PTE 763: exam 3
1/116
Earn XP
Description and Tags
NICU, medical complications with premies, motor and cognitive delays, aging and dementia, TBIs, and meningitis
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
117 Terms
what populations use the neonatal intensive care unit (NICU)?
used for newborns who are born prematurely, have a low birth weight, or have serious health conditions like breathing trouble, heart problems, infections, or birth defects
how long is the ideal pregnancy?
38-40 weeks (up to 36 weeks is okay tho)
a pregnancy duration of ___ or less is dangerous because the _____ are the last organs to develop around this time.
26 weeks; lungs
the APGAR neonate assessment is used to grade newborns immediately after birth to assess their health and determine if they need immediate medical assistance. what does the assessment look at?
Appearance, Pulse, Grimace, Activity, and Respiration
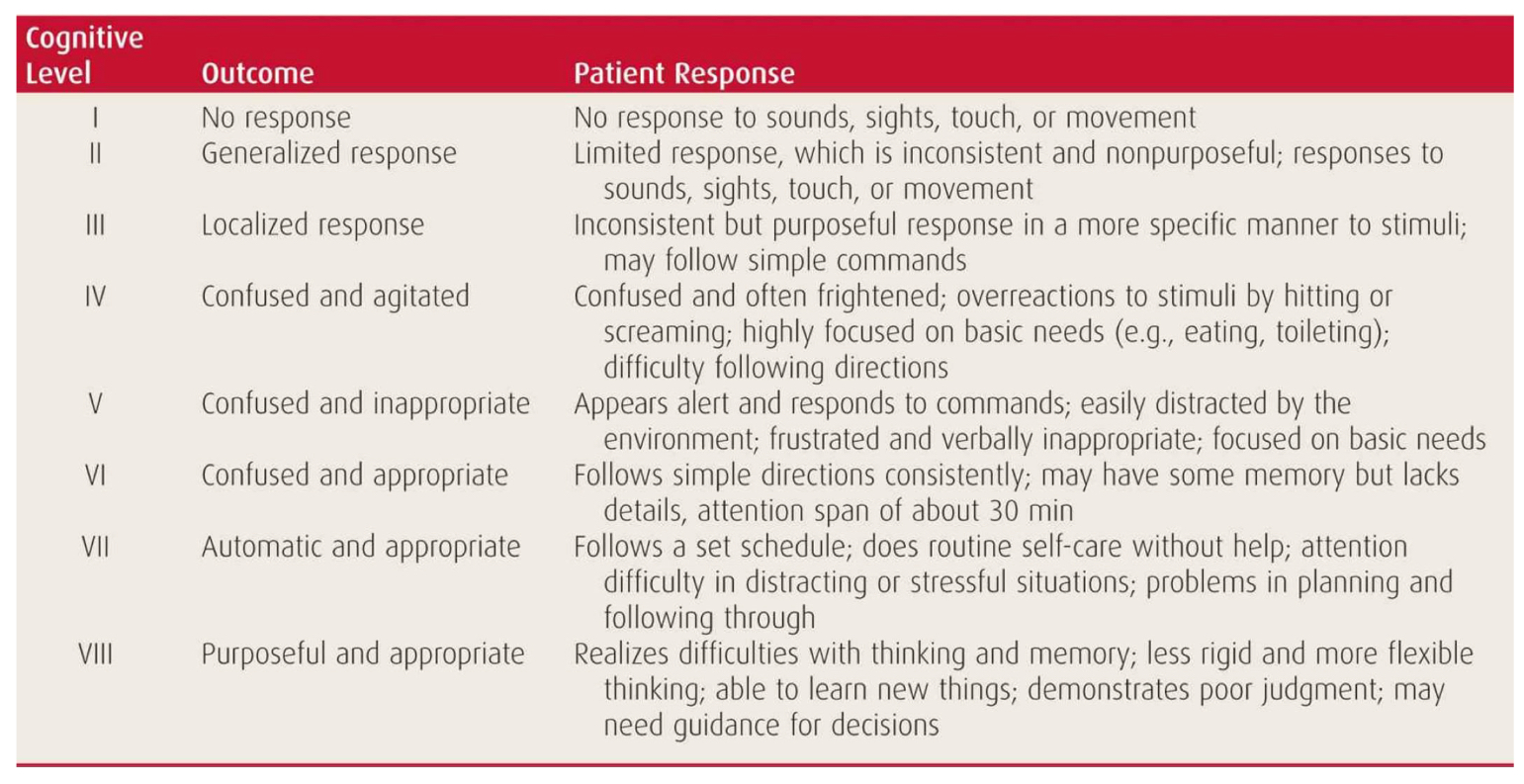
APGAR scale
what’s the indications of a low and high APGAR score?
