MCAT Biology - Homeostasis
1/85
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
Ibuprofen
nonsteroidal anti-inflammatory drug; analgesic; can cause analgesic nephropathy
dialysis
performs filtration to purify the blood and excrete wastes externally, a crucial function that the kidneys would normally perform
excretory system
regulation of blood pressure, blood osmolarity, acid–base balance, and removal of nitrogenous wastes
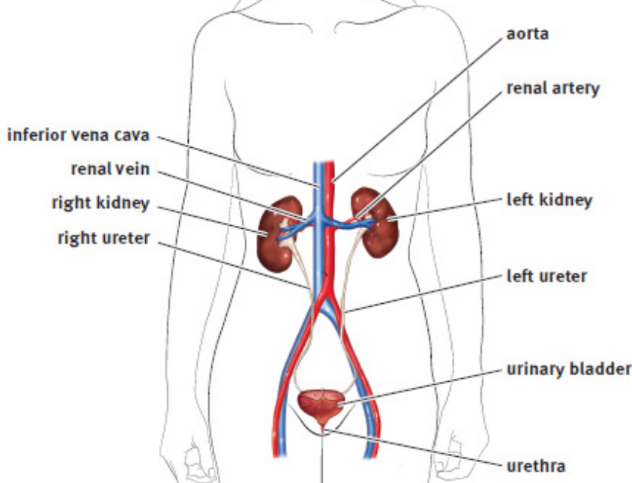
kidneys
two bean-shaped structures located behind the digestive organs at the level of the bottom rib
nephron
functional unit of the kidney; approx. 1 million per kidney
ureter
nephrons eventually empty into this tube in the renal pelvis towards the bladder
bladder
storrs urine for later excretion
urethra
tube through which urine exists the body
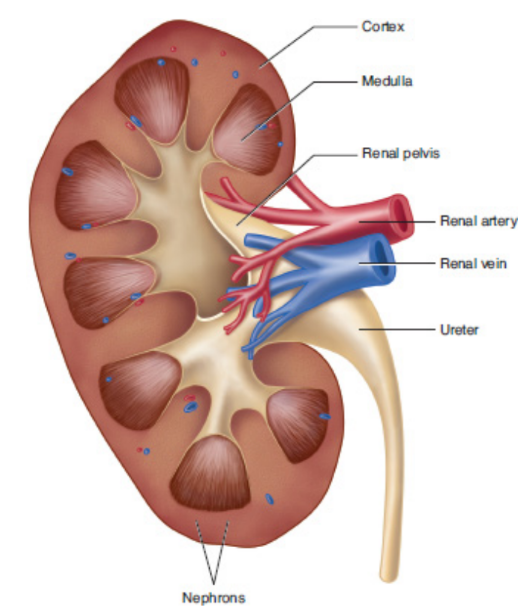
renal cortex
kidney’s outermost layer; isotonic to blood
renal medulla
sits within kidney; deeper than cortex; isotonic to 4x concentration of blood
renal hilum
deep slit in the center of a kidney’s medial surface
renal pelvis
widest part of the ureter; spans almost the entire width of the renal hilum
renal artery
branches out, passes through the medulla, and enters the cortex as afferent arterioles through the renal hilum
renal vein
exit through the renal hilum
portal system
consists of two capillary beds in series through which blood must travel before returning to the heart
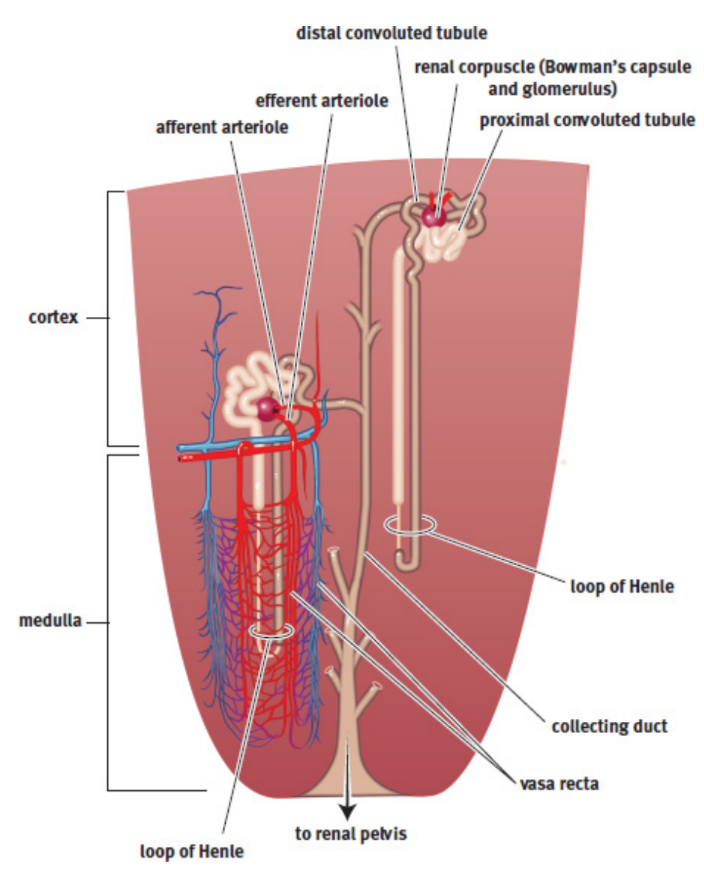
glomerulus (pl. -i)
highly convoluted capillary tufts derived from afferent arterioles in the nephrons
afferent arterioles
carry blood to the glomerulus
efferent arterioles
carry blood away from the glomerulus
vasa recta
capillary bed around the loop of Henle
Bowman’s capsule
cup-like structure around the glomerulus that leads to a long tubule with many distinct areas
detrusor muscle
muscular lining of bladder; parasympathetic activity causes the detrusor muscle to contract
internal urethral sphincter
smooth muscle; contracted in its normal state; under involuntary control
external urethral sphincter
skeletal muscle; under voluntary control
stretch receptors
convey to the nervous system that the bladder requires emptying, causes parasympathetic neurons to fire
micturition reflex
Stretch receptors signal for the detrusor muscle contracts and the internal sphincter to relax when bladder is full; disspates in a few minutes if urge not sated but will begin again
Urination
facilitated by the contraction of the abdominal musculature, which increases pressure within the abdominal cavity, resulting in compression of the bladder and increased urine flow rate
