Pediatrics
1/137
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
138 Terms
what is the most common elbow injury in children < 5 y/o?
nursemaid's elbow
- subluxation of the radial head
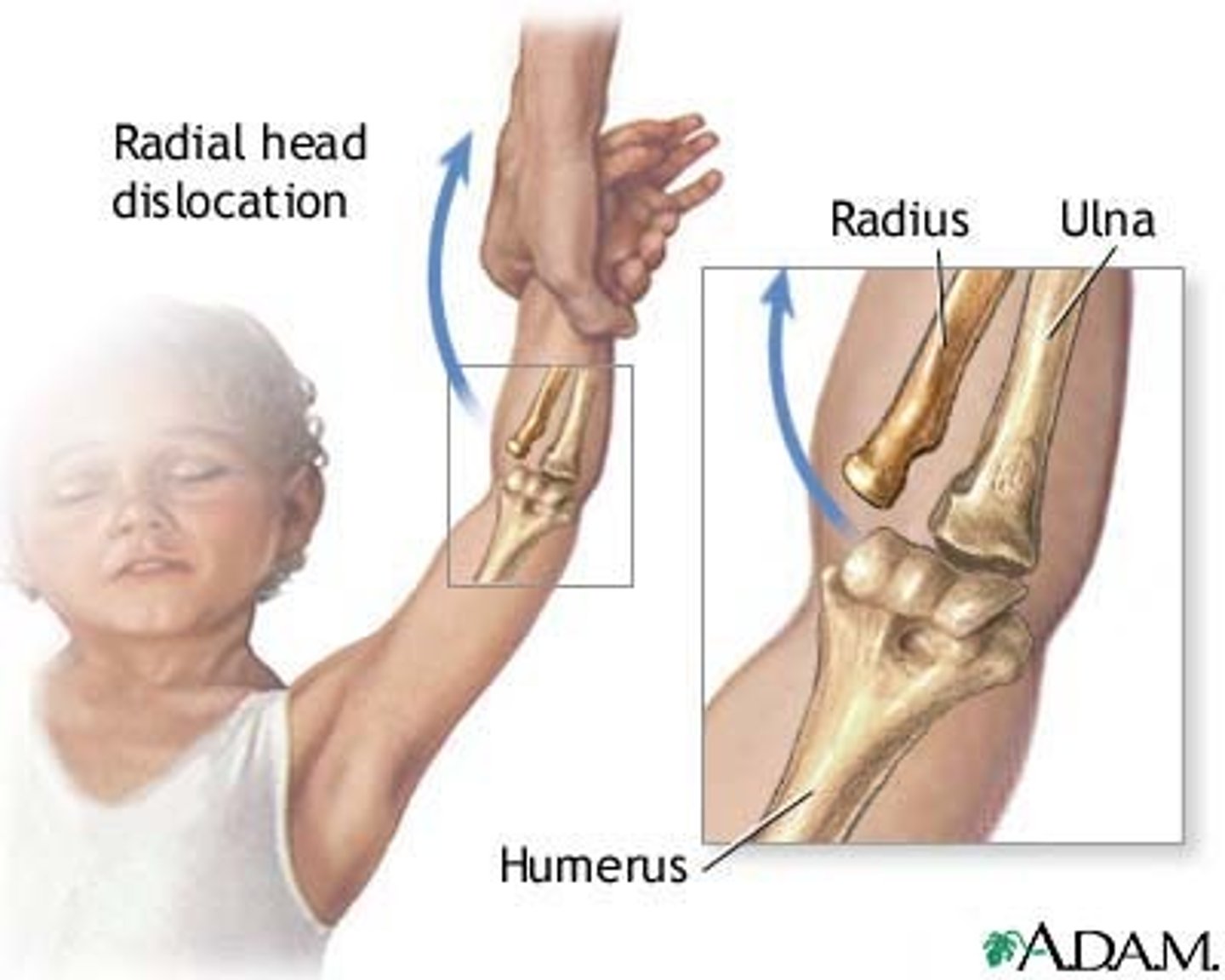
why is nursemaid's elbow common in children < 5 y/o?
due to ligamentous laxity, the annular ligament can slip from its normal position around the radial head
- can occur when the elbow is extended, & the forearm or hand is being pulled on in a pronated position
does nursemaid's elbow cause a lot of pain?
NO
- but the child will be unwilling to use his arm & will resist supination
1 multiple choice option
when is imaging warranted for nursemaid's elbow?
only if child is > 5 y/o
how is nursemaid's elbow treated?