low: poor health; medical issue occurring
high: good health; congrats!
what types of monitors are found throughout the NICU for continuous medical management?
temperature monitor
EKG and respiration
pulse oximeter
dynamap (measures BP and HR)
arterial lines (measures PCO2 and PO2)
apnea monitor
what types of monitors are found throughout the NICU for ventilation and oxygen administration?
extracorporeal membraneous oxygenation (ECMO)
high frequency ventilators
ventilator endotracheal tube
tracheostomy
nasal canula
oxyhood
nutrition is a huge concern for premies due to their lack of endurance for traditional feeding. what are some methods to provide nutrition for premies?
parenteral (central venous catheter)
gavage tube feeding (via oro or nasal)
gastrostomy
premies may suffer from GERD. what is that?
Gastroesophageal Reflux Disease: happens when stomach acid flows back up into the esophagus and causes heartburn.
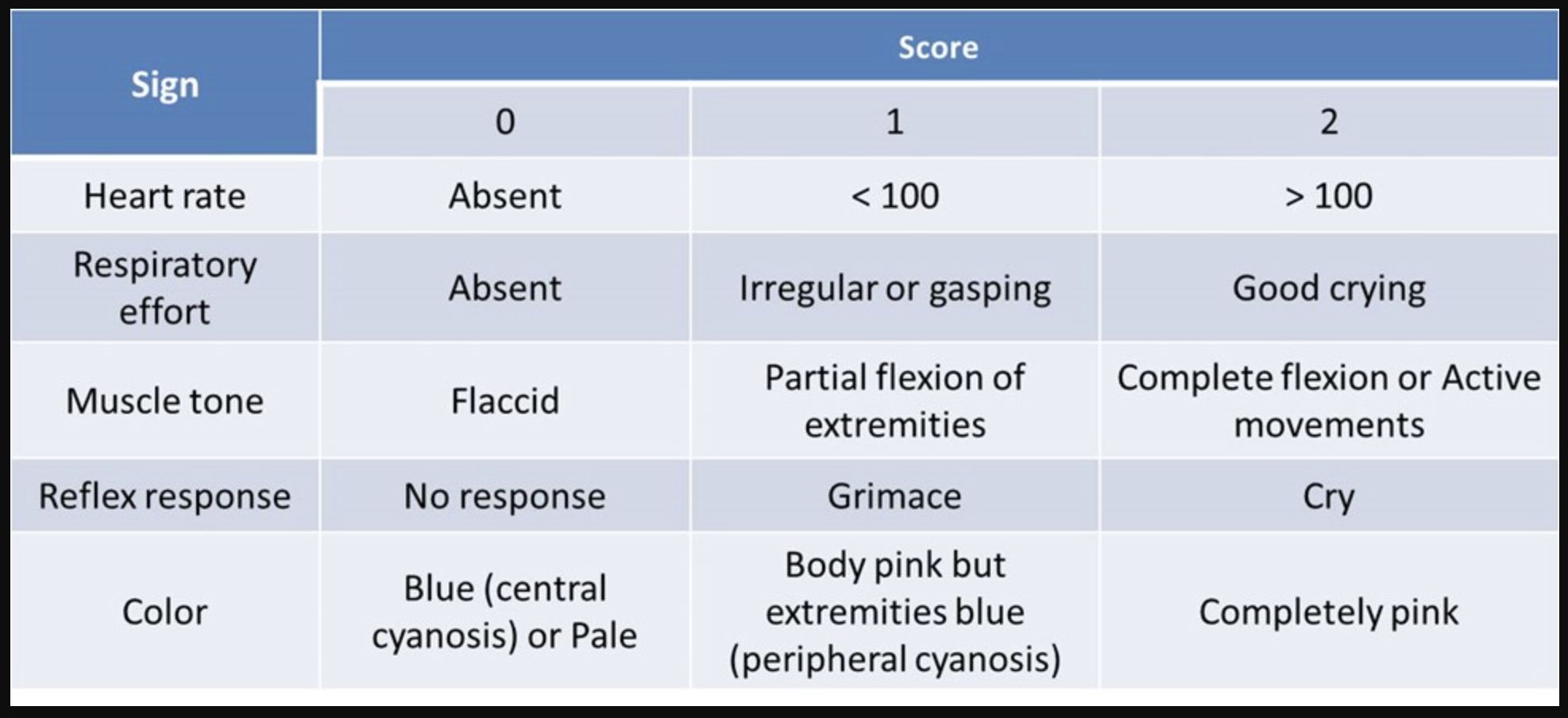
how should a caretaker position a patient suffering from GERD?