filtration
approximately 20 percent of the blood that passes through the glomerulus is filtered as fluid into Bowman’s space
filtrate
collected fluid in Bowman’s space; similar in composition to blood but does not contain cells or proteins
Starling forces
account for the pressure differentials in both hydrostatic and oncotic pressures between the blood and Bowman’s space
hydrostatic pressure of glomerulus higher than Bowman → osmotic pressure opposes but is weaker
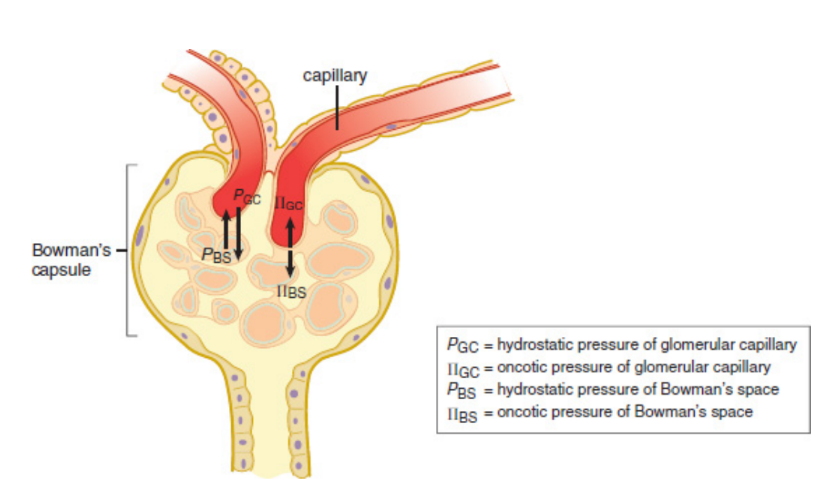
kidney stone
blocks ureter; buildup of urine; may reverse Starling forces
secretion
nephrons put salts, acids, bases, and urea directly into the tubule by either active or passive transport
Ammonia (NH3)
byproduct of the metabolism of nitrogen-containing compounds; highly basic so can disturb the pH of blood and cells
urea
what the liver converts ammonia to; travels to the kidney and is secreted into the nephron for excretion in the urine
reabsorption
Some compounds that are filtered or secreted may be taken back up for use
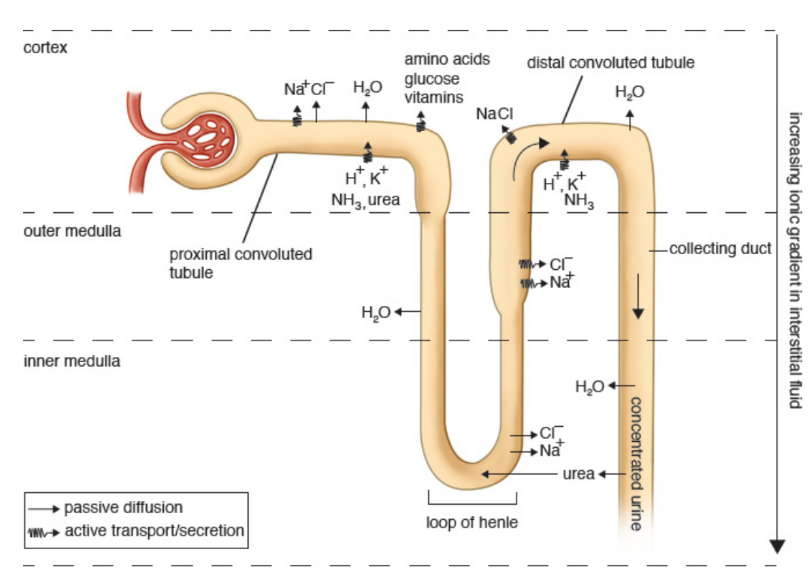
proximal convoluted tubule (PCT)
filtrate first enters; stays isotonic to the interstitium
reabsorbed: water, amino acids, glucose, water-soluble vitamins, and the majority of salts → picked up by vasa recta
secreted: hydrogen ions, potassium ions, ammonia, and urea
interstitium
connective tissue surrounding the nephron
descending limb of the loop of Henle
dives deep into the medulla; permeable only to water; creates interstitium gradient to maximise reabsorption
reabsorbs: water
countercurrent multiplier system
flow of filtrate through the loop of Henle is in the opposite direction from the flow of blood through the vasa recta
(think gills!)
ascending limb of the loop of Henle
climbs up from the medulla; permeable only to salts; creates interstitium gradient to maximise reabsorption
reabsorbs: salts
diluting segment
while ascending to the outer medulla, the loop of Henle becomes thicker because the cells lining the tube are larger; contain large amounts of mitochondria, which allow the reabsorption of sodium and chloride by active transport; only portion of the nephron that can produce urine that is more dilute than the blood
distal convoluted tubule (DCT)
responds to aldosterone
reabsorbs: sodium (water follows sodium)
secretes: hydrogen ions, urea, ammonia, potassium ions
edema
body accumulates excess fluid in the lungs or peripheral tissues
Collecting Duct
responsive to aldosterone and ADH