manual reduction
- have the child extend their elbow w/ their arm hanging down in a natural position, turn their palm forward (supinate), then flex the elbow (keeping the palm in the supine position)
- alt. technique = hyperpronation
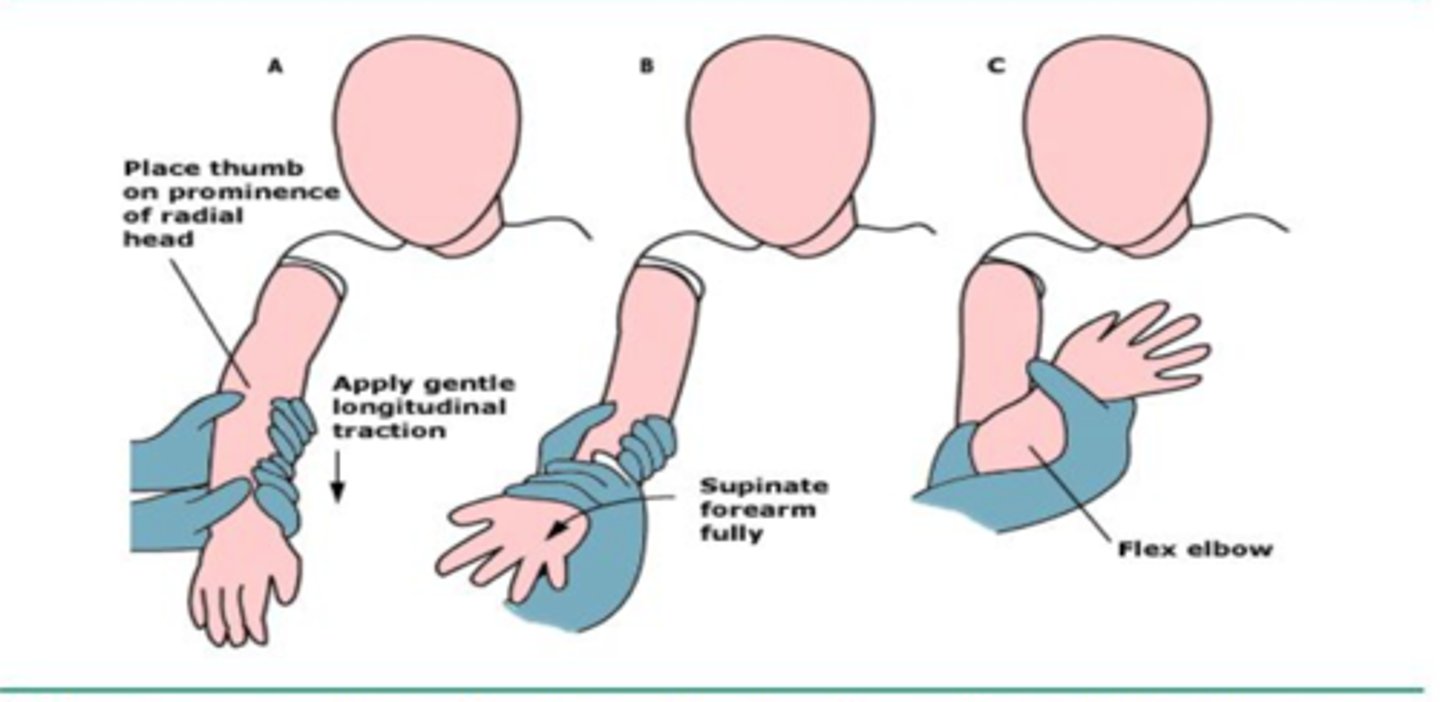
how do you know if the manual reduction has been successful?
if the elbow has full flexion & supination after manual reduction
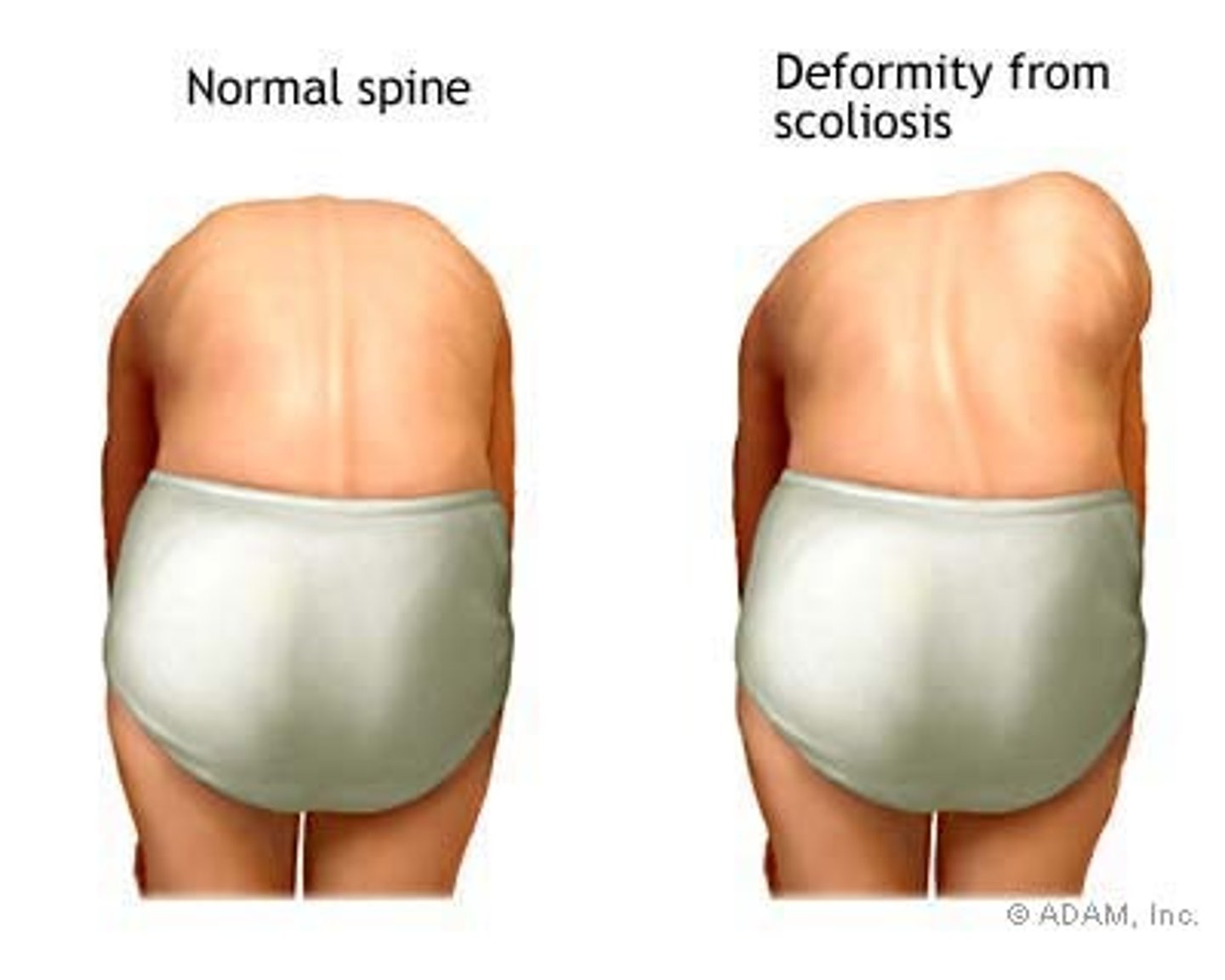
what is scoliosis?