either 1) in prone with apnea monitor 2) supine with head elevated or 3) left sidelying
explain why a patient suffering from GERD should avoid right sidelying.
due to the shape and curve of the esophagus into the stomach, the acid has a tendency to flow back up easier. here’s a picture to show this:
a therapist is going to the NICU to assess a new premie born at 30 weeks. what should she include in her PT initial evaluation process?
the neonate’s environment and medical state while assessing the integumentary, musculoskeletal, and neuromuscular systems
list the newborn assessments of neurobehavioral function.
neurological assessment of the preterm and full-term newborn infant (Dubowitz)
neonatal behavioral assessment scale (NBAS)
assessment of preterm infant behavior (APIB)
neonatal intensive care unti network neurobehavioral scale (NNN)
newborn behavioral observation system (NBO)
newborn individualized developmental care and assessment program (NIDCAP)
neurobehavioral assessment of preterm infant
list the newborn assessments of motor function.
test of infant motor performance (TIMP)
general movements assessment (GMA)
a therapist visits a premie who was born at 34 weeks old. the baby is improving and upon entering the NICU room, the therapist notices the baby is alert, cooing, and relaxing. what is the baby’s presentation?
expressing signals of comfort :)
a therapist visits a premie who was born at 29 weeks old. the baby is having a rough day as his GERD is flaring up today. he is sucking his fists that are held tightly together while wiggling around his isolette. what is the baby’s presentation?
expressing signals of self calming
a therapist visits a premie who was born at 26 weeks old. the baby is not progressing well and struggling through the session. she is fussy with a grimace-look on her face and is hyper-alert while reaching out to anyone near. what is the baby’s presentation?
expressing signals of distress :(
the therapist revisits the premie born at 26 weeks old the next day, but finds the baby is still struggling. she arches her back and flails her limbs at any touch and spits up near the end of the 20 minutes therapy session. what is the baby’s presentation?
still expressing signals of distress :(
what are important aspects to include in the developmental care of premies?
reduce light and noise
cluster care with limited interruptions during sleep
encourage parent participation using kangaroo care
manage pain
how should a therapist handle a premie during a therapy session?
position baby with limbs and head in midline with limbs flexed close to body
massage in the form of firm touch
graded movement experience timed with infant’s readiness for social engagment
therapy treatments for _______ premies include cluster care, avoiding overstimulation, smooth and supported handling, positioning in prone, and placing pressure on feet.
hypertonic
therapy treatments for _______ premies include arousing, applying firm tactile input, stimulating the vestibular system, maintaining upright position for head control, and add unimodal/graded sensory stimulation.
hypotonic
what are some predictive variables of developmental problems?
time of onset of labor (pre-term and post-term)
body size of infant (too big or too small)
risks associated with multiple gestation (twins, triplets, etc.)
late fetal heart declerations
premature rupture of membranes
breeching
meconium aspiration (baby inhales his/her first stool passed in womb into their lungs)
what are the two pulmonary syndromes that are common with an under-developed pulmonary system?
