a susceptible host, meaning no one is immune and there is no way to control the spread of the disease.
(On a relative scale, since the R-naught is less than 1, this disease causing agent is not very infectious)
SUMMARY OF IMMUNE RESPONSE
SUMMARY OF IMMUNE RESPONSE
PRIMARY RESPONSE: Innate Immunity
Your own damaged cells release cytokine chemicals into the tissue, alerting the immune system that they need help.
Meanwhile, the invading pathogens begin to damage the cells and tissue.
If the pathogen is bacteria: Invading Bacteria steal resources, leaving their toxic waste everywhere.
If the pathogen is virus: Invading Viruses enter cells & enslave them to make more viruses (infecting/killing more cells).
WBC Macrophages show up at the site: engulf and kill pathogens (up to 100!) and call for help.
WBC Neutrophils go to injured tissue, killing both your own tissue and pathogens with their toxic chemicals, creating pus.
Blood vessels “get leaky”, allowing plasma into damaged tissue, causing inflammation (redness, swelling and heat).
Inflammation attracts Compliment: toxic chemicals that kill pathogens.
SECONDARY RESPONSE: Adaptive Immunity (AKA Acquired/Cell Mediated Immunity)
WBC Dendritic Cells are attracted to the wound site, collecting antigens from the viruses or bacteria. Dendritic cells then display the antigens on the surface of their membrane. They then travel through the lymphatic vessels to a lymph node.
In lymph node, Dendritic Cell shows the antigens to WBC Helper T Cells until it finds one that “matches” the antigen type.
The Helper T Cell clones themselves…
One cloned group, now called Cytotoxic T Cells, go to the site of your damaged tissue/cells and
stimulate the Macrophages to keep killing the bacteria.
kill any of your own human cells that may be infected with a virus.
The other group of cloned Helper T Cells stimulate WBC B Cells to make specific antibody proteins.
B Cells make a huge number of antibodies that bind to the pathogen’s surface antigens, rendering them harmless. This is called the “humoral response” and takes about a week after infection to come to full force.
Macrophages gobble up any pathogens that have been bound up by antibodies, and the infection (hopefully) ends.
By the end of the infection, some Helper T cells become Memory T Cells, and some B cells become Memory B Cells which can be activated quickly if you are infected with the same pathogen again one day.