a lateral curve of the spine >10º
- usually complicated w/ rotation of vertebrae (twist of spine), &/or kyphosis or lordosis
in which age group is scoliosis the most common?
girls between 10-16 y/o
- if occurring outside of this group (i.e. boy or <10 or >16) look for other causes
s/s of scoliosis
often asymptomatic & may be identified in a sports physical
- clothes may hang to one side, one hip may seem higher & one shoulder lower, etc
- flank crease & scapular prominence when standing upright
what can severe scoliosis lead to?
rib deformity & respiratory impairment
what is the forward bending test?
patient stands & bends forward, keeping the knees straight & hangs arms loosely towards the floor
- assess the patient from behind for thoracic/lumbar prominence or "rib hump"
what is the cobb angle?
measures the degree of curvature seen on XR
- request this w/ PA XR order (laterals are often obtained as well)
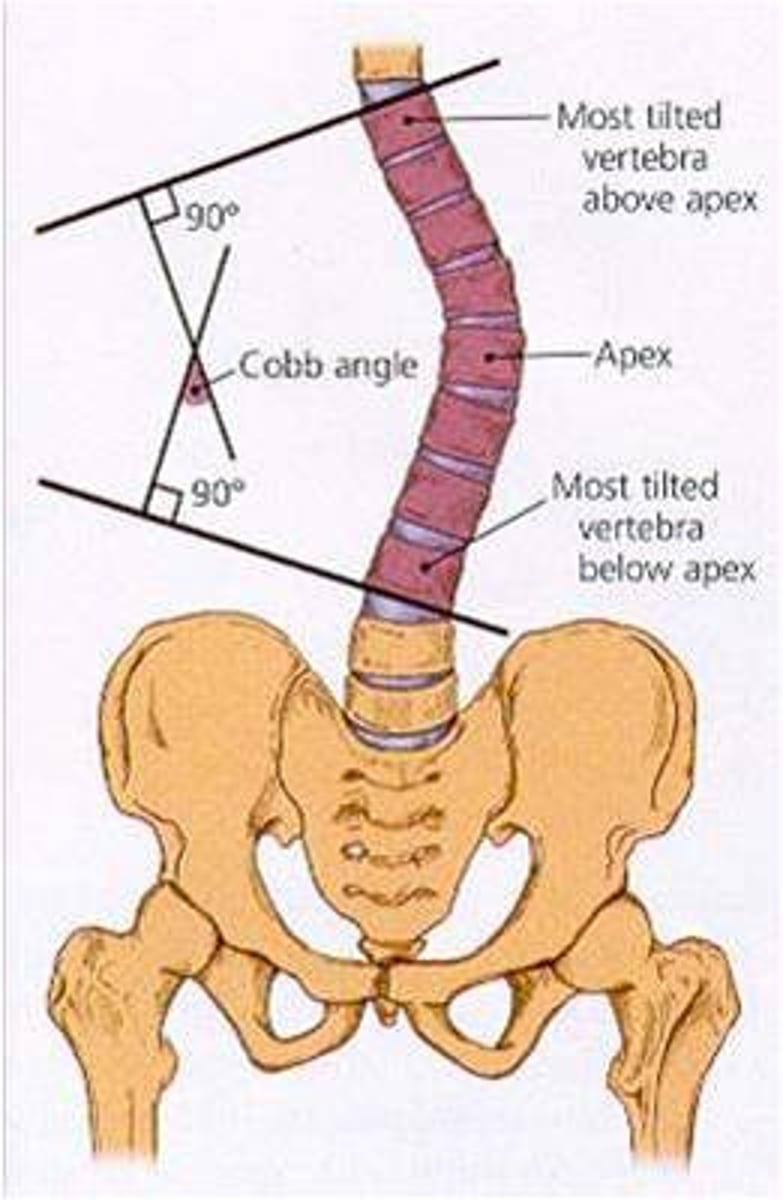
which scoliosis patients are at the highest risk for curve progression?
10-11 y/o females, who are premenarchal, & have an initial cobb angle of >/= 20º
what is the treatment for a spinal curve of <5º?
no treatment or follow-up
- considered insignificant
what is the treatment for a spinal curve of 5-20º?
observation w/ serial exams q 6 months
- no referral recommended
what is the treatment for a spinal curve of 20-40º?
full time bracing or stapling to arrest progression
- REFER!
what is the treatment for a spinal curve of >40º?
surgery evaluation
- REFER!
what is developmental dysplasia of the hip (DDH)?