RDS: respiratory distress syndrome
BPD: bronchopulmonary dysplasia
ischemia of an under-developed pulmonary system can lead to:
selective neuronal necrosis
focal ischemia brain necrosis and cavitation
parasagittal cerebral injury
PVL: periventricular leukomalacia
ROP: retinopathy of prematurity
NEC: necrotizing enterocolitis
ischemia of an under-developed nervous system can lead to __________ __________.
periventricular leukomalacia (PVL)
PVL diagnosed from an under-developed nervous system can lead to:
seizure disorders
cognitive impairments
visual and auditory deficits
atonic quadriplegia CP
athetoid CP
spastic quadriplegia, hemiplegia, and diplegia CP
what is retinopathy of prematurity (ROP)?
an eye disease in premature babies where abnormal blood vessels grow in the retina (hyperpoliferative neovascular response) leading to swelling and possible detachment of the retina
what is necrotizing enterocolitis (NEC)?
inflammation of the bowel (gut proper) that causes the death of mucosal cells which leads to a decrease production in mucus and an increase risk of proteolytic damage
what is hyperbilirubinemia?
occurs in newborns due to the breakdown of red blood cells and the immature liver's inability to process bilirubin efficiently; baby’s skin is yellowish
which common complications of newborns are the number one reasons for the baby’s referral into the foster care system?
fetal alcohol syndrome (FAS) and neonatal abstinence syndrome
how does an individual qualify for the American Association of Intellectual and Developmental Disabilities (AAIDD)?
must have a disability characterized by significant limitations in both intellectual functioning and adaptive behaviors (conceptual, social, and practical skills)
define developmental disability.
a severe, chronic disability that is attributable to a physical or mental disability that is likely to continue throughout the person’s life and results in clear functional limitations in 3 or more areas of life activities
usually diagnosed within first year of life
what is the DSM-V’s criteria to qualify as a developmental disabled individual?
score significantly sub-average intellectual functioning
concurrent deficits or impairments in present adaptive functioning in at least 2 areas
onset before 18 years of age
the score of ___ on an individually administered IQ test indicates sub-average intellectual functioning.
70 or below
list the IQ score ranges associated with mild, moderate, serve, and profound intellectual disability.
mild: 70-50
moderate: 49-40
severe: 39-20
profound: less than 20
the DSM-V’s criteria to qualify as a developmental disabled individual specifies an individual must be impaired in 2 adaptive functioning areas. name some examples of such.
communication, self-care, home living, social skills, self-direction, work, leisure, health, safety, and finances
infants may receive an assessment of intellectual function via sensorimotor-based evaluations. what is it a valid predictor of?
severe cognitive delay at that age
infants may receive an assessment of intellectual function via informational processing capacity. describe this assessment.
it is motor and language free assessment that observes how quickly children get bored of a task via monitoring their HR and time spent on task
higher intelligence = bored quicker
list the assessments of intellectual function for children with motor and cognitive impairments.
stanford-binet intelligence scale- IV or wechsler intelligence scale for children- III
columbia mental maturity scale for CP
raven’s progressive matrices
leiter international performance sclae for language delayed
kaufman assessment battery for children
which of the assessments of intellectual function for children allows for IQ measurement without using speech? (quiz question)
raven’s progressive matrices
leiter international performance sclae for language delayed
kaufman assessment battery for children
list the assessments of adaptive behavior for children with motor and cognitive impairments.
PEDI
aamr adaptive behavior scale-school (ABS-S2)
vineland adaptive behavior scales (VABS-II)
which assessments of adaptive behavior assess children with down syndrome and other cognitive issues?
aamr adaptive behavior scale-school (ABS-S2)
vineland adaptive behavior scales (VABS-II)
list the measuring outcomes used for children with motor and cognitive impairments.
goal attainment scale (GAS)
canadian occupational performance measure (COPM)
single-subject research method
what is the ecological assessment of children with motor and cognitive impairments?
an assessment that determines the domains (home, community, vocational, recreation, and lesion) to be included in the child’s program
looks at environments and sub-environments of these domains
T or F: it is important to consider current and future environments the child will be exposed to when creating an ecological assessment.