reabsorbs: water and sodium
urine
mostly urea, uric acid, and excess ions (sodium, potassium, magnesium, and calcium); flows through the ureter to the bladder where it is stored until voiding
Aldosterone
steroid hormone that is secreted by the adrenal cortex in response to decreased blood pressure
renin
released from juxtaglomerular cells in kidney with decreased blood pressure
angiotensinogen
liver protein; cleaved by renin → angiotensin I
angiotensin I
metabolized by angiotensin-converting enzyme in the lungs → angiotensin II
angiotensin-converting enzyme
angiotensin I → angiotensin II
angiotensin II
promotes the release of aldosterone from the adrenal cortex
Antidiuretic hormone (ADH, vasopressin)
peptide hormone synthesized by the hypothalamus and released by the posterior pituitary in response to high blood osmolarity; directly alters the permeability of the collecting duct, allowing more water to be reabsorbed by making the cell junctions of the duct leaky
inhibited by alcohol and caffeine
osmotic pressure
“sucking” pressure that draws water into the vasculature caused by all dissolved particle
Oncotic pressure
osmotic pressure that is attributable to dissolved proteins specifically
average blood osmolarity
maintained at approximately 290 milliosmoles (mOsm) per liter
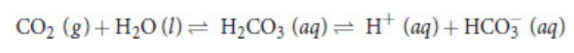
bicarbonate buffer system
major regulator of blood pH
skin (integument)
largest organ in our bodies by both weight and size; one of the major components of nonspecific immune defense, protecting us from exposure to the elements and invasion by pathogens; derived from the ectoderm
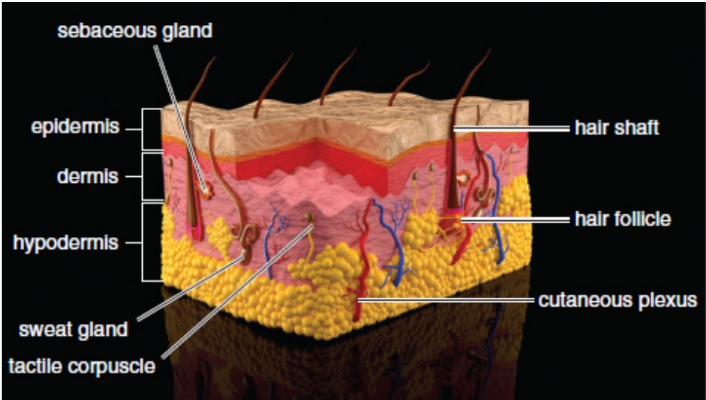
hypodermis (subcutaneous layer)
layer of connective tissue that connects the skin to the rest of the body; contains fat and fibrous tissue
dermis
middle layer of skin
epidermis
most superficial layer of skin; subdivided into strata
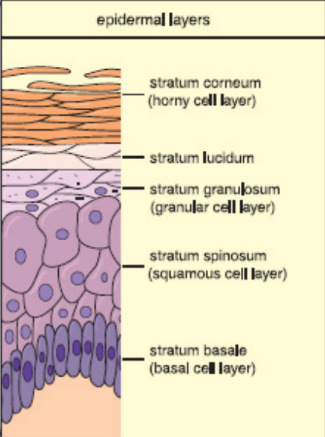
strata
layers of the epidermis
stratum basale (deepest)
stratum spinosum
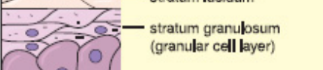
stratum granulosum
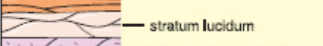
stratum lucidum
stratum corneum (shallowest)
reverse: Come, Let’s Get Sun Burned
stratum basale
contains stem cells and is responsible for proliferation of keratinocytes
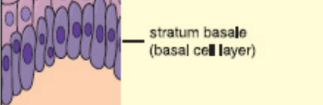
keratinocytes
the predominant cells of the skin, that produce keratin
keratin
protein; resistant to damage and provides protection against injury, water, and pathogens
ex. hair, fingernails, calluses
stratum spinosum
cells become connected to each other; also the site of Langerhans cells