spectrum of disorders usually seen in infancy that result in a femur/acetabulum joint that is dislocatable or partially dislocatable
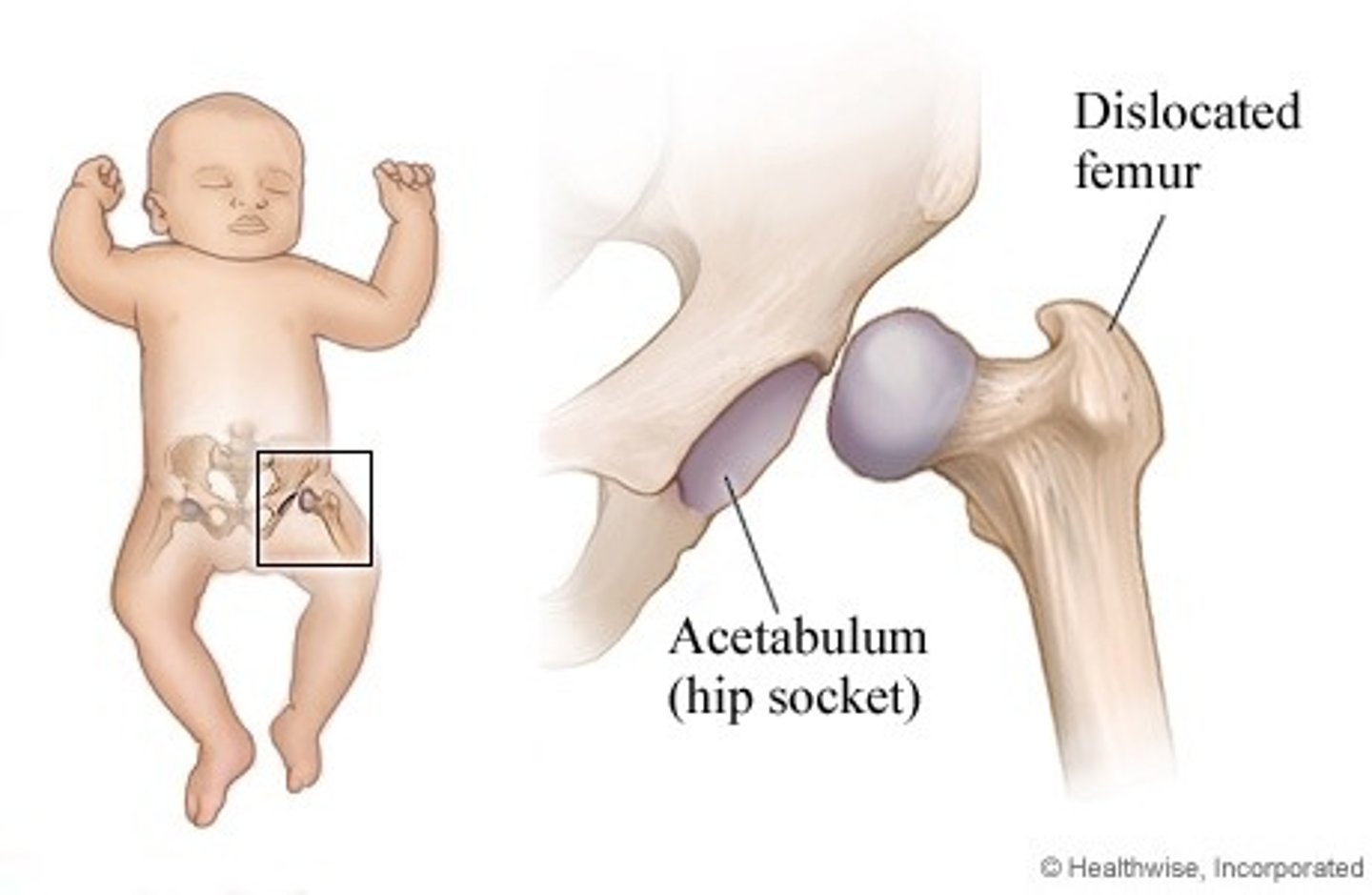
which age range is DDH seen in?
infancy (birth - 1 yr)
3 multiple choice options
what are the risk factors for DDH?
- inherited joint laxity/fam hx of DDH
- increased or extended levels of progesterone or relaxin in 3rd trimester of pregnancy (can ↑ joint laxity in baby)
- female
- 1st born child
- breech presentation at birth
- oligohydraminos
- custom of binding infants (restricts hip movement)
- associated deformity (such as foot or knee)
what can occur if DDH is not detected early?
a limp or waddling gait, or limb-length descrepancy when child begins to walk
what are the PE tests commonly used to diagnose DDH up to 3 months of age?
ortolani & barlow
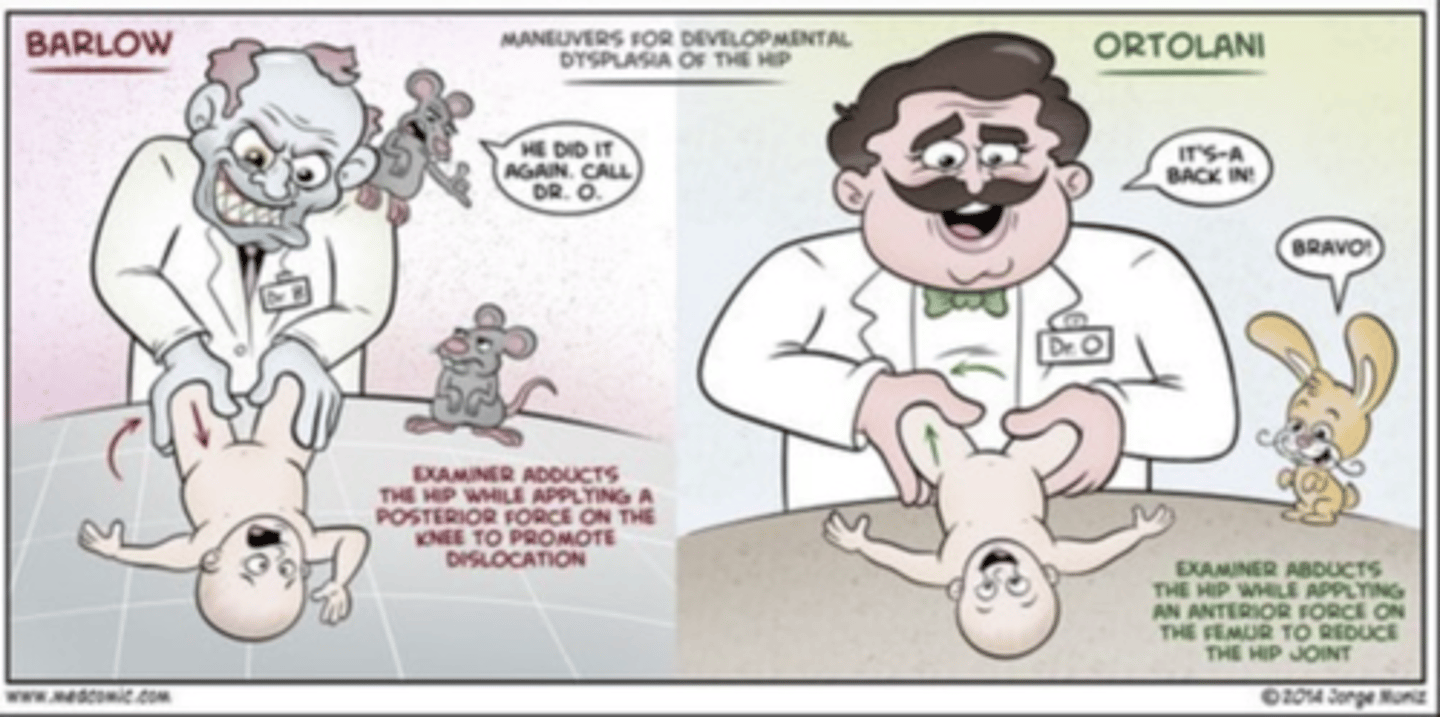
what does the ortolani test evaluate for?