T
T or F: when evaluating a child with motor and cognitive impairments, partial participation or partial completion of a task is an acceptable outcome.
T
what aspects should be included when focusing on long-term goals for children with motor and cognitive impairments?
development of self-determination (freedom, control, support system)
employment or vocation
group home or extended care facility
list the PT interventions commonly used in children with motor and cognitive impairments.
errorless learning
differential reinforcement
minimize erros
instructed in natural environments
positive behavioral program
practice!!
what in the world is “errorless learning”?
an instructional strategy that minimizes errors by using prompts to ensure the learner provides the correct response. below is the progression:
instructional cueing
stimulus prompts
respond prompts
prompts fading
what is the difference between gradual decline vs pathological decline?
gradual: the slow, subtle changes in thinking and memory that are a normal part of aging
pathological: the more severe and accelerated decline caused by a disease which significantly impairs daily functioning
the nervous system declines at a rate of __ each year after the age of 30.
1%
neurotransmitter decline is noted in aging adults and plays a crucial role in their decline. describe the changes associated with the decline of acetylcholine, serotonin, norepinephrine, and dopamine.
acetylcholine: memory los
serotonin: mood, sleep, cognition changes
norepinephrine: diminished motor learning
dopamine: preclinical PD and worsening executive function and working memory
T or F: typical neuromuscular changes in aging individuals include the degeneration of motor components.
F; motor and sensory
the mid-thoracic preganglionic cell bodies decline at a rate of __ per decade resulting in a less efficient sympathetic nervous system (SNS).
8%
a therapist is treating an elderly patient for stability after a some falls. at the beginning of the session, the patient complains of lightheadedness and dizziness upon standing. he states this is a common occurrence and believes is the reason for his falls. why?
he has impaired regulation of his blood pressure (due to degeneration of SNS)
T or F: older individuals typically experience a decline in both bimanual and multi-joint coordination.
T
while watching two older professors walking, a DPT student notices they walk slow with small careful steps and the older man has to turn his full torso to talk to the older woman (decreased rotation). testing knowledge of the gait pattern, the student notices the older woman walks flat-footed with less heel strike and push off. is this typical or atypical?
typical gait for elderly!
what is the dementia?
a chronic disorder of mental processes due to brain disease or injury
usually caused by neurodegenerative or cerebrovascular incidents
to qualify for the diagnosis of dementia, an older individual must have at least 3/5 deficits. what are the 5 deficits?
language
memory
emotion
cognition
visuospatial
dementia is considered a _____ disease.
global
can a person with dementia learn motor skills?
yes because the cerebellum and basal ganglion are less affected areas of the brain
T or F: depression is considered dementia and is among the reversible dementias.
T
what is delirium?
a transient change (acute onset) in mental status with fluctuating symptoms
consciousness is affected
which has a better prognosis: dementia or delirium?
delirium
___-_______ delirium is the most common form.
post-anesthetic
why do older patients usually experience post-anesthetic delirium more than younger patients?
older = nervous system capacity is lower and metabolism is slower which increases the time to achieve the general anesthetic drug’s ½ life
what is alzheimers?
a progressive brain disorder that causes memory loss, confusion, and other cognitive decline
most common form of dementia
what two characteristics develop within a brain of an individual suffering from alzheimers?
neurofibrillary tangles
amyloid plaques
where does alzheimers affect first within the brain?
hippocampus and pre-frontal cortex
what is normal pressure hydrocephalus (NPH)?
a condition where there is an excessive buildup of cerebrospinal fluid (CSF) in the brain's ventricles
gradual buildup/slow process
T or F: normal pressure hydrocephalus has easily identifiable signs and symptoms.