stratum granulosum
keratinocytes die and lose their nuclei
stratum lucidum
present in thick, hairless skin, such as the skin on the sole of the foot or the palms, and is nearly transparent
stratum corneum
contains up to several dozen layers of flattened keratinocytes, forming a barrier that prevents invasion by pathogens and that helps to prevent loss of fluids and salt
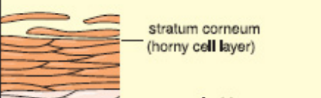
Calluses
form from excessive keratin deposition in areas of repeated strain due to friction; they provide protection to avoid damage in the future
Melanocytes
found in the stratum basale; derived from neural crest cells; produce melanin; same number in everyone but different activity; increase activity in response to UV light
melanin
pigment that serves to protect the skin from DNA damage caused by ultraviolet radiation; produced in melanocytes and transferred to keratinocytes
albinism
genetic (autosomal recessive) metabolic disorder characterized by the inability to synthesize melanin
vitiligo
autoimmune disorder in which melanocytes are killed by the individual’s immune system
Langerhans cells
special macrophages that reside within the stratum spinosum; capable of presenting antigens to T-cells in order to activate the immune system
papillary layer
upper layer of dermis; consists of loose connective tissue
reticular layer
lower layer of dermis; denser; sweat glands, blood vessels, hair follicles, sensory receptors
Merkel cells (discs)
sensory receptors present at the epidermal–dermal junction; responsible for deep pressure and texture sensation
free nerve endings
respond to pain
Meissner’s corpuscles
respond to light touch
Ruffini endings
respond to stretch
Pacinian corpuscles
respond to deep pressure and vibration
Thermoregulation
control of internal temperature
Sweating
excellent cooling mechanism that is controlled by the autonomic nervous system; Postganglionic sympathetic neurons that utilize acetylcholine innervate sweat glands and promote the secretion of water with certain ions onto the skin; Heat is then absorbed from the body as the water molecules undergo a phase change to evaporate
piloerection
arrector pili muscles contract, causing the hairs of the skin to stand up on end; trap a layer of heated air near the skin
Shivering
Skeletal muscle contracts rapidly; requires a sizeable amount of ATP
white fat
layer of fat just below the skin; helps to insulate the body
brown fat
much less efficient electron transport chain, which means that more heat energy is released as fuel is burned