an already dislocated hip
1 multiple choice option
what does the barlow test evaluate for?
if a hip is dislocatable
1 multiple choice option
what is the ortolani test?
- infant lying on back
- flex the hips
- abduct to full capacity while applying gentle pressure to push the femur anteriorly
- if hip was dislocated, this will reduce it & a pop/clunk will be felt
1 multiple choice option
what is the barlow test?
- infant lying on back
- abduct the hips
- adduct the hips back into their normal position while applying gentle pressure to push the femur posteriorly
- if dislocation occurs, a clunk will be felt
1 multiple choice option
brings the knees out
a. ortolani
b. barlow
a. ortolani
1 multiple choice option
brings the knees back to normal position
a. ortolani
b. barlow
b. barlow
1 multiple choice option
hips should be examined for DDH at routine physicals up until _______ of age.
9 mo
ortolani & barlow tests can be used to assess for DDH in infants up to __________ of age.
3 mo
what can be done to assess for DDH in infants > 3 mo?
compare L & R hip abduction w/ the patient supine & the hips flexed 90º
- f/u is needed if L & R vary by > 20º
how is DDH diagnosed?
through PE unless results are inconclusive
- if obvious "clunk" occurs on PE, immediately refer
- if inconclusive, repeat exam in 2 wks, & if still uncertain order an US
when is an ultrasound recommended in diagnosis of DDH?
in infants that have signs of instability
- usually done about 4-6 wks of age, but is test of choice up to 4 months of age
- may also be used as a screening in high risk infants, even when PE is normal (ex: female infant & older sister had DDH)
how is DDH treated?
referral to orthopedic specialist
- splinting (pavlik harness)
- more rigid orthosis
- closed or open reduction, followed by spica cast
success for treatment of DDH w/ the pavlik harness decreases after __________ of age, & is NOT attempted after 18 mo of age.
3 mo
for infants < 18 months old,
what can be tried if the pavlik harness fails?
a more rigid orthosis
or
closed reduction, followed by a spica cast
when may open reduction sometimes be tried for treatment of DDH?
in toddlers between 18-30 months
- follow the operation w/ spica casting
is treatment recommended for DDH in a child > 30 months old?
no
1 multiple choice option
what is legg-calve-perthes disease (LCPD)?
idiopathic, osteonecrosis of the femoral head in children
- usually between the ages of 4-8 y/o, but can range from 2-18 y/o
which age range is LCPD seen in?
4-8 yrs
3 multiple choice options
is LCPD more common in boys or girls?
boys
1 multiple choice option
LCPD is uncommon in blacks,
so what should you consider as a cause of the vascular disruption if it does occur?
sickle cell anemia
which is the most common cause of acute hip pain in children?
a. LCPD
b. transient synovitis
b. transient synovitis
1 multiple choice option
which has an acute onset?
a. LCPD
b. transient synovitis
b. transient synovitis
1 multiple choice option
which has a gradual onset?
a. LCPD
b. transient synovitis
a. LCPD
1 multiple choice option
which may have pain at rest, in the morning, or in an irregular pattern?
a. LCPD
b. transient synovitis
b. transient synovitis
1 multiple choice option
in which may the pain be temporarily relieved w/ rest?
a. LCPD
b. transient synovitis
a. LCPD
1 multiple choice option
in which have 50% of patients had a previous infection (URI, etc..)?
a. LCPD
b. transient synovitis
b. transient synovitis
1 multiple choice option
in which do NSAIDs & rest result in resolution w/o complications?
a. LCPD
b. transient synovitis
b. transient synovitis
1 multiple choice option
which may have big complications & NSAIDs & rest do NOT result in resolution?
a. LCPD
b. transient synovitis
a. LCPD
1 multiple choice option
what is the main complaint w/ LCPD?
insidious onset of a limp
s/s of LCPD
- insidious onset of limp
- +/- pain (often worsened w/ activity)
- abnormal gait & limited ROM (both passive & active), particularly w/ abduction & internal rotation
- possible leg length discrepency
what is the earliest sign on PE of LCPD?
loss of internal rotation
how is leg length measured?
from the anterior-superior iliac spine (ASIS) to the medial malleolus

how is LCPD diagnosed?
AP & frog lateral view XRs
- if XRs are normal, but s/s point to LCPD, get an MRI
how is LCPD treated?
refer!
- determined by age, amount of femoral head involved, & degree of ROM that has been lost
- varies from observation w/ activity restriction only to bed rest w/ traction, bracing, or surgery
- slow (taking up to 18 months)
what are the possible adverse outcomes of LCPD?