F; signs and symptoms are often mistaken for aging causing others to overlook the possibility of NPH
what’s the triad that makes up signs and symptoms of NPH?
global deficits seen in gait disturbances, impaired cognition, and incontinence
what is the difference between a traumatic (TBI) and non-traumatic brain injury (NTBI)?
traumatic: an injury to the brain caused by an external physical force, such as a fall, MVA, or sports injury
non-traumatic: a type of brain damage that is caused by internal factors that disrupt brain function like stroke or tumors
a 20 year old male patient presents to the ER clinic following a MVA. he presents with a huge open gash across his forehead, bruising along his L cheek, a stiff neck, and is unconscious. what do these signs indicate?
indicate a head injury duh
____ _______ is blood or CSF leaking from the nose and/or ears and is indicative of a head injury.
nasal discharge
what are the mechanisms of injury related to TBIs?
injuries to face and/or neck causing damage to brain’s blood supply
direct impact injury
coup-countercoup injury
penetrating objects
acceleration/deceleration injuries
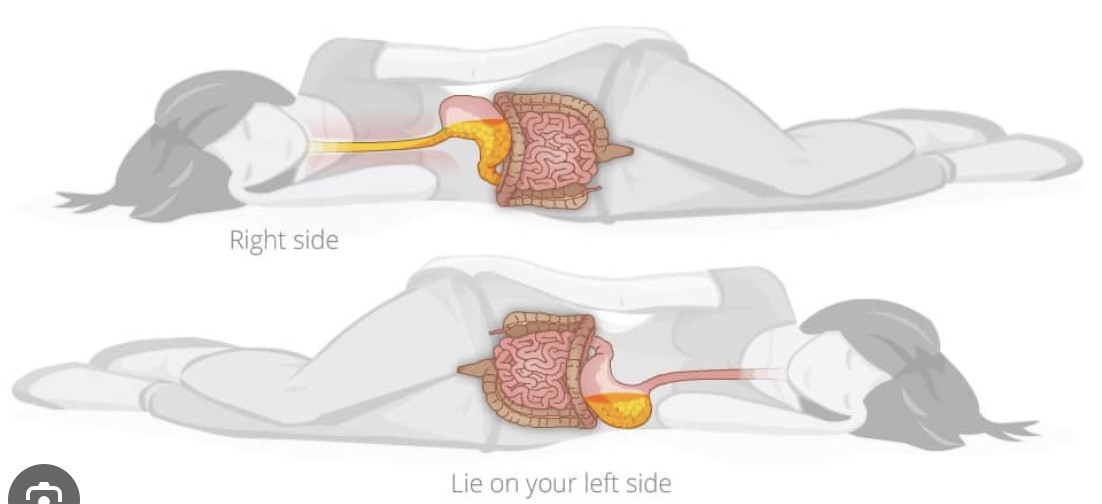
describe what happens to the brain in a coup-countercoup injury.
brain is injured at site of impact, then bounces back and hits site opposite from impact → damage on both sides
unequal acceleration/deceleration injuries occur from high velocity incidents that result in the tearing of vessels and axonal shearing. what are some deficits that may be observed in a patient following this type of injury?
widespread globa deficits including memory, cognition, and balance issues
what is diffuse axonal injury?
a type of TBI that occurs when the brain experiences sudden acceleration or deceleration forces, causing widespread damage to the axons throughout the brain
caused via MVAs, blasting injuries from combat, etc.
what are the primary damages seen following a TBI?
epidural and subdural hematomas
what’s the difference between epidural and subdural hematomas?
epidural: tearing of meningeal vessels resulting in blood collecting between skull and dura; fast onset
subdural: tearing of veins to superior sagittal sinus resulting in blood collecting between dura and arachnoid; slow onset
a patient comes into the ER at midnight following a rough football tackle incident. his mom states this occurred early in the night at his high school football game and since then her son has been vomiting, confused, and fatigued. the ER nurse rushes him to get a CT scan. why?
the ER nurse suspects an epidural hematoma (increased intracranial pressure)
increased intracranial pressure and ______ _____ are common secondary damages observed following a TBI.
cerebral hypoxia (or ischemia)
a therapist is seeing a patient from another therapist’s schedule. he was advised that this patient suffered from a huge hematoma in the L frontotemporal lobe and experiences bilateral UE motor and sensory deficits along with speech deficits. why?
the L frontotemporal hematoma shifted the brain towards the R causing the R side to be squished = affected both sides
what is an intracranial hemorrhage?
bleeding that occurs within the skull that causes hypoxia, increased pressure, and distortion to the brain tissue
leads to cell death within minutes from the ischemia, edema, necrosis, and/or toxic effects of the blood on neural tissue
what are the four grades of hemorrhage?
minimal bleed without significant findings
bleeding moves into ventricles; no significant findings
dilation of ventricles from bleeding; some neurological signs and symptoms
bleeding into white matter; severe neurological signs and symptoms
T or F: seizures are most common right after injury from the increased pressure and again between 6-24 months after injury from the scarring with any brain bleeding incident.
T
a TBI patient attending an inpatient rehabilitation therapy session suddenly begins convulsing. his eyelids are fluttering with horizontal jerking of his eyes and his jaw is moving in a chewing-like motion. what is happening?
seizure
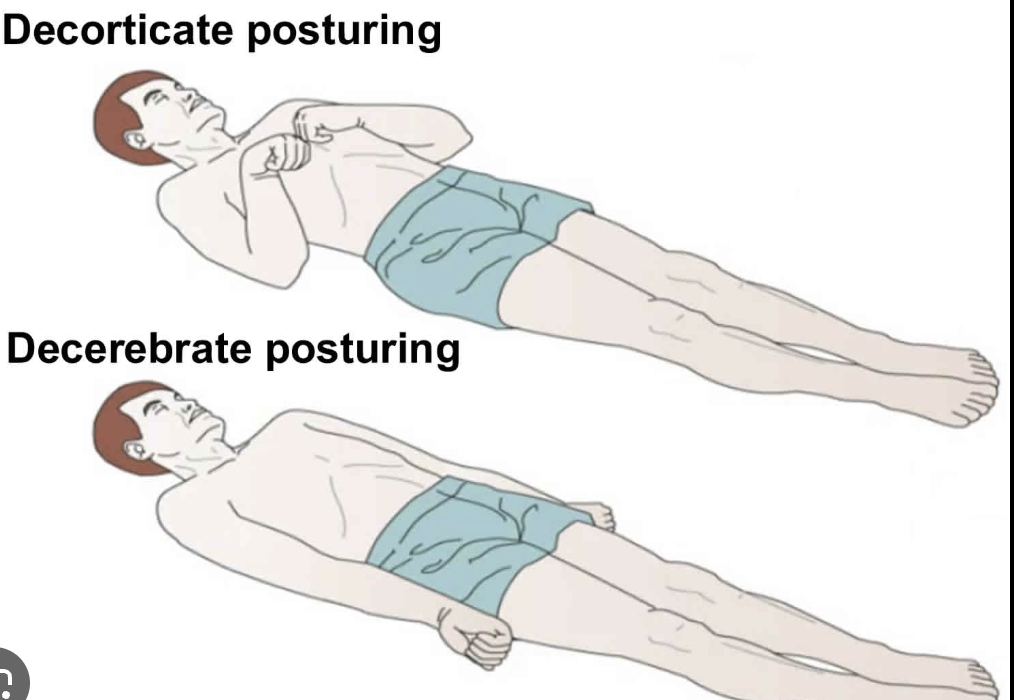
abnormal posturing like decorticate and decerebrate can be noted following a TBI. explain both postures.
what are some examples of physiological changes following a TBI?
monoplegia or hemiplegia
initially flaccid → spastic or rigid
motor disturbances of timing, sequencing, and coordination
return of primitive reflexes
cranial nerve involvement
changes in consciousness/coma
what are some examples of cognitive and behavioral changes following a TBI?
irritability and impulsivity
uncontrolled emotions and inappropriate behaviors
memory loss
problems with attention and concentration
perseveration
reduce problem-solving skills
depression
what are the main pharmacological interventions given to patients suffering a TBI?
drugs that decrease intracranial pressure (ICP) and drugs taht control blood pressure
what is the Glasgow Coma Scale (GCS)?