- premature degenerative changes of the hip
- limb-length discrepancies
what is slipped capital femoral epiphysis (SCFE)?
the femoral epiphysis becomes displaced from the metaphysis through the physeal plate
- during asolescence (8-15 y/o) when the orientation of the physeal plate changes from horizontal to oblique
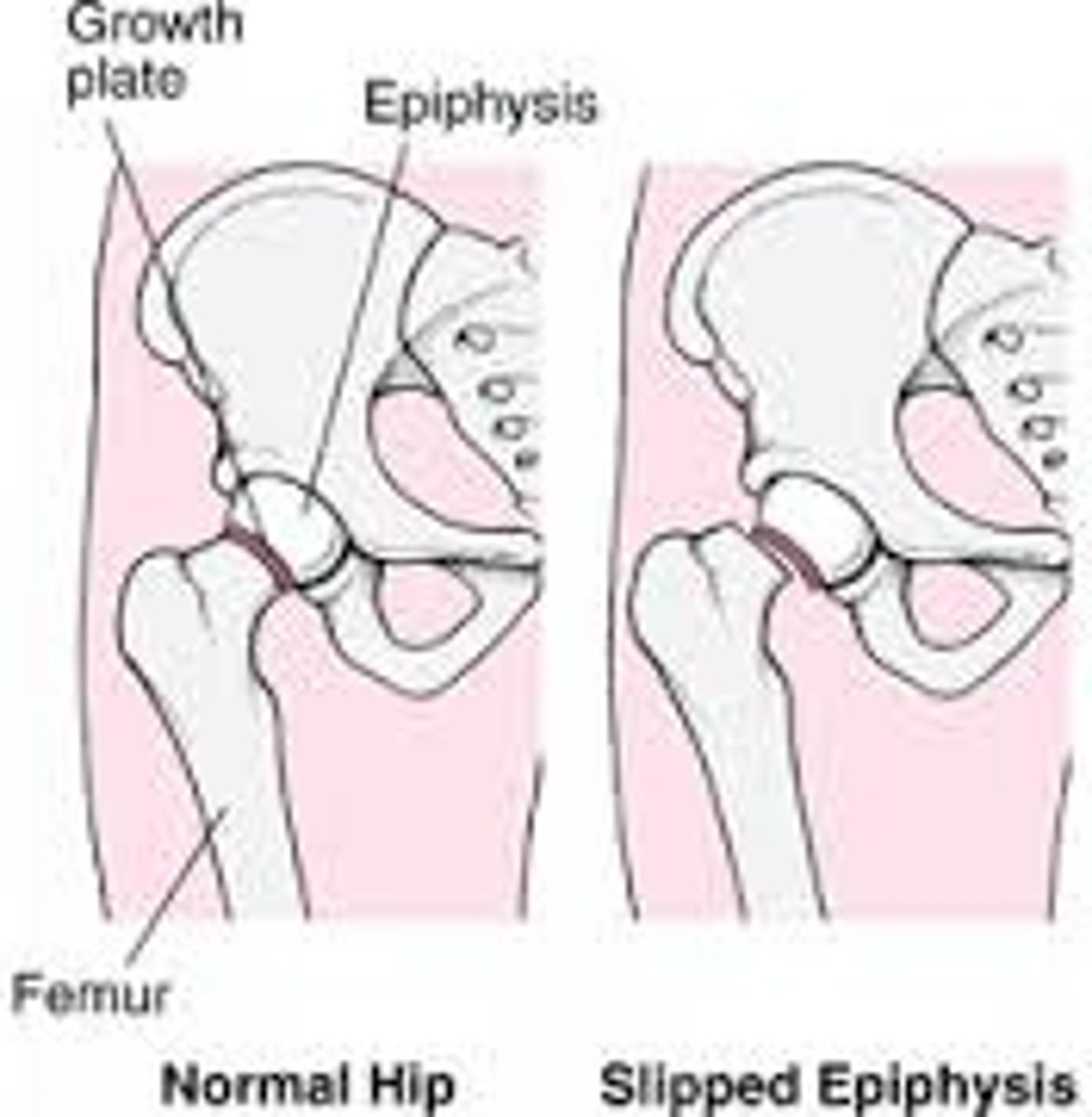
which age range is SCFE seen in?
adolescence (8-15 y/o)
3 multiple choice options
predisposing factors for SCFE include:
- obesity
- male
- african american
- endocrine abnormalities
- growth hormone supplementation
- various anatomic anomalies
what is the most common presentation of SCFE?
obese adolescent w/ pain & no hx of trauma
what should occurrence of SCFE outside of adolescence cause you to look for?
an endocrine disorder that could affect bone health
what are the possible complications of SCFE?
- osteonecrosis (most serious)
- cartilage necrosis
- osteoarthritis (OA)
s/s of SCFE
- pain, exacerbated by activity (most commonly in anterior thigh)
- asymmetric out toeing gait w/ limp
- limb length discrepancy
if the SCFE patient presents walking, w/ or w/o crutches, they are classified as _______.
a. unstable
b. stable
b. stable (90%)
1 multiple choice option
if the SCFE patient presents unable to walk, they are classified as _______, & will have a more complicated treatment regimen.
a. unstable
b. stable
a. unstable (10%)
1 multiple choice option
what test should be done on all adolescents that have lower extremity pain?
examination of hip rotation
- flex the hip to 90º, then internally rotate or place patient in prone position w/ knees bent & feet in the air (normal rotation will be symmetrical R & L)
similar to LCPD, SCFE will cause loss of:
a. external rotation
b. lateral rotation
c. internal rotation
c. internal rotation
2 multiple choice options
how is SCFE diagnosed?
AP & frog-lateral view XRs
- on AP view, if the line drawn on the superior surface of the femoral neck does NOT pass through a portion of the head
- if XR inconclusive, order MRI
on AP view, a line drawn on the superior surface of the femoral neck should pass through a portion of the head.
what finding here allows for a SCFE diagnosis?
if the line drawn on the surperior surface of the femoral neck DOES NOT pass through a portion of the head
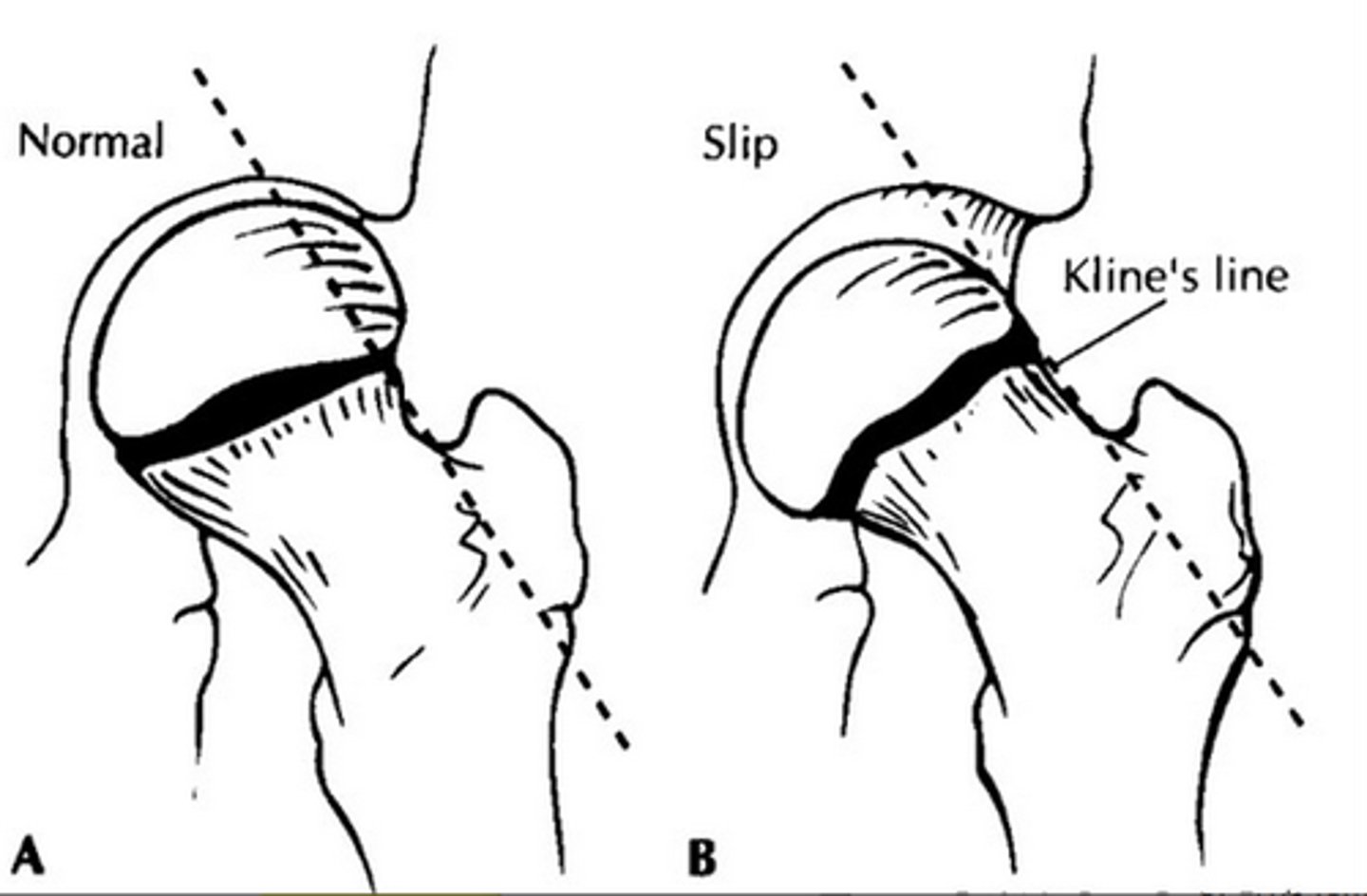
how is SCFE treated?
patient should immediately become non-weight bearing to avoid additional slippage
- DO NOT DELAY TREATMENT
- REFER for surgery (fixation w/ 1-2 screws, followed by 6-9 mo of activity restriction)!
which is a bowlegged appearance?
a. genu valgum
b. genu varum
b. genu varum
1 multiple choice option
which is a knock-kneed appearance?
a. genu valgum
b. genu varum
a. genu valgum
1 multiple choice option
what is the goal of evaluation of genu varum or valgum?
to determine if it's normal physiologic development or if a pathologic process may be involved
- it's typically a normal variation w/i certain stages of development & resolves spontaneously
what things should you consider during PE of a patient w/ genu varum or valgum?
- does the child have normal height & proportion?
- are other deformities present?
- are the limb lengths equal? is there symmetry?
- is the "disorder" occurring at appropriate time in development?
- is there a familial tendency?
what is blount's disease?
an inherited form of extreme bowleggedness
genu varum (bowlegged) is common up to _____________.
18 months
1 multiple choice option
genu valgum (knock-kneed) is common between _____________ (& if found during this time will spontaneously correct 99% of the time).
3-4 years
1 multiple choice option
genu varum is normal up to ___ inches between the knees.
2 inches
3 multiple choice options
genu valgum is common between 3-4 years, & usually resolves by ______ years.
5-8 years
3 multiple choice options
when should you consider referral for genu varum?
- no improvement by age 2
- other concerns found on PE
when should you consider referral for genu valgum?
- > 2 inches between medial malleoli when the patient is standing with their knees together (knock knees come in together but he ankles go out the other way)
- other concerns found on PE
what is osteochondrosis?
a defect in endochondral ossification which causes the deeper layers of articular cartilage to die
- a loosely connected group of disorders that affect the growing skeleton; typically resolves w/ skeletal maturity & no operative treatment
what is osgood-schlatters (OSD)?
outgrowing of bone, inflammation & possible separation of the apohysis of the tibial tubercle due to repetitive microtrauma
- overuse of quadriceps
- most common in athletic boys, but also seen in girls, ages 10-14
types of osteochondrosis:
- medial condyle apophysitis
- panner disease
- osgood schlatter disease (OSD)
- sinding larsen johansson (SLJ) disease
- calcaneal apophysitis (sever's disease)
- kohler disease
- freiberg disease
which age range is OSD most common in?