a neurological assessment tool used to objectively rate a person's level of consciousness on a scale of 3 to 15
mild concussion = score 13-15
moderate concussion = score 9-12
severe concussion = score 3-8
Glasgow Coma Scale
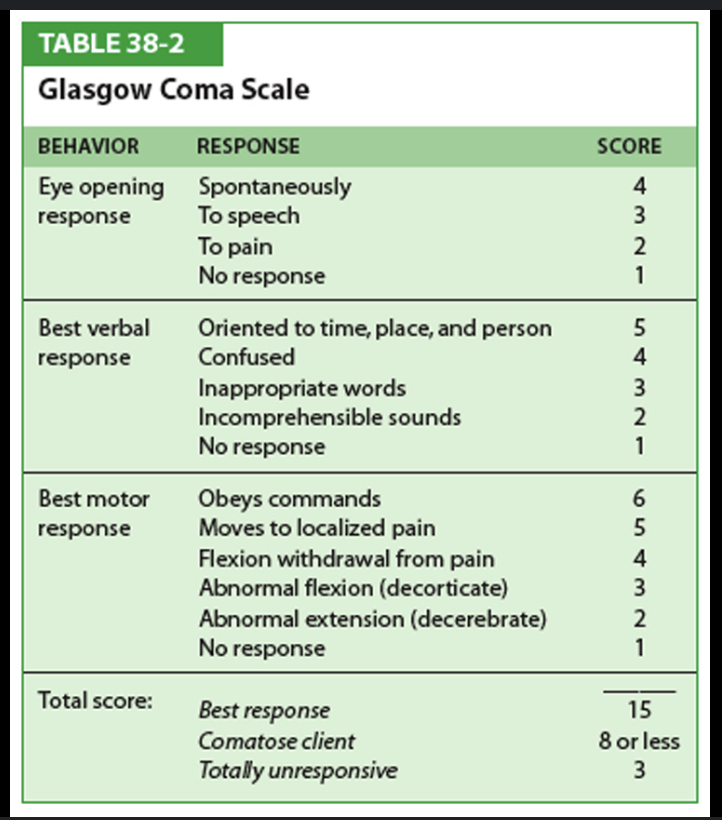
an EMS personnel assesses an individual who loss consciousness after hitting her head on a car’s dash in a MVA. she opened her eye’s in response to him asking her questions but she responded with inappropriate words. the EMS personnel then tested her motor response to which she moved away from a painful stimulus. what is her GCS score?
3 + 3 + 5 = 11
an EMS personnel assesses an individual who loss consciousness after colliding head-first into the boards during his hockey game. he opened his eyes immediately upon regaining consciousness yet was confused at how he ended up off the ice. the EMS personnel then tested his motor response to which he moved away from a painful stimulus but he couldn’t obey commands due to his confusion. what is his GCS score?
4 + 4 + 5 = 13
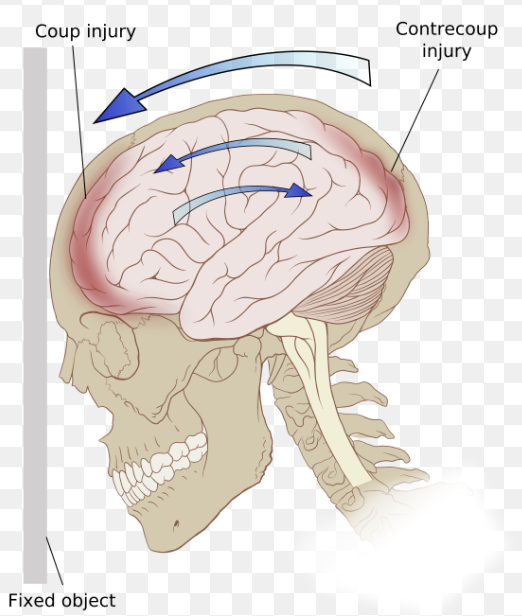
what are the Ranchos Los Amigos levels?
a 10-point scale used to assess cognitive and behavioral recovery in patients after a traumatic brain injury
Ranchos Los Amigos