10-14 y/o
3 multiple choice options
s/s of OSD
- swelling or firm prominence & tenderness over tibial tubercle
- pain which increases w/ activity (esp. running, jumping, & kneeling)
- stable knee joint
- normal ROM
how is OSD diagnosed?
XR NOT required, but may be helpful
- lateral view can show prominence of tibial tubercle & fragmentation
how is osgood schlatters treated?
NSAIDs & decreased activity
- rehab of quads & hamstrings
- pain > 3 months = inj. of hyperosmolar dextrose (NO steroid inj.)
what is sinding-larson-johansson disease (SLJ)?
very similar to OSD, but the point of pain is at the inferior patella instead of the tibial tuberosity
- same treatment
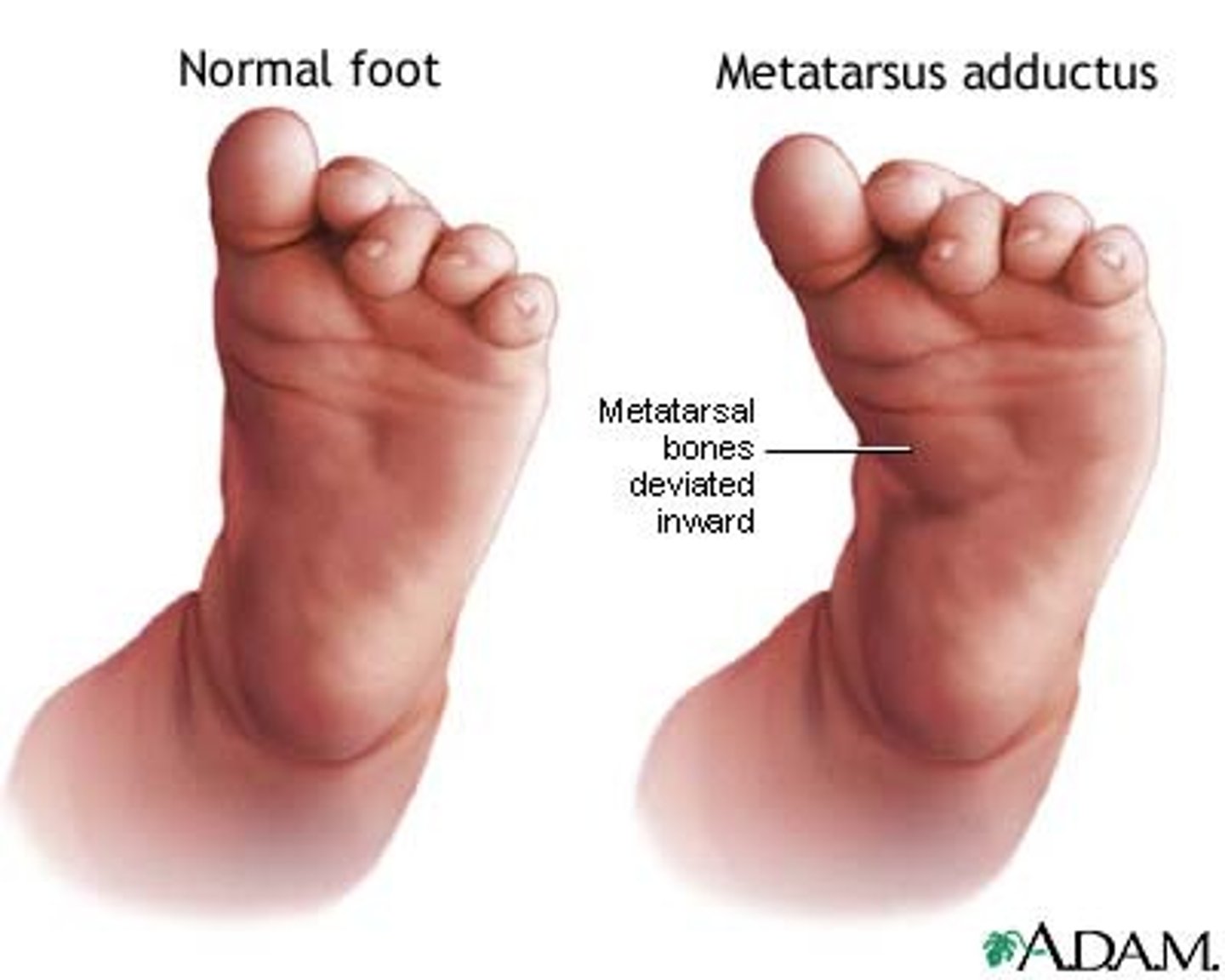
what is metatarsus adductus (MTA)?
medial deviation of the forefoot
- commonly seen in infants
- often a result of intrauterine position
- must differentiate between flexible vs inflexible on PE
similar to DDH, which age range is MTA commonly seen in?
infancy
3 multiple choice options
which form of MTA can be manually straightened on PE?
a. flexible
b. inflexible (rigid)
a. flexible
1 multiple choice option
which form of MTA CANNOT be manually corrected on PE?
a. flexible
b. inflexible (rigid)
b. inflexible (rigid)
1 multiple choice option
what is the inflexible form of MTA sometimes also called?
metatarsus varus (MTV)
which type of MTA spontaneously resolves w/i 1 yr?
a. inflexible (MTV)
b. flexible
b. flexible
1 multiple choice option
which type of MTA DOES NOT spontaneously resolve, & is persistent?
a. inflexible (MTV)
b. flexible
a. inflexible (MTV)
1 multiple choice option
which type of MTA may result in a cosmetic problem?
a. inflexible (MTV)
b. flexible
a. inflexible (MTV)
1 multiple choice option
which type of MTA warrants a referral if persistent to >/= 1 yr?
a. inflexible (MTV)
b. flexible
b. flexible
1 multiple choice option
which type of MTA warrants a referral before 6 months of age?
a. inflexible (MTV)
b. flexible
a. inflexible (MTV)
1 multiple